Understanding HPV Vaccination Policymaking in Rwanda: A Case of Health Prioritization and Public-Private-Partnership in a Low-Resource Setting
Abstract
:1. Introduction
2. Methods
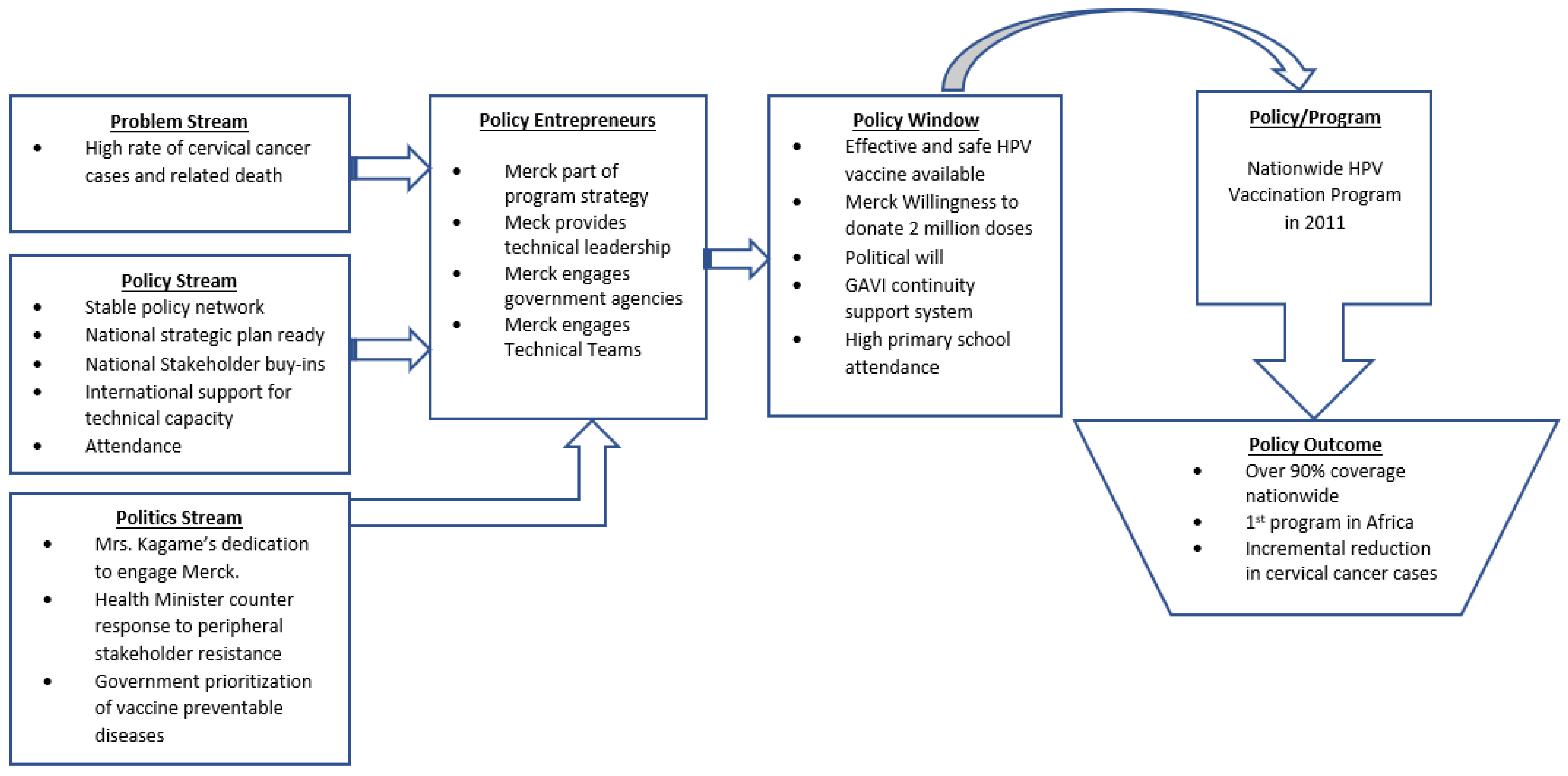
Theoretical Lens
3. Results
3.1. Problem Stream
3.2. Policy Stream
3.3. Politics Stream
3.4. Policy Entrepreneurs
3.5. Policy Window
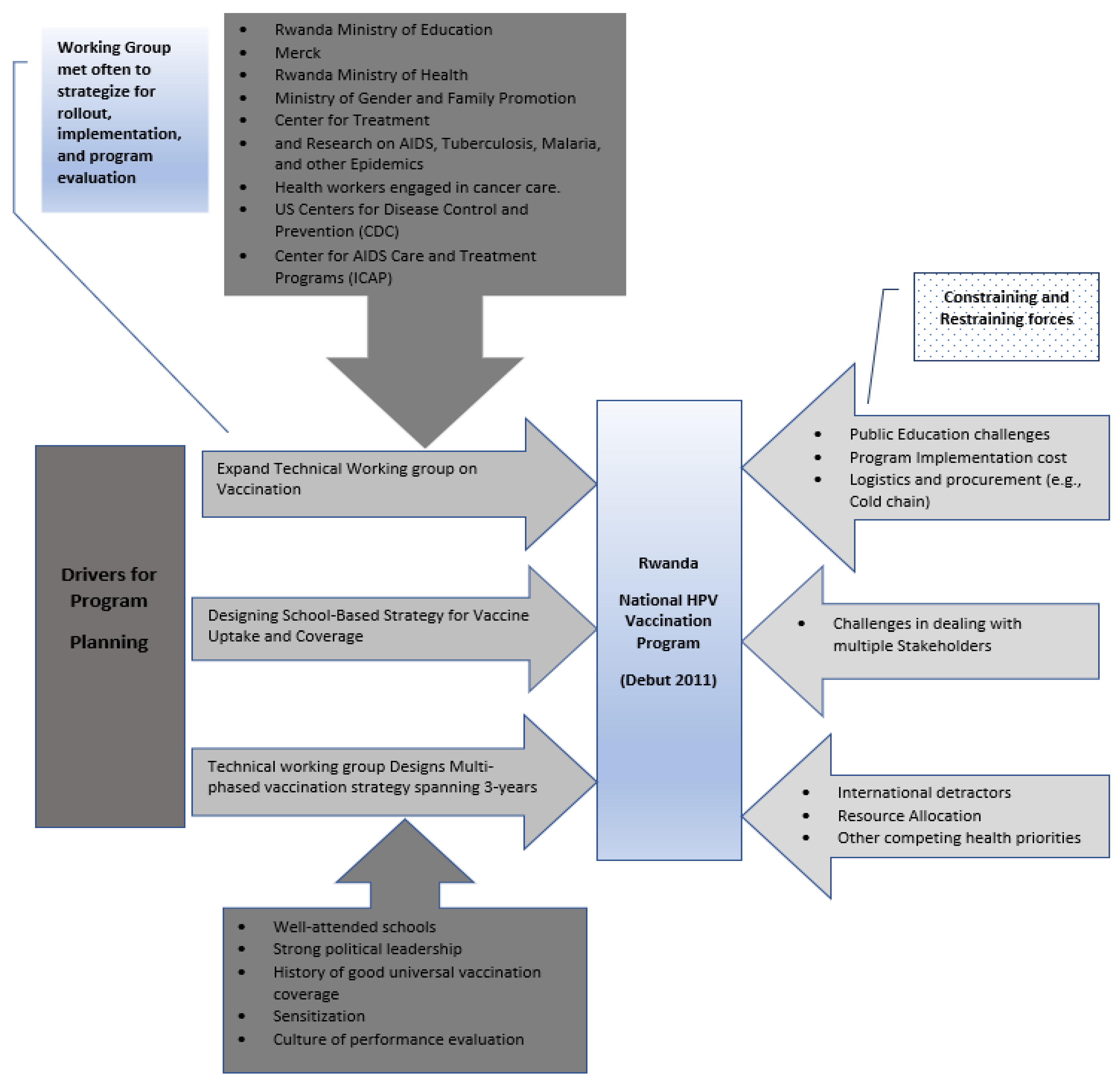
3.6. Policy Network Stability
3.7. Local Policy Accountability Frameworks
4. Discussion
4.1. Planning and Prioritization
4.2. State-Non-State Relationships
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holmes, D. Rwanda: An Injection of Hope. Lancet 2010, 376, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Binagwaho, A.; Farmer, P.E.; Nsanzimana, S.; Karema, C.; Gasana, M.; de Dieu Ngirabega, J.; Ngabo, F.; Wagner, C.M.; Nutt, C.T.; Nyatanyi, T. Rwanda 20 Years on: Investing in Life. Lancet 2014, 384, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Schneider, P.; Diop, F. Community-Based Health Insurance in Rwanda. In Health Financing for Poor People—Resource Mobilization and Risk Sharing; World Bank: Washington, DC, USA, 2004; pp. 251–274. [Google Scholar]
- Shimeles, A. Community Based Health Insurance Schemes in Africa: The Case of Rwanda; University of Gothenburg, Department of Economics: Gothenburg, Sweden, 2010. [Google Scholar]
- Saksena, P.; Antunes, A.F.; Xu, K.; Musango, L.; Carrin, G. Mutual Health Insurance in Rwanda: Evidence on Access to Care and Financial Risk Protection. Health Policy 2011, 99, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Saksena, P.; Antunes, A.F.; Xu, K.; Musango, L.; Carrin, G. Impact of Mutual Health Insurance on Access to Health Care and Financial Risk Protection in Rwanda; World Health Report; WHO: Geneva, Switzerland, 2010.
- Musafili, A.; Essén, B.; Baribwira, C.; Binagwaho, A.; Persson, L.-Å.; Selling, K.E. Trends and Social Differentials in Child Mortality in Rwanda 1990–2010: Results from Three Demographic and Health Surveys. J. Epidemiol. Community Health 2015, 69, 834–840. [Google Scholar] [CrossRef]
- UNICEF. Health Budget Brief: Investing in Children’s Health in Rwanda; UNICEF: Kigali, Rwanda, 2018. [Google Scholar]
- Chemouni, B. The Political Path to Universal Health Coverage: Power, Ideas and Community-Based Health Insurance in Rwanda. World Dev. 2018, 106, 87–98. [Google Scholar] [CrossRef]
- Makaka, A.; Breen, S.; Binagwaho, A. Universal Health Coverage in Rwanda: A Report of Innovations to Increase Enrolment in Community-Based Health Insurance. Lancet 2012, 380, S7. [Google Scholar] [CrossRef]
- Twahirwa, A. Sharing the Burden of Sickness: Mutual Health Insurance in Rwanda. Bull. World Health Organ. 2008, 86, 823. [Google Scholar] [CrossRef]
- Binagwaho, A.; Ngabo, F.; Wagner, C.M.; Mugeni, C.; Gatera, M.; Nutt, C.T.; Nsanzimana, S. Integration of Comprehensive Women’s Health Programmes into Health Systems: Cervical Cancer Prevention, Care and Control in Rwanda. Bull. World Health Organ. 2013, 91, 697–703. [Google Scholar] [CrossRef]
- Cousins, S. How Rwanda Could Be the First Country to Wipe out Cervical Cancer. Mosaic 2019, 13, 7–19. [Google Scholar]
- Binagwaho, A.; Wagner, C.M.; Gatera, M.; Karema, C.; Nutt, C.T.; Ngabo, F. Achieving High Coverage in Rwanda’s National Human Papillomavirus Vaccination Programme. Bull. World Health Organ. 2012, 90, 623–628. [Google Scholar] [CrossRef]
- Binagwaho, A.; Wagner, C.M.; Nutt, C.T. HPV Vaccine in Rwanda: Different Disease, Same Double Standard. Lancet 2011, 378, 1916. [Google Scholar] [CrossRef] [PubMed]
- Kramer, J. Eradicating Cervical Cancer: Lessons Learned from Rwanda and Australia. Int. J. Gynecol. Obstet. 2021, 154, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Sayinzoga, F.; Umulisa, M.C.; Sibomana, H.; Tenet, V.; Baussano, I.; Clifford, G.M. Human Papillomavirus Vaccine Coverage in Rwanda: A Population-Level Analysis by Birth Cohort. Vaccine 2020, 38, 4001–4005. [Google Scholar] [CrossRef] [PubMed]
- Ruzigana, G.; Bazzet-Matabele, L.; Rulisa, S.; Martin, A.N.; Ghebre, R.G. Cervical Cancer Screening at a Tertiary Care Center in Rwanda. Gynecol. Oncol. Rep. 2017, 21, 13–16. [Google Scholar] [CrossRef]
- Africanews. Rwanda Ramps up Screening for Cervical Cancer with New Device. Africanews, 10 March 2023. [Google Scholar]
- Bao, J.; McAlister, H.; Robson, J.; Wang, A.; Koswin, K.; Sayinzoga, F.; Sibomana, H.; Uwizihiwe, J.; de Dieu Hakizimana, J.; Nyamusore, J. Near Universal Childhood Vaccination Rates in Rwanda: How Was This Achieved and Can It Be Duplicated? Lancet Glob. Health 2018, 6, S47. [Google Scholar] [CrossRef]
- Larsson, O.L. The Governmentality of Network Governance: Collaboration as a New Facet of the Liberal Art of Governing. Constellations 2020, 27, 111–126. [Google Scholar] [CrossRef]
- Rimal, R.N.; Real, K. Understanding the Influence of Perceived Norms on Behaviors. Commun. Theory 2003, 13, 184–203. [Google Scholar] [CrossRef]
- Foucault, M. The Foucault Effect: Studies in Governmentality; University of Chicago Press: Chicago, IL, USA, 1991. [Google Scholar]
- Nica, E. Foucault on Managerial Governmentality and Biopolitical Neoliberalism. J. Self-Gov. Manag. Econ. 2017, 5, 80–86. [Google Scholar]
- Foucault, M. The Will to Knowledge: The History of Sexuality; Penguin Books: London, UK, 1976; Volume 1. [Google Scholar]
- Foucault, M. The History of Sexuality: An Introduction; Vintage: New York, NY, USA, 1990. [Google Scholar]
- Herzog, T.J.; Huh, W.K.; Downs, L.S.; Smith, J.S.; Monk, B.J. Initial Lessons Learned in HPV Vaccination. Gynecol. Oncol. 2008, 109, S4–S11. [Google Scholar] [CrossRef]
- Ouedraogo, N.; Müller, O.; Jahn, A.; Gerhardus, A. Human Papillomavirus Vaccination in Africa. Lancet 2011, 378, 315–316. [Google Scholar] [CrossRef]
- Chitale, R. CDC Report Stirs Controversy for Merck’s Gardasil Vaccine; ABC News Medical Unit: New York, NY, USA, 2009. [Google Scholar]
- Colgrove, J.; Abiola, S.; Mello, M.M. HPV Vaccination Mandates—Lawmaking amid Political and Scientific Controversy. N. Engl. J. Med. 2010, 363, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Agorastos, T.; Chatzigeorgiou, K.; Brotherton, J.M.; Garland, S.M. Safety of Human Papillomavirus (HPV) Vaccines: A Review of the International Experience so Far. Vaccine 2009, 27, 7270–7281. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, L.E.; Hariri, S.; Unger, E.R.; Saraiya, M.; Datta, S.D.; Dunne, E.F. Post-Licensure Monitoring of HPV Vaccine in the United States. Vaccine 2010, 28, 4731–4737. [Google Scholar] [CrossRef] [PubMed]
- Wilkin, T.; Lee, J.Y.; Lensing, S.Y.; Stier, E.A.; Goldstone, S.E.; Berry, J.M.; Jay, N.; Aboulafia, D.; Cohn, D.L.; Einstein, M.H. Safety and Immunogenicity of the Quadrivalent Human Papillomavirus Vaccine in HIV-1-Infected Men. J. Infect. Dis. 2010, 202, 1246–1253. [Google Scholar] [CrossRef]
- Gee, J.; Naleway, A.; Shui, I.; Baggs, J.; Yin, R.; Li, R.; Kulldorff, M.; Lewis, E.; Fireman, B.; Daley, M.F. Monitoring the Safety of Quadrivalent Human Papillomavirus Vaccine: Findings from the Vaccine Safety Datalink. Vaccine 2011, 29, 8279–8284. [Google Scholar] [CrossRef]
- Kingdon, J.W.; Stano, E. Agendas, Alternatives, and Public Policies; Little, Brown: Boston, MA, USA, 1984; Volume 45. [Google Scholar]
- Kingdon, J.W. Agendas, Alternatives, and Public Policies, 2nd ed.; HarperCollins Publishers: New York, NY, USA, 1995; Volume 2. [Google Scholar]
- Béland, D.; Howlett, M. The Role and Impact of the Multiple-Streams Approach in Comparative Policy Analysis; Taylor & Francis: Abingdon, UK, 2016. [Google Scholar]
- Gökgür, N. Rwanda’s Ruling Party-Owned Enterprises: Do They Enhance or Impede Development?’; IOB Discussion Papers; Universiteit Antwerpen, Institute of Development Policy (IOB): Antwerpen, Belgium, 2012. [Google Scholar]
- Gready, P. ‘You’Re Either with Us or against Us’: Civil Society and Policy Making in Post-Genocide Rwanda. Afr. Aff. 2010, 109, 637–657. [Google Scholar] [CrossRef]
- Reyntjens, F. Political Governance in Post-Genocide Rwanda; Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Bisoka, A.N.; Geens, H. The Price of Progress: Economic Growth, Authoritarianism, and Human Rights in Rwanda. In The Governance, Security and Development Nexus; Springer: Berlin/Heidelberg, Germany, 2021; pp. 253–271. [Google Scholar]
- Desrosiers, M.-E. “Making Do” with Soft Authoritarianism in Pre-Genocide Rwanda. Comp. Politics 2020, 52, 557–579. [Google Scholar] [CrossRef]
- Hagmann, T.; Reyntjens, F. Aid and Authoritarianism in Africa: Development without Democracy; Zed Books Ltd.: London, UK, 2016. [Google Scholar]
- Habarurema, R.D.V.; Ntakirutimana, M.E. Ubudehe and Diaconia: Theological and Moral Perspectives for Social Solidarity in Rwanda. Globeethics.net Focus 2019, 1, 225–256. [Google Scholar]
- Rutikanga, C. A Social Work Analysis of Home-Grown Solutions and Poverty Reduction in Rwanda: The Traditional Approach of Ubudehe. In Social Work Practice in Africa Indigenous and Innovative Approaches; Fountain Publishers: Kampala, Uganda, 2019; pp. 61–80. ISBN 978-9970-617-92-0. [Google Scholar]
- Ngamije, J. Promising Approach to Addressing 2019 New-Ubudehe Categorization Challenges: Community-Based Participatory Research. SSRN-Elsivier 2020, 1–7. [Google Scholar] [CrossRef]
- Bird, C. Aid and Authoritarianism in Africa. Med. Confl. Surviv. 2017, 33, 85. [Google Scholar] [CrossRef]
- Reese, R. Paul Kagame: Machiavelli’s Prince. Seton Hall J. Dipl. Int’l Rel. 2014, 15, 107. [Google Scholar]
- Agbaenyi, A.N.; Anekwe, S.C. Illiberal Governance And Human Rights Situation In Africa’s Democracies. Int. J. Innov. Res. Adv. Stud. 2019, 6, 76–77. [Google Scholar]
- Hintjens, H.; Asiimwe, H. Post-Liberal Politics in East Africa: The Tickbird and the Rhino. Dev. Issues 2019, 20, 5–8. [Google Scholar]
- Russell, S. The Benevolent Dictatorship in Rwanda: Negative Government, Positive Outcomes? Appl. Anthropol. 2012, 32, 12–22. [Google Scholar]
- Waldorf, L. Apotheosis of a Warlord: Paul Kagame. In Warlord Democrats in Africa: Ex-Military Leaders and Electoral Politics; Zed Books: London, UK, 2017; pp. 68–94. [Google Scholar]
- Sayinzoga, F.; Tenet, V.; Heideman, D.A.; Sibomana, H.; Umulisa, M.-C.; Franceschi, S.; de Dieu Hakizimana, J.; Clifford, G.M.; Baussano, I. Human Papillomavirus Vaccine Effect against Human Papillomavirus Infection in Rwanda: Evidence from Repeated Cross-Sectional Cervical-Cell-Based Surveys. Lancet Glob. Health 2023, 11, e1096–e1104. [Google Scholar] [CrossRef]
- Bruni, L.; Barrionuevo-Rosas, L.; Albero, G.; Serrano, B.; Mena, M.; Gomez, D. Human Papillomavirus and Related Diseases Report; HPV Information Centre: Barcelona, Spain, 2017. [Google Scholar]
- Bangura, M.S.; Zhao, Y.; Gonzalez Mendez, M.J.; Wang, Y.; Didier Sama, S.; Xu, K.; Ren, R.; Ma, L.; Qiao, Y.-L. Case Study of Cervical Cancer Prevention in Two Sub-Saharan African Countries: Rwanda and Sierra Leone. Front. Med. 2022, 9, 928685. [Google Scholar] [CrossRef]
- Abiola, S.E.; Colgrove, J.; Mello, M.M. The Politics of HPV Vaccination Policy Formation in the United States. J. Health Politics Policy Law 2013, 38, 645–681. [Google Scholar] [CrossRef]
- Mello, M.M.; Abiola, S.; Colgrove, J. Pharmaceutical Companies’ Role in State Vaccination Policymaking: The Case of Human Papillomavirus Vaccination. Am. J. Public Health 2012, 102, 893–898. [Google Scholar] [CrossRef]
- Collins, K.L. Profitable Gifts: A History of the Merck Mectizan Donation Program and Its Implications for International Health. Perspect. Biol. Med. 2004, 47, 100–109. [Google Scholar] [CrossRef]
- Perkins, L. Pharmaceutical Companies Must Make Decisions Based on Profit. West. J. Med. 2001, 175, 422. [Google Scholar] [CrossRef]
- Ledley, F.D.; McCoy, S.S.; Vaughan, G.; Cleary, E.G. Profitability of Large Pharmaceutical Companies Compared with Other Large Public Companies. JAMA 2020, 323, 834–843. [Google Scholar] [CrossRef]
- Levin, A.; Wang, S.A.; Levin, C.; Tsu, V.; Hutubessy, R. Costs of Introducing and Delivering HPV Vaccines in Low and Lower Middle Income Countries: Inputs for GAVI Policy on Introduction Grant Support to Countries. PLoS ONE 2014, 9, e101114. [Google Scholar] [CrossRef] [PubMed]
- Hanson, C.M.; Eckert, L.; Bloem, P.; Cernuschi, T. Gavi HPV Programs: Application to Implementation. Vaccines 2015, 3, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Shinkafi-Bagudu, Z. Global Partnerships for HPV Vaccine Must Look Beyond National Income. JCO Glob. Oncol. 2020, 6, 1746–1748. [Google Scholar] [CrossRef] [PubMed]
- Reich, M.R. Public–Private Partnerships for Public Health. Nat. Med. 2000, 6, 617–620. [Google Scholar] [CrossRef]
- Ruckert, A.; Labonté, R. Public–Private Partnerships (PPPs) in Global Health: The Good, the Bad and the Ugly. Third World Q. 2014, 35, 1598–1614. [Google Scholar] [CrossRef]
| Argument a | Counterargument b |
|---|---|
| We have serious doubts that this arrangement Merck providing HPV vaccines to Rwanda] is in the best interest of the people. | Are the 330,000 Rwandan girls who will be vaccinated against a highly prevalent, oncogenic virus for free during the first phase of this programme not regarded as “the people”? |
| Although the burden of cervical cancer in low-income and middle-income countries is substantial (3 · 8 million disability-adjusted life-years [DALYs]), it ranks well behind that of other vaccine-preventable diseases such as tetanus (8 · 3 million DALYs) and measles (23 million DALYs). | For the diseases cited (measles and tetanus), Rwanda has 95% and 96·8% vaccination coverage rates, respectively. |
| The effectiveness of the HPV vaccine against cervical cancer is still unknown. | Many studies say otherwise. |
| To remain cost-effective in GAVI-eligible countries, the costs for a vaccinated individual should not exceed US$10 for the three doses. | The initial price of the pneumococcal vaccine provides a helpful lesson, and Merck announced a two-thirds reduction in the price of Gardasil for GAVI-eligible countries (to US$5 per dose). |
| Representatives of vaccine manufacturers and the Rwandan Minister of Health are on the GAVI Board—an obvious conflict of interest. | Merck representatives are non-voting GAVI observers, and GAVI’s website clearly shows Rwanda’s board membership terminating on 31 December 2011. GAVI will have no role in the HPV vaccine program before 2014. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asempah, E.; Wiktorowicz, M.E. Understanding HPV Vaccination Policymaking in Rwanda: A Case of Health Prioritization and Public-Private-Partnership in a Low-Resource Setting. Int. J. Environ. Res. Public Health 2023, 20, 6998. https://doi.org/10.3390/ijerph20216998
Asempah E, Wiktorowicz ME. Understanding HPV Vaccination Policymaking in Rwanda: A Case of Health Prioritization and Public-Private-Partnership in a Low-Resource Setting. International Journal of Environmental Research and Public Health. 2023; 20(21):6998. https://doi.org/10.3390/ijerph20216998
Chicago/Turabian StyleAsempah, Eric, and Mary E. Wiktorowicz. 2023. "Understanding HPV Vaccination Policymaking in Rwanda: A Case of Health Prioritization and Public-Private-Partnership in a Low-Resource Setting" International Journal of Environmental Research and Public Health 20, no. 21: 6998. https://doi.org/10.3390/ijerph20216998
APA StyleAsempah, E., & Wiktorowicz, M. E. (2023). Understanding HPV Vaccination Policymaking in Rwanda: A Case of Health Prioritization and Public-Private-Partnership in a Low-Resource Setting. International Journal of Environmental Research and Public Health, 20(21), 6998. https://doi.org/10.3390/ijerph20216998






