Impact of the Rise of Artificial Intelligence in Radiology: What Do Students Think?
Abstract
1. Introduction
- To check the general knowledge that students have about AI.
- To assess the importance given by students to academic training in AI.
- To determine the influence of AI on human decision-making and capabilities, as well as the need for the implementation of well-established ethical principles.
- To investigate the role assigned to the use of AI in radiology and its impact on the professional performance of specialists and radiology services.
2. Materials and Methods
- Theoretical: A review of the subject to be investigated was accomplished through different search engines such as: PubMed, Scopus, Dialnet and Google Scholar. Articles from the last 5 years were included, limiting the references to our objectives using the keywords: artificial intelligence; medicine; radiology; students; perception; ethics.
- Empirical: The tool used was an anonymous online questionnaire (Supplementary Materials), carried out through the Google Forms platform to high school and university Medical students in Santiago de Compostela during the 2021–2022 academic year. The distribution of the survey was made through the class delegates in the Faculty of Medicine and through the directors of the institutes. It was open from 3 January to 31 March 2022.
3. Results
3.1. Demographics
- According to age (22.2 ± 3.5), the sample was divided into three age groups from highest to lowest frequency:
- -
- Group 1. Between 21 and 22 years old: With 42.34% (n = 119).
- -
- Group 2. Age equal to or less than 20 years: Represented by 34.16% (n = 96).
- -
- Group 3. Age equal to or greater than 23 years: 23.48% (n = 66) of the students belong to this group.
- The distribution of students in different courses, from highest to lowest participation, showed that 25.62% (n = 72) corresponded to the 6th grade, followed by the 2nd and 5th grades with the same number of students, respectively, 50 (17.80%), 13.52% from 1st year (n = 38), 12.81% (n = 36) correspond to those from 3rd and, finally, those from 4th that represent 12.45% (n = 35) of the sample.
- According to the origin of the respondents, the majority belonged to the University of Santiago de Compostela (USC), making up 97.86% (n = 275). The rest came from the University of Murcia, with 1.06% (n = 3), the University de las Palmas de Gran Canaria (ULPGC), with 0.36% (n = 1), UCS, with 0.36% (n = 1) and the UNED, with another 0.36% (n = 1).
3.2. Ranking Radiology
- When asked about the choice of radiology as a specialty, 75.09% (n = 211) of those surveyed answered that they would NOT choose it, compared with 24.91% (n = 70), that YES, they would choose it. Age was associated with a greater probability when choosing radiology as a specialty p = 0.007 (p < 0.05). These results were independent of gender and the course in which they were (p = 0.31 and p = 0.13, respectively).
- Among the students who wanted to do radiology, 6.74% (n = 6) said that they would choose radiology as the first option, 3.37% (n = 3) as the second option, 30.34% (n = 27) as the third option and 59.55% (n = 53) said they would be indifferent to the order of preference.
- At the end of the questionnaire, we asked them if they would change their choice considering the impact of AI, and we found that 159 (56.58%) would not change their preferences when choosing specialty, regardless of the impact that AI would have on them, while only 27 (9.61%) would and 95 (the remaining 33.81%) said that perhaps they would reconsider their choice.
3.3. Knowledge of AI
3.3.1. Subjective
- They were first asked if they knew what AI was and its uses.
- Regarding the use of AI in our daily lives (voice and face recognition systems, web search engines, cybersecurity, autonomous vehicles, robots, online shopping, advertising…), 81.14% (n = 228) answered YES, 16.72% (n = 47) chose NO as an answer, and the remaining 2.14% (n = 6) chose NS/NA in terms of being aware of the use of AI in daily life.
- As for the source from which they obtained information, MEDIA was the most chosen (250; 88.97%), followed by articles and journals (118; 41.99%), friends/family (104; 37.01%), teachers/center (101; 35.94%), radiologists (29; 10.32%) and other specialists (21; 7.47%).
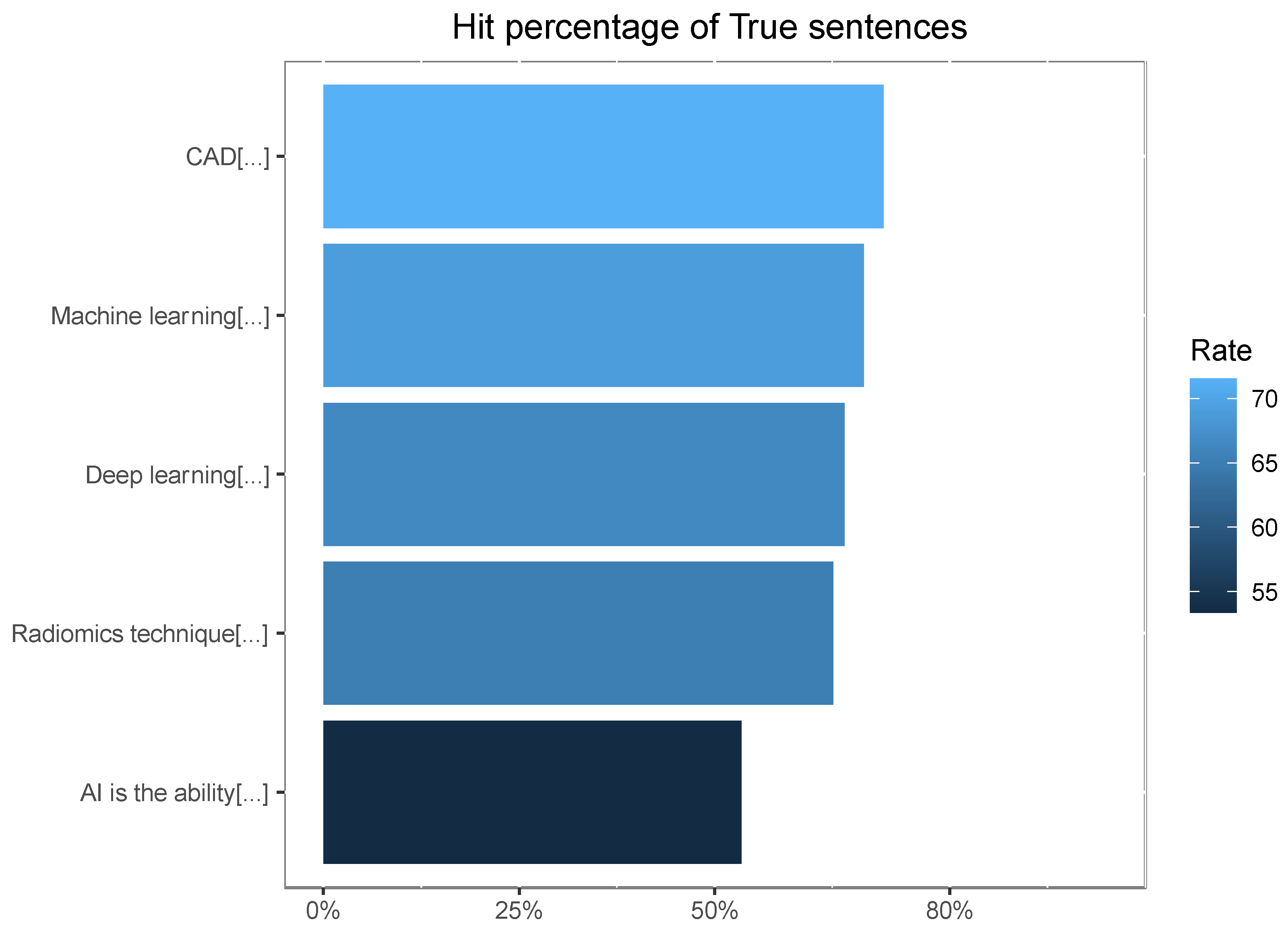
3.3.2. Objective
3.4. General Perception of the Impact of AI
- A total of 56.23% (n = 158) stated that AI improved human capabilities. Meanwhile, 38.08% (n = 107) stated that it increased them and only 5.69% (n = 16) answered that it did not influence these capacities.
- When asked whether AI could affect human autonomy by interfering with decision-making, 46.99% (n = 132) agreed and 8.13% (n = 23) strongly agreed.
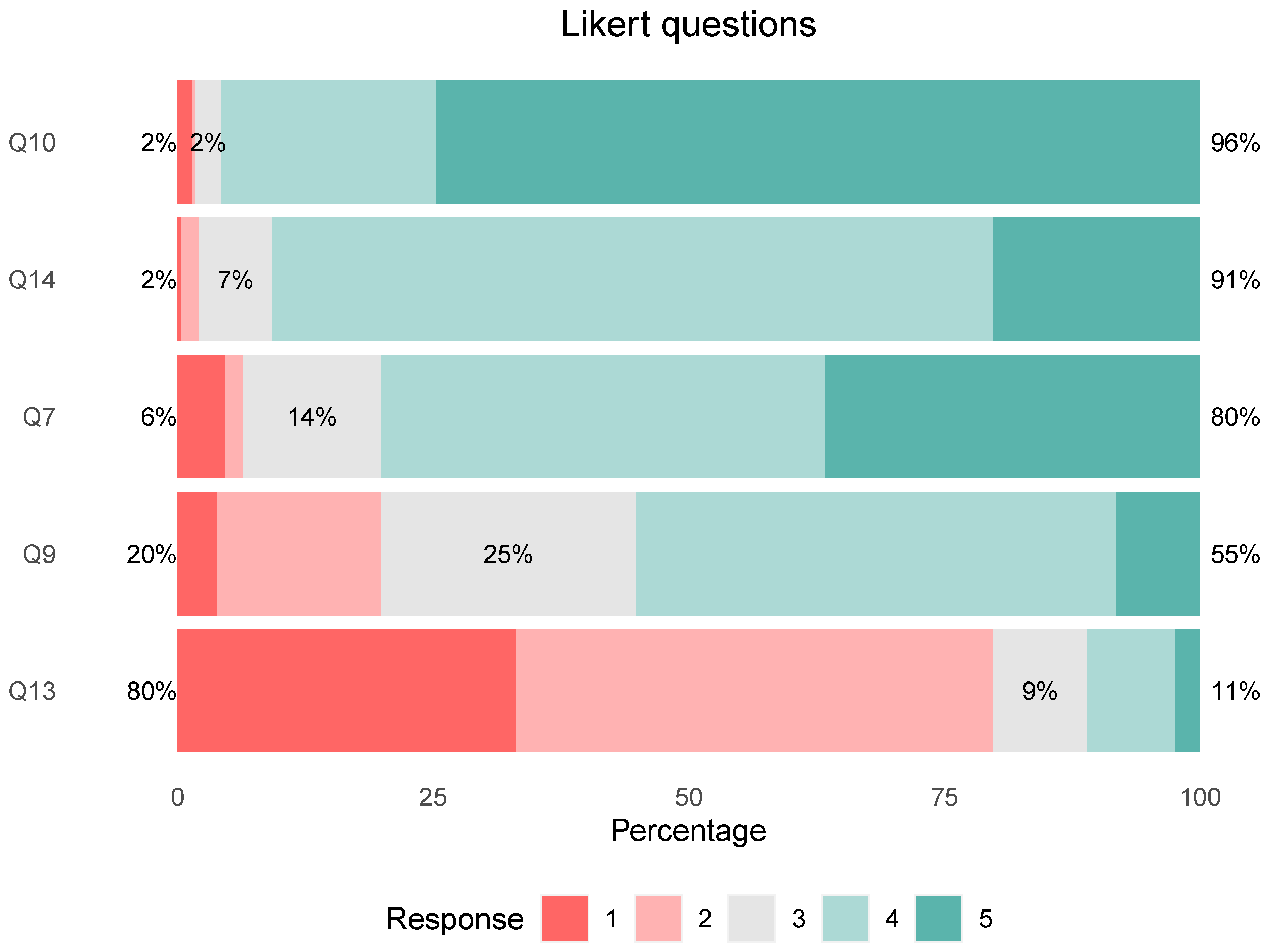
3.5. Perception of the Impact of AI in Radiology
- 91% of respondents said AI will change the way radiologists work [Agree, 70.46% (n = 198) and Strongly Agree, 20.28% (n = 57)]. Figure 2.
- Most of the respondents, 90.39% (n = 254), assigned a support role to the use of AI in radiology, followed by 8.90% (n = 25), who opted for preponderant and only 0.71% (n = 2) were against its use.
- 99.64% (n = 280) agreed that the main role of radiologists should be “Lead the algorithm validation process, contribute their experience in the global clinical approach of patients, and make the final decision”.
- In question 13 we explored the fear of replacement.
- Finally, we investigated what aspects of the radiology service would improve with AI.
- It favors early diagnosis and treatment of diseases: 244 (86.83%).
- It improves the management and quality of radiology services: 193 (68.68%).
- It allows radiologists to focus on patient care in a general clinical context by making their work easier: 137 (48.75%).
- It reduces the number and qualification of the professionals needed in the service: 27 (9.61%).
3.6. Ethics
3.7. Teaching
3.8. Drawbacks of Using AI in Medicine
4. Discussion
5. Conclusions
- Applications of AI in medicine, and especially in radiology, are positively valued by the vast majority, considering it a useful tool.
- A high percentage of students have an acceptable knowledge of what AI is and its applications in daily life, however it could be improved. MEDIA was the main source of information.
- Most of the students consider their academic training in this discipline of vital importance for the future.
- They also agree on the need to implement well-established ethical principles in the field of AI.
- Most of them agree that the impact of AI in the specialty will not replace radiologists, but their work will undergo modifications.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- González, A.H. The Value of Data and Its Applicability in the Health Sector. Rev. Esp. Med. Nucl. Imagen Mol. (Engl. Ed.) 2022, 41, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Neri, E.; de Souza, N.; Brady, A.; Bayarri, A.A.; Becker, C.D.; Coppola, F.; Visser, J. What the Radiologist Should Know about Artificial Intelligence—An ESR White Paper. Insights Imaging 2019, 10, 44. [Google Scholar] [CrossRef]
- Ahmad, Z.; Rahim, S.; Zubair, M.; Abdul-Ghafar, J. Artificial Intelligence (AI) in Medicine, Current Applications and Future Role with Special Emphasis on Its Potential and Promise in Pathology: Present and Future Impact, Obstacles Including Costs and Acceptance among Pathologists, Practical and Philosoph. Diagn. Pathol. 2021, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Noguerol, T.M.; Paulano-Godino, F.; Martín-Valdivia, M.T.; Menias, C.O.; Luna, A. Strengths, Weaknesses, Opportunities, and Threats Analysis of Artificial Intelligence and Machine Learning Applications in Radiology. J. Am. Coll. Radiol. 2019, 16, 1239–1247. [Google Scholar] [CrossRef]
- Langs, G.; Röhrich, S.; Hofmanninger, J.; Prayer, F.; Pan, J.; Herold, C.; Prosch, H. Machine Learning: From Radiomics to Discovery and Routine the Emergence of Machine Learning in Radiology. Radiologe 2018, 58, 1–6. [Google Scholar] [CrossRef]
- Casas, J.A.V.; Rodríguez-Caceres, E. Artificial Intelligence and Nuclear Medicine. Today Is Already the Future. Rev. Esp. Med. Nucl. Imagen Mol. (Engl. Ed.) 2022, 41, 1–2. [Google Scholar] [CrossRef]
- Chong, L.R.; Tzan, K.; Lee, T.; Seck, L.L.; Foo, G.; Chim, P.; Lr, C.C.; Kt, T.; Ll, L.; Sg, F.; et al. Artificial Intelligence Predictive Analytics in the Management of Outpatient MRI Appointment No-Shows. AJR Am. J. Roentgenol. 2020, 215, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- McCollough, C.H.; Leng, S. Use of Artificial Intelligence in Computed Tomography Dose Optimisation. Ann. ICRP 2020, 49, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.W.; Lee, S.; Kwon, S.; Nam, W.; Cha, I.H.; Kim, H.J. Deep Learning-Based Survival Prediction of Oral Cancer Patients. Sci. Rep. 2019, 9, 6994. [Google Scholar] [CrossRef]
- Higaki, T.; Nakamura, Y.; Tatsugami, F.; Nakaura, T.; Awai, K. Improvement of Image Quality at CT and MRI Using Deep Learning. Jpn. J. Radiol. 2019, 37, 73–80. [Google Scholar] [CrossRef]
- Avila-Tomás, J.F.; Mayer-Pujadas, M.A.; Quesada-Varela, V.J. La Inteligencia Artificial y Sus Aplicaciones En Medicina I: Introducción Antecedentes a La IA y Robótica. Atención Primaria 2020, 52, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Ozsahin, I.; Sekeroglu, B.; Musa, M.S.; Mustapha, M.T.; Ozsahin, D.U. Review on Diagnosis of COVID-19 from Chest CT Images Using Artificial Intelligence. Comput. Math. Methods Med. 2020, 2020, 9756518. [Google Scholar] [CrossRef] [PubMed]
- Alsharif, M.H.; Alsharif, Y.H.; Yahya, K.; Alomari, O.A.; Albreem, M.A.; Jahid, A. Deep Learning Applications to Combat the Dissemination of COVID-19 Disease: A Review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 11455–11460. [Google Scholar] [CrossRef] [PubMed]
- Nasrullah, N.; Sang, J.; Alam, M.S.; Mateen, M.; Cai, B.; Hu, H. Automated Lung Nodule Detection and Classification Using Deep Learning Combined with Multiple Strategies. Sensors 2019, 19, 3722. [Google Scholar] [CrossRef] [PubMed]
- Chieregato, M.; Frangiamore, F.; Morassi, M.; Baresi, C.; Nici, S.; Bassetti, C.; Bnà, C.; Galelli, M. A Hybrid Machine Learning/Deep Learning COVID-19 Severity Predictive Model from CT Images and Clinical Data. Sci. Rep. 2022, 12, 4329. [Google Scholar] [CrossRef]
- Abdollahi, H.; Mofid, B.; Shiri, I.; Razzaghdoust, A.; Saadipoor, A.; Mahdavi, A.; Galandooz, H.M.; Mahdavi, S.R. Machine Learning-Based Radiomic Models to Predict Intensity-Modulated Radiation Therapy Response, Gleason Score and Stage in Prostate Cancer. Radiol. Med. 2019, 124, 555–567. [Google Scholar] [CrossRef]
- Neri, E.; Del Re, M.; Paiar, F.; Erba, P.; Cocuzza, P.; Regge, D.; Danesi, R. Radiomics and Liquid Biopsy in Oncology: The Holons of Systems Medicine. Insights Imaging 2018, 9, 915–924. [Google Scholar] [CrossRef]
- Mazurowski, M.A. Artificial Intelligence May Cause a Significant Disruption to the Radiology Workforce. J. Am. Coll. Radiol. 2019, 16, 1077–1082. [Google Scholar] [CrossRef]
- Tajmir, S.H.; Alkasab, T.K. Toward Augmented Radiologists: Changes in Radiology Education in the Era of Machine Learning and Artificial Intelligence. Acad. Radiol. 2018, 25, 747–750. [Google Scholar] [CrossRef]
- Liew, C. The Future of Radiology Augmented with Artificial Intelligence: A Strategy for Success. Eur. J. Radiol. 2018, 102, 152–156. [Google Scholar] [CrossRef]
- Martín-Noguerol, T.; Paulano-Godino, F.; López-Ortega, R.; Górriz, J.M.; Riascos, R.F.; Luna, A. Artificial Intelligence in Radiology: Relevance of Collaborative Work between Radiologists and Engineers for Building a Multidisciplinary Team. Clin. Radiol. 2021, 76, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.K.; Shetty, A.S. Artificial Intelligence and Machine Learning: Opportunities for Radiologists in Training. J. Am. Coll. Radiol. 2018, 15, 1320–1321. [Google Scholar] [CrossRef] [PubMed]
- Gorospe-Sarasúa, L.; Muñoz-Olmedo, J.M.; Sendra-Portero, F.; de Luis-García, R. Challenges of Radiology Education in the Era of Artificial Intelligence. Radiología (Engl. Ed.) 2022, 64, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Schuur, F.; Mehrizi, M.H.R.; Ranschaert, E. Training Opportunities of Artificial Intelligence (AI) in Radiology: A Systematic Review. Eur. Radiol. 2021, 31, 6021–6029. [Google Scholar] [CrossRef] [PubMed]
- Collado-Mesa, F.; Alvarez, E.; Arheart, K. The Role of Artificial Intelligence in Diagnostic Radiology: A Survey at a Single Radiology Residency Training Program. J. Am. Coll. Radiol. 2018, 15, 1753–1757. [Google Scholar] [CrossRef]
- Rainey, C.; O’Regan, T.; Matthew, J.; Skelton, E.; Woznitza, N.; Chu, K.-Y.; Goodman, S.; McConnell, J.; Hughes, C.; Bond, R.; et al. Beauty Is in the AI of the Beholder: Are We Ready for the Clinical Integration of Artificial Intelligence in Radiography? An Exploratory Analysis of Perceived AI Knowledge, Skills, Confidence, and Education Perspectives of UK Radiographers. Front. Digit. Health 2021, 3, 166. [Google Scholar] [CrossRef]
- Caparrós Galán, G.; Sendra Portero, F. Percepciones de Estudiantes de Medicina Sobre El Impacto de La Inteligencia Artificial En Radiología. Radiologia 2021, 64, 516–524. [Google Scholar] [CrossRef]
- Sit, C.; Srinivasan, R.; Amlani, A.; Muthuswamy, K.; Azam, A.; Monzon, L.; Poon, D.S. Attitudes and Perceptions of UK Medical Students towards Artificial Intelligence and Radiology: A Multicentre Survey. Insights Imaging 2020, 11, 14. [Google Scholar] [CrossRef]
- Gong, B.; Nugent, J.P.; Guest, W.; Parker, W.; Chang, P.J.; Khosa, F.; Nicolaou, S. Influence of Artificial Intelligence on Canadian Medical Students’ Preference for Radiology Specialty: ANational Survey Study. Acad. Radiol. 2019, 26, 566–577. [Google Scholar] [CrossRef]
- Bin Dahmash, A.; Alabdulkareem, M.; Alfutais, A.; Kamel, A.M.; Alkholaiwi, F.; Alshehri, S.; Al Zahrani, Y.; Almoaiqel, M. Artificial Intelligence in Radiology: Does It Impact Medical Students Preference for Radiology as Their Future Career? BJR Open 2020, 2, 20200037. [Google Scholar] [CrossRef]
- Pinto dos Santos, D.; Giese, D.; Brodehl, S.; Chon, S.H.; Staab, W.; Kleinert, R.; Maintz, D.; Baeßler, B. Medical Students’ Attitude towards Artificial Intelligence: A Multicentre Survey. Eur. Radiol. 2019, 29, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- Park, C.J.; Yi, P.H.; Siegel, E.L. Medical Student Perspectives on the Impact of Artificial Intelligence on the Practice of Medicine. Curr. Probl. Diagn. Radiol. 2021, 50, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Gillissen, A.; Kochanek, T.; Zupanic, M.; Ehlers, J. Medical Students’ Perceptions towards Digitization and Artificial Intelligence: A Mixed-Methods Study. Healthcare 2022, 10, 723. [Google Scholar] [CrossRef] [PubMed]
- Brandes, G.I.G.; D’ippolito, G.; Azzolini, A.G.; Meirelles, G. Impact of Artificial Intelligence on the Choice of Radiology as a Specialty by Medical Students from the City of São Paulo. Radiol. Bras. 2020, 53, 167–170. [Google Scholar] [CrossRef]
| Demographics | N = 281 | |
|---|---|---|
| Sex | ||
| Men | 81 (29%) | |
| Women | 200 (71%) | |
| Grade | ||
| 1 | 38 (14%) | |
| 2 | 50 (18%) | |
| 3 | 36 (13%) | |
| 4 | 35 (12%) | |
| 5 | 50 (18%) | |
| 6 | 72 (26%) | |
| Age | 22.2 (3.5) 1 |
| Objective Knowledge Based on TRUE/FALSE Statements | N = 281 | % | |
|---|---|---|---|
| Radiomics emerged from the fields of radiology and oncology and its application is exclusive to them. A(answer)/False. | 261 | 93 | |
| The use of deep learning in radiology does not require large databases of medical images for good pattern recognition. A/False. | 261 | 93 | |
| CAD (computer-aided diagnosis): these are computer-aided diagnosis tools developed to detect, to segment and to classify lesions or complex patterns in radiological images. A/True. | 201 | 72 | |
| Machine learning (automatic learning) allows machines, through algorithms and mathematical models, to learn without being expressly programmed for it. R/True. | 194 | 69 | |
| Deep learning: techniques based on artificial neural networks that process data and are capable of automatically recognizing patterns in biomedical images.A/True. | 187 | 67 | |
| Radiomics: technique that consists of obtaining quantifiable information from medical images such as magnetic resonance, computed tomography or PET.They are important in detecting, evaluating and monitoring diseases. A/True. | 183 | 65 | |
| AI is the ability of advanced computer systems to perform the same tasks as human beings (capabilities such as: reasoning, learning, creating and planning). A/True. | 150 | 53 | |
| Subjective knowledge: Do you know what artificial intelligence (AI) is and its applications? (Q3) | Men, N = 81 | Women, N = 200 | p-value |
| No | 6 (7.4%) | 23 (12%) | 0.009 |
| I don’t know | 2 (2.5%) | 27 (14%) | |
| Yes | 73 (90%) | 150 (75%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barreiro-Ares, A.; Morales-Santiago, A.; Sendra-Portero, F.; Souto-Bayarri, M. Impact of the Rise of Artificial Intelligence in Radiology: What Do Students Think? Int. J. Environ. Res. Public Health 2023, 20, 1589. https://doi.org/10.3390/ijerph20021589
Barreiro-Ares A, Morales-Santiago A, Sendra-Portero F, Souto-Bayarri M. Impact of the Rise of Artificial Intelligence in Radiology: What Do Students Think? International Journal of Environmental Research and Public Health. 2023; 20(2):1589. https://doi.org/10.3390/ijerph20021589
Chicago/Turabian StyleBarreiro-Ares, Andrés, Annia Morales-Santiago, Francisco Sendra-Portero, and Miguel Souto-Bayarri. 2023. "Impact of the Rise of Artificial Intelligence in Radiology: What Do Students Think?" International Journal of Environmental Research and Public Health 20, no. 2: 1589. https://doi.org/10.3390/ijerph20021589
APA StyleBarreiro-Ares, A., Morales-Santiago, A., Sendra-Portero, F., & Souto-Bayarri, M. (2023). Impact of the Rise of Artificial Intelligence in Radiology: What Do Students Think? International Journal of Environmental Research and Public Health, 20(2), 1589. https://doi.org/10.3390/ijerph20021589







