Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Survey Instrument, and Study Population
2.2. Outcome Variables
2.3. Demographics
2.4. Pandemic Indicator and Time Variables
2.5. Statistical Analysis
2.6. Identifying Priority Occupation Groups
2.7. Ethical Considerations
3. Results
3.1. Study Population
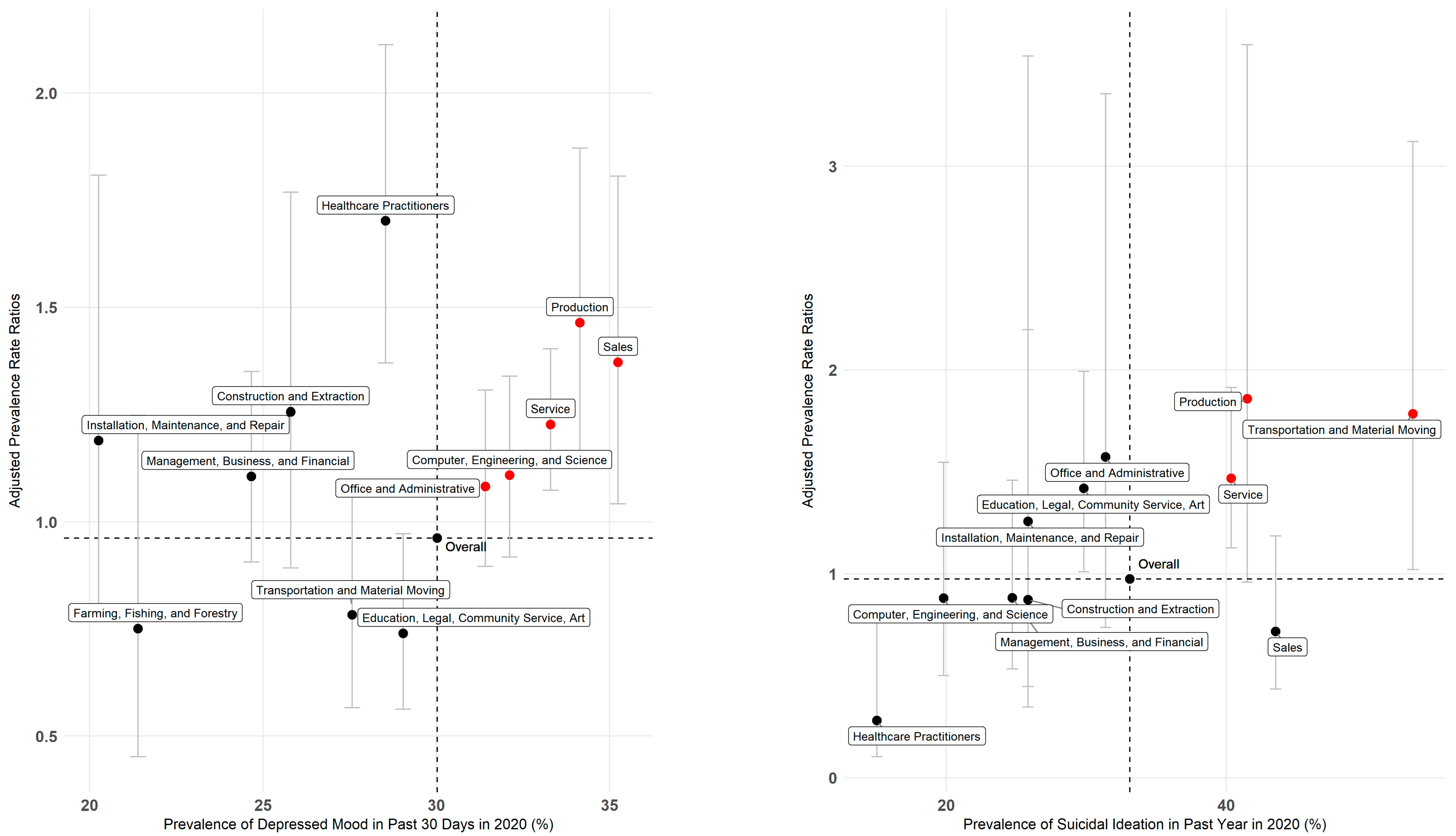
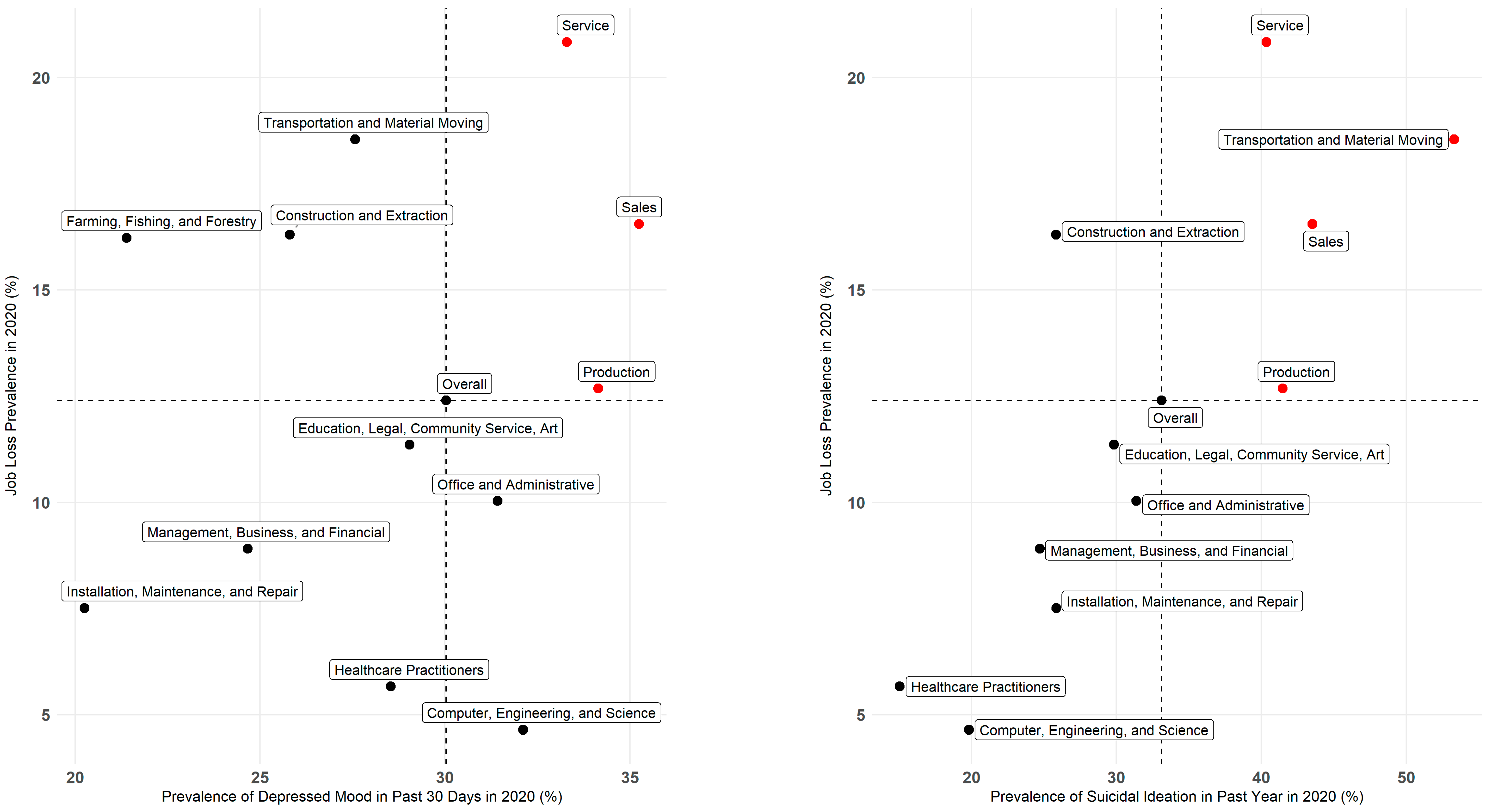
3.2. Depressed Mood
3.3. Suicidal Ideation
3.4. Other High-Risk Worker Groups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Czeisler, M.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, 24–30 June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef] [PubMed]
- Wilkialis, L.; Rodrigues, N.B.; Cha, D.S.; Siegel, A.; Majeed, A.; Lui, L.M.W.; Tamura, J.K.; Gill, B.; Teopiz, K.; McIntyre, R.S. Social Isolation, Loneliness and Generalized Anxiety: Implications and Associations during the COVID-19 Quarantine. Brain Sci. 2021, 11, 1620. [Google Scholar] [CrossRef] [PubMed]
- Stack, S.; Rockett, I.R.H. Social distancing predicts suicide rates: Analysis of the 1918 flu pandemic in 43 large cities, research note. Suicide Life Threat. Behav. 2021, 51, 833–835. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Liu, S.; Li, G.; Lu, Y.; Wu, Y.; Ding, Y.; Ke, C. Role of depressive symptoms in cardiometabolic diseases and subsequent transitions to all-cause mortality: An application of multistate models in a prospective cohort study. Stroke Vasc. Neurol. 2021, 6, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; Ames, M.; Cui, L.; Stang, P.E.; Ustun, T.B.; Von Korff, M.; Kessler, R.C. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Arch. Gen. Psychiatry 2007, 64, 1180–1188. [Google Scholar] [CrossRef]
- Kessler, R.C.; Akiskal, H.S.; Ames, M.; Birnbaum, H.; Greenberg, P.; Hirschfeld, R.M.A.; Jin, R.; Merikangas, K.R.; Simon, G.E.; Wang, P.S. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am. J. Psychiatry 2006, 163, 1561–1568. [Google Scholar] [CrossRef]
- Whooley, M.A.; Kiefe, C.I.; Chesney, M.A.; Markovitz, J.H.; Matthews, K.; Hulley, S.B. Depressive symptoms, unemployment, and loss of income: The CARDIA Study. Arch. Intern. Med. 2002, 162, 2614–2620. [Google Scholar] [CrossRef]
- Abrams, L.R.; Finlay, J.M.; Kobayashi, L.C. Job transitions and mental health outcomes among US adults aged 55 and older during the COVID-19 pandemic. J. Gerontol. Psychol. Sci. Soc. Sci. 2021, 77, e106–e116. [Google Scholar] [CrossRef]
- Burgard, S.A.; Brand, J.E.; House, J.S. Toward a Better Estimation of the Effect of Job Loss on Health. J. Health Soc. Behav. 2007, 48, 369–384. [Google Scholar] [CrossRef]
- Prasad, K.; McLoughlin, C.; Stillman, M.; Poplau, S.; Goelz, E.; Taylor, S.; Nankivil, N.; Brown, R.; Linzer, M.; Cappelucci, K.; et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine 2021, 35, 100879. [Google Scholar] [CrossRef]
- Benhamou, K.; Piedra, A. CBT-Informed Interventions for Essential Workers During the COVID-19 Pandemic. J. Contemp. Psychother. 2020, 50, 275–283. [Google Scholar] [CrossRef]
- Panchal, N.; Kamal, R.; Cox, C.; Garfield, R. The Implications of COVID-19 for Mental Health and Substance Use; Kaiser Family Foundation: San Francisco, CA, USA, 2021; Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ (accessed on 29 April 2022).
- Coe, E.; Enomoto, K.; Herbig, B.; Kothari, A.; Stueland, J. COVID-19 and Burnout Are Straining the Mental Health of Employed Parents. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/covid-19-and-burnout-are-straining-the-mental-health-of-employed-parents (accessed on 3 June 2022).
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Cree, R.A.; Okoro, C.A.; Zack, M.M.; Carbone, E. Frequent Mental Distress Among Adults, by Disability Status, Disability Type, and Selected Characteristics—United States, 2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1238–1243. [Google Scholar] [CrossRef]
- California Health Interview Survey. CHIS Methodology Documentation. 2022. Available online: https://healthpolicy.ucla.edu/chis/design/pages/methodology.aspx (accessed on 23 May 2022).
- NIOSH. NIOSH Industry and Occupation Computerized Coding System (NIOCCS). 2021. Available online: https://csams.cdc.gov/nioccs/Default.aspx (accessed on 29 April 2022).
- Ponce, N.A.; Paycao, D.; Wells, B.M.; Park, R.; Hughes, T. COVID-19 Rapid Response: How the California Health Interview Survey Adapted During the Global Pandemic. Am. J. Public Health 2021, 111, 2122–2126. [Google Scholar] [CrossRef]
- Gardner, W.; Mulvey, E.P.; Shaw, E.C. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol. Bull. 1995, 118, 392–404. [Google Scholar] [CrossRef]
- Lumley, T. Package ‘Survey’. 2021. Available online: https://cran.r-project.org/web/packages/survey/survey.pdf (accessed on 29 April 2022).
- Hammonds, C.; Kerriseey, J. We Are not Heroes Because It Is not a Choice: A Survey of Essential Workers’ Safety and Security during COVID-19; University of Massachusetts Amherst Labor Center: Amherst, MA, USA, 2020. [Google Scholar]
- Heinzerling, A.; Nguyen, A.; Frederick, M.; Chan, E.; Gibb, K.; Rodriguez, A.; Wong, J.; Epson, E.; Watt, J.; Materna, B.; et al. Workplaces Most Affected by COVID-19 Outbreaks in California, January 2020–August 2021. Am. J. Public Health 2022, 112, 1180–1190. [Google Scholar] [CrossRef]
- Cummings, K.J.; Beckman, J.; Frederick, M.; Harrison, R.; Nguyen, A.; Snyder, R.; Chan, E.; Gibb, K.; Rodriguez, A.; Wong, J.; et al. Disparities in COVID-19 fatalities among working Californians. PLoS ONE 2022, 17, e0266058. [Google Scholar] [CrossRef]
- Kniffin, K.M.; Narayanan, J.; Anseel, F.; Antonakis, J.; Ashford, S.P.; Bakker, A.B.; Bamberger, P.; Bapuji, H.; Bhave, D.P.; Choi, V.K.; et al. COVID-19 and the workplace: Implications, issues, and insights for future research and action. Am. Psychol. 2021, 76, 63–77. [Google Scholar] [CrossRef]
- Koma, W.; True, S.; Biniek, J.F.; Cubanski, J.; Orgera, K.; Garfield, R. One in Four Older Adults Report Anxiety or Depression Amid the COVID-19 Pandemic. 2020. Available online: https://www.kff.org/medicare/issue-brief/one-in-four-older-adults-report-anxiety-or-depression-amid-the-covid-19-pandemic/ (accessed on 3 June 2022).
- Parcesepe, A.M.; Cabassa, L.J. Public stigma of mental illness in the United States: A systematic literature review. Adm. Policy Ment. Health 2013, 40, 384–399. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, A.; Nazem, S.; Fiske, A.; Nadorff, M.R.; Smith, M.D. Self-concealment and suicidal behaviors. Suicide Life-Threat. Behav. 2012, 42, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Workplace Health Promotion: Programs|Depression Interventions. Available online: https://www.cdc.gov/workplacehealthpromotion/health-strategies/depression/interventions/programs.html (accessed on 23 May 2022).
- Goordin, A.; Frank, R.; Glied, S. Addressing Mental Illness Requires Workplace Policy as Well as Health Care Policy; Health Affairs: Washington, DC, USA, 2021; Available online: https://www.healthaffairs.org/do/10.1377/forefront.20210615.243332/full/ (accessed on 6 June 2022).
| Study Population | 2020 | |
|---|---|---|
| Workers | Nonworkers | |
| Weighted % (CI) | Weighted % (CI) | |
| Unweighted N | 12,982 | 8967 |
| Weighted N (CI), millions | 19.7 (19, 20) | 10 (10, 10) |
| Age, years | ||
| 18–29 | 22.5 (22, 23) | 18.7 (17.6, 19.8) |
| 30–44 | 33.9 (33.4, 34.5) | 10.7 (9.7, 11.7) |
| 45–64 | 36.8 (36.2, 37.5) | 21.7 (20.6, 22.8) |
| 65+ | 6.7 (6.3, 7.1) | 48.9 (47.6, 50.2) |
| Sex | ||
| Male | 52.8 (52.2, 53.4) | 41.8 (40.6, 43) |
| Female | 47.2 (46.6, 47.8) | 58.2 (57, 59.4) |
| Race/Ethnicity | ||
| Hispanic/Latino | 41.8 (41, 42.5) | 34.3 (32.8, 35.8) |
| White, NH | 35.6 (35, 36.1) | 43.9 (42.7, 45.2) |
| Black, NH | 5.2 (4.8, 5.6) | 6.1 (5.3, 6.8) |
| Asian, NH | 13.7 (13.2, 14.2) | 12.5 (11.5, 13.6) |
| AI/AN, NH/PI, 2+, NH | 3.8 (3.5, 4.1) | 3.1 (2.5, 3.7) |
| Annual household income, $ | ||
| <20,000 | 9.4 (8.5, 10.2) | 20.1 (18.7, 21.5) |
| 20,000–39,999 | 13.7 (12.7, 14.8) | 22.4 (20.8, 24) |
| 40,000–74,999 | 21.7 (20.5, 22.9) | 22.6 (21.4, 23.8) |
| 75,000–99,999 | 12.5 (11.6, 13.4) | 10.5 (9.5, 11.6) |
| 100,000–129,999 | 13.5 (12.6, 14.4) | 9.9 (8.9, 11) |
| 130,000+ | 29.2 (28.3, 30) | 14.5 (13.4, 15.5) |
| Disability | ||
| Blind/deaf or has severe vision/hearing problem | 3.4 (2.9, 4) | 10.7 (9.7, 11.7) |
| Difficulty concentrating (2019–2020 only) | 7.4 (6.8, 8.1) | 12.4 (11.2, 13.6) |
| Difficulty dressing or bathing (2019–2020 only) | 0.6 (0.4, 0.9) | 5.5 (4.6, 6.3) |
| Difficulty doing errands alone (2019–2020 only) | 2.6 (2.1, 3) | 11.2 (10.2, 12.3) |
| Any of the above disabilities | 11.6 (10.7, 12.5) | 26.6 (25.1, 28.1) |
| Main Occupation (2010 Census Codes) | ||
| Management, business, and financial | 14.4 (13.5, 15.3) | |
| Computer, engineering, and science | 10.6 (9.9, 11.3) | |
| Education, legal, community service, arts, and media | 13.3 (12.5, 14) | |
| Healthcare practitioners and technical | 5.1 (4.6, 5.6) | |
| Service | 16.6 (15.3, 17.8) | |
| Sales and related | 7.6 (6.9, 8.2) | |
| Office and administrative support | 11.9 (11.1, 12.7) | |
| Farming, fishing, and forestry | 0.9 (0.6, 1.2) | |
| Construction and extraction | 3.7 (3, 4.3) | |
| Installation, maintenance, and repair | 2.5 (1.9, 3) | |
| Production | 4.8 (4.1, 5.5) | |
| Transportation and material moving | 5.5 (4.9, 6.1) | |
| Depressed Mood All, Most, Some, or a Little of the Time in the Past 30 Days | Suicidal Ideation in the Past Year among Workers Who Have Ever Thought of Suicide | |||||||
|---|---|---|---|---|---|---|---|---|
| Prevalence in 2019, % (95% CI) | Absolute Change in Prevalence from 2019 to 2020, % (95% CI) | Trend Adjusted Prevalence Ratio, PR (CI) | Model Type | Prevalence in 2019, % (95% CI) | Absolute Change in Prevalence from 2019 to 2020, % (95% CI) | Trend Adjusted Prevalence Ratio, PR (CI) | Model Type | |
| All Workers | 27.23 (25.9, 28.6) | 2.80 (1.1, 4.5) | 0.96 (0.9, 1.1) | ††† | 31.41 (27.7, 35.3) | 1.71 (−3.5, 7.0) | 0.98 (0.8, 1.2) | †† |
| Age | ||||||||
| 18–29 | 37.59 (34.2, 41.1) | 5.40 (1.1, 9.8) | 1.06 (0.9, 1.2) | †† | 38.44 (31.1, 46.2) | 9.62 (0.2, 19.0) | 1.08 (0.9, 1.3) | †† |
| 30–44 | 29.77 (27.8, 31.8) | −0.04 (−2.8, 2.7) | 0.81 (0.7, 0.9) | ††† | 29.94 (24.1, 36.3) | −4.37 (−11.8, 3.1) | 0.82 (0.6, 1.1) | †† |
| 45–64 | 19.78 (18.2, 21.5) | 4.86 (2.5, 7.2) | 1.39 (1.3, 1.5) | † | 23.75 (19.7, 28.2) | −0.78 (−7.9, 6.3) | 1.31 (1.0, 1.8) | † |
| 65+ | 16.22 (13.3, 19.5) | 1.40 (−3.0, 5.8) | 1.09 (0.8, 1.5) | †† | 12.15 (6.4, 20.3) | 7.41 (−5.0, 19.8) | 1.65 (0.8, 3.5) | † |
| Sex | ||||||||
| Male | 24.42 (22.7, 26.2) | 2.80 (0.4, 5.2) | 1.09 (1.0, 1.2) | †† | 31.83 (26.4, 37.7) | 3.69 (−4.5, 11.9) | 1.03 (0.8, 1.3) | †† |
| Female | 30.47 (28.6, 32.4) | 2.70 (0.2, 5.2) | 0.91 (0.8, 1.1) | ††† | 31.01 (26.3, 36.1) | −0.29 (−7.1, 6.5) | 0.92 (0.7, 1.2) | †† |
| Race/Ethnicity | ||||||||
| Hispanic/Latino | 27.78 (25.4, 30.3) | 4.48 (1.2, 7.7) | 1.00 (0.9, 1.2) | ††† | 35.03 (28.3, 42.3) | 5.37 (−4.1, 14.8) | 1.14 (0.9, 1.5) | †† |
| White, NH | 25.03 (23.5, 26.6) | 3.04 (0.9, 5.1) | 0.97 (0.8, 1.2) | ††† | 28.45 (24.4, 32.8) | −0.48 (−6.7, 5.7) | 0.95 (0.7, 1.2) | †† |
| Black, NH | 23.78 (19.4, 28.6) | −1.28 (−7.9, 5.3) | 0.88 (0.6, 1.2) | †† | 25.23 (12.8, 41.5) | 10.55 (−15.8, 36.9) | 1.31 (0.6, 2.6) | † |
| Asian, NH | 31.78 (28.7, 35.0) | −0.71 (−4.9, 3.5) | 0.99 (0.8, 1.2) | †† | 45.64 (25.4, 56.2) | −16.09 (−30.5, −1.7) | 0.52 (0.3, 0.8) | †† |
| AI/AN, NH/PI, 2+, NH | 29.68 (22.9, 37.2) | 0.59 (−9.0, 10.2) | 0.91 (0.7, 1.3) | †† | 14.41 (5.3, 29.3) | 12.51 (−4.5, 29.6) | 1.47 (0.8, 2.8) | † |
| Annual household income | ||||||||
| <20,000 | 36.06 (31.3, 41.0) | 2.53 (−4.1, 9.1) | 1.05 (0.9, 1.3) | †† | 48.62 (33.1, 64.3) | −5.69 (−25.5, 14.1) | 0.82 (0.5, 1.3) | †† |
| 20,000–39,999 | 36.58 (33.0, 40.3) | 3.25 (−2.0, 8.5) | 0.93 (0.7, 1.2) | ††† | 38.41 (28.6, 48.9) | 4.85 (−8.5, 18.2) | 1.48 (1.1, 1.9) | † |
| 40,000–74,999 | 27.59 (25.0, 30.3) | 3.80 (0.1, 7.5) | 1.01 (0.9, 1.2) | †† | 31.28 (23.1, 40.4) | 7.61 (−3.9, 19.1) | 1.11 (0.8, 1.6) | †† |
| 75,000–99,999 | 25.45 (21.9, 29.3) | 2.51 (−2.2, 7.2) | 1.11 (0.9, 1.4) | †† | 31.43 (22.1, 42.0) | −2.56, (−16.1, 11.0) | 1.27 (0.8, 1.9) | † |
| 100,000–129,999 | 25.73 (22.5, 29.2) | 2.63 (−1.8, 7.0) | 1.04 (0.9, 1.3) | †† | 33.57 (23.8, 44.5) | −9.95 (−22.5, 2.5) | 0.68 (0.4, 1.1) | †† |
| 130,000+ | 20.48 (18.5, 22.6) | 2.84 (0.1, 5.5) | 1.21 (1.0, 1.4) | †† | 18.86 (13.8, 24.8) | 6.15 (−2.5, 14.8) | 2.14 (0.9, 5.2) | ††† |
| Disability | ||||||||
| Blind/deaf or has severe vision/hearing problem | ||||||||
| Yes | 37.91 (30.2, 46.1) | 1.23 (−10.8, 13.3) | 0.96 (0.7, 1.3) | †† | 47.53 (29.1, 66.5) | −27.91 (−51.3, −4.5) | 0.58 (0.3, 1.3) | † |
| No | 26.88 (25.5, 28.2) | 2.82 (1.1, 4.6) | 0.95 (0.9, 1.1) | ††† | 30.90 (27.3, 34.7) | 2.65 (−2.6, 7.9) | 1.02 (0.9, 1.2) | †† |
| Difficulty concentrating (2019 and later) | ||||||||
| Yes | 71.32 (64.8, 77.3) | −1.30 (−8.9, 6.3) | … | … | 50.87 (41.9, 59.8) | −1.53 (−12.8, 9.7) | … | … |
| No | 24.34 (23.0, 25.7) | 2.47 (0.7, 4.2) | … | … | 27.26 (23.3, 31.5) | 0.40 (−5.4, 6.2) | … | … |
| Difficulty dressing or bathing (2019 and later) | ||||||||
| Yes | 61.68 (42.4, 78.6) | 4.37 (−19.0, 27.8) | … | … | 57.81 (33.1, 80.0) | 2.08 (−32.8, 36.9) | … | … |
| No | 26.94 (25.6, 28.3) | 2.86 (1.1, 4.6) | … | … | 30.83 (27.1, 34.7) | 1.62 (−3.6, 6.8) | … | … |
| Difficulty doing errands alone (2019 and later) | ||||||||
| Yes | 61.86 (52.8, 70.4) | 3.95 (−8.4, 16.3) | … | … | 50.26 (38.5, 62.0) | 1.55 (−15.2, 18.3) | … | … |
| No | 26.26 (24.9, 27.6) | 2.84 (1.1, 4.6) | … | … | 30.05 (26.2, 34.1) | 1.26 (−4.3, 6.8) | … | … |
| Any of the above disabilities | 57.53 (52.5, 62.4) | 1.42 (−4.8, 7.6) | … | … | 50.48 (42.1, 58.8) | −5.20 (−16.0, 5.7) | … | … |
| Main Occupation (2010 Census Codes) | ||||||||
| Management, business, and financial | 25.39 (22.6, 28.4) | 0.72 (−4.6, 3.1) | 1.11 (0.9, 1.4) | †† | 27.68 (19.6, 37.0) | −2.95 (−14.7, 8.8) | 0.88 (0.5, 1.5) | †† |
| Computer, engineering, and science | 28.47 (24.9, 32.3) | 3.65 (−1.0, 8.3) | 1.11 (0.9, 1.3) | †† | 26.16 (16.8, 37.4) | −6.34 (−18.6, 6.0) | 0.88 (0.5, 1.5) | † |
| Education, legal, community service, arts, and media | 29.08 (25.8, 32.5) | −0.04 (−4.4, 4.4) | 0.74 (0.6, 1.0) | ††† | 21.87 (15.2, 29.8) | 7.95 (−2.5, 18.4) | 1.42 (1.0, 2.0) | † |
| Healthcare practitioners and technical | 21.98 (18.2, 26.1) | 6.56 (0.9, 12.3) | 1.70 (1.4, 2.1) | † | 36.97 (20.5, 56.0) | −21.91 (−42.2, −1.6) | 0.28 (0.1, 0.8) | †† |
| Service | 31.65 (28.1, 35.3) | 1.64 (−3.6, 6.9) | 1.23 (1.1, 1.4) | † | 41.15 (29.9, 53.1) | −0.80 (−14.5, 12.9) | 1.47 (1.1, 1.9) | † |
| Sales and related | 24.15 (20.0, 28.7) | 11.10 (4.3, 17.8) | 1.37 (1.0, 1.8) | †† | 52.84 (37.7, 67.6) | −9.32 (−28.7, 10.1) | 0.72 (0.4, 1.2) | †† |
| Office and administrative support | 27.47 (23.8, 31.4) | 3.95 (−1.0, 8.9) | 1.08 (0.9, 1.3) | †† | 31.69 (22.5, 42.1) | −0.31 (−13.5, 12.9) | 1.57 (0.7, 3.4) | ††† |
| Farming, fishing, and forestry * | 18.86 (9.6, 31.6) | 2.53 (−12.0, 17.1) | 0.75 (0.5, 1.2) | † | … | … | … | † |
| Construction and extraction | 24.22 (15.6, 34.7) | 1.59 (−10.4, 13.6) | 1.26 (0.9, 1.8) | † | 38.48 (10.3, 74.0) | −12.63 (−52.2, 27.0) | 0.87 (0.3, 2.2) | † |
| Installation, maintenance, and repair | 17.69 (9.8, 28.3) | 2.57 (−8.7, 13.8) | 1.19 (0.8, 1.8) | † | 12.90 (1.1, 43.1) | 12.96 (−18.0, 43.9) | 1.26 (0.4, 3.5) | † |
| Production | 19.70 (14.3, 26.1) | 14.44 (5.3, 23.6) | 1.46 (1.1, 1.9) | † | 37.07 (4.2, 83.9) | 4.42 (−44.0, 52.8) | 1.86 (1.0, 3.6) | † |
| Transportation and material moving | 32.85 (24.3, 42.3) | −5.28 (−15.5, 4.9) | 0.78 (0.6, 1.1) | †† | 28.80 (10.3, 54.6) | 24.51 (−6.2, 55.3) | 1.79 (1.0, 3.1) | † |
| Suicidal Ideation in the Past Year among Workers Who Have Ever Thought of Suicide | Depressed Mood All, Most, Some, or a Little of the Time in the Past 30 Days | All Workers | ||||
|---|---|---|---|---|---|---|
| Prevalence in 2020 (%) | (95% CI) | Prevalence in 2020 (%) | (95% CI) | Prevalence in 2020 (%) | (95% CI) | |
| Job Changes | ||||||
| Lost job | 44.81 | (34.7, 55.3) | 38.68 | (34.8, 42.6) | 12.40 | (11.5, 13.3) |
| Did not lose job | 31.11 | (27.0, 35.4) | 28.8 | (27.6, 30.1) | ||
| Reduced hours | 38.10 | (32.0, 44.5) | 35.65 | (33.0, 38.4) | 24.37 | (23.2, 25.6) |
| Did not have reduced hours | 30.94 | (26.5, 35.7) | 28.22 | (27.1, 29.4) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gibb, K.; Bui, D.P.; Vergara, X.P. Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey. Int. J. Environ. Res. Public Health 2023, 20, 1253. https://doi.org/10.3390/ijerph20021253
Gibb K, Bui DP, Vergara XP. Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey. International Journal of Environmental Research and Public Health. 2023; 20(2):1253. https://doi.org/10.3390/ijerph20021253
Chicago/Turabian StyleGibb, Kathryn, David Pham Bui, and Ximena P. Vergara. 2023. "Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey" International Journal of Environmental Research and Public Health 20, no. 2: 1253. https://doi.org/10.3390/ijerph20021253
APA StyleGibb, K., Bui, D. P., & Vergara, X. P. (2023). Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey. International Journal of Environmental Research and Public Health, 20(2), 1253. https://doi.org/10.3390/ijerph20021253






