Comparison of Single and Combined Treatment with Exercise Therapy and Collagen Supplementation on Early Knee Arthritis among Athletes—A Quasi-Randomized Trial
Abstract
:1. Introduction
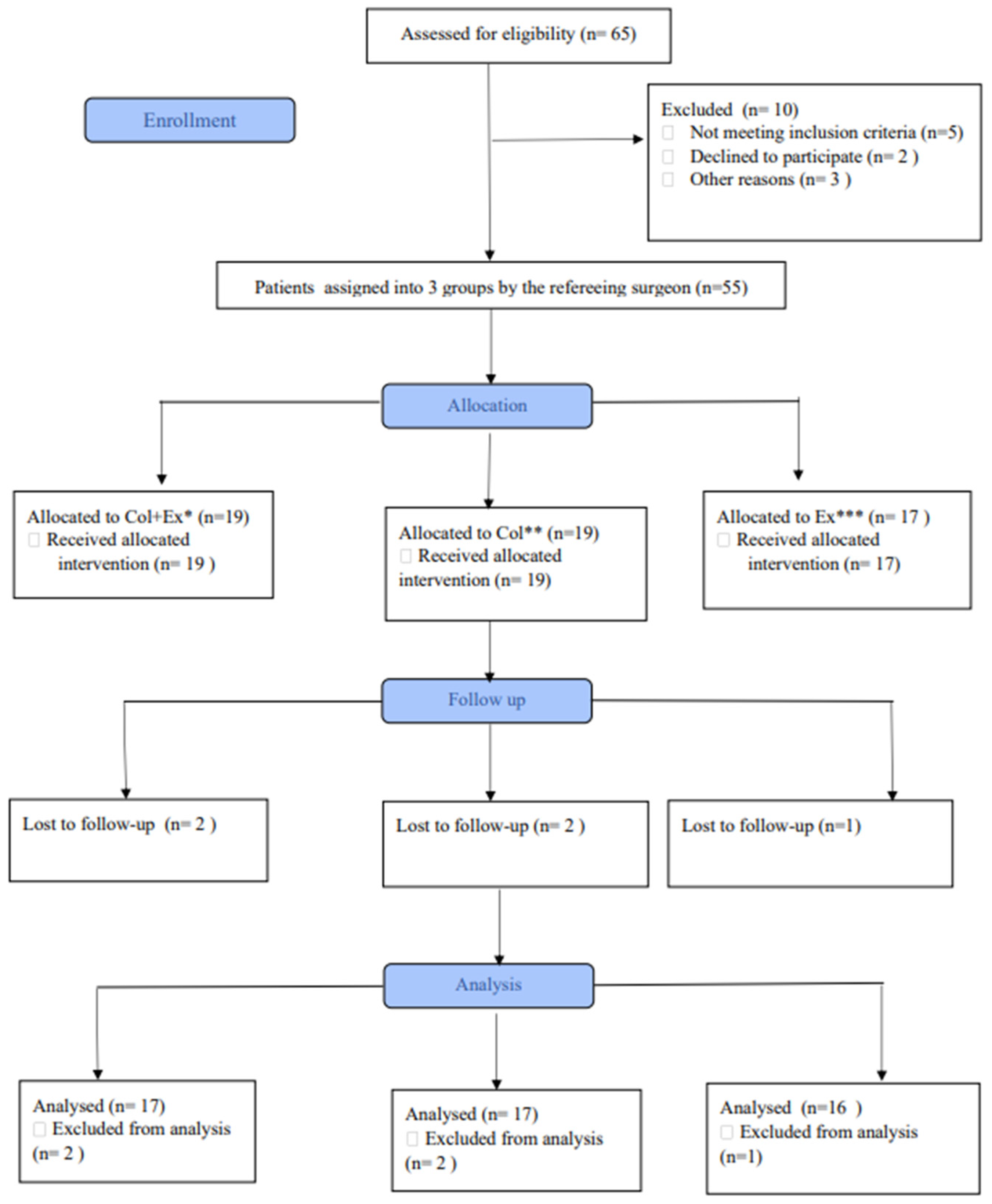
2. Methods
2.1. Design and Participants
2.2. Instruments
2.3. Intervention
- (1)
- hip muscle strengthening exercises, including hip flexors, abductors, adductors, and extensors;
- (2)
- knee muscle strengthening exercises, including dynamic quadriceps exercise, hamstring curls, gastrocnemius stretching, and squatting;
- (3)
- cycling.
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics
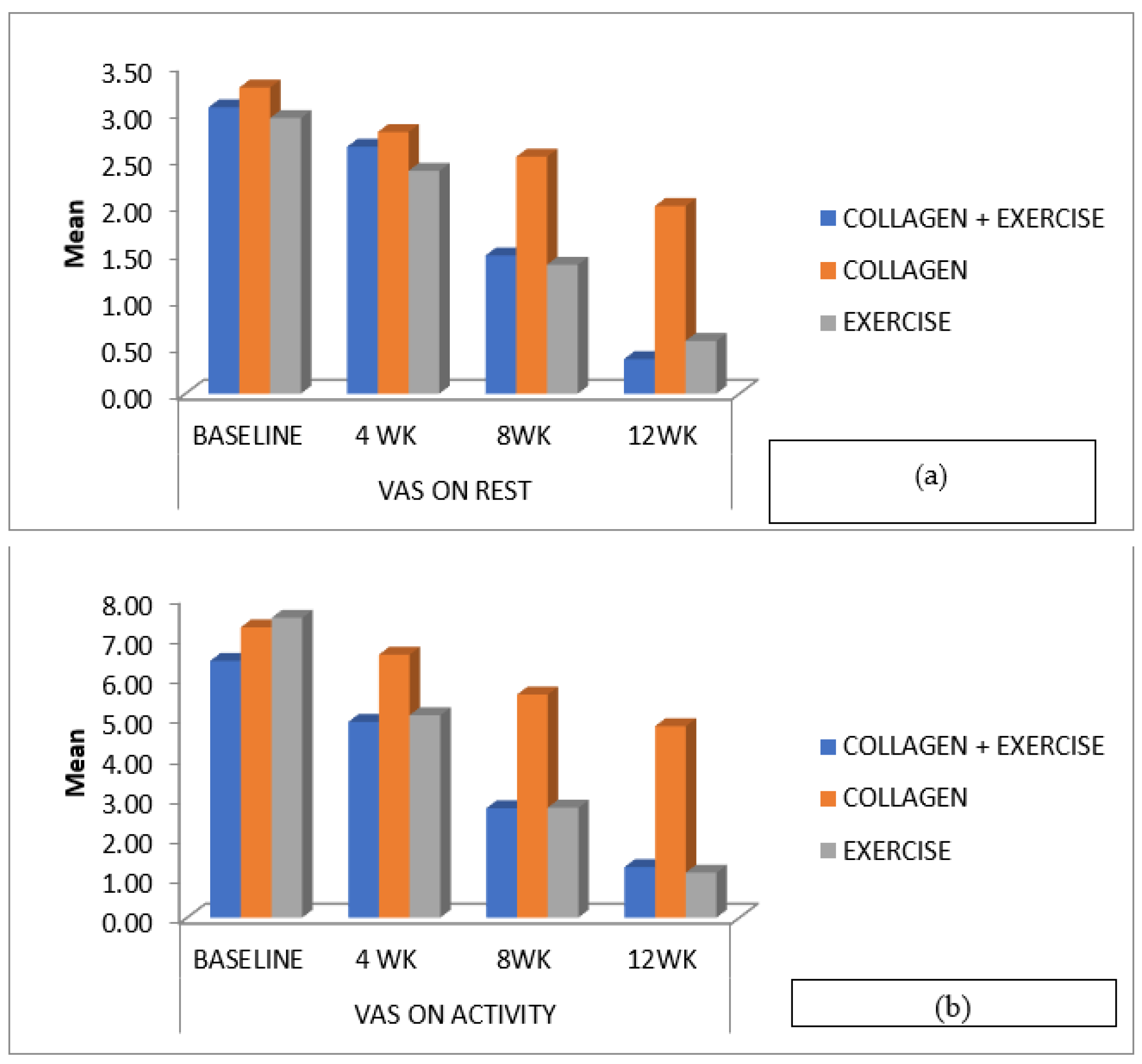
3.2. Pain Score at Weeks 4, 8 and 12
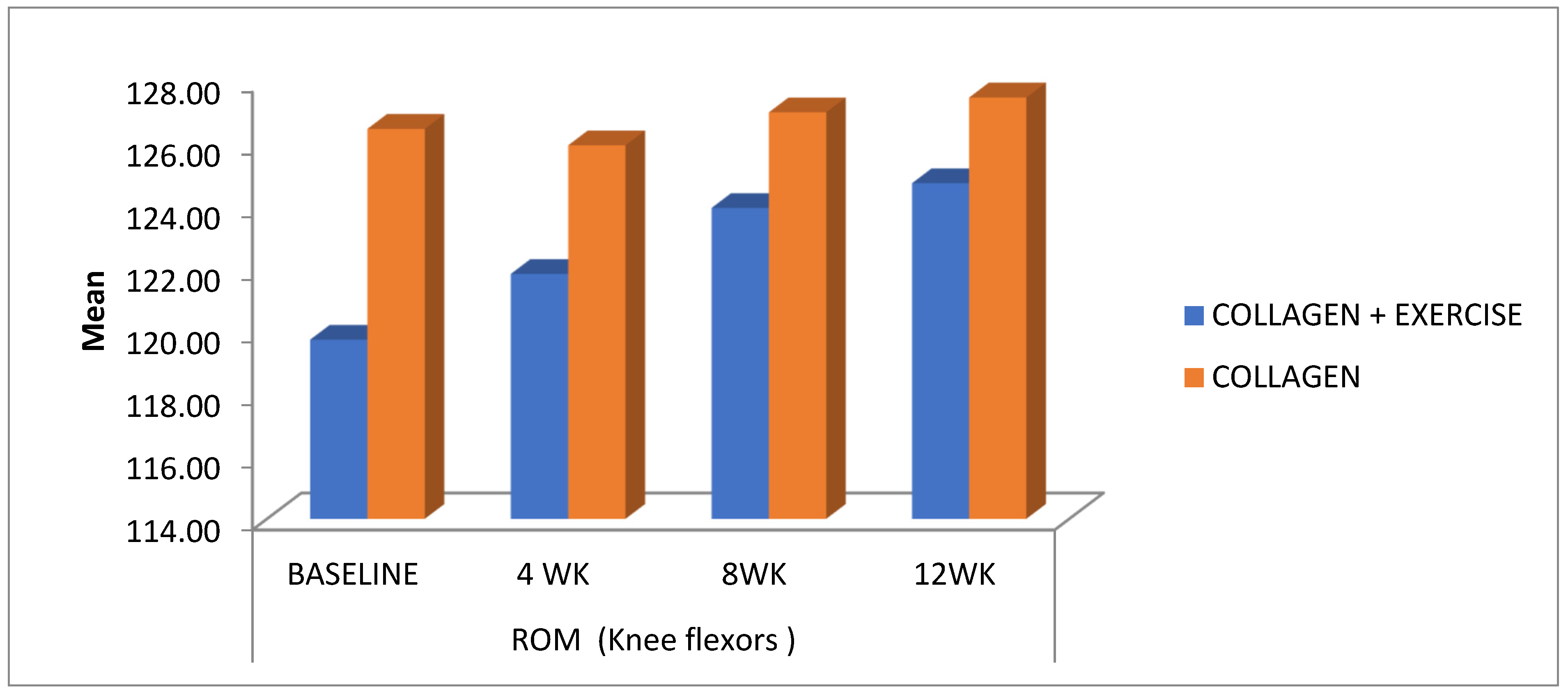
3.3. Knee Flexion ROM at Weeks 4, 8 and 12
3.4. Knee Flexor Strength at Weeks 4, 8 and 12
3.5. KOOS Score at Weeks 4, 8 and 12
4. Discussion
5. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Papalia, R.; Torre, G.; Zampogna, B.; Vorini, F.; Grasso, A.; Denaro, V. Sport activity as risk factor for early knee osteoarthritis. J. Biol. Regul. Homeost. Agents 2019, 33, 29–37. [Google Scholar] [PubMed]
- Louw, Q.A.; Manilall, J.; Grimmer, K.A. Epidemiology of knee injuries among adolescents: A systematic review. Br. J. Sports Med. 2008, 42, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Filardo, G.; Kon, E.; Longo, U.G.; Madry, H.; Marchettini, P.; Marmotti, A.; Van Assche, D.; Zanon, G.; Peretti, G.M. Non-surgical treatments for the management of early osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1775–1785. [Google Scholar] [CrossRef] [PubMed]
- John, R.; Dhillon, M.; Syam, K.; Prabhakar, S.; Behera, P.; Singh, H. Epidemiological profile of sports-related knee injuries in northern India: An observational study at a tertiary care centre. J. Clin. Orthop. Trauma 2016, 7, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Vannini, F.; Spalding, T.; Andriolo, L.; Berruto, M.; Denti, M.; Espregueira-Mendes, J.; Menetrey, J.; Peretti, G.; Seil, R.; Filardo, G. Sport and early osteoarthritis: The role of sport in aetiology, progression and treatment of knee osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1786–1796. [Google Scholar] [CrossRef]
- Pal, C.P.; Singh, P.; Chaturvedi, S.; Pruthi, K.K.; Vij, A. Epidemiology of knee osteoarthritis in India and related factors. Indian J. Orthop. 2016, 50, 518. [Google Scholar] [CrossRef]
- Heidari, B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Casp. J. Intern. Med. 2021, 2, 205. [Google Scholar]
- Madry, H.; Luyten, F.P.; Facchini, A. Biological aspects of early osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 407–422. [Google Scholar] [CrossRef]
- Grazina, R.; Andrade, R.; Bastos, R.; Costa, D.; Pereira, R.; Marinhas, J.; Maestro, A.; Espregueira-Mendes, J. Clinical management in early OA. Adv. Exp. Med. Biol. 2018, 1059, 111–135. [Google Scholar] [CrossRef]
- Prabhakar, A.J.; Joshua, A.M.; Prabhu, S.; Kamat, Y.D. Effectiveness of proprioceptive training versus conventional exercises on postural sway in patients with early knee osteoarthritis—A randomized controlled trial protocol. Int. J. Surg. Protoc. 2020, 24, 6–11. [Google Scholar] [CrossRef]
- Michael, J.W.-P.; Schlüter-Brust, K.U.; Eysel, P. The Epidemiology, Etiology, Diagnosis, and Treatment of Osteoarthritis of the Knee. Dtsch. Arztebl. Int. 2010, 107, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Villalobos, A. Evaluation and management of knee pain in young athletes: Overuse injuries of the knee. Transl. Pediatr. 2017, 6, 190–198. [Google Scholar] [CrossRef]
- Zhang, W.; Jones, A.; Doherty, M. Does paracetamol (acetaminophen) reduce the pain of osteoarthritis?: A meta-analysis of randomised controlled trials. Ann. Rheum. Dis. 2004, 63, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Paterson, K.L.; Metcalf, B.R.; Duong, V.; Eyles, J.; Kasza, J.; Wang, Y.; Cicuttini, F.; Buchbinder, R.; Forbes, A.; et al. Effect of Intra-Articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients with Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2021, 326, 2021–2030. [Google Scholar] [CrossRef]
- Zdzieblik, D.; Oesser, S.; Gollhofer, A.; König, D. Improvement of activity-related knee joint discomfort following supplementation of specific collagen peptides. Appl. Physiol. Nutr. Metab. 2017, 42, 588–595. [Google Scholar] [CrossRef]
- Iwai, K.; Hasegawa, T.; Taguchi, Y.; Morimatsu, F.; Sato, K.; Nakamura, Y.; Higashi, A.; Kido, Y.; Nakabo, Y.; Ohtsuki, K. Identification of food-derived collagen peptides in human blood after oral ingestion of gelatin hydrolysates. J. Agric. Food Chem. 2005, 53, 6531–6536. [Google Scholar] [CrossRef]
- Ohara, H.; Iida, H.; Ito, K.; Takeuchi, Y.; Nomura, Y. Effects of Pro-Hyp, a collagen hydrolysate-derived peptide, on hyaluronic acid synthesis using in vitro cultured synovium cells and oral ingestion of collagen hydrolysates in a guinea pig model of osteoarthritis. Biosci. Biotechnol. Biochem. 2010, 74, 2096–2099. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.R.; Vincent, H.K. Concentric and Eccentric Resistance Training Comparison on Physical Function and Functional Pain Outcomes in Knee Osteoarthritis: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2020, 99, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Olagbegi, O.M.; Adegoke, B.O.A.; Odole, A.C. Effectiveness of combined chain exercises on pain and function in patients with knee osteoarthritis. Bangladesh J. Med. Sci. 2016, 15, 178–188. [Google Scholar] [CrossRef]
- Goh, S.-L.; Persson, M.S.; Stocks, J.; Hou, Y.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Efficacy and potential determinants of exercise therapy in knee and hip osteoarthritis: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2019, 62, 356–365. [Google Scholar] [CrossRef]
- García-Coronado, J.M.; Martínez-Olvera, L.; Elizondo-Omaña, R.E.; Acosta-Olivo, C.A.; Vilchez-Cavazos, F.; Simental-Mendía, L.E.; Simental-Mendía, M. Effect of collagen supplementation on osteoarthritis symptoms: A meta-analysis of randomized placebo-controlled trials. Int. Orthop. 2019, 43, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Favero, M.; Ramonda, R.; Goldring, M.B.; Goldring, S.R.; Punzi, L. Early knee osteoarthritis. RMD Open 2015, 1, e000062. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, T.T.; Arghandawi, S.; Brand, J.; Akanji, O.; Bader, D.L.; Salter, D.M.; Lee, D.A. Dynamic compression counteracts IL-1β induced inducible nitric oxide synthase and cyclo-oxygenase-2 expression in chondrocyte/agarose constructs. Arthritis Res. Ther. 2008, 10, R35. [Google Scholar] [CrossRef] [PubMed]
- Bokaeian, H.R.; Bakhtiary, A.H.; Mirmohammadkhani, M.; Moghimi, J. Quadriceps strengthening exercises may not change pain and function in knee osteoarthritis. J. Bodyw. Mov. Ther. 2018, 22, 528–533. [Google Scholar] [CrossRef]
- Bartholdy, C.; Klokker, L.; Bandak, E.; Bliddal, H.; Henriksen, M. A Standardized ‘Rescue’ Exercise Program for Symptomatic Flare-up of Knee Osteoarthritis: Description and Safety Considerations. J. Orthop. Sports Phys. Ther. 2016, 46, 942–946. [Google Scholar] [CrossRef]
- Clark, K.L.; Sebastianelli, W.; Flechsenhar, K.R.; Aukermann, D.F.; Meza, F.; Millard, R.L.; Deitch, J.R.; Sherbondy, P.S.; Albert, A. 24-Week study on the use of collagen hydrolysate as a dietary supplement in athletes with activity-related joint pain. Curr. Med. Res. Opin. 2008, 24, 1485–1496. [Google Scholar] [CrossRef]
- Bruyère, O.; Zegels, B.; Leonori, L.; Rabenda, V.; Janssen, A.; Bourges, C.; Reginster, J.-Y. Effect of collagen hydrolysate in articular pain: A 6-month randomized, double-blind, placebo controlled study. Complement. Ther. Med. 2012, 20, 124–130. [Google Scholar] [CrossRef]
- Lugo, J.P.; Saiyed, Z.M.; Lane, N.E. Efficacy and tolerability of an undenatured type II collagen supplement in modulating knee osteoarthritis symptoms: A multicenter randomized, double-blind, placebo-controlled study. Nutr. J. 2016, 15, 14. [Google Scholar] [CrossRef]
- Jayabalan, P.; Ihm, J. Rehabilitation strategies for the athletic individual with early knee osteoarthritis. Curr. Sports Med. Rep. 2016, 15, 177–183. [Google Scholar] [CrossRef]

| Outcome | Time | ColEx | Col | Ex | p-Value ColEx | p-Value Col | p-Value Ex |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | (p < 0.05) | (p < 0.05) | (p < 0.05) | ||
| VAS on rest | Baseline | 3.05 ± 1.649 | 3.26 ± 1.628 | 2.94 ± 1.769 | |||
| 4 WK | 2.63 ± 1.802 | 2.79 ± 1.437 | 2.38 ± 1.544 | 0.119 | 0.008 ** | 0.007 ** | |
| 8 WK | 1.47 ± 1.349 | 2.53 ± 1.504 | 1.38 ± 1.204 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 0.37 ± 0.597 | 2.00 ± 1.291 | 0.56 ± 0.629 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| VAS on activity | Baseline | 6.42 ± 1.216 | 7.26 ± 1.327 | 7.50 ± 0.894 | |||
| 4 WK | 4.89 ± 1.883 | 6.58 ± 1.305 | 5.06 ± 0.998 | 0.0001 **** | 0.001 *** | 0.0001 **** | |
| 8 WK | 2.74 ± 1.327 | 5.58 ± 1.387 | 2.75 ± 1.125 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 1.26 ± 0.872 | 4.79 ± 1.548 | 1.13 ± 1.769 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| KOOS ADL | Baseline | 50.74 ± 12.823 | 46.84 ± 17.069 | 54.88 ± 8.801 | |||
| 4 WK | 60.42 ± 9.063 | 51.00 ± 13.178 | 68.75 ± 7.479 | 0.0001 **** | 0.002 * | 0.0001 **** | |
| 8 WK | 75.47 ± 6.883 | 54.84 ± 11.899 | 82.38 ± 8.065 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 87.32 ± 6.709 | 59.05 ± 12.236 | 89.25 ± 5.040 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| KOOS pain | Baseline | 48.11 ± 13.984 | 43.68 ± 12.845 | 50.19 ± 9.897 | |||
| 4 WK | 59.26 ± 10.514 | 46.05 ± 12.058 | 66.50 ± 10.040 | 0.001 *** | 0.038 * | 0.0001 **** | |
| 8 WK | 74.26 ± 7.164 | 51.00 ± 9.383 | 80.63 ± 9.323 | 0.0001 **** | 0.001 *** | 0.0001 **** | |
| 12 WK | 85.26 ± 6.707 | 57.84 ± 11.969 | 89.50 ± 40761 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| KOOS QOL | Baseline | 36.00 ± 11.324 | 35.63 ± 15.582 | 39.56 ± 10.013 | |||
| 4 WK | 47.42 ± 8.965 | 42.89 ± 13.008 | 56.38 ± 10.443 | 0.0001 **** | 0.003 * | 0.0001 **** | |
| 8 WK | 65.26 ± 7.362 | 50.47 ± 12.330 | 69.94 ± 9.849 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 75.74 ± 69.10 | 55.05 ± 9.936 | 77.50 ± 8.532 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| KOOS sports/rec | Baseline | 36.05 ± 17.206 | 26.05 ± 14.296 | 37.56 ± 9.919 | |||
| 4 WK | 50.53 ± 13.218 | 33.68 ± 13.107 | 57.63 ± 10.782 | 0.0001 **** | 0.003 **** | 0.0001 **** | |
| 8 WK | 68.68 ± 9.405 | 44.21 ± 9.897 | 74.56 ± 8.148 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 79.47 ± 8.481 | 50.26 ± 7.723 | 82.76 ± 7.767 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| KOOS symptoms | Baseline | 54.16 ± 18.679 | 44.21 ± 10.438 | 60.25 ± 15.864 | 0.0001 **** | ||
| 4 WK | 61.11 ± 12.635 | 46.16 ± 9.518 | 74.25 ± 9.657 | 0.037 * | 0.057 * | 0.0001 **** | |
| 8 WK | 76.16 ± 9.002 | 54.79 ± 7.850 | 85.56 ± 7.248 | 0.0001 **** | 0.0001 **** | 0.0001 **** | |
| 12 WK | 86.37 ± 8.050 | 59.00 ± 9.292 | 90.81 ± 5.294 | 0.0001 **** | 0.0001 **** | 0.0001 **** |
| Outcome | Time | ColEx | Col | Ex | p-Value ColEx | p-Value Col | p-Value Ex |
|---|---|---|---|---|---|---|---|
| ROM (knee flexors) | Baseline | 119.74 ± 10.862 | 126.47 ± 5.491 | 122.50 ± 9.129 | |||
| 4 WK | 121.84 ± 8.852 | 125.95 ± 6.527 | 126.50 ± 5.888 | 0.016 * | 0.331 | 0.081 | |
| 8 WK | 123.95 ± 7.920 | 127.00 ± 5.568 | 129.69 ± 5.313 | 0.001 * | 0.163 | 0.012 * | |
| 12 WK | 124.74 ± 7.355 | 127.47 ± 5.197 | 129.69 ± 5.313 | 0.001 * | 0.111 | 0.012 * | |
| Muscle strength (flexors) | Baseline | 4.89 ± 1.370 | 6.79 ± 3.084 | 6.00 ± 2.366 | |||
| 4 WK | 5.37 ± 1.422 | 6.74 ± 3.160 | 6.44 ± 2.529 | 0.003 * | 0.331 | 0.110 | |
| 8 WK | 6.21 ± 1.475 | 6.95 ± 3.135 | 7.13 ± 2.527 | 0.000 * | 0.268 | 0.000 * | |
| 12 WK | 6.63 ± 1.383 | 7.16 ± 3.351 | 7.75 ± 2.408 | 0.000 * | 0.031 * | 0.000 * | |
| Muscle strength (extensors) | Baseline | 8.53 ± 2.736 | 10.32 ± 3.351 | 9.31 ± 3.439 | |||
| 4 WK | 8.74 ± 2.746 | 10.32 ± 3.318 | 9.50 ± 3.307 | 0.259 | 1.000 | 0.270 | |
| 8 WK | 9.68 ± 2.849 | 10.42 ± 3.237 | 10.25 ± 3.568 | 0.000 * | 0.494 | 0.000 * | |
| 12 WK | 10.11 ± 2.622 | 10.63 ± 3.270 | 10.94 ± 3.376 | 0.000 * | 0.111 | 0.000 * |
| TIME | ColEx vs. Col (p < 0.05) | ColEx vs. Ex (p < 0.05) | Col vs. Ex (p < 0.05) | |
|---|---|---|---|---|
| VAS on rest | Baseline - 4 WK | 1.000 | 1.000 | 1.000 |
| Baseline - 8 WK | 0.081 | 1.000 | 0.113 | |
| Baseline - 12 WK | 0.010 * | 1.000 | 0.077 | |
| VAS on activity | Baseline - 4 WK | 0.083 | 0.069 | 0.000 * |
| Baseline - 8 WK | 0.000 * | 0.041 * | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 0.023 * | 0.000 * | |
| ROM (knee flexion) | Baseline - 4 WK | 0.388 | 0.880 | 0.043 * |
| Baseline - 8 WK | 0.218 | 0.488 | 0.008 * | |
| Baseline - 12 WK | 0.193 | 0.983 | 0.022 * | |
| Muscle strength (flexors) | Baseline - 4 WK | 0.063 | 1.000 | 0.116 |
| Baseline - 8 WK | 0.000 * | 1.000 | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| Muscle strength (extensors) | Baseline - 4 WK | 0.900 | 1.000 | 1.000 |
| Baseline - 8 WK | 0.000 * | 1.000 | 0.002 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| KOOS ADL | Baseline - 4 WK | 0.069 | 0.286 | 0.001 * |
| Baseline - 8 WK | 0.000 * | 1.000 | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| KOOS pain | Baseline - 4 WK | 0.017 * | 0.337 | 0.000 * |
| Baseline - 8 WK | 0.000 * | 0.727 | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| KOOS QOL | Baseline - 4 WK | 0.517 | 0.277 | 0.011 * |
| Baseline - 8 WK | 0.000 * | 1.000 | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| KOOS sports/rec | Baseline - 4 WK | 0.142 | 0.355 | 0.003 * |
| Baseline - 8 WK | 0.001 * | 0.865 | 0.000 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.000 * | |
| KOOS symptoms | Baseline - 4 WK | 0.379 | 0.123 | 0.002 * |
| Baseline - 8 WK | 0.008 * | 1.000 | 0.001 * | |
| Baseline - 12 WK | 0.000 * | 1.000 | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomas, D.T.; Prabhakar, A.J.; Eapen, C.; Patel, V.D.; Palaniswamy, V.; Dsouza, M.C.; R, S.; Kamat, Y.D. Comparison of Single and Combined Treatment with Exercise Therapy and Collagen Supplementation on Early Knee Arthritis among Athletes—A Quasi-Randomized Trial. Int. J. Environ. Res. Public Health 2023, 20, 7088. https://doi.org/10.3390/ijerph20237088
Thomas DT, Prabhakar AJ, Eapen C, Patel VD, Palaniswamy V, Dsouza MC, R S, Kamat YD. Comparison of Single and Combined Treatment with Exercise Therapy and Collagen Supplementation on Early Knee Arthritis among Athletes—A Quasi-Randomized Trial. International Journal of Environmental Research and Public Health. 2023; 20(23):7088. https://doi.org/10.3390/ijerph20237088
Chicago/Turabian StyleThomas, Dias Tina, Ashish John Prabhakar, Charu Eapen, Vivek D. Patel, Vijayakumar Palaniswamy, Molly Cynthia Dsouza, Shruthi R, and Yogeesh Dattakumar Kamat. 2023. "Comparison of Single and Combined Treatment with Exercise Therapy and Collagen Supplementation on Early Knee Arthritis among Athletes—A Quasi-Randomized Trial" International Journal of Environmental Research and Public Health 20, no. 23: 7088. https://doi.org/10.3390/ijerph20237088
APA StyleThomas, D. T., Prabhakar, A. J., Eapen, C., Patel, V. D., Palaniswamy, V., Dsouza, M. C., R, S., & Kamat, Y. D. (2023). Comparison of Single and Combined Treatment with Exercise Therapy and Collagen Supplementation on Early Knee Arthritis among Athletes—A Quasi-Randomized Trial. International Journal of Environmental Research and Public Health, 20(23), 7088. https://doi.org/10.3390/ijerph20237088






