1. Introduction
Patient inflow into the emergency department (ED) has increased in recent years [
1]. Coping strategies, beyond increasing staff, need to be developed. While extra clinical solutions such as hotlines and general practitioner gatekeepers have been established in some countries, other countries have to optimize their EDs to increase patient outflow [
2]. Triage systems such as the Manchester triage, have been developed to identify critically ill or injured patients, not to increase patient flow into the ED [
3]. Many decision-making algorithms and heuristics have been implemented since the development of the triage system to address the issue of increased ED inflow [
4,
5,
6].
Orthopedic trauma EDs face similar problems concerning the overwhelming number of patients and the lack of algorithms or tools to increase patient flow sufficiently, except by increasing infrastructure [
7]. The main focus of orthopedic traumatology EDs is the detection and treatment of fractures. In most hospitals, a radiological diagnosis must be preceded by an examination by a physician, sometimes even by a specialist. Thus, if a questionnaire or algorithm significantly increases the likelihood of the presence of a fracture, the patient flow could be optimized and the traditional route could be skipped. Similar to modern hospitals where patients are guided by tablets [
8] between outpatient departments, in the ED, patients can fill out questionnaires that could sort and direct them efficiently before the first contact with a doctor. There is no doubt that physicians’ roles need to be reduced, starting with simple diagnoses that could be delegated to nurses, telemedicine, or even artificial intelligence [
9,
10,
11].
The goal of this study was to determine simple factors that could detect fractures in patients without the need for specialized personnel.
The hypothesis was that factors exist that could predict a fractured bone or, at least, a high probability of fracture. These factors would result from two different sources from the patient: objective information, such as localization of the fracture and patient age, and subjective information that the patient can articulate, such as pain. Although very different in reliability, both these types of information can be collected.
2. Materials and Methods
From 2014 to 2015, we prospectively enrolled 798, 445 men (55.4%) and 356 women (44.6%), with an average age of 42.67 years (SD 20.55), consecutive patients in our orthopedic trauma ED, a level-one trauma university hospital. The inclusion criterion was patients with an extremity mono-trauma; the exclusion criteria were polytraumatized patients and patients without a mechanism leading to a fracture such as stab wounds, pregnancy, and cognitive impairment.
Objective and subjective data were evaluated from questionnaires given to patients in the ED (the questionnaire can be found in the
Appendix A). These questionnaires were completed before contact with a doctor and placed in a box. So, the diagnosing doctor never saw the questionnaire and was blinded to it. The level of experience of the diagnosing doctor was 2.23 years (SD 3.42 y; range from 0–6), post-university. The questionnaire was related to the patient and the diagnosis.
For objective data, we evaluated the incidence of upper extremity (UE) and lower extremity (LE) fractures by anatomic region and age.
Subjective data collected included: visual analogue scale (VAS) [
12], time of pain onset, and two functional questions for UE and LE:
Finally, patients were asked if they thought a bone was broken.
For subjective data, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were assessed for the functional questions and patient assessment of a fracture. The functional questions (A1, A2, B1, and B2) were positive for fracture if the answer was “no”. The risk of fracture was assessed for the VAS and compared with the different pain outbreaks using Fisher’s exact test. The radiological examination served as a benchmark. As the questionnaires were adopted during the study, some analyzed subgroups (onset of pain and functional questions A2 and B2) had a lower number of patients. The mechanism of untwisting a bottle (A2) should involve the hand and that of walking on the toes (B2) should involve the foot.
Note that the patients were not supposed to complete questions A and B but just answer them hypothetically.
The study was conducted in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. It was reviewed and approved by the Charité Ethics Committee. Informed consent was obtained from all individual participants included in the study.
A power analysis for the sample size estimation was performed before study initiation with pain intensity as the primary endpoint with a beta error = 0.80. Differences were considered statistically significant if the null hypothesis could be rejected with >95% confidence (p < 0.05). The different parameters (objective and subjective) were analyzed with the Chi-squared test.
3. Results
3.1. Objective Data
3.1.1. Injured Regions
A total of 798 patients were included, of whom 281 (35.21%) had a fracture.
More patients with injuries to the LE (n = 474; 59.40%) presented in the ED than those with injuries to the UE (n = 324; 40.60%), but the fracture risk was higher for the UE (n = 150; 46.30%) than for the LE (n = 131; 27.64%). This difference was highly significant (p < 0.00001, Chi-square test).
The highest risk for fractures in one region was the hip (73.21%;
n = 56), followed by the wrist (60.32%;
n = 63) and femoral shaft (4 of 7, 57.14%;
n = 7); the regions with the lowest risk were the knee (8.41%;
n = 107), ankle (18.29%;
n = 164), and forearm shaft (30.00%;
n = 10) (
Table 1).
3.1.2. Age
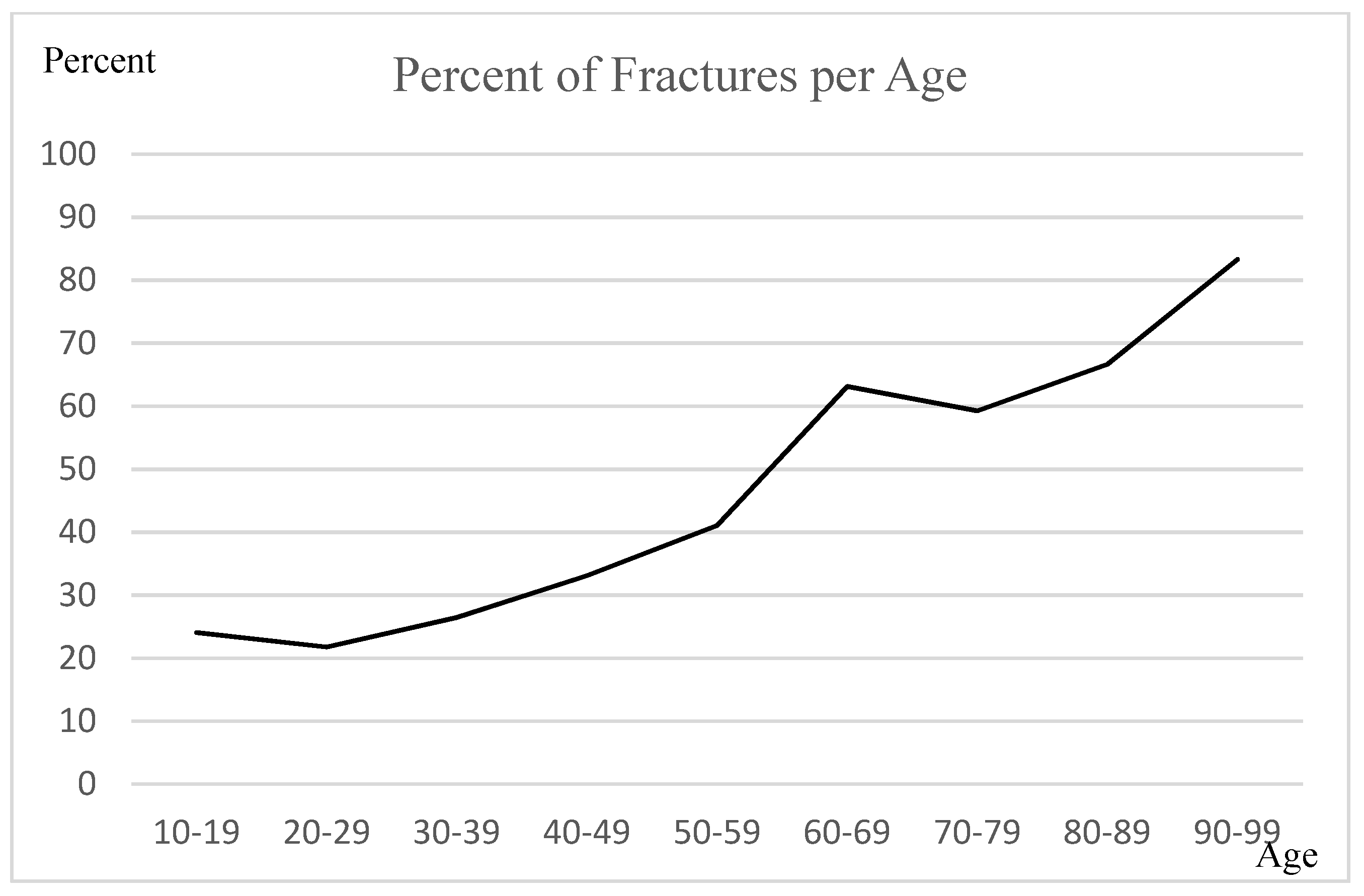
Half of the patients in the ED were younger than 40 years (n= 413; 51.73%) and accounted for one-third of the fractures (n = 99; 35.23%). Geriatric patients represented one-fifth of the study population (age > 59 years, n = 152; 19.05%) and accounted for one-third of the fractures (n = 98; 34.88%). The probability for patients older than 59 years of age to have a fracture was higher than 59.26%; patients older than 90 years had an 83.33% probability of a fracture. The percentage of fractures in patients older than 59 years was significantly higher than that in patients below 59 years (p < 0.00001, Chi-square test).
From young to old age, the fracture risk increased almost linearly (
Figure 1).
3.2. Subjective Data
Functional Questions
The sensitivity, specificity, PPV, and NPV were evaluated for anatomic regions (
Table 2). The regions where the number of patients was too low were excluded (femoral shaft,
n = 7; tibial shaft,
n = 25; humeral shaft,
n = 8; and forearm shaft,
n = 10) for this evaluation.
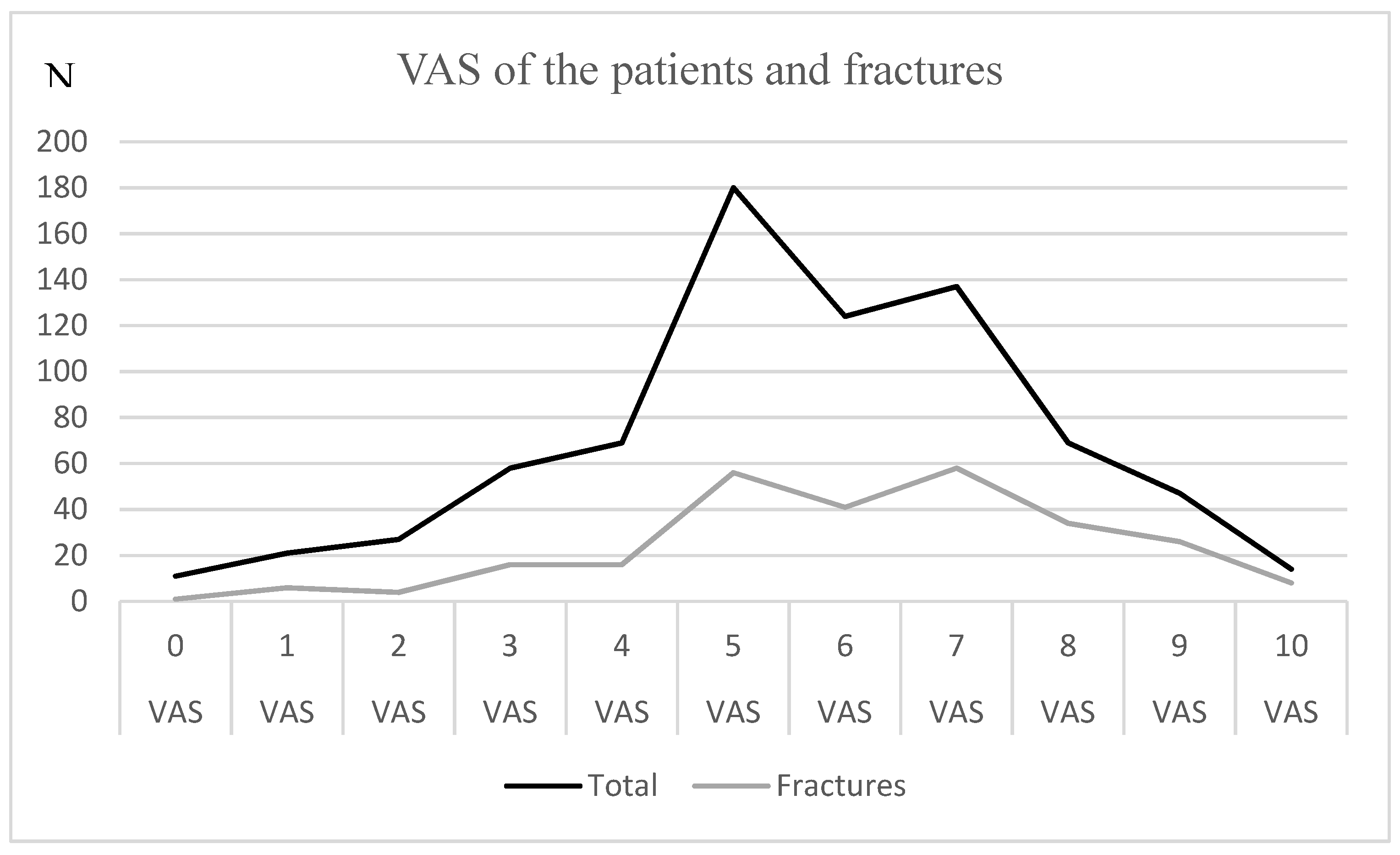
3.3. VAS (n = 795)
The VAS values throughout the study population and for the fractured patients are shown in
Figure 2. A normal distribution seemed to be apparent, with the highest number of patients having a VAS value of five among all patients in the ED. Most patients with fractures had a VAS score of seven.
For VAS values higher than six, the risk for fracture was higher than 40%, and for a VAS value of 10, the risk was 57.14%. The number of patients with VAS values < 3 and VAS values > 8 was too low to draw a clear conclusion (n = 11–47).
3.4. Pain Onset (n = 363)
The onset of pain showed no significant difference between patients with and without fractures (
Table 3).
3.5. Patient Fracture Assessments (n = 798)
The patient’s sensitivity was 58.64%, and the specificity was 71.77%. The PPV was 54.92%, and the NPV was 74.74%.
4. Discussion
Increasing patient influx, staff reductions, and demographic trends must lead to further coping measures for Eds. Automation processes will not eliminate professional medical skills, hands-on or complex diagnostics, nor will they lead to a reduction in medical staff tasks. Our suspicion that Eds are overloaded with patients without significant injuries seems to be confirmed, as only 35.21% of patients actually had a fracture. Excluding missed fractures and soft tissue injuries such as ligament tears, a high percentage of patients are still likely to be left with nothing but pain and temporary functional limitations.
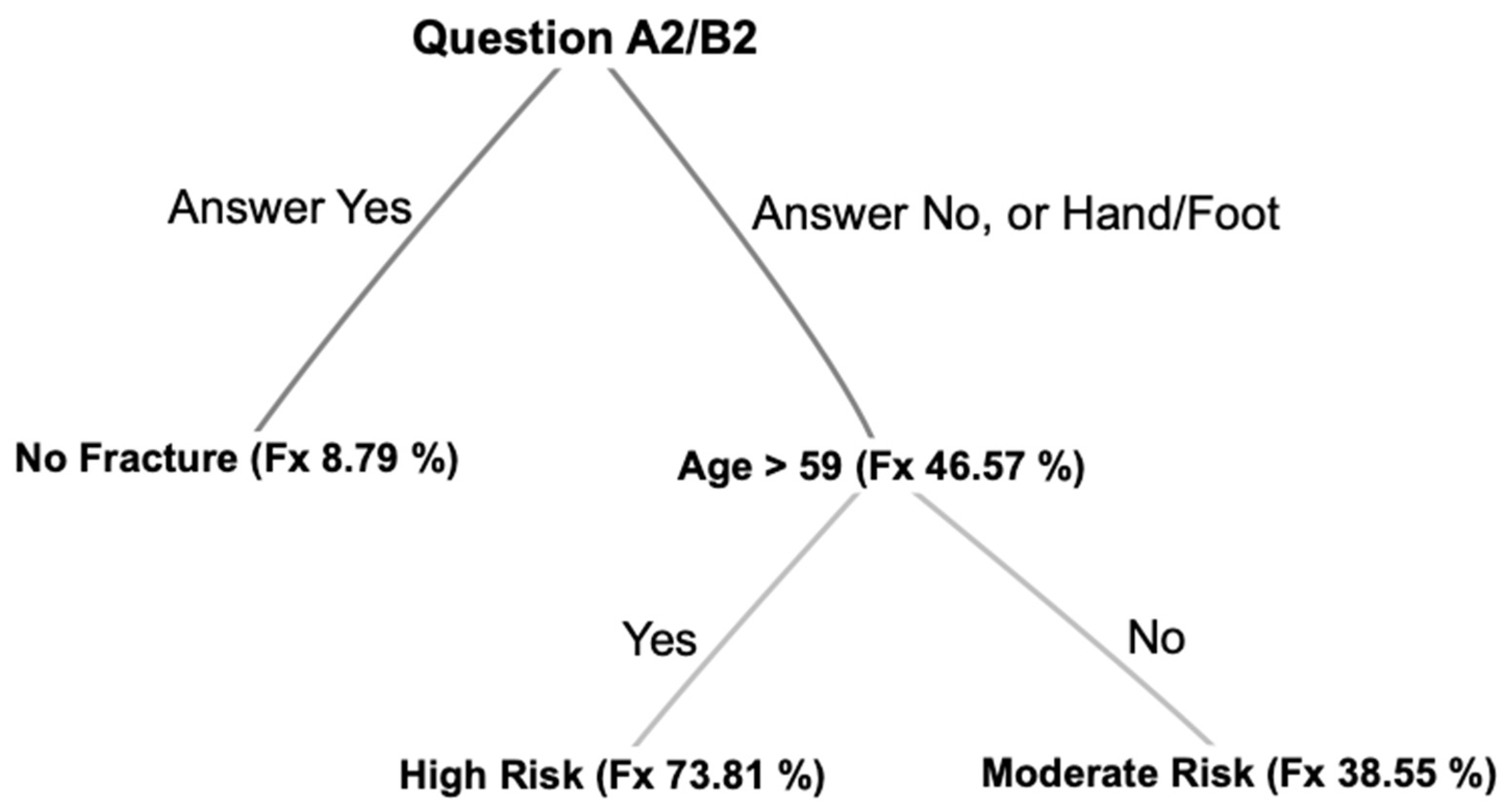
We found two objective and one subjective factor that can be used to detect fractures in the ED: the anatomic region of injury, the age of the patient, and the response to functional questions.
4.1. Objective Factors
Region/Age
The most frequently injured region was the ankle, hand, and foot. The highest fracture risk was at the hip and wrist, and the lowest was at the ankle and knee. Due to the frequent injury at the ankle with low fracture risk, the Ottawa ankle rules already tried to narrow down the radiographic diagnosis [
13].
While patients with hip injuries were comparatively the oldest, those with ankle and knee injuries were young. Although most patients coming into the ED are younger than 50 years, the risk of fracture is significantly higher in older patients, especially for hip fractures. Age above 59 years seems to be a very good predictor for fracture in the ED. It is not possible to say whether the factor “age” or “region” is more important. The hip has the highest fracture risk and represents the oldest patient subgroup (age > 59 years); the wrist has the second highest risk, but the age at risk is 30 years younger. Nevertheless, in the subgroup analysis of each region, the percentage of fractures increased with age. Lack of coordination due to mental degeneration and sarcopenia combined with osteoporosis, altered medication, and malnutrition are known factors that lead to falls and higher fracture rates among older adults [
14,
15,
16]. The data appear to confirm the demographics of orthopaedic trauma patients [
17]. These findings speak to the need for fall prevention programs, as falls are often the first symptom in older people who are no longer able to manage their daily lives on their own.
4.2. Subjective Factors
4.2.1. Questions
Functional questions have shown by their high sensitivity that they are a suitable tool to exclude a fracture. This was true for both UE and LE. However, the sensitivity was lower in comparison for both hand and foot injuries. It is well known that fractures of the hand or foot are most likely to be missed. Two classic examples, in particular, are cited in the literature: the scaphoid bone in the hand and the Lisfranc joint in the foot [
18]. These are often not clearly identified in radiography. Due to the mild symptoms associated with these injuries, further diagnosis by computed tomography or magnetic resonance imaging is often not initially initiated. Therefore, we have attempted to integrate these injuries into the functional questions by including the hand with a twisting maneuver (A2) and the foot with walking on the toes (B2). Among the functional questions, questions A2 and B2 had the highest sensitivity. Although the questions were intended primarily to detect hand and foot injuries, sensitivity increased when these were excluded. Thus, a sensitivity of 100% was shown for the wrist as well as at the LE for the hip, ankle, and knee. An NPV of 100% shows that questions related to a corresponding body region can almost exclude a fracture.
4.2.2. VAS
The recorded VAS score showed a normal distribution. The pain perception of the patient with and without fracture showed no clear differences. Our primary assumption that a fracture was more painful could not be confirmed by the data. The reasons for this are manifold. Non-displaced fractures could cause less pain intensity than displaced fractures. Further cofactors could be stress, anxiety, sociocultural background, or even assessment of faster treatment in the emergency department [
19,
20,
21]. However, the frequency of fractures increased with higher scores, but the curve was flat; for VAS scores < 3 and VAS scores > 8, the number of patients was too small to draw a conclusion. In conclusion, VAS does not appear to be a reliable indicator of fracture detection. Thus, VAS should be critically questioned as a triage tool in EDs. Its reliability in elderly patients has already been questioned [
22].
The onset of pain was assessed because we assumed that a fracture causes immediate pain because of tears in the tissues, whereas a sprain causes an inflammatory response that leads to a delay in symptoms. However, this assumption could not be confirmed by the data, as again no correlation was found between the onset of pain and a fracture.
The purpose of this work was to determine objective and subjective data indicative of a fracture. The three factors of the region, age, and functional issues can be used for decision-making processes and algorithms as shown in
Figure 3. We propose a probatory heuristic that needs to be tested in a prospective procedure. In addition, the questions and pathways need to be further adapted.
Such a heuristic is consistent with the evolution of modern medicine, as tasks are transferred from physicians to nurses, who are becoming highly specialized in health care, and earlier tasks are transferred from nurses to nonphysician staff [
23,
24]. Time management is critical for physicians who are responsible for many tasks, such as in the ED, documentation, or the operating room [
25].
The formulation of the functional questions comes from the experience of physicians in the emergency department. This was intended to take advantage of physicians’ experience, as an intuitive triage system has been shown to be equivalent to conventional ones [
26].
4.3. Limitations
It is problematic to generalize these findings for every ED, but the results may demonstrate the principle that in a given setting, factors can lead to diagnoses. The current design of the study only includes bony injuries, so severe ligamentous injuries must be considered separately. In other countries or hospitals, the regions and the age would certainly be different. The functional questions, on the other hand, could still be appropriate for other places. This means that subjective factors are more robust and versatile than objective factors.
5. Conclusions
The hip and wrist should raise high suspicion for fractures, while the ankle and knee have a low risk. Hand and foot injuries are easily overlooked.
For medical staff in EDs, older patients should be prioritized, and diagnostics should be achieved quickly because their fracture risk is high. The factor “age” should be respected in any orthopedic trauma triage model. Functional questions can be used specifically to virtually rule out fractures. These data suggest that transferring physician knowledge to an algorithm-based computer program can help optimize the emergency department workflow.
Author Contributions
Conceptualization, F.W., S.T., T.L. and C.D.; Methodology, F.W., T.L., T.M. and V.H.; Software, F.M.H.; Formal analysis, F.W., S.T., T.L. and V.H.; Investigation, F.W., F.M.H., S.T., T.M. and C.D.; Resources, T.L. and V.H.; Data curation, F.M.H. and T.M.; Writing—original draft, F.W., C.D. and V.H.; Writing—review & editing, F.M.H., S.T., T.L., T.M. and C.D.; Visualization, F.M.H., C.D. and V.H.; Supervision, F.W., S.T. and T.M.; Project administration, F.W., S.T. and C.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. It was reviewed and approved by the Charité Ethics Committee, Berlin, Germay (Protocol Number: EA2/142/14).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Questionnaire
These questions were asked on the questionnaires:
Do you think that you have a broken bone?
When was the onset of pain?
- ○
Immediately
- ○
After 10 minutes
- ○
After hours
- ○
The next day
Mark your pain now, at rest, on the scale (VAS).
In case of an injury to the upper extremity (questions A1 and A2): Yes or no.
- ○
In that moment, were you able to take a bottle of water out of a cupboard with the injured arm? (A1)
- ○
In that moment, were you able to untwist a bottle of water with the injured arm? (A2)
In case of an injury to the lower extremity (questions B1 and B2): Yes or no.
- ○
In that moment, were you able to walk and take four steps without any help, even if there was limping? (B1)
- ○
In that moment, were you able to walk and take a few steps on your toes? (B2)
Mark the region of your injury (on a diagram of the human body).
How old are you?
References
- Brasseur, E.; Gilbert, A.; Servotte, J.-C.; Donneau, A.-F.; D’Orio, V.; Ghuysen, A. Emergency Department Crowding: Why Do Patients Walk-In? Acta Clin. Belg. 2021, 76, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Frank, C.; Elmqvist, C. Staff Strategies for Dealing with Care Situations at an Emergency Department. Scand. J. Caring Sci. 2020, 34, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- Mirhaghi, A.; Mazlom, R.; Heydari, A.; Ebrahimi, M. The Reliability of the Manchester Triage System (MTS): A Meta-Analysis: The Reliability of the MTS. J. Evid. Based Med. 2017, 10, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Ming, T.; Lai, A.; Lau, P. Can Team Triage Improve Patient Flow in the Emergency Department? A Systematic Review and Meta-Analysis. Adv. Emerg. Nurs. J. 2016, 38, 233–250. [Google Scholar] [CrossRef]
- Arya, R.; Wei, G.; McCoy, J.V.; Crane, J.; Ohman-Strickland, P.; Eisenstein, R.M. Decreasing Length of Stay in the Emergency Department With a Split Emergency Severity Index 3 Patient Flow Model. Acad. Emerg. Med. 2013, 20, 1171–1179. [Google Scholar] [CrossRef]
- Oredsson, S.; Jonsson, H.; Rognes, J.; Lind, L.; Göransson, K.E.; Ehrenberg, A.; Asplund, K.; Castrén, M.; Farrohknia, N. A Systematic Review of Triage-Related Interventions to Improve Patient Flow in Emergency Departments. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 43. [Google Scholar] [CrossRef]
- Ruffing, T.; Danko, T.; Weiss, C.; Winkler, H.; Muhm, M. Treatment duration of trauma and orthopedic patients in an emergency department. Chirurg 2014, 85, 904–910. [Google Scholar] [CrossRef]
- Stribling, J.C.; Richardson, J.E. Placing Wireless Tablets in Clinical Settings for Patient Education. JMLA 2016, 104, 159–164. [Google Scholar] [CrossRef]
- Yordanov, Y.; Chouihed, T.; Riou, B.; Boursin, P. Task Shifting and Emergency Nurse Practitioners—Are Nurses the Future of Emergency Medicine?: The French Experience. Eur. J. Emerg. Med. 2020, 27, 9–10. [Google Scholar] [CrossRef]
- Rademacher, N.J.; Cole, G.; Psoter, K.J.; Kelen, G.; Fan, J.W.Z.; Gordon, D.; Razzak, J. Use of Telemedicine to Screen Patients in the Emergency Department: Matched Cohort Study Evaluating Efficiency and Patient Safety of Telemedicine. JMIR Med. Inf. 2019, 7, e11233. [Google Scholar] [CrossRef]
- Lapointe, L.; Lavallee-Bourget, M.-H.; Pichard-Jolicoeur, A.; Turgeon-Pelchat, C.; Fleet, R. Impact of Telemedicine on Diagnosis, Clinical Management and Outcomes in Rural Trauma Patients: A Rapid Review. Can. J. Rural Med. 2020, 25, 31. [Google Scholar] [CrossRef] [PubMed]
- Freyd, M. The Graphic Rating Scale. J. Educ. Psychol. 1923, 14, 83–102. [Google Scholar] [CrossRef]
- Shell, I.G. Decision Rules for the Use of Radiography in Acute Ankle Injuries: Refinement and Prospective Validation. JAMA 1993, 269, 1127. [Google Scholar] [CrossRef]
- Crandall, M.; Duncan, T.; Mallat, A.; Greene, W.; Violano, P.; Christmas, A.B.; Barraco, R. Prevention of Fall-Related Injuries in the Elderly: An Eastern Association for the Surgery of Trauma Practice Management Guideline. J. Trauma Acute Care Surg. 2016, 81, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Himes, J.H. Nutrition, Bone Mass, and Subsequent Risk of Hip Fracture in White Women. Am. J. Hum. Biol. 1998, 10, 661–667. [Google Scholar] [CrossRef]
- Milos, V.; Bondesson, Å.; Magnusson, M.; Jakobsson, U.; Westerlund, T.; Midlöv, P. Fall Risk-Increasing Drugs and Falls: A Cross-Sectional Study among Elderly Patients in Primary Care. BMC Geriatr. 2014, 14, 40. [Google Scholar] [CrossRef]
- Peterson, B.E.; Jiwanlal, A.; Della Rocca, G.J.; Crist, B.D. Orthopedic Trauma and Aging: It Isn’t Just About Mortality. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 33–36. [Google Scholar] [CrossRef]
- Pinto, A.; Berritto, D.; Russo, A.; Riccitiello, F.; Caruso, M.; Belfiore, M.P.; Papapietro, V.R.; Carotti, M.; Pinto, F.; Giovagnoni, A.; et al. Traumatic Fractures in Adults: Missed Diagnosis on Plain Radiographs in the Emergency Department. Acta Biomed. Atenei Parm. 2018, 89, 111–123. [Google Scholar] [CrossRef]
- Metzger, S.; Poliakov, B.; Lautenbacher, S. Differential Effects of Experimentally Induced Anxiety and Fear on Pain: The Role of Anxiety Sensitivity. JPR 2019, 12, 1791–1801. [Google Scholar] [CrossRef]
- Botti, M.; Khaw, D.; Jørgensen, E.B.; Rasmussen, B.; Hunter, S.; Redley, B. Cross-Cultural Examination of the Structure of the Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R). J. Pain 2015, 16, 727–740. [Google Scholar] [CrossRef]
- Geva, N.; Pruessner, J.; Defrin, R. Acute Psychosocial Stress Reduces Pain Modulation Capabilities in Healthy Men. Pain 2014, 155, 2418–2425. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.; Sim, T.; Hughes, J. Pain Assessment of Elderly Patients with Cognitive Impairment in the Emergency Department: Implications for Pain Management—A Narrative Review of Current Practices. Pharmacy 2017, 5, 30. [Google Scholar] [CrossRef] [PubMed]
- Laurant, M.; van der Biezen, M.; Wijers, N.; Watananirun, K.; Kontopantelis, E.; van Vught, A.J. Nurses as Substitutes for Doctors in Primary Care. Cochrane Database Syst. Rev. 2018, 2019, CD001271. [Google Scholar] [CrossRef] [PubMed]
- Roche, T.E.; Gardner, G.; Jack, L. The Effectiveness of Emergency Nurse Practitioner Service in the Management of Patients Presenting to Rural Hospitals with Chest Pain: A Multisite Prospective Longitudinal Nested Cohort Study. BMC Health Serv. Res. 2017, 17, 445. [Google Scholar] [CrossRef]
- Jagsi, R.; Surender, R. Regulation of Junior Doctors’ Work Hours: An Analysis of British and American Doctors’ Experiences and Attitudes. Soc. Sci. Med. 2004, 58, 2181–2191. [Google Scholar] [CrossRef]
- Hart, A.; Nammour, E.; Mangolds, V.; Broach, J. Intuitive versus Algorithmic Triage. Prehosp. Disaster Med. 2018, 33, 355–361. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).