Should I Stay or Should I Go? A Qualitative Exploration of Stigma and Other Factors Influencing Opioid Agonist Treatment Journeys
Abstract
Highlights
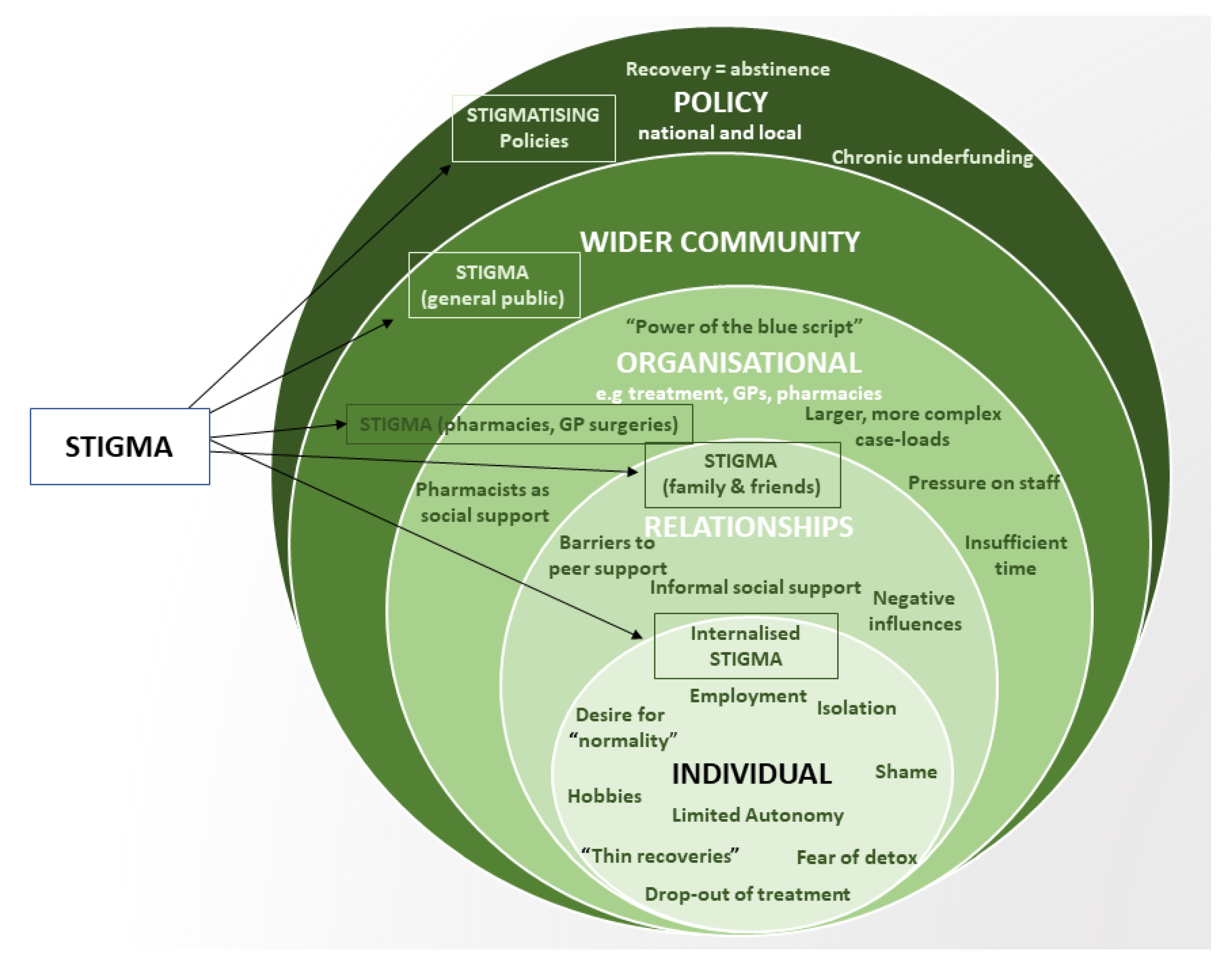
- OAT treatment journeys in our sample were influenced by a broad range of individual, social and structural factors, with stigma presenting a pervasive barrier to treatment retention and recovery.
- Pharmacies were a particularly strong source of enacted and anticipated stigma.
- Recovery from opioid dependency is more than simply abstinence—it is a complex, self-defined and circuitous process.
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Setting
2.2. Sampling and Recruitment
2.3. Data Analysis
3. Results
3.1. The System Is Broken
I think another barrier [to recovery] is time…often I don’t have time to build those working relationships with people within the capacity of our sessions, or a day, or a surgery, or a timetable. (Russel, SP).
I’ve got to get this person drug free, how am I going to get them drug free? You’re not, that’s not going to happen with half an hour, once a fortnight (Gabor, SP).
The pressure…Give us time to do our jobs! (Eric, SP).
When they stop using opioids, hey it’s a successful completion. Are they? Or are they now just angry young men in an old man’s body who we are not supporting to actually grow emotionally and grow as people…do they just get left by the wayside because they’re no longer opioid users? […] what have we left them with? And we wonder why people relapse (Brené, SP).
… it varies across the city and it depends on how responsive the GPs are willing to be in that scenario, so if somebody’s missed three days [picking up medications] and they approach the surgeries directly on day 4, some GPs are really proactive, others will say, ‘No, you need to talk to [treatment organisation], we don’t want anything to do with that’ (Ronnie, SP).
Re-Framing Recovery
3.2. Power Struggles
3.2.1. Autonomy
[…] it’s always a fear in the back of your head [losing access to OAT] so yeah you feel like it’s a big job to hold a script…it’s quite controversial I suppose isn’t it to say it….it’s not like give it to them for 10 years…it could be every three months or six months to have a chat…(Anne-Marie, SU).
… I was just chasing it [recovery] and then it felt like it was other people’s plan […] so it was like you were sort of more steered by other people rather than it being ‘right, I want to do this and then I want to do that and do that’ (Keith, SU).
3.2.2. Stigma
My Dad made a comment [to participant] about some druggies getting their medication before he got his or something […] (Ringo, SU)
It might mean that the stigma [they] receive as [they] walk into a GP’s surgery—often even the people behind reception, [they] could have been at school with, or they’re a family friend or something (Stephen, SP)
When you’ve got treatment systems that are authoritarian and judgemental and massive […] Part of this is increasingly driven by the whole recovery definition so recovery is about not using drug and alcohol so by definition if you are using drugs and alcohol you’re not a success so I think that helps drive that [stigma] (Brené, SP).
… they’ve got the queue there for people with normal prescriptions and then they’ve got you on the side so you’re like palmed off to the side yeah and they will serve every person in that queue before they’d even come to you man. (Ringo, SU).
It’s difficult and it does make you feel less than and not worthy and you know, you’re already beating yourself up because you’re in the situation you’re in so you don’t need someone looking down on you […] (Keith, SU).
3.3. Filling the Void
3.3.1. A Sense of Purpose: Filling the Time Void
I had a client who worked for a window-fitting company, he was a lovely bloke, kept his job and everything, but it was impossible to get him off the script…because then you get to the point where the job then becomes a barrier to reducing, ‘If I reduce I’ll be in withdrawal, and I can’t be in withdrawal whilst I’m at work’. (Gabor, SP).
They [pharmacy] discourage you from going before half past eight even though they open at eight which, if you had a job or something, is like [laugh] and they are open late but you aren’t allowed to go late (Peter, SU).
3.3.2. Connecting with Others: Filling the Social Void
…it has been really hard. It’s a bit depressing but it’s the only way I can find [blocking friends’ phone numbers] […] I’ve got a car so maybe they need a lift, […] they can tug on my heart strings and then I give them a lift and then it turns out that they’re scoring and not getting their meds [Peter, SU].
…I’ve got this friend who’s in the flat below […] he’s been clean seventeen years, so he’s a good person to have around me, you know. Yeah, because he used to see me and say ‘no, I don’t want to know you today mate’, I’d say ‘why’s that?’, he’d say ‘you’re pinned mate, you’ve been using’ Yeah, made me feel bad as well! (Hugh, SU).
4. Discussion
4.1. Implications for Policy and Practice
4.2. Implications for Intervention Development
4.3. Strengths and Limitations
4.4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. WHO Policy Perspectives on Medicines-The Selection of Essential Medicines; WHO: Geneva, Switzerland, 2002.
- UK Department of Health. Drug Misuse and Dependence: UK Guidelines on Clinical Management. 2017. Available online: www.gov.uk/dh (accessed on 1 November 2022).
- National Treatment Agency. National Treatment Agency National Treatment Agency Independent Expert Working Group. In Clinical Guidelines on Drug Misuse and Dependence Update: Consultation Draft June 2007; National Treatment Agency: London, UK, 2007. [Google Scholar]
- Mattick, R.P.; Breen, C.; Kimber, J.; Davoli, M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev 2009, 3, CD002209. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Part 1: Introducing Opioid Substitution Treatment (OST). London. 2021. Available online: https://www.gov.uk/government/publications/opioid-substitution-treatment-guide-for-keyworkers/part-1-introducing-opioid-substitution-treatment-ost (accessed on 1 November 2022).
- Ferraro, C.F.; Stewart, D.E.; Grebely, J.; Tran, L.T.; Zhou, S.; Puca, C.; Hajarizadeh, B.; Larney, S.; Santo Jr, T.; Higgins, J.P.; et al. Association between opioid agonist therapy use and HIV testing uptake among people who have recently injected drugs: A systematic review and meta-analysis. Addiction 2020, 166, 1664–1676. [Google Scholar] [CrossRef] [PubMed]
- Gowing, L.R.; Hickman, M.; Degenhardt, L. Mitigating the risk of HIV infection with opioid substitution treatment. Bull. World Health Organ. 2013, 91, 148–149. [Google Scholar] [CrossRef] [PubMed]
- MacArthur, G.J.; Minozzi, S.; Martin, N.; Vickerman, P.; Deren, S.; Bruneau, J.; Degenhardt, L.; Hickman, M. Opiate substitution treatment and HIV transmission in people who inject drugs: Systematic review and meta-analysis. Bmj 2012, 345, e5945. [Google Scholar] [CrossRef]
- Platt, L.; Minozzi, S.; Reed, J.; Vickerman, P.; Hagan, H.; French, C.; Jordan, A.; Degenhardt, L.; Hope, V.; Hutchinson, S.; et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst. Rev. 2017, 9, CD012021. [Google Scholar] [CrossRef]
- Sordo, L.; Barrio, G.; Bravo, M.J.; Indave, B.I.; Degenhardt, L.; Wiessing, L.; Ferri, M.; Pastor-Barriuso, R. Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ 2017, 357, j1550. [Google Scholar] [CrossRef]
- Colledge-Frisby, S.; Jones, N.; Larney, S.; Peacock, A.; Lewer, D.; Brothers, T.D.; Hickman, M.; Farrell, M.; Degenhardt, L. The impact of opioid agonist treatment on hospitalisations for injecting-related diseases among an opioid dependent population: A retrospective data linkage study. Drug Alcohol Depend. 2022, 236, 109494. [Google Scholar] [CrossRef]
- O’Connor, A.M.; Cousins, G.; Durand, L.; Barry, J.; Boland, F. Retention of patients in opioid substitution treatment: A systematic review. PLoS ONE 2020, 15, e0232086. [Google Scholar] [CrossRef]
- NDTMS. Substance Misuse Treatment for Adults: Statistics 2020 to 2021. GOV.UK. 2021. Available online: https://www.gov.uk/government/statistics/substance-misuse-treatment-for-adults-statistics-2020-to-2021 (accessed on 11 October 2022).
- Carlisle, V. “Holding on by the Seat of Their Pants” A Mixed Methods Exploration of Retention, Completion and Recovery in Opioid Substitution Treatment. University of Bristol. 2021. Available online: https://research-information.bris.ac.uk/en/studentTheses/holding-on-by-the-seat-of-their-pants-a-mixed-methods-exploration (accessed on 10 October 2022).
- Bell, J.; Burrell, T.; Indig, D.; Gilmour, S. Cycling in and out of treatment; participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend. 2006, 81, 55–61. [Google Scholar] [CrossRef]
- Santo, T.; Clark, B.; Hickman, M.; Grebely, J.; Campbell, G.; Sordo, L.; Chen, A.; Tran, L.T.; Bharat, C.; Padmanathan, P.; et al. Association of opioid agonist treatment with all-cause mortality and specific causes of death among people with opioid dependence: A systematic review and meta-analysis. JAMA Psychiatry 2021, 78, 979–993. [Google Scholar] [CrossRef]
- HM Government. 2017 Drug Strategy. 2017. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/628148/Drug_strategy_2017.PDF (accessed on 24 October 2022).
- Ford, C.; Nutt, D.; Eastwood, N.; Gold, D.; Jolly, J.; Murphy, F.; Halliday, K.; Bridge, J. Is the UK’s 2017 drug strategy fit for purpose? BMJ 2017, 358, j4405. [Google Scholar] [CrossRef] [PubMed]
- Neale, J.; Nettleton, S.; Pickering, L. Does recovery-oriented treatment prompt heroin users prematurely into detoxification and abstinence programmes? Qualitative study. Drug Alcohol Depend. 2013, 127, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Duke, K.; Thom, B. The role of evidence and the expert in contemporary processes of governance: The case of opioid substitution treatment policy in England. Int. J. Drug Policy 2014, 25, 964–971. [Google Scholar] [CrossRef]
- Kalk, N.J.; Robertson, J.R.; Kidd, B.; Day, E.; Kelleher, M.J.; Gilvarry, E.; Strang, J. Treatment and intervention for opiate dependence in the United Kingdom: Lessons from triumph and failure. Eur. J. Crim. Policy Res. 2018, 24, 183–200. [Google Scholar] [CrossRef]
- Day, E. Recovery Orientated Systems of Care. Has Their Time Finally Come? 2020. In Proceedings of the NHS APA 2020 Virtual Conference, 9 September 2020; Available online: https://www.nhsapa.org/post/session-1-2020conf (accessed on 19 March 2021).
- Lancaster, K. Rethinking recovery. Addiction 2017, 112, 758–759. [Google Scholar] [CrossRef] [PubMed]
- Neale, J.; Finch, E.; Marsden, J.; Mitcheson, L.; Rose, D.; Strang, J.; Tompkins, C.; Wheeler, C.; Wykes, T. How should we measure addiction recovery? Analysis of service provider perspectives using online Delphi groups. Drugs Educ. Prev. Policy 2014, 21, 310–323. [Google Scholar] [CrossRef]
- Neale, J.; Tompkins, C.; Wheeler, C.; Finch, E.; Marsden, J.; Mitcheson, L.; Rose, D.; Wykes, T.; Strang, J. “You’re all going to hate the word ‘recovery’ by the end of this”: Service users’ views of measuring addiction recovery. Drugs Educ. Prev. Policy 2015, 22, 26–34. [Google Scholar] [CrossRef]
- Anstice, S.; Strike, C.J.; Brands, B. Supervised methadone consumption: Client issues and stigma. Subst. Use Misuse 2009, 44, 794–808. [Google Scholar] [CrossRef]
- Gourlay, J.; Ricciardelli, L.; Ridge, D. Users’ Experiences of Heroin and Methadone Treatment. Subst. Use Misuse 2005, 40, 1875–1882. [Google Scholar] [CrossRef]
- Harris, J.; McElrath, K. Methadone as social control: Institutionalized stigma and the prospect of recovery. Qual. Health Res. 2012, 22, 810–824. [Google Scholar] [CrossRef]
- McPhee, I.; Brown, A.; Martin, C. Stigma and perceptions of recovery in Scotland: A qualitative study of injecting drug users attending methadone treatment. Drugs Alcohol Today 2013, 13, 244–257. [Google Scholar] [CrossRef]
- Treloar, C.; Lancaster, K.; Gendera, S.; Rhodes, T.; Shahbazi, J.; Byrne, M.; Degenhardt, L.; Farrell, M. Can a new formulation of opiate agonist treatment alter stigma?: Place, time and things in the experience of extended-release buprenorphine depot. Int. J. Drug Policy 2022, 107, 103788. [Google Scholar] [PubMed]
- Woo, J.; Bhalerao, A.; Bawor, M.; Bhatt, M.; Dennis, B.; Mouravska, N.; Zielinski, L.; Samaan, Z. “Don’t Judge a Book by Its Cover”: A Qualitative Study of Methadone Patients’ Experiences of Stigma. Subst. Abuse Res. Treat. 2017, 11, 117822181668508. [Google Scholar] [CrossRef] [PubMed]
- Goffman, E. Stigma: Notes on The Management of Spoiled Identity; Simon and Shuster: New York, NY, USA, 1963. [Google Scholar]
- Link, B.G.; Phelan, J.C. Conceptualizing Stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Earnshaw, V.A.; Chaudoir, S.R. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav. 2009, 13, 1160–1177. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Mittal, M.L.; Wagner, K.; Copenhaver, M.M.; Cunningham, C.O.; Earnshaw, V.A. Factor structure, internal reliability and construct validity of the Methadone Maintenance Treatment Stigma Mechanisms Scale (MMT-SMS). Addiction 2020, 115, 354–367. [Google Scholar] [CrossRef]
- Cordella, B.; Greco, F.; Elia, P.; Varazi, M. Lifelong maintenance treatment or “positive” dropout? J. Subst. Use 2017, 22, 372–376. [Google Scholar] [CrossRef]
- Smith, M.L.; Rosen, D. Mistrust and self-isolation: Barriers to social support for older adult methadone clients. J. Gerontol. Soc. Work 2009, 52, 653–667. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Carlisle, V.; Maynard, O.; Padmanathan, P.; Hickman, M.; Thomas, K.; Kesten, J. Factors influencing recovery in opioid substitution treatment: A systematic review and thematic synthesis. arXiv 2020. [Google Scholar] [CrossRef]
- Cowan, E.; Khan, M.R.; Shastry, S.; Edelman, E.J. Conceptualizing the effects of the COVID-19 pandemic on people with opioid use disorder: An application of the social ecological model. Addict. Sci. Clin. Pract. 2021, 16, 4. [Google Scholar] [CrossRef]
- Jalali, M.S.; Botticelli, M.; Hwang, R.C.; Koh, H.K.; McHugh, R.K. The opioid crisis: A contextual, social-ecological framework. Health Res. Policy Syst. 2020, 18, 87. [Google Scholar] [CrossRef]
- Komalasari, R.; Wilson, S.; Haw, S. A social ecological model (SEM) to exploring barriers of and facilitators to the implementation of opioid agonist treatment (OAT) programmes in prisons. Int. J. Prison. Health 2021, 17, 477–496. [Google Scholar] [CrossRef]
- Mair, C.; Sumetsky, N.; Burke, J.G.; Gaidus, A. Investigating the Social Ecological Contexts of Opioid Use Disorder and Poisoning Hospitalizations in Pennsylvania. J. Stud. Alcohol Drugs 2018, 79, 899–908. [Google Scholar] [CrossRef]
- Russell, C.; Pang, M.; Nafeh, F.; MacDonald, S.F.; Derkzen, D.; Rehm, J.; Fischer, B. Applying the socio-ecological model to understand community reintegration experiences among individuals on opioid agonist treatment (OAT) released from federal incarceration in Ontario, Canada. SSM-Qual. Res. Health 2022, 2, 100083. [Google Scholar] [CrossRef]
- Bunting, A.M.; Oser, C.B.; Staton, M.; Eddens, K.S.; Knudsen, H. Clinician identified barriers to treatment for individuals in Appalachia with opioid use disorder following release from prison: A social ecological approach. Addict. Sci. Clin. Pract. 2018, 13, 23. [Google Scholar] [CrossRef]
- Kahn, L.S.; Wozniak, M.L.; Doscher, T.; Moore, C.; Vest, B.M. Treatment Experiences Among People Who Use Opioids: A Social Ecological Approach. Qual. Health Res. 2022, 32, 1386–1398. [Google Scholar] [CrossRef]
- Black, D.C. Review of Drugs Executive Summary; The Home Office: London, UK, 2020.
- Black, D.C. Review of Drugs Part Two: Prevention, Treatment and Recovery: Annexes; Department of Health & Social Care: London, UK, 2021.
- HM Government. From Harm to Hope: A 10-Year Drugs Plan to Cut Crime and Save Lives. 2021. Available online: https://www.gov.uk/government/publications/from-harm-to-hope-a-10-year-drugs-plan-to-cut-crime-and-save-lives (accessed on 22 August 2022).
- HM Government. Government Response to the Independent Review of Drugs by Dame Carol Black. GOV.UK. 2021. Available online: https://www.gov.uk/government/publications/independent-review-of-drugs-by-dame-carol-black-government-response/government-response-to-the-independent-review-of-drugs-by-dame-carol-black (accessed on 26 September 2022).
- The White House. FACT SHEET: Biden-Harris Administration Announces New Actions and Funding to Address the Overdose Epidemic and Support Recovery. The White House. 2022. Available online: https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/23/fact-sheet-biden-harris-administration-announces-new-actions-and-funding-to-address-the-overdose-epidemic-and-support-recovery/ (accessed on 26 September 2022).
- Hay, G.; Rael dos Santos, A.; Reed, H.; Hope, V. Estimates of the Prevalence of Opiate Use and/or Crack Cocaine Use, 2016/17: Sweep 13 Report. 2019. Available online: www.ljmu.ac.uk/phi (accessed on 24 October 2022).
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual. Health Res. 2016, 26, 1753–1760. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Bhaskar, R. A Realist Theory of Science; Leeds Books Limited: Leeds, UK, 1975. [Google Scholar]
- Gorski, P.S. What is critical realism? And why should you care? ontemp. Sociol. 2013, 42, 658–670. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo (Version 12). 2020. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed on 1 November 2022).
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE: New York, NY, USA, 2013; 402p. [Google Scholar]
- Lilly, R.; Quirk, A.; Rhodes, T.; Stimson, G.V. Juggling multiple roles: Staff and client perceptions of keyworker roles and the constraints on delivering counselling and support services in methadone treatment. Addict Res. Vol. 1999, 7, 267–289. [Google Scholar] [CrossRef]
- Frank, D.; Mateu-Gelabert, P.; Perlman, D.C.; Walters, S.M.; Curran, L.; Guarino, H. “It’s like ‘liquid handcuffs”: The effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives. Harm. Reduct. J. 2021, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Carlisle, V. A Pharmacy Resolution for 2021: Let’s Improve the Way Patients with Addiction are Treated. Pharm. J. 2021. Available online: https://www.pharmaceutical-journal.com/news-and-analysis/opinion/comment/a-pharmacy-resolution-for-2021-lets-improve-the-way-patients-with-addiction-are-treated/20208688.article (accessed on 9 January 2021).
- Van Hout, M.C.; Bingham, T. Methadone maintenance and Special Community Employment schemes: A study of Irish participants’ views. J. Vocat. Rehabil. 2012, 37, 63–73. [Google Scholar] [CrossRef]
- Cloud, W.; Granfield, R. Conceptualizing recovery capital: Expansion of a theoretical construct. Subst. Use Misuse. 2008, 43, 1971–1986. Available online: http://www.tandfonline.com/doi/pdf/10.1080/10826080802289762?needAccess=true. (accessed on 1 November 2022). [CrossRef]
- Aslan, L.; Parkman, T.J.; Skagerlind, N. An Evaluation of the Mutual Aid Facilitation Sessions Pilot Program, “You do the MAFS”. J. Groups Addict. Recovery 2016, 11, 109–124. [Google Scholar] [CrossRef]
- Gronnestad, T.E.; Sagvaag, H. Stuck in limbo: Illicit drug users’ experiences with opioid maintenance treatment and the relation to recovery. Int. J. Qual. Stud. Health Well-Being 2016, 11, 31992. [Google Scholar] [CrossRef]
- Notley, C.; Blyth, A.; Maskrey, V.; Pinto, H.; Holland, R. Exploring the Concepts of Abstinence and Recovery Through the Experiences of Long-Term Opiate Substitution Clients. Subst. Abuse 2015, 36, 232–239. [Google Scholar] [CrossRef]
- O’Byrne, P.; Jeske Pearson, C. Methadone maintenance treatment as social control: Analyzing patient experiences. Nurs Inq. 2018, 26, e12275. [Google Scholar]
- Rance, J.; Treloar, C. “Not just methadone Tracy”: Transformations in service-user identity following the introduction of hepatitis C treatment into Australian opiate substitution settings. Addict Vol. 2014, 109, 452–459. [Google Scholar] [CrossRef]
- Fischer, B.; Chin, A.T.; Kuo, I.; Kirst, M.; Vlahov, D. Canadian Opioid Users’ Views on Methadone and other Opiate Prescription Treatment: An Exploratory Qualitative Study. Subst Use Misuse 2002, 37, 495–522. [Google Scholar] [CrossRef]
- Lindgren, B.M.; Eklund, M.; Melin, Y.; Graneheim, U.H. From Resistance to Existence—Experiences of Medication-Assisted Treatment as Disclosed by People with Opioid Dependence. Issues Ment. Health Nurs. 2015, 36, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Yarborough, B.J.H.; Stumbo, S.P.; McCarty, D.; Mertens, J.; Weisner, C.; Green, C.A. Methadone, buprenorphine and preferences for opioid agonist treatment: A qualitative analysis. Drug Alcohol Depend. Vol. 2016, 160, 112–118. [Google Scholar] [CrossRef]
- Madden, E.F. Intervention stigma: How medication-assisted treatment marginalizes patients and providers. Soc. Sci. Med. 2019, 232, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Earnshaw, V.A.; Smith, L.R.; Chaudoir, S.R.; Amico, K.R.; Copenhaver, M.M. HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav. 2013, 17, 1785–1795. [Google Scholar] [CrossRef]
- Medina-Perucha, L.; Scott, J.; Chapman, S.; Barnett, J.; Dack, C.; Family, H. Sexual health services in community pharmacy for women on opioid substitution treatment: A qualitative study. Eur. J. Public Health 2020, 30, 733–738. [Google Scholar] [CrossRef]
- Turan, J.M.; Elafros, M.A.; Logie, C.H.; Banik, S.; Turan, B.; Crockett, K.B.; Pescosolido, B.; Murray, S.M. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019, 17, 7. [Google Scholar]
- Kesten, J.M.; Holland, A.; Linton, M.J.; Family, H.; Scott, J.; Horwood, J.; Hickman, M.; Telfer, M.; Ayres, R.; Hussey, D.; et al. Living Under Coronavirus and Injecting Drugs in Bristol (LUCID-B): A qualitative study of experiences of COVID-19 among people who inject drugs. Int. J. Drug Policy 2021, Vol 98, 103391. [Google Scholar] [CrossRef]
- Deci, E.; Ryan, R. The Support of Autonomy and the Control of Behavior. J. Pers. Soc. Psychol. 1987, 53, 1024–1037. [Google Scholar] [CrossRef]
- Brener, L.; Broady, T.; Cama, E.; Hopwood, M.; Byrne, J.; Treloar, C. Positive effects of community attachment on internalised stigma and wellbeing among people who inject drugs. Int. J. Drug Policy 2021, 97, 103323. [Google Scholar] [CrossRef] [PubMed]
- Birtel, M.D.; Wood, L.; Kempa, N.J. Stigma and social support in substance abuse: Implications for mental health and well-being. Psychiatry Res. 2017, 252, 1–8. [Google Scholar] [CrossRef] [PubMed]
- De Maeyer, J.; Vanderplasschen, W.; Camfield, L.; Vanheule, S.; Sabbe, B.; Broekaert, E. A good quality of life under the influence of methadone: A qualitative study among opiate-dependent individuals. Int. J. Nurs. Stud. 2011, 48, 1244–1257. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.D.; Stevens, A.; Harris, M.; Lewer, D.; Sumnall, H.; Stewart, D.; Gilvarry, E.; Wiseman, A.; Howkins, J.; McManus, J.; et al. Analysis of the UK Government’s 10-Year Drugs Strategy—A resource for practitioners and policymakers. J. Public Health 2022, fdac114. [Google Scholar] [CrossRef]
- NHS Addictions Provider Alliance. Dame Carol Black’s Independent Review of Drugs-Part Two Report is Welcomed by the NHS APA. 2021. Available online: https://www.nhsapa.org/post/dame-carol-black-phase-2-report (accessed on 23 September 2022).
- HM Government. About Project ADDER. GOV.UK. 2022. Available online: https://www.gov.uk/government/publications/project-adder/about-project-adder (accessed on 23 September 2022).
- Day, E.; Mitcheson, L. Psychosocial interventions in opiate substitution treatment services: Does the evidence provide a case for optimism or nihilism? Addiction 2017, 112, 1329–1336. [Google Scholar] [CrossRef]
- Livingston, J.D.; Adams, E.; Jordan, M.; MacMillan, Z.; Hering, R. Primary Care Physicians’ Views about Prescribing Methadone to Treat Opioid Use Disorder. Subst. Use Misuse 2018, 53, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Medina-Perucha, L.; Scott, J.; Chapman, S.; Barnett, J.; Dack, C.; Family, H. A qualitative study on intersectional stigma and sexual health among women on opioid substitution treatment in England: Implications for research, policy and practice. Soc. Sci. Med. 2019, 222, 315–322. [Google Scholar] [CrossRef]
- Notley, C.; Holland, R.; Maskrey, V.; Nagar, J.; Kouimtsidis, C. Regaining control: The patient experience of supervised compared with unsupervised consumption in opiate substitution treatment. Drug Alcohol Rev. 2014, 33, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Centre for Social Research in Health. Stigma Indicators Monitoring Project|Arts & Social Sciences-UNSW Sydney. Available online: https://www.arts.unsw.edu.au/centre-social-research-health/our-projects/stigma-indicators-monitoring-project (accessed on 21 July 2021).
- Hawe, P.; Shiell, A.; Riley, T. Theorising interventions as events in systems. Am. J. Community Psychol. 2009, 43, 267–276. [Google Scholar] [CrossRef]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ 2021, 374, n2061. [Google Scholar] [CrossRef]
- Lintzeris, N.; Deacon, R.M.; Hayes, V.; Cowan, T.; Mills, L.; Parvaresh, L.; Harvey Dodds, L.; Jansen, L.; Dojcinovic, R.; Leung, M.C.; et al. Opioid agonist treatment and patient outcomes during the COVID-19 pandemic in south east Sydney, Australia. Drug Alcohol Rev. 2022, 41, 1009–1019. [Google Scholar] [CrossRef] [PubMed]
- Crowley, D.; Delargy, I. A national model of remote care for assessing and providing opioid agonist treatment during the COVID-19 pandemic: A report. Harm Reduct. J. 2020, 17, 49. [Google Scholar] [CrossRef] [PubMed]
- Aldabergenov, D.; Reynolds, L.; Scott, J.; Kelleher, M.J.; Strang, J.; Copeland, C.S.; Kalk, N.J. Methadone and buprenorphine-related deaths among people prescribed and not prescribed Opioid Agonist Therapy during the COVID-19 pandemic in England. Int. J. Drug Policy 2022, 110, 103877. [Google Scholar] [CrossRef] [PubMed]
| Pseudonym | Gender | Medication | Treatment History * | Age (Years) |
|---|---|---|---|---|
| Andy | Male | None (post-detox) | 3 months | 45 |
| Ringo | Male | None (post-detox) | 4 years | 39 |
| Robert | Male | None (post-detox) | 7 months | 50 |
| Stuart | Male | None (post-detox) | 18 years | 42 |
| Anne-Marie | Female | Buprenorphine | 20 years | 52 |
| Hannah | Female | Buprenorphine | >20 years | 56 |
| Jack | Male | Buprenorphine | >10 years | 53 |
| Peter | Male | Buprenorphine | 12 years | 37 |
| Davina | Female | Methadone | 20 years | 56 |
| Hugh | Male | Methadone | >25 years | 75 |
| Keith | Male | Methadone | 25 years | 46 |
| Will | Male | Methadone | 13 years | 41 |
| n (%) | |
|---|---|
| Role | |
| Shared care worker | 5 (38) |
| Shared care team leader | 2 (15) |
| Community detox link worker | 2 (15) |
| Clinical psychologist | 1 (8) |
| Service manager | 3 (23) |
| Years of experience in current/similar role | |
| 1–5 | 5 (38) |
| 6–10 | 3 (23) |
| 11–20 | 5 (38) |
| Outcome | Participant | Illustrative Extracts |
|---|---|---|
| Health | ||
| Help-seeking for health complaints | Jenny (SP) Marc (SP) Brené (SP) | […] getting people to engage with Hep [hepatitis] treatment to maintain all their appointments with the [Unit for hepatitis treatment] and just address their physical health problems. We’re contributing to get more people into hepatitis treatment, to get more people tested… There’s so many more outcomes that you can be looking at, like well-being, physical health, emotional health, education, employment… We need to start looking at how many people have got a GP practice… |
| Individual | ||
| Stability | Anne-Marie (SU) | You can’t be constantly detoxing you get a point where you’re just like ‘I need to just get on with my life and I’ll worry about it in six months’ or something’. |
| Russel (SP) | I think being on that script has made a massive difference to his [service user’s] life. Now as a consequence he is living in a lower supported accommodation. He is much more stable. | |
| Gabor (SP) | Stability, life stability, that’s more important than being drug free to me, and I know that can mean being on a script for a lot longer… | |
| Stuart (SU) | […] putting the foundations in place…and then the next stuff are like your hobbies and things you want you know you’re sort of building that wall higher and higher because the shits’ over there and you’re not going to be able to climb over it anymore because you’ve built up so much stuff that it’s solid enough to keep you safe on that side… | |
| Stable housing | Jack (SU) | I’ve come a long way from the days of homelessness and being in the gutter with nothing not even any drugs then, you know what I mean? nothing, just some clothes. |
| Self-care | Russel (SP) | I think being on that script has made a massive difference to his life…He is looking after himself. He has got himself a bike, he is cycling every day on the bike. |
| Inter-personal | ||
| Wellbeing of children | Eric (SP) | Stop defining positive recovery as drug free. I mean, we have all got loads of clients who come into us and been chaotic and made slow changes and you know, now the kids are being fed […]. Fucking amazing, that alone is positive. |
| Russel (SP) | I had a client today that came in. Him and his partner have been using on and off for years. They have got three children. Social services are involved. Children are on the child protection register. He came in today buzzing saying to me, I haven’t used for three weeks…and he said to me, the children are happy. I said, well, mum and dad are happy, children are probably more likely to be happy. If he didn’t have that script where would he be? It is life changing. I can’t emphasise enough really how I think it is crucial that people that need OST [OAT] get OST. | |
| Healthy support networks | Russel (SP) | We need to start looking at…how many people have got positive social relationships outside of the drug user networks |
| Relationships | Russel (SP) | He [service user] didn’t have a good relationship with his mother; he suffered physical abuse and neglect.…emotional abuse…He actually said to me, when we were coming to the end of his treatment that because of what he had experienced he didn’t trust women and found it really difficult. And, actually, after working with me over a long period of time, he felt he could trust women now. The person that took over from me was another female and he had a good relationship with her. |
| Russel (SP) | I think being on that script has made a massive difference to his life…He has talked about regaining contact with his adult daughter. They had a good relationship, but he said they had not seen each other for a couple of years. He went to prison and he has not been in touch with her since…I saw him yesterday and I thought, wow, you’re a different person than I met the first time | |
| Domestic violence | Jenny (SP) | The only thing that’s counted is the drug free stat, all the little steps that get you there aren’t really… when it comes to my supervision—how many have you got drug free? Any drug frees coming in the next month? It’s sort of like, well no really, but then all this work I’ve done with this client who’s having horrific domestic violence…what about that? Is that not counted? […] I was worried that I was going to come into surgery and find out that she’d been murdered or something, whereas now it feels like the early days of recovery for her. |
| Financial | ||
| Access to benefits | Brené (SP) | […] we need to start looking at how many people have been linked up with housing services, how many people have been in touch with benefits advice… |
| Access to education and employment | Gabor (SP) | there’s so many more outcomes that you can be looking at, like well-being, physical health, emotional health, education, employment… |
| General | ||
| Medically Assisted Recovery (MAR) = successful treatment | Brené (SP) | I don’t see why there can’t be an exit code to say actually successful completion, medically assisted recovery and we have recovery check-ins with them. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carlisle, V.R.; Maynard, O.M.; Bagnall, D.; Hickman, M.; Shorrock, J.; Thomas, K.; Kesten, J. Should I Stay or Should I Go? A Qualitative Exploration of Stigma and Other Factors Influencing Opioid Agonist Treatment Journeys. Int. J. Environ. Res. Public Health 2023, 20, 1526. https://doi.org/10.3390/ijerph20021526
Carlisle VR, Maynard OM, Bagnall D, Hickman M, Shorrock J, Thomas K, Kesten J. Should I Stay or Should I Go? A Qualitative Exploration of Stigma and Other Factors Influencing Opioid Agonist Treatment Journeys. International Journal of Environmental Research and Public Health. 2023; 20(2):1526. https://doi.org/10.3390/ijerph20021526
Chicago/Turabian StyleCarlisle, Victoria Rice, Olivia M. Maynard, Darren Bagnall, Matthew Hickman, Jon Shorrock, Kyla Thomas, and Joanna Kesten. 2023. "Should I Stay or Should I Go? A Qualitative Exploration of Stigma and Other Factors Influencing Opioid Agonist Treatment Journeys" International Journal of Environmental Research and Public Health 20, no. 2: 1526. https://doi.org/10.3390/ijerph20021526
APA StyleCarlisle, V. R., Maynard, O. M., Bagnall, D., Hickman, M., Shorrock, J., Thomas, K., & Kesten, J. (2023). Should I Stay or Should I Go? A Qualitative Exploration of Stigma and Other Factors Influencing Opioid Agonist Treatment Journeys. International Journal of Environmental Research and Public Health, 20(2), 1526. https://doi.org/10.3390/ijerph20021526






