COVID-19 as an Occupational Disease—Temporal Trends in the Number and Severity of Claims in Germany
Abstract
1. Introduction
2. Materials and Methods
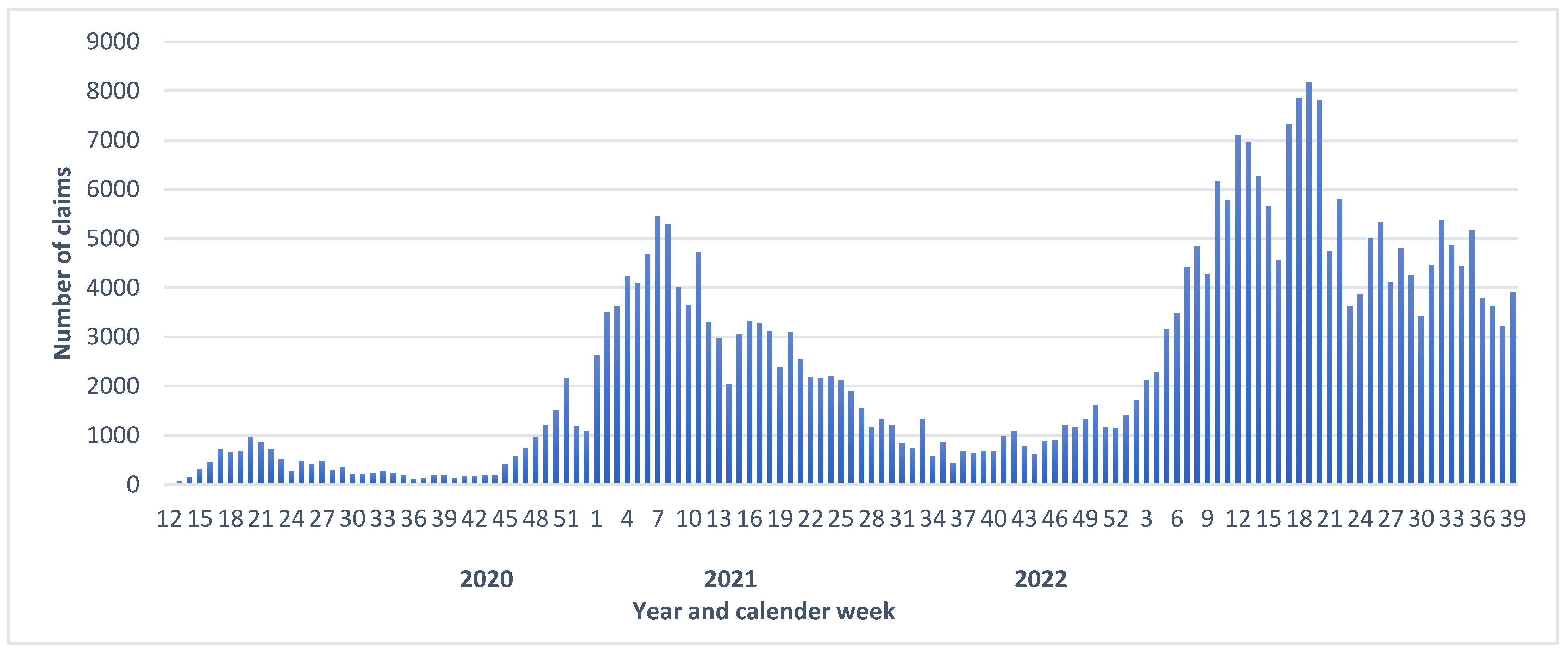
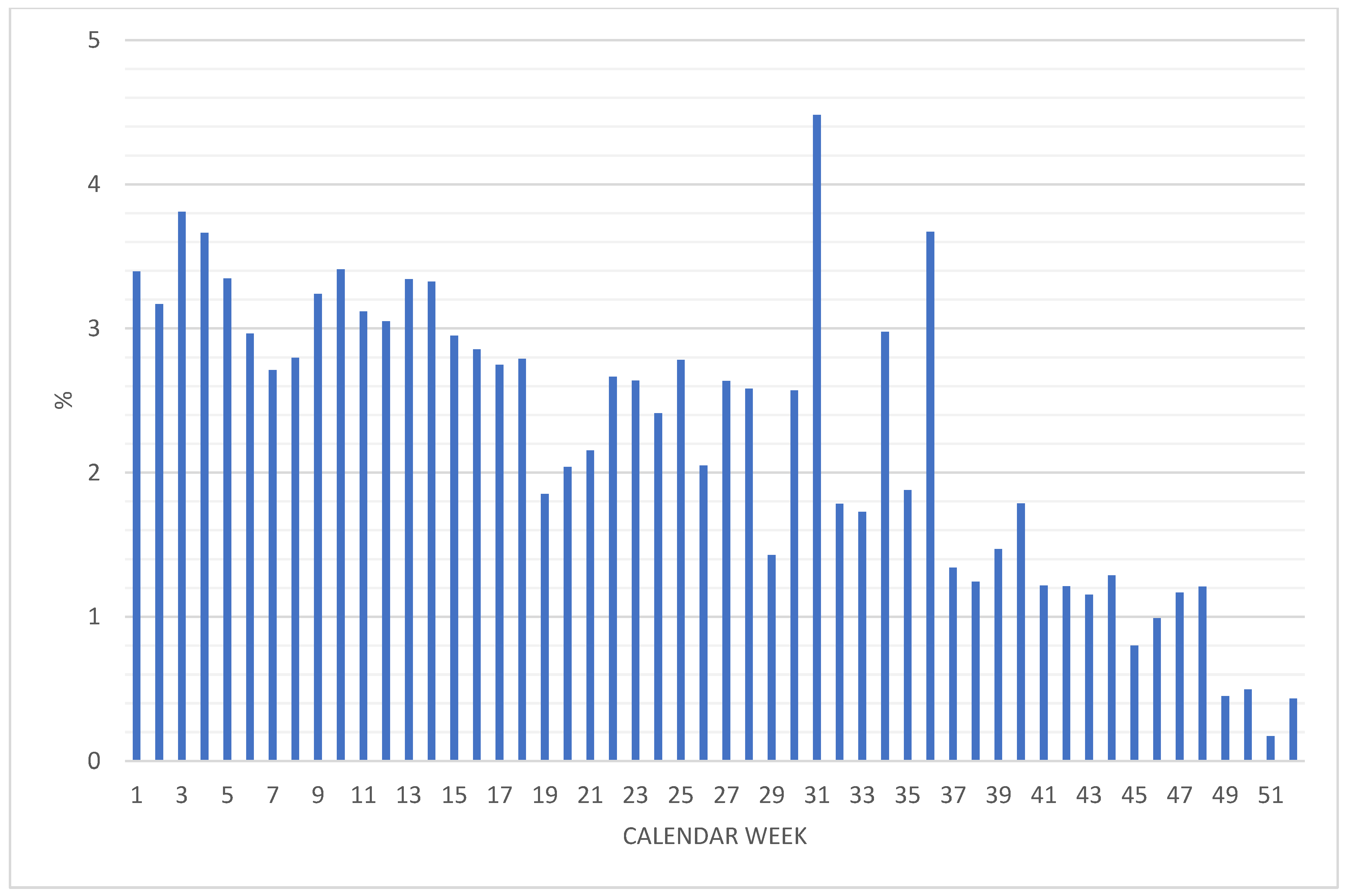
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shah, A.S.V.; Wood, R.; Gribben, C.; Caldwell, D.; Bishop, J.; Weir, A.; Kennedy, S.; Reid, M.; Smith-Palmer, A.; Goldberg, D.; et al. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: Nationwide linkage cohort study. BMJ 2020, 371, m3582. [Google Scholar] [CrossRef] [PubMed]
- Möhner, M.; Wolik, A. Differences in COVID-19 Risk Between Occupational Groups and Employment Sectors in Germany. Dtsch. Ärzteblatt Int. 2020, 117, 641–642. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M. Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am. J. Ind. Med. 2021, 64, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.J.; Lear, S.; Sithole, N.; Shaw, A.; Stark, H.; Ferris, M.; Bradley, J.; Maxwell, P.; Goodfellow, I.; Weekes, M.P.; et al. Demographic, behavioural and occupational risk factors associated with SARS-CoV-2 infection in UK healthcare workers: A retrospective observational study. BMJ Open 2022, 12, e063159. [Google Scholar] [CrossRef] [PubMed]
- Modji, K.K.S.; Morris, C.R.; Creswell, P.D.; McCoy, K.; Aiello, T.; Grajewski, B.; Tomasallo, C.D.; Pray, I.; Meiman, J.G. Lost time: COVID-19 indemnity claim reporting and results in the Wisconsin workers’ compensation system from March 12 to December 31, 2020. Am. J. Ind. Med. 2022, 65, 1006–1021. [Google Scholar] [CrossRef]
- Stüven, P.; Mühlenbruch, G.; Evenschor-Ascheid, A.; Conzen, E.; Peters, C.; Schablon, A.; Nienhaus, A. COVID-19 infections in staff of an emergency care hospital after the first wave of the pandemic in Germany. GMS Hyg. Infect. Control. 2022, 17, Doc04. [Google Scholar] [CrossRef]
- Platten, M.; Nienhaus, A.; Peters, C.; Cranen, R.; Wisplinghoff, H.; Kersten, J.F.; Bach, A.D.; Michels, G. Cumulative Incidence of SARS-CoV-2 in Healthcare Workers at a General Hospital in Germany during the Pandemic—A Longitudinal Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2429. [Google Scholar] [CrossRef]
- Chandan, S.; Khan, S.R.; Deliwala, S.; Mohan, B.P.; Ramai, D.; Chandan, O.C.; Facciorusso, A. Postvaccination SARS-CoV-2 infection among healthcare workers: A Systematic Review and meta-analysis. J. Med. Virol. 2022, 94, 1428–1441. [Google Scholar] [CrossRef]
- Feikin, D.R.; Higdon, M.M.; Abu-Raddad, L.J.; Andrews, N.; Araos, R.; Goldberg, Y.; Groome, M.J.; Huppert, A.; O’Brien, K.L.; Smith, P.G.; et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: Results of a systematic review and meta-regression. Lancet 2022, 399, 924–944. [Google Scholar] [CrossRef]
- Pilishvili, T.; Gierke, R.; Fleming-Dutra, K.E.; Farrar, J.L.; Mohr, N.M.; Talan, D.A.; Krishnadasan, A.; Harland, K.K.; Smithline, H.A.; Hou, P.C.; et al. Effectiveness of mRNA Covid-19 Vaccine among U.S. Health Care Personnel. N. Engl. J. Med. 2001, 385, e90. [Google Scholar] [CrossRef]
- Poukka, E.; Baum, U.; Palmu, A.A.; Lehtonen, T.O.; Salo, H.; Nohynek, H.; Leino, T. Cohort study of Covid-19 vaccine effectiveness among healthcare workers in Finland, December 2020–October 2021. Vaccine 2022, 40, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Havers, F.P.; Pham, H.; Taylor, C.A.; Whitaker, M.; Patel, K.; Anglin, O.; Kambhampati, A.K.; Milucky, J.; Zell, E.; Moline, H.L.; et al. COVID-19-Associated Hospitalizations Among Vaccinated and Unvaccinated Adults 18 Years or Older in 13 US States, January 2021 to April 2022. JAMA Intern. Med. 2022, 182, 1071–1081. [Google Scholar] [CrossRef]
- Bauernfeind, S.; Hitzenbichler, F.; Huppertz, G.; Zeman, F.; Koller, M.; Schmidt, B.; Plentz, A.; Bauswein, M.; Mohr, A.; Salzberger, B. Brief report: Attitudes towards Covid-19 vaccination among hospital employees in a tertiary care university hospital in Germany in December 2020. Infection 2022, 49, 1307–1311. [Google Scholar] [CrossRef] [PubMed]
- Karagiannidis, C.; Spies, C.; Kluge, S.; Marx, G.; Janssens, U. Impfbereitschaft unter intensivmedizinischem Personal: Ängsten entgegenwirken [Willingness to vaccinate among intensive care personnel: Counteracting fears]. Med. Klin. Intensivmed. Notf. 2021, 116, 216–219. [Google Scholar] [CrossRef]
- Kozak, A.; Nienhaus, A. COVID-19 Vaccination: Status and Willingness to Be Vaccinated among Employees in Health and Welfare Care in Germany. Int. J. Environ. Res. Public Health. 2021, 18, 6688. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch Institut (RKI). KROCO—die Krankenhausbasierte Online-Befragung zur COVID-19-Impfung Ergebnisbericht zur Vierten Befragungswelle 15.08.2022 [Hospital Based Survey on COVID-19 Vaccination, Results of the Forth Wave 15.08.2022] KROCO—die Krankenhausbasierte Online-Befragung zur COVID-19-Impfung (rki.de). RKI—Coronavirus SARS-CoV-2—KROCO—Krankenhausbasierte Online-Befragung zur COVID-19-Impfung. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Projekte_RKI/Kroco-Report-2022-08-15.html (accessed on 4 January 2023).
- Nowak, D.; Ochmann, U.; Brandenburg, S.; Nienhaus, A.; Woltjen, M. COVID-19 as an occupational disease or work-related accident: Considerations regarding insurance cover and reporting obligation in the statutory accident insurance. Dtsch. Med. Wochenschr. 2021, 146, 198–204. (In German) [Google Scholar] [CrossRef]
- Nienhaus, A. COVID-19 among Health Workers in Germany—An Update. Int. J. Environ. Res. Public Health 2021, 18, 9185. [Google Scholar] [CrossRef]
- Cherrie, M.; Rhodes, S.; Wilkinson, J.; Mueller, W.; Nafilyan, V.; Van Tongeren, M.; Pearce, N. Longitudinal changes in proportionate mortality due to COVID-19 by occupation in England and Wales. Scand. J. Work Environ. Health 2022, 48, 611–620. [Google Scholar] [CrossRef]
- Flury, B.B.; Güsewell, S.; Egger, T.; Leal, O.; Brucher, A.; Lemmenmeier, E.; Kleeb, D.M.; Möller, J.C.; Rieder, P.; Rütti, M.; et al. Risk and symptoms of COVID-19 in health professionals according to baseline immune status and booster vaccination during the Delta and Omicron waves in Switzerland—A multicentre cohort study. PLoS Med. 2022, 19, e1004125. [Google Scholar] [CrossRef]
- Nienhaus, A.; Hod, R. COVID-19 among Health Workers in Germany and Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 4881. [Google Scholar] [CrossRef]
- Nienhaus, A. Infections in Healthcare Workers in Germany-22-Year Time Trends. Int. J. Environ. Res. Public Health 2018, 26, 2656. [Google Scholar] [CrossRef] [PubMed]
- Neuhauser, H.; Rosario, A.S.; Butschalowsky, H.; Haller, S.; Hoebel, J.; Michel, J.; Nitsche, A.; Poethko-Müller, C.; Prütz, F.; Schlaud, M.; et al. Nationally representative results on SARS-CoV-2 seroprevalence and testing in Germany at the end of 2020. Sci. Rep. 2022, 12, 19492. [Google Scholar] [CrossRef] [PubMed]
- Leiner, J.; Pellissier, V.; Hohenstein, S.; König, S.; Schuler, E.; Möller, R.; Nachtigall, I.; Bonsignore, M.; Hindricks, G.; Kuhlen, R.; et al. Characteristics and outcomes of COVID-19 patients during B.1.1.529 (Omicron) dominance compared to B.1.617.2 (Delta) in 89 German hospitals. BMC Infect. Dis. 2022, 22, 802. [Google Scholar] [CrossRef] [PubMed]
- Drinhaus, H.; Hart, D.; Böttiger, B.W.; Wetsch, W.A. The incidence of SARS-CoV-2 with different hygiene regulations during the carnival periods in 2021 and 2022. Dtsch. Ärztebl. Int. 2022, 119, 759–760. [Google Scholar] [CrossRef]
- Rovida, F.; Cassaniti, I.; Percivalle, E.; Sarasini, A.; Paolucci, S.; Klersy, C.; Cutti, S.; Novelli, V.; Marena, C.; Luzzaro, F.; et al. Incidence of SARS-CoV-2 infection in health care workers from Northern Italy based on antibody status: Immune protection from secondary infection- A retrospective observational case-controlled study. Int. J. Infect. Dis. 2021, 109, 199–202. [Google Scholar] [CrossRef]
- Lumley, S.F.; O’Donnell, D.; Stoesser, N.E.; Matthews, P.C.; Howarth, A.; Hatch, S.B.; Marsden, B.D.; Cox, S.; James, T.; Warren, F.; et al. Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers. N. Engl. J. Med. 2021, 384, 533–540. [Google Scholar] [CrossRef]
- Shah, M.M.; Spencer, B.R.; Feldstein, L.R.; Haynes, J.M.; Benoit, T.J.; Saydah, S.H.; Groenewold, M.R.; Stramer, S.L.; Jones, J.M. Occupations Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Vaccination, US Blood Donors, May 2021–December 2021. Clin. Infect. Dis, 2022; ciac883, ahead of print. [Google Scholar] [CrossRef]
- Consonni, D.; Lombardi, A.; Mangioni, D.; Bono, P.; Oggioni, M.; Uceda Renteria, S.; Valzano, A.; Bordini, L.; Nava, C.D.; Tiwana, N.; et al. Immunogenicity and effectiveness of BNT162b2 COVID-19 vaccine in a cohort of healthcare workers in Milan (Lombardy Region, Northern Italy). Epidemiol. Prev. 2022, 46, 250–258. [Google Scholar] [CrossRef]
- Bowe, B.; Xie, Y.; Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 2022, 28, 2398–2405. [Google Scholar] [CrossRef]

| Year | Notifiable Cases | Recognized Cases | Rehabilitation Management | Benefits for Medical Treatment | |||
|---|---|---|---|---|---|---|---|
| N | n | % | n * | % | n ** | % | |
| 2020 | 21,147 | 16,538 | 78.2 | 747 | 4.5 | 2816 | 13.3 |
| 2021 | 111,099 | 76,164 | 68.6 | 2420 | 3.2 | 10,752 | 9.7 |
| September 2022 | 185,157 | 107,803 | 58.2 | 122 | 0.1 | 2866 | 1.6 |
| Total | 317,403 | 200,505 | 63.2 | 3289 | 1.6 | 16,434 | 5.2 |
| Year | Inpatient Treatment | Injury Benefit | Death | |||
|---|---|---|---|---|---|---|
| N | % | N | % | n | % | |
| 2020 | 947 | 4.5 | 884 | 4.2 | 31 | 0.15 |
| 2021 | 2914 | 2.6 | 4012 | 3.6 | 105 | 0.095 |
| September 2022 | 83 | 0.04 | 181 | 0.1 | 26 | 0.014 |
| Total | 3944 | 1.2 | 5077 | 1.6 | 162 | 0.05 |
| Reduction from 2020 to 2022 | 99.2 | 97.6 | 90.7 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nienhaus, A.; Stranzinger, J.; Kozak, A. COVID-19 as an Occupational Disease—Temporal Trends in the Number and Severity of Claims in Germany. Int. J. Environ. Res. Public Health 2023, 20, 1182. https://doi.org/10.3390/ijerph20021182
Nienhaus A, Stranzinger J, Kozak A. COVID-19 as an Occupational Disease—Temporal Trends in the Number and Severity of Claims in Germany. International Journal of Environmental Research and Public Health. 2023; 20(2):1182. https://doi.org/10.3390/ijerph20021182
Chicago/Turabian StyleNienhaus, Albert, Johanna Stranzinger, and Agnessa Kozak. 2023. "COVID-19 as an Occupational Disease—Temporal Trends in the Number and Severity of Claims in Germany" International Journal of Environmental Research and Public Health 20, no. 2: 1182. https://doi.org/10.3390/ijerph20021182
APA StyleNienhaus, A., Stranzinger, J., & Kozak, A. (2023). COVID-19 as an Occupational Disease—Temporal Trends in the Number and Severity of Claims in Germany. International Journal of Environmental Research and Public Health, 20(2), 1182. https://doi.org/10.3390/ijerph20021182







