Foam Rolling vs. Proprioceptive Neuromuscular Facilitation Stretching in the Hamstring Flexibility of Amateur Athletes: Control Trials
Abstract
1. Introduction
2. Materials and Methods
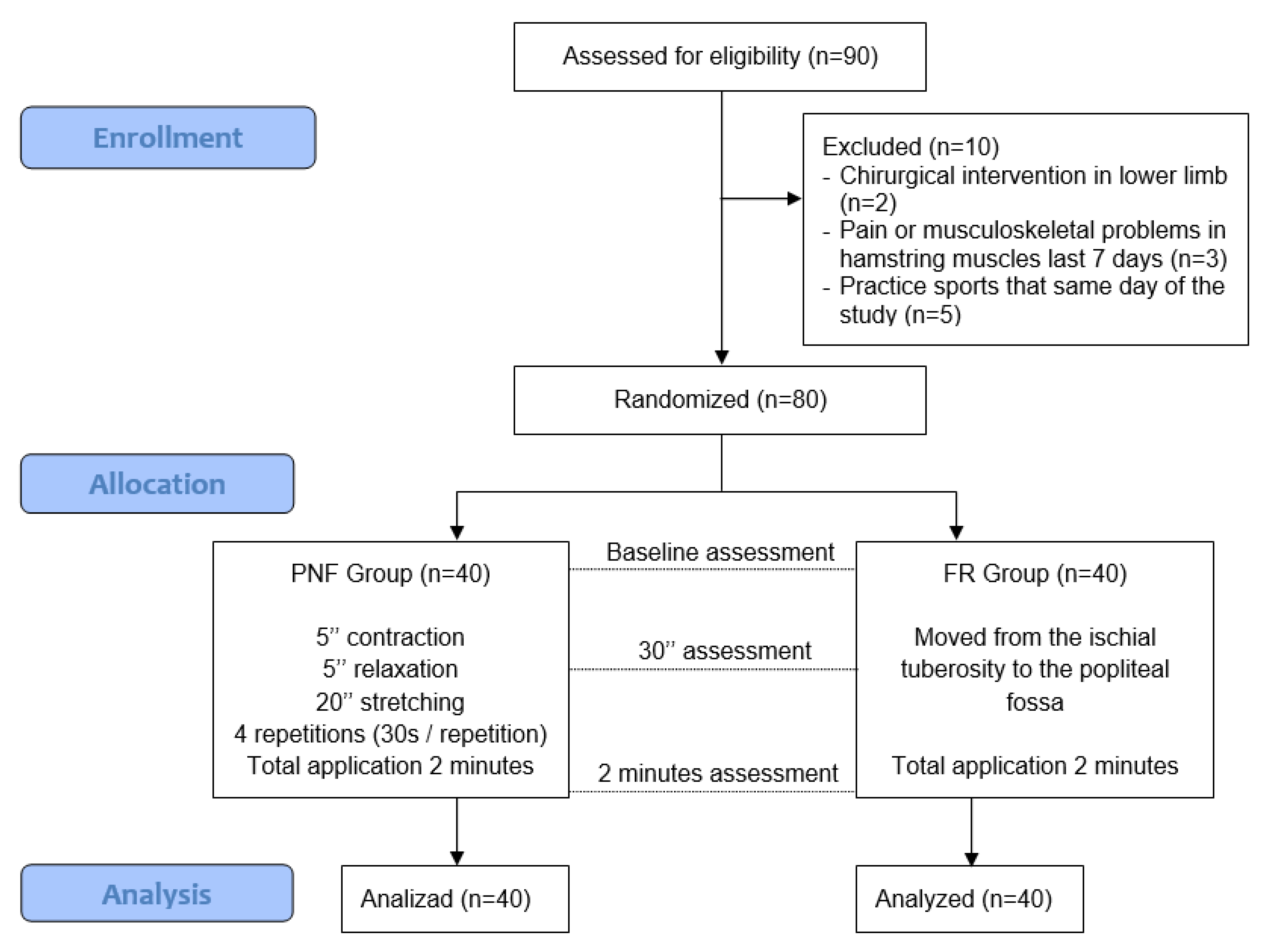
2.1. Study Design
2.2. Participants
2.3. Variables and Measurements
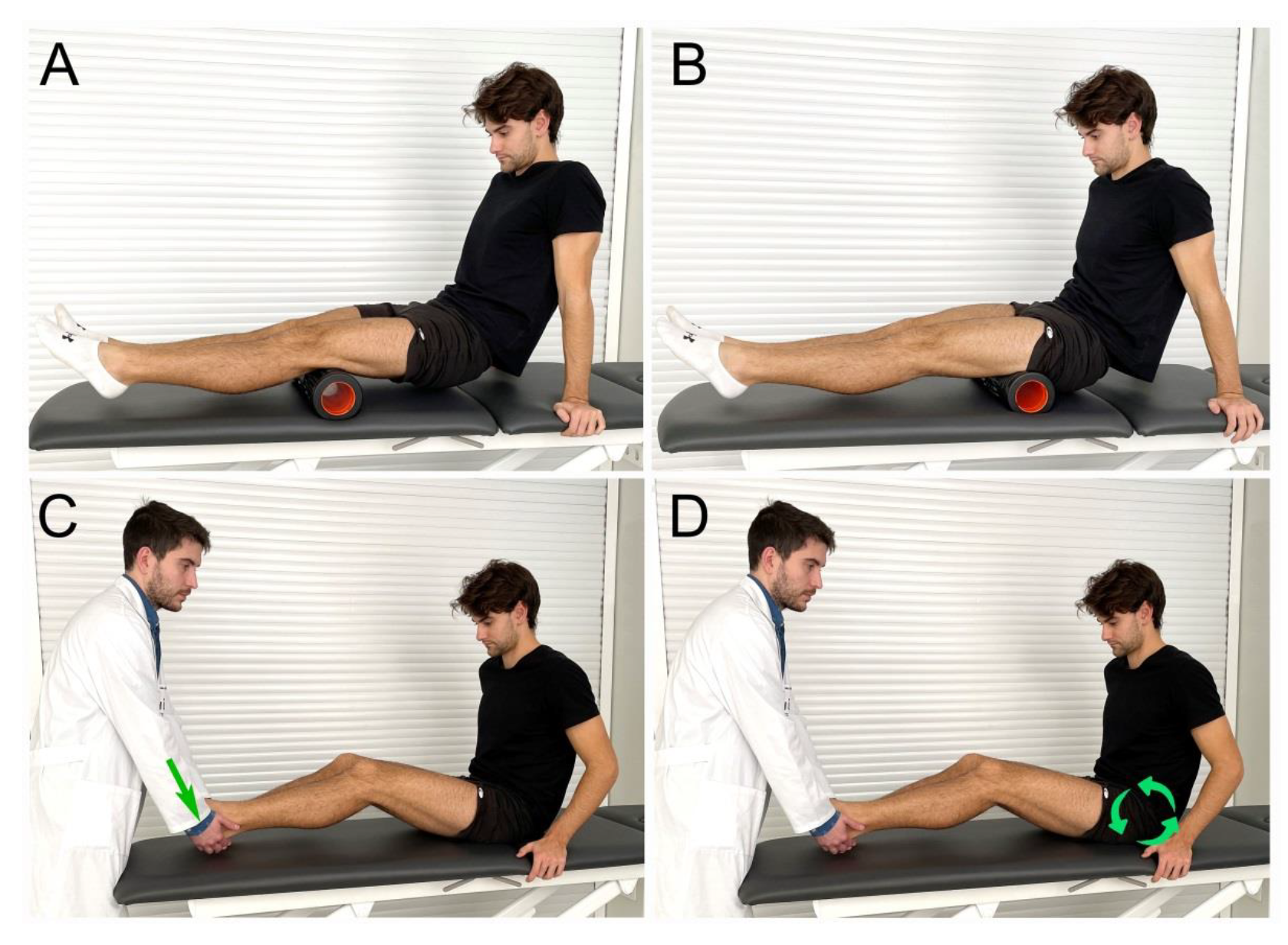
2.4. Interventions
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dadebo, B.; White, J.; George, K.P. A survey of flexibility training protocols and hamstring strains in professional football clubs in england. Br. J. Sports Med. 2004, 38, 388–394. [Google Scholar] [CrossRef]
- Woods, C.; Hawkins, R.D.; Maltby, S.; Hulse, M.; Thomas, A.; Hodson, A. The football association medical research programme: An audit of injuries in professional football—Analysis of hamstring injuries. Br. J. Sports Med. 2004, 38, 36–41. [Google Scholar] [CrossRef]
- Hoskins, W.; Pollard, H. The management of hamstring injury—Part 1: Issues in diagnosis. Man Ther. 2005, 10, 96–107. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Shield, A.J. Hamstring strain injuries: Factors that lead to injury and re-injury. Sports Med. 2012, 42, 209–226. [Google Scholar] [CrossRef]
- Sherry, M.A.; Best, T.M. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J. Orthop. Sport. Phys. Ther. 2004, 34, 116–125. [Google Scholar] [CrossRef]
- Bacurau, R.F.; Monteiro, G.A.; Ugrinowitsch, C.; Tricoli, V.; Cabral, L.F.; Aoki, M.S. Acute effect of a ballistic and a static stretching exercise bout on flexibility and maximal strength. J. Strength Cond. Res. 2009, 23, 304–308. [Google Scholar] [CrossRef]
- Engebretsen, A.H.; Myklebust, G.; Holme, I.; Engebretsen, L.; Bahr, R. Intrinsic risk factors for hamstring injuries among male soccer players: A prospective cohort study. Am. J. Sports Med. 2010, 38, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Perez-Bellmunt, A.; Miguel-Perez, M.; Brugue, M.B.; Cabús, J.B.; Casals, M.; Martinoli, C.; Kuisma, R. An anatomical and histological study of the structures surrounding the proximal attachment of the hamstring muscles. Man. Ther. 2015, 20, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Borman, N.P.; Trudelle-Jackson, E.; Smith, S.S. Effect of stretch positions on hamstring muscle length, lumbar flexion range of motion, and lumbar curvature in healthy adults. Physiother. Theory Pract. 2011, 27, 146–154. [Google Scholar] [CrossRef] [PubMed]
- López-Miñarro, P.; Muyor, J.; Belmonte, F.; Alacid, F. Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. J. Hum. Kinet. 2012, 31, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, M.S. The argument against static stretching before sport and physical activity. Athl. Ther. Today 2010, 11, 6–8. [Google Scholar] [CrossRef]
- Covert, C.A.; Alexander, M.P.; Petronis, J.J.; Davis, D.S. Comparison of ballistic and static stretching on hamstring muscle length using an equal stretching dose. J. Strength Cond. Res. 2010, 24, 3008–3014. [Google Scholar] [CrossRef] [PubMed]
- Funk, D.C.; Swank, A.M.; Mikla, B.M.; Fagan, T.A.; Farr, B.K. Impact of prior exercise on hamstring flexibility: A comparison of proprioceptive neuromuscular facilitation and static stretching. J. Strength Cond. Res. 2003, 17, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Schuback, B.; Hooper, J.; Salisbury, L. A comparison of a self-stretch incorporating proprioceptive neuromuscular facilitation components and a therapist-applied PNF-technique on hamstring flexibility. Physiotherapy 2004, 90, 151–157. [Google Scholar] [CrossRef]
- Sharman, M.J.; Cresswell, A.G.; Riek, S. Proprioceptive neuromuscular facilitation stretching. Sports Med. 2006, 36, 929–939. [Google Scholar] [CrossRef]
- Pacheco, L.; Balius, R.; Aliste, L.; Pujol, M.; Pedret, C. The acute effects of different stretching exercises on jump performance. J. Strength Cond. Res. 2011, 25, 2991–2998. [Google Scholar] [CrossRef]
- Fauris, P.; López-de-Celis, C.; Canet-Vintró, M.; Martin, J.C.; Llurda-Almuzara, L.; Rodríguez-Sanz, J.; Labata-Lezaun, N.; Simon, M.; Pérez-Bellmunt, A. Does self-myofascial release cause a remote hamstring stretching effect based on myofascial chains? A randomized controlled trial. Int. J. Environ. Res. Public Health 2021, 18, 12356. [Google Scholar] [CrossRef]
- Wilke, J.; Müller, A.; Giesche, F.; Power, G.; Ahmedi, H.; Behm, D.G. Acute effects of foam rolling on range of motion in healthy adults: A systematic review with multilevel meta-analysis. Sports Med. 2020, 50, 387–402. [Google Scholar] [CrossRef]
- Nakamura, M.; Onuma, R.; Kiyono, R.; Yasaka, K.; Sato, S.; Yahata, K.; Fukaya, T.; Konrad, A. The acute and prolonged effects of different durations of foam rolling on range of motion, muscle stiffness, and muscle strength. J. Sports Sci. Med. 2021, 20, 62–68. [Google Scholar] [CrossRef]
- Konrad, A.; Nakamura, M.; Paternoster, F.K.; Tilp, M.; Behm, D.G. A comparison of a single bout of stretching or foam rolling on range of motion in healthy adults. Eur J Appl Physiol. 2022, 122, 1545–1557. [Google Scholar] [CrossRef]
- Monteiro, E.R.; Cavanaugh, M.T.; Frost, D.M.; Novaes, J.D. Is self-massage an effective joint range-of-motion strategy? A pilot study. J. Bodyw. Mov. Ther. 2017, 21, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, K.M.; Silvey, D.B.; Button, D.C.; Behm, D.G. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int. J. Sports Phys. Ther. 2013, 8, 228–236. [Google Scholar]
- Cheatham, S.W.; Kolber, M.J.; Cain, M.; Lee, M. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: A systematic review. Int. J. Sports Phys. Ther. 2015, 10, 827–838. [Google Scholar]
- MacDonald, G.Z. Foam Rolling as a Recovery Tool Following an Intense Bout of Physical Activity. PhD Thesis, Memorial University of Newfoundland, St. John’s, NL, Canada, 2013. [Google Scholar]
- Healey, K.C.; Hatfield, D.L.; Blanpied, P.; Dorfman, L.R.; Riebe, D. The effects of myofascial release with foam rolling on performance. J. Strength Cond. Res. 2014, 28, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Konrad, A.; Nakamura, M.; Behm, D.G. The effects of foam rolling training on performance parameters: A systematic review and meta-analysis including controlled and randomized controlled trials. Int. J. Environ. Res. Public Health 2022, 19, 11638. [Google Scholar] [CrossRef]
- Halperin, I.; Aboodarda, S.J.; Button, D.C.; Andersen, L.L.; Behm, D.G. Roller massager improves range of motion of plantar flexor muscles without subsequent decreases in force parameters. Int. J. Sports Phys. Ther. 2014, 9, 92–102. [Google Scholar] [PubMed]
- Su, H.; Chang, N.; Wu, W.; Guo, L.; Chu, I. Acute effects of foam rolling, static stretching, and dynamic stretching during warm-ups on muscular flexibility and strength in young adults. J. Sport Rehab. 2017, 26, 469–477. [Google Scholar] [CrossRef]
- Fairall, R.R.; Cabell, L.; Boergers, R.J.; Battaglia, F. Acute effects of self-myofascial release and stretching in overhead athletes with GIRD. J. Bodyw. Mov. Ther. 2017, 21, 648–652. [Google Scholar] [CrossRef]
- Harriss, D.; MacSween, A.; Atkinson, G. Ethical standards in sport and exercise science research: 2020 update. Int. J. Sports Med. 2019, 40, 813–817. [Google Scholar] [CrossRef]
- Castro-Piñero, J.; Chillon, P.; Ortega, F.; Montesinos, J.; Sjöström, M.; Ruiz, J. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6–17 years. Int. J. Sports Med. 2009, 30, 658–662. [Google Scholar] [CrossRef]
- Ayala, F.; de Baranda, P.S.; Croix, M.D.S.; Santonja, F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef]
- Mayorga Vega, D.; Viciana, J.; Cocca, A.; Merino Marban, R. Criterion-related validity of toe-touch test for estimating hamstring extensibility: A meta-analysis. Hum. Sport Exerc. 2014, 9, 188–200. [Google Scholar] [CrossRef]
- Ayala, F.; de Baranda, P.S. Fiabilidad absoluta de las pruebas sit and reach modificado y back saber sit and reach para estimar la flexibilidad isquiosural en jugadores de fútbol sala. Apunts. Med. de l’Esport 2011, 46, 81–88. [Google Scholar] [CrossRef]
- Hoeger, W.W.; Hopkins, D.R.; Button, S.; Palmer, T.A. Comparing the sit and reach with the modified sit and reach in measuring flexibility in adolescents. Pediatr. Exerc. Sci. 1990, 2, 156–162. [Google Scholar] [CrossRef]
- Esnault, M.; Viel, É. Stretching: Estiramientos de las Cadenas Musculares; Elsevier: Barcelona, Spain, 2003. [Google Scholar]
- Jung, J.; Choi, W.; Lee, Y.; Kim, J.; Kim, H.; Lee, K.; Lee, J.; Lee, S. Immediate effect of self-myofascial release on hamstring flexibility. Phys. Ther. Rehabil. Sci. 2017, 6, 45–51. [Google Scholar] [CrossRef]
- Curran, P.F.; Fiore, R.D.; Crisco, J.J. A comparison of the pressure exerted on soft tissue by 2 myofascial rollers. J. Sport Rehab. 2008, 17, 432–442. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Mohr, A.R.; Long, B.C.; Goad, C.L. Effect of foam rolling and static stretching on passive hip-flexion range of motion. J. Sport Rehab. 2014, 23, 296–299. [Google Scholar] [CrossRef]
- Skarabot, J.; Beardsley, C.; Stirn, I. Comparing the effects of self-myofascial release with static stretching on ankle range-of-motion in adolescent athletes. Int. J. Sports Phys. Ther. 2015, 10, 203–212. [Google Scholar]
- Somers, K.; Aune, D.; Horten, A.; Kim, J.; Rogers, J. Acute effects of Gastrocnemius/Soleus self-myofascial release vs. dynamic stretching on closed chain dorsiflexion. J. Sport Rehab. 2019, 29, 287–293. [Google Scholar] [CrossRef]
- Perez-Bellmunt, A.; Casasayas, O.; Navarro, R.; Simon, M.; Martin, J.C.; Pérez-Corbella, C.; Blasi, M.; Ortiz, S.; Álvarez, P.; Pacheco, L. Effectiveness of low-frequency electrical stimulation in proprioceptive neuromuscular facilitation techniques in healthy males: A randomized controlled trial. J. Sports Med. Phys. Fit. 2019, 59, 469–475. [Google Scholar] [CrossRef]
- Schleip, R. Fascial plasticity—A new neurobiological explanation: Part 1. J. Bodyw. Mov. Ther. 2003, 7, 11–19. [Google Scholar] [CrossRef]
- DeBruyne, D.M.; Dewhurst, M.M.; Fischer, K.M.; Wojtanowski, M.S.; Durall, C. Self-mobilization using a foam roller versus a roller massager: Which is more effective for increasing hamstrings flexibility? J. Sport Rehab. 2017, 26, 94–100. [Google Scholar] [CrossRef] [PubMed]
| PNF Group | FR Group | |
|---|---|---|
| Sex | ||
| Men | 29 (72.5%) | 24 (60%) |
| Women | 11 (27.5%) | 16 (40%) |
| Age | 23.38 (4.24) | 22.5 (4.54) |
| Flexibility | 22.48 (10.36) | 22.3 (11.29) |
| SR-0 | SR-1 | SR-2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Difference SR-0 to SR-1 | Difference SR-0 to SR-2 | ||||||||||
| Variables | Mean ± SD | Mean ± SD | Mean | 95% CI | p | ES | Mean ± SD | Mean | 95% CI | p | ES |
| FR group | 22.35 ± 11.30 | 24.02 ± 11.31 | 1.67 | [0.940; 2.410] | <0.001 | 0.15 | 25.90 ± 10.87 | 3.55 | [2.700; 4.400] | <0.001 | 0.32 |
| PNF group | 22.48 ± 10.36 | 25.67 ± 9.92 | 3.19 | [2.395; 30.990] | <0.001 | 0.32 | 28.12 ± 9.71 | 5.64 | [4.772; 6.509] | <0.001 | 0.56 |
| Difference between SR-0 and SR-1 | Difference between SR-0 and SR-2 | Difference between SR-1 and SR-2 | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| FR group | 1.67 ± 1.85 | 3.55 ± 2.14 | 1.87 ± 1.30 |
| PNF group | 3.19 ± 2.01 | 5.64 ± 2.19 | 2.44 ± 1.47 |
| p-value | 0.001 | 0.070 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Bellmunt, A.; Casasayas-Cos, O.; Ragazzi, P.; Rodríguez-Sanz, J.; Hidalgo-García, C.; Canet-Vintró, M.; Caballero-Martínez, I.; Pacheco, L.; López-de-Celis, C. Foam Rolling vs. Proprioceptive Neuromuscular Facilitation Stretching in the Hamstring Flexibility of Amateur Athletes: Control Trials. Int. J. Environ. Res. Public Health 2023, 20, 1439. https://doi.org/10.3390/ijerph20021439
Pérez-Bellmunt A, Casasayas-Cos O, Ragazzi P, Rodríguez-Sanz J, Hidalgo-García C, Canet-Vintró M, Caballero-Martínez I, Pacheco L, López-de-Celis C. Foam Rolling vs. Proprioceptive Neuromuscular Facilitation Stretching in the Hamstring Flexibility of Amateur Athletes: Control Trials. International Journal of Environmental Research and Public Health. 2023; 20(2):1439. https://doi.org/10.3390/ijerph20021439
Chicago/Turabian StylePérez-Bellmunt, Albert, Oriol Casasayas-Cos, Paolo Ragazzi, Jacobo Rodríguez-Sanz, César Hidalgo-García, Max Canet-Vintró, Iván Caballero-Martínez, Laura Pacheco, and Carlos López-de-Celis. 2023. "Foam Rolling vs. Proprioceptive Neuromuscular Facilitation Stretching in the Hamstring Flexibility of Amateur Athletes: Control Trials" International Journal of Environmental Research and Public Health 20, no. 2: 1439. https://doi.org/10.3390/ijerph20021439
APA StylePérez-Bellmunt, A., Casasayas-Cos, O., Ragazzi, P., Rodríguez-Sanz, J., Hidalgo-García, C., Canet-Vintró, M., Caballero-Martínez, I., Pacheco, L., & López-de-Celis, C. (2023). Foam Rolling vs. Proprioceptive Neuromuscular Facilitation Stretching in the Hamstring Flexibility of Amateur Athletes: Control Trials. International Journal of Environmental Research and Public Health, 20(2), 1439. https://doi.org/10.3390/ijerph20021439










