Differentiating Use of Facial Expression between Individuals with and without Traumatic Brain Injury Using Affectiva Software: A Pilot Study
Abstract
1. Introduction
Aims
- Were there any differences in the use of facial expression between TBI participants and controls during narrative tasks using Affectiva?
- Were there any differences in the use of facial expression between a personal event narrative task and a story narrative retell task?
- Were there any confounding factors in video samples that may influence the validity or feasibility of the Affectiva analysis?
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.2.1. Selection of Participants
- (a)
- Participants were aged between 18–65 years;
- (b)
- Video samples were available for both a personal event narrative task and a story narrative retell. For participants with TBI, it was required that these video samples be available from their 6 month post-injury assessment.
- (c)
- (d)
- Narrative tasks were spoken in English
- (a)
- Participant videos that were unable to be processed sufficiently for analysis (less than 70% of the video sample processed) by Affectiva. For example, where the participant was not front-facing the camera, or poor lighting conditions.
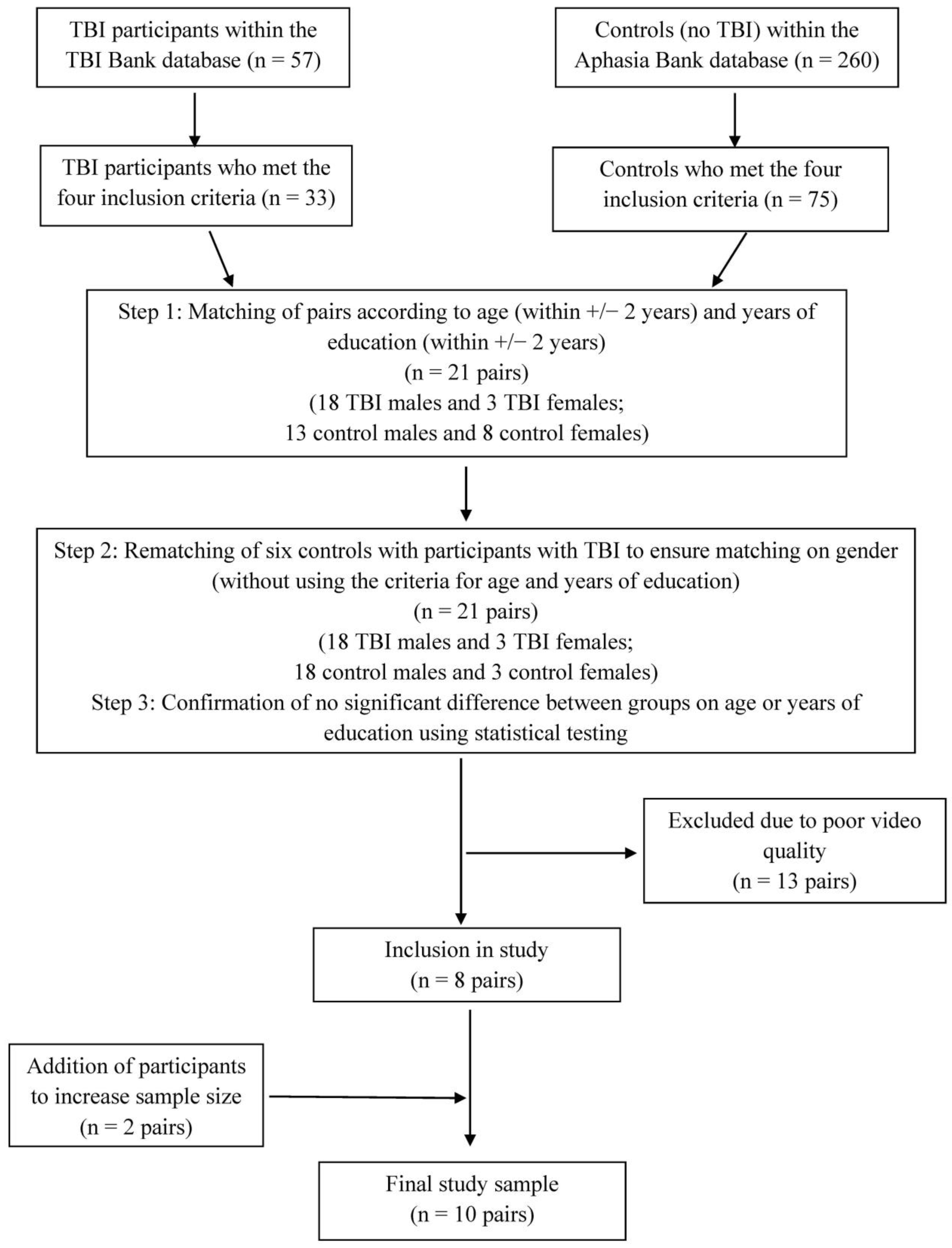
2.2.2. Matching of TBI and Control Participants
2.2.3. Participants with TBI
2.2.4. Controls
2.2.5. Comparison between Groups
2.3. Video Samples
2.3.1. Narrative Tasks
- (a)
- Personal event narrative
- i.
- For participants with TBI, “Tell me what you remember about when you had your head injury”.
- ii.
- For controls, “I wonder if you could tell me what you remember about any illness or injury you’ve had”.
- (b)
- Story narrative retell
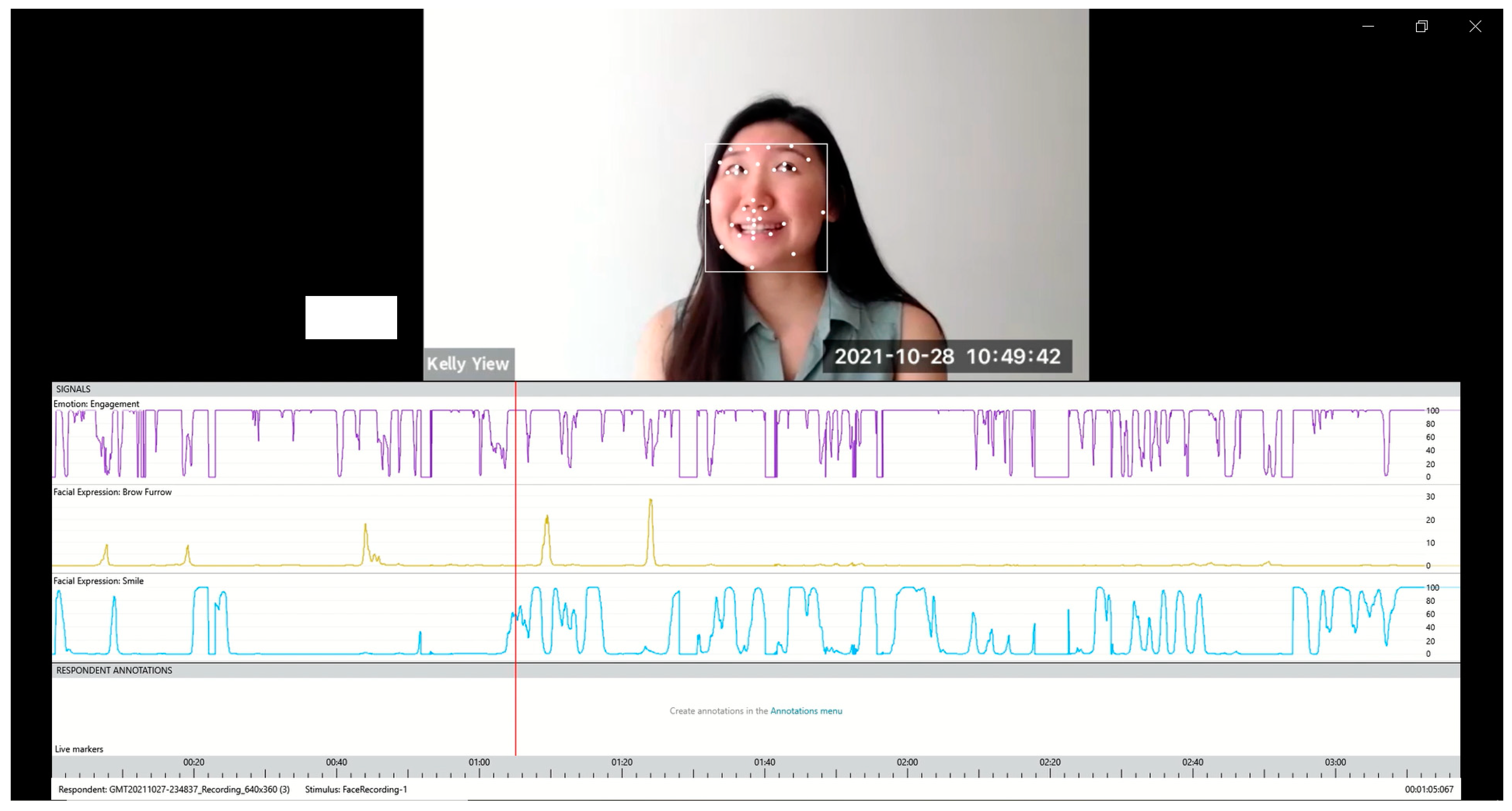
2.3.2. Affectiva Analysis
2.3.3. Facial Measures
2.3.4. Qualitative Observation
2.4. Data Analysis
3. Results
3.1. Affectiva Data
3.2. Qualitative Observations
3.3. Case Studies
3.3.1. Case Study 1—Zero Values
3.3.2. Case Study 2—Outlier Data
3.3.3. Case Study 3—Divergent Data between Narrative Tasks
4. Discussion
4.1. Limitations
4.2. Clinical Implications and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Qualitative Observation Form
| TBI Participant/Control | Rating | Describing the Context | Impression | Is the Use of Facial Expression Socially Appropriate? | ||
|---|---|---|---|---|---|---|
| Engagement (Rating 1–5) | Smile (Rating 1–5) | Brow Furrow (Rating 1–5) | ||||
| TBI Participant Brain Injury Story | ||||||
| TBI1 | 1 | 1 | 1 | Brain injury story—cannot remember the incident, but remember events 3 weeks afterwards, remember the treatment, but cannot remember details |
| Appropriate. |
| TBI2 | 1 | 1 | 1 | Brain injury story—talked about how he remembered being aggressive after coming out of coma, snapping at things, how he coped with it, and how it improved over time |
| Appropriate facial expression in the context of story recount. Facial expression matched tone of voice, flat. |
| TBI3 | 3 | 3 | 1 | Brain injury story—talked about what he remembered and his body functions |
| Appropriate facial expression. |
| TBI4 | 2 | 1 | 1 | Brain injury story—talked about how his injury happened
|
| Appropriate facial expression according to context. |
| TBI5 | 2 | 1 | 1 | Brain injury story—talked about what people told him
|
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished) |
| TBI6 | 1 | 2 | 1 | Brain injury story—unsure topic content
|
| Appropriate facial expression. Inappropriate. The participant’s conversation lacked content, was confused. |
| TBI7 | 2 | 2 | 1 | Brain injury story—talked about what he remembered → cannot remember about the accident day, cannot remember that he went to the doctor or CT scan, but remembered events at the rehabilitation centre
|
| Appropriate in this context—conversation topic did not involve strong emotions Monotonous voice, flat voice throughout |
| TBI8 | 4 | 3 | 1 | Brain injury story—talked about his hospital experience/memories → peed in bed, on crutches, having lunch, talking to nurses and doctors
|
| Appropriate. |
| TBI9 | 4 | 3 | 1 | Brain injury story—talked about her accident → could not eat, could not remember her husband, parents, only remembered her son
|
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished) |
| TBI10 | 2 | 1 | 1 | Brain injury story—talked about his accident → reported the accident to the police, waiting for police report
|
| Inappropriate. The participant maintained a fixed facial expression throughout the 1 min conversation. |
| Control Injury/Illness Story | ||||||
| C1 | 4 | 2 | 3 | Injury story—talked about his hip replacement
|
| Appropriate. |
| C2 | 2 | 1 | 1 | Injury story—described how he sprained his ankle
|
| Appropriate. |
| C3 | 3 | 2 | 1 | Injury story—described how they found out about his meningitis and events at the hospital and how he had no TV for 4 days Situation: retell |
| Appropriate. |
| C4 | 1 | 2 | 1 | Injury story—tackled by a jock, broken wrist Situation: retell, no strong emotion involved |
| Appropriate. |
| C5 | 3 | 2 | 3 | Injury story—went to freshman camp, bitten by fleas/bed bugs all over, broke out into rashes/hives Situation: retell |
| Appropriate. |
| C6 | 2 | 1 | 1 | Injury story—“cracked” his shoulders during a football drill (dislocation) |
| Appropriate. |
| C7 | 3 | 4 | 2 | Injury story—talked about his meningitis |
| Appropriate. |
| C8 | 1 | 1 | 1 | Injury story—talked about how she got diagnosed with type 1 diabetes |
| Appropriate. |
| C9 | 3 | 3 | 1 | Injury story—talked about his accident, hospitalised and how he got stitched up without anaesthesia Situation: retell, no strong emotions involved |
| Appropriate. |
| C10 | 2 | 1 | 1 | Injury story—talked about hurting his back, went for physical therapy |
| Appropriate. |
| TBI Participant Cinderella Story | ||||||
| TBI1 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| TBI2 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| TBI3 | 3 | 4 | 1 | Cinderella story |
| Appropriate. |
| TBI4 | 1 | 1 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI5 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| TBI6 | 2 | 2 | 3 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI7 | 1 | 1 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI8 | 3 | 1 | 1 | Cinderella story |
| Appropriate. |
| TBI9 | 2 | 2 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished). |
| TBI10 | 1 | 2 | 1 | Cinderella story |
| Inappropriate. The participant maintained a fixed facial expression throughout the narrative retell (except when he turned away on one occasion, and on another occasion, smiled when he finished). |
| Control Cinderella Story | ||||||
| C1 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C2 | 1 | 2 | 2 | Cinderella story |
| Appropriate. |
| C3 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| C4 | 1 | 2 | 1 | Cinderella story |
| Appropriate. |
| C5 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| C6 | 1 | 2 | 1 | Cinderella story |
| Appropriate. |
| C7 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C8 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C9 | 2 | 3 | 1 | Cinderella story |
| Appropriate. |
| C10 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
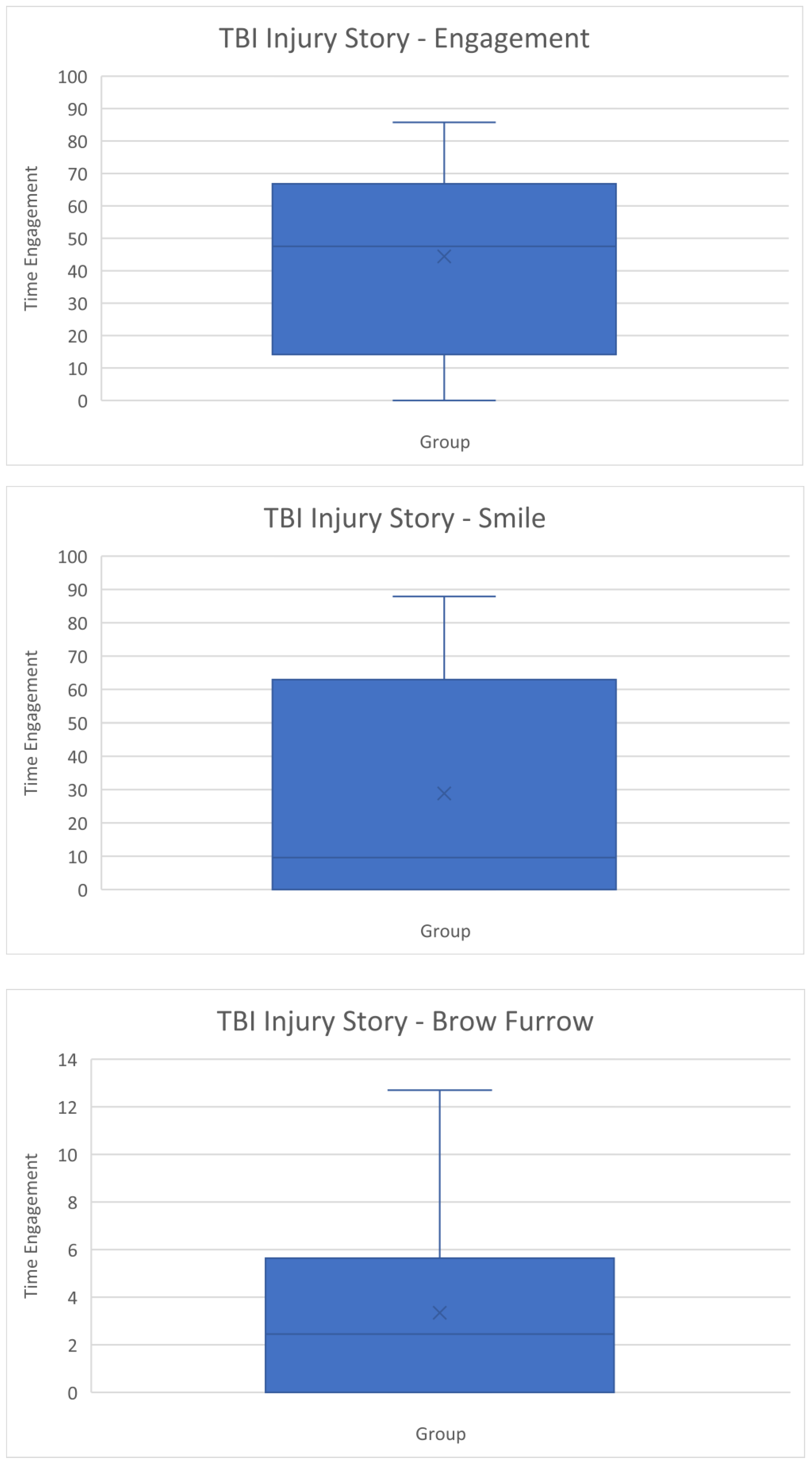
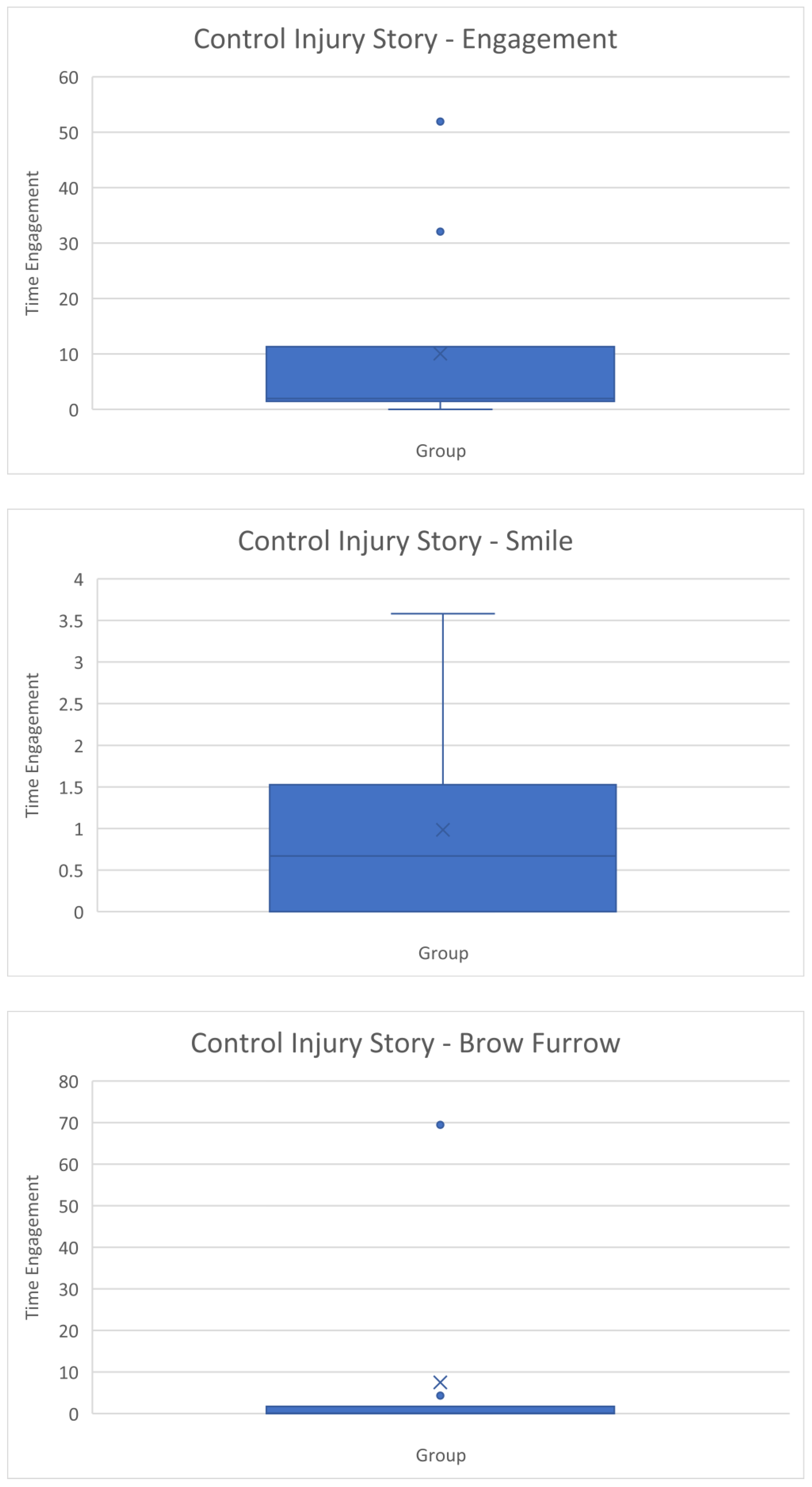
Appendix B. Box and Whisker Plots


References
- Johnson, J.E.; Turkstra, L.S. Inference in conversation of adults with traumatic brain injury. Brain Inj. 2012, 26, 1118–1126. [Google Scholar] [CrossRef] [PubMed]
- Sarno, M.T. The Nature of Verbal Impairment after Closed Head Injury. J. Nerv. Ment. Dis. 1980, 168, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Ruusuvuori, J.; Peräkylä, A. Facial and verbal expressions in assessing stories and topics. Res. Lang. Soc. Interact. Assess. Soc. Interact. 2009, 42, 377–394. [Google Scholar] [CrossRef]
- Croker, V.; McDonald, S. Recognition of emotion from facial expression following traumatic brain injury. Brain Inj. 2005, 19, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Zupan, B.; Neumann, D.; Babbage, D.; Willer, B. Exploration of a new tool for assessing emotional inferencing after traumatic brain injury. Brain Inj. 2015, 29, 877–887. [Google Scholar] [CrossRef] [PubMed]
- Karow, C.M.; Connors, E.C. Affective Communication in Normal and Brain-Damaged Adults: An Overview. Semin. Speech Lang. 2003, 24, 69–92. [Google Scholar] [CrossRef]
- Struchen, M.A.; Pappadis, M.R.; Sander, A.M.; Burrows, C.S.; Myszka, K.A. Examining the Contribution of Social Communication Abilities and Affective/Behavioral Functioning to Social Integration Outcomes for Adults With Traumatic Brain Injury. J. Head Trauma Rehabil. 2011, 26, 30–42. [Google Scholar] [CrossRef]
- Wauters, L.; Marquardt, T.P. Disorders of Emotional Communication in Traumatic Brain Injury. Semin. Speech Lang. 2019, 40, 13–26. [Google Scholar] [CrossRef]
- Bond, F.; Godfrey, H.P.D. Conversation with traumatically brain-injured individuals: A controlled study of behavioural changes and their impact. Brain Inj. 1997, 11, 319–330. [Google Scholar] [CrossRef]
- Rigon, A.; Turkstra, L.S.; Mutlu, B.; Duff, M.C. Facial-affect recognition deficit as a predictor of different aspects of social-communication impairment in traumatic brain injury. Neuropsychology 2018, 32, 476–483. [Google Scholar] [CrossRef]
- Shorland, J.; Douglas, J.M. Understanding the role of communication in maintaining and forming friendships following traumatic brain injury. Brain Inj. 2010, 24, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Morton, M.V.; Wehman, P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: A literature review and recommendations. Brain Injury. J. Head Trauma Rehabil. 1996, 11, 104. [Google Scholar] [CrossRef]
- Rauch, R.J.; Ferry, S.M. Social networks as support interventions following traumatic brain injury. NeuroRehabilitation 2001, 16, 11–16. [Google Scholar] [CrossRef]
- Paterson, J.; Stewart, J. Adults with Acquired Brain Injury: Perceptions of Their Social World. Rehabil. Nurs. 2002, 27, 13–18. [Google Scholar] [CrossRef]
- Temkin, N.R.; Corrigan, J.D.; Dikmen, S.S.; Machamer, J. Social Functioning After Traumatic Brain Injury. J. Head Trauma Rehabil. 2009, 24, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Finch, E.; French, A.; Ou, R.J.; Fleming, J. Participation in communication activities following traumatic brain injury: A time use diary study. Brain Inj. 2016, 30, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Arnould, A.; Rochat, L.; Azouvi, P.; Van Der Linden, M. Apathetic symptom presentations in patients with severe traumatic brain injury: Assessment, heterogeneity and relationships with psychosocial functioning and caregivers’ burden. Brain Inj. 2015, 29, 1597–1603. [Google Scholar] [CrossRef]
- Roy, D.; McCann, U.; Han, D.; Rao, V. Pathological Laughter and Crying and Psychiatric Comorbidity After Traumatic Brain Injury. J. Neuropsychiatry Clin. Neurosci. 2015, 27, 299–303. [Google Scholar] [CrossRef]
- Marquardt, T.P.; Rios-Brown, M.; Richburg, T.; Seibert, L.K.; Cannito, M.P. Comprehension and expression of affective sentences in traumatic brain injury. Aphasiology 2001, 15, 1091–1101. [Google Scholar] [CrossRef]
- McDonald, S.; Bornhofen, C.; Shum, D.H.K.; Long, E.; Saunders, C.; Neulinger, K. Reliability and validity of The Awareness of Social Inference Test (TASIT): A clinical test of social perception. Disabil. Rehabil. 2006, 28, 1529–1542. [Google Scholar] [CrossRef]
- Prutting, C.A.; Kirchner, D.M. A clinical appraisal of the pragmatic aspects of language. J. Speech Hear. Disord. 1987, 52, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Linscott, R.; Knight, R.G.; Godfrey, H.P.D. The Profile of Functional Impairment in Communication (PFIC): A measure of communication impairment for clinical use. Brain Inj. 1996, 10, 397–412. [Google Scholar] [CrossRef] [PubMed]
- iMotions. Facial Expression Analysis: The Complete Pocket Guide; iMotions: Copenhagen, Denmark, 2017. [Google Scholar]
- iMotions. iMotions Core: The World’s Leading Biosensor Platform; iMotions: Copenhagen, Denmark, 2019. [Google Scholar]
- iMotions. Facial Expression Analysis. Available online: https://imotions.com/biosensor/fea-facial-expression-analysis/ (accessed on 25 October 2021).
- Kulke, L.; Feyerabend, D.; Schacht, A. A Comparison of the Affectiva iMotions Facial Expression Analysis Software With EMG for Identifying Facial Expressions of Emotion. Front. Psychol. 2020, 11, 329. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, J.M.; Penichet, V.M.R.; Lozano, M.D.; Fernando, A. Using emotion recognition technologies to teach children with autism spectrum disorder how to identify and express emotions. Univers. Access Inf. Soc. 2021, 21, 809–825. [Google Scholar] [CrossRef]
- Ho, M.W.-R.; Chien, S.H.-L.; Lu, M.-K.; Chen, J.-C.; Aoh, Y.; Chen, C.-M.; Lane, H.-Y.; Tsai, C.-H. Impairments in face discrimination and emotion recognition are related to aging and cognitive dysfunctions in Parkinson’s disease with dementia. Sci. Rep. 2020, 10, 4367. [Google Scholar] [CrossRef] [PubMed]
- TalkBank. The TalkBank System. Available online: https://www.talkbank.org/ (accessed on 20 August 2022).
- Elbourn, E.; Kenny, B.; Power, E.; Togher, L. Psychosocial Outcomes of Severe Traumatic Brain Injury in Relation to Discourse Recovery: A Longitudinal Study up to 1 Year Post-Injury. Am. J. Speech-Lang. Pathol. 2019, 28, 1463–1478. [Google Scholar] [CrossRef]
- MacWhinney, B.; Fromm, D.; Forbes, M.; Holland, A. AphasiaBank: Methods for studying discourse. Aphasiology 2011, 25, 1286–1307. [Google Scholar] [CrossRef]
- Teasdale, G.M. Head injury. J. Neurol. Neurosurg. Psychiatry 1995, 58, 526–539. [Google Scholar] [CrossRef]
- Russell, W.; Smith, A. A post-traumatic amnesia in head injury. Arch. Neurol. 1961, 5, 16–29. [Google Scholar] [CrossRef]
- Ponsford, J.; Sloan, S.; Snow, P. Traumatic Brain Injury: Rehabilitation for Everyday Adaptive Living, 2nd ed.; Sloan, S., Snow, P., Eds.; Psychology Press: Hove, UK, 2013. [Google Scholar]
- Power, E.; Weir, S.; Richardson, J.; Fromm, D.; Forbes, M.; MacWhinney, B.; Togher, L. Patterns of narrative discourse in early recovery following severe Traumatic Brain Injury. Brain Inj. 2019, 34, 98–109. [Google Scholar] [CrossRef]
- Stark, B.C. A Comparison of Three Discourse Elicitation Methods in Aphasia and Age-Matched Adults: Implications for Language Assessment and Outcome. Am. J. Speech-Lang. Pathol. 2019, 28, 1067–1083. [Google Scholar] [CrossRef] [PubMed]
- Affectiva. Emotion AI 101: All about Emotion Detection and Affectiva’s Emotion Metrics. Available online: https://blog.affectiva.com/emotion-ai-101-all-about-emotion-detection-and-affectivas-emotion-metrics (accessed on 25 October 2021).
- Perneger, T.V. What’s wrong with Bonferroni adjustments. BMJ 1998, 316, 1236–1238. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L. Best (but oft-forgotten) practices: The multiple problems of multiplicity—Whether and how to correct for many statistical tests. Am. J. Clin. Nutr. 2015, 102, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Turkstra, L.S.; Quinn-Padron, M.; Johnson, J.E.; Workinger, M.S.; Antoniotti, N. In-Person Versus Telehealth Assessment of Discourse Ability in Adults With Traumatic Brain Injury. J. Head Trauma Rehabil. 2012, 27, 424–432. [Google Scholar] [CrossRef]
- Maryn, Y. Practical Acoustics in Clinical Voice Assessment: A Praat Primer. Perspect. ASHA Spéc. Interes. Groups 2017, 2, 14–32. [Google Scholar] [CrossRef]
- Cohen, N.S. The Effect of Vocal Instruction and Visi-Pitch Feedback on the Speech of Persons with Neurogenic Communication Disorders: Two Case Studies. Music. Ther. Perspect. 1995, 13, 70–75. [Google Scholar] [CrossRef]
- TalkBank. TalkBank Software. Available online: https://talkbank.org/software/ (accessed on 3 November 2021).
- Kabir, M. Does artificial intelligence (AI) constitute an opportunity or a threat to the future of medicine as we know it? Future Healthc. J. 2019, 6, 190–191. [Google Scholar] [CrossRef]
- iMotions. EDA/GSR (Electrodermal Activity). Available online: https://imotions.com/products/imotions-lab/modules/eda-gsr-electrodermal-activity/ (accessed on 19 December 2022).
- VanSolkema, M.; McCann, C.; Barker-Collo, S.; Foster, A. Attention and Communication Following TBI: Making the Connection through a Meta-Narrative Systematic Review. Neuropsychol. Rev. 2020, 30, 345–361. [Google Scholar] [CrossRef]
- Neumann, D.; Westerhof-Evers, H.J.; Visser-Keizer, A.C.; Fasotti, L.; Schönherr, M.C.; Vink, M.; van der Naalt, J.; Spikman, J.M. Effectiveness of a treatment for impairments in social cognition and emotion regulation (T-ScEmo) after traumatic brain injury: A randomized controlled trial. J. Head Trauma Rehabil. 2017, 32, 296–307. [Google Scholar] [CrossRef]
| Participant | Gender | Age | Years of Education | Language | Primary Language | Cause of Injury | PTA Days |
|---|---|---|---|---|---|---|---|
| TBI1 | Male | 49 | 17 | Monolingual | English | MVA | 41 |
| TBI2 | Male | 48 | 10 | Monolingual | English | Fall (height > 1 m) | 14 |
| TBI3 | Male | 32 | 16 | Monolingual | English | Assault and/or fall (ground) | 34 |
| TBI4 | Male | 44 | 13 | Monolingual | English | Fall (stairs) | 19 |
| TBI5 | Male | 40 | 17 | Monolingual | English | MVA | 55 |
| TBI6 | Male | 28 | 15 | Monolingual | English | MVA | 64 |
| TBI7 | Male | 26 | 18 | Multilingual | Urdu | MVA | 44 |
| TBI8 | Male | 24 | 16 | Bilingual | English | MVA | 25 |
| TBI9 | Female | 33 | 10 | Bilingual | Singhalese | MVA | 103 |
| TBI10 | Male | 54 | 13 | Monolingual | English | MVA | 18 |
| Participant | Gender | Age | Years of Education | Language | Primary Language |
|---|---|---|---|---|---|
| C1 | Male | 44.3 | 16 | Multilingual | English |
| C2 | Male | 42.2 | 18 | Monolingual | English |
| C3 | Male | 47.5 | 12 | Monolingual | English |
| C4 | Male | 57.5 | 14 | Monolingual | English |
| C5 | Male | 31.7 | 18 | Monolingual | English |
| C6 | Male | 23 | 16 | Monolingual | English |
| C7 | Male | 23.3 | 15 | Monolingual | English |
| C8 | Female | 33.7 | 12 | Monolingual | English |
| C9 | Male | 31.2 | 16 | Multilingual | English |
| C10 | Male | 48.1 | 16 | Monolingual | English |
| TBI/Control Participant | Rating | Describing the Context | Impression | Is the Use of Facial Expression Socially Appropriate? | ||
|---|---|---|---|---|---|---|
| Engagement (Rating 1–5) | Smile (Rating 1–5) | Brow Furrow (Rating 1–5) | ||||
| TBI10 | 2 | 1 | 1 | Brain injury story—talked about his accident → reported the accident to the police, waiting for police report. Situation: disheartening, unable to do much at the moment. | Startled facial expression (raised eyebrows), maintained throughout the video/expression did not change. Did not blink at all. However, used eye contact, body posture (leaning forward), and gesture to show engagement. Answered the interviewer’s question appropriately. | Inappropriate. The participant maintained a fixed facial expression throughout the 1 min conversation. |
| TBI Participants | Engagement Time Percentage | Smile Time Percentage | Brow Furrow Time Percentage |
| TBI1 | 48.78 | 0 | 12.7 |
| TBI2 | 65.88 | 0 | 1.95 |
| TBI3 | 85.75 | 47.6 | 2.95 |
| TBI4 | 0 | 0 | 0 |
| TBI5 | 46.27 | 0 | 3.63 |
| TBI6 | 60.04 | 87.89 | 5.17 |
| TBI7 | 17.55 | 19.22 | 0 |
| TBI8 | 69.51 | 75.06 | 0 |
| TBI9 | 46.23 | 58.91 | 7.05 |
| TBI10 | 4.03 | 0 | 0 |
| Control Participants | Engagement Time Percentage | Smile Time Percentage | Brow Furrow Time Percentage |
| C1 | 2.07 | 1.12 | 0.03 |
| C2 | 51.93 | 0 | 69.44 |
| C3 | 32.07 | 1.06 | 0.09 |
| C4 | 1.32 | 0.51 | 0.07 |
| C5 | 1.50 | 0 | 0.86 |
| C6 | 1.78 | 0 | 0.12 |
| C7 | 4.39 | 0.83 | 0.17 |
| C8 | 0 | 0 | 0 |
| C9 | 3.72 | 3.58 | 0 |
| C10 | 1.84 | 2.75 | 4.31 |
| TBI Participants | Engagement Time Percentage | Smile Time Percentage | Brow Furrow Time Percentage |
| TBI1 | 57.81 | 1.69 | 8.81 |
| TBI2 | 72.28 | 7.87 | 26.41 |
| TBI3 | 92.31 | 83.20 | 1.39 |
| TBI4 | 1.83 | 0.83 | 0.88 |
| TBI5 | 73.03 | 1.65 | 1.65 |
| TBI6 | 51.65 | 47.00 | 8.43 |
| TBI7 | 31.10 | 28.58 | 3.73 |
| TBI8 | 51.54 | 49.89 | 0 |
| TBI9 | 30.54 | 40.89 | 4.05 |
| TBI10 | 83.53 | 0.41 | 0.19 |
| Control Participants | Engagement Time Percentage | Smile Time Percentage | Brow Furrow Time Percentage |
| C1 | 1.93 | 0.08 | 0 |
| C2 | 10.41 | 2.93 | 13.44 |
| C3 | 25.23 | 0.15 | 0.56 |
| C4 | 21.92 | 13.64 | 1.02 |
| C5 | 0.58 | 0.16 | 0.28 |
| C6 | 7.01 | 0.26 | 0.38 |
| C7 | 0.39 | 0 | 0.01 |
| C8 | 29.59 | 4.55 | 0.50 |
| C9 | 0.38 | 0.38 | 0 |
| C10 | 4.95 | 12.46 | 0.66 |
| Facial Measures | TBI Participants (n = 10) | Control Participants (n = 10) | Statistical Significance |
|---|---|---|---|
| Engagement time percentage | Median: 47.53 Range: 0.00–85.75 | Median: 1.96 Range: 0.00–51.93 | p = 0.011 * U = 82.50 |
| Smile time percentage | Median: 9.61 Range: 0.00–87.89 | Median: 0.67 Range: 0.00–3.58 | p = 0.481 U = 60.00 |
| Brow furrow time percentage | Median: 2.45 Range: 0.00–12.70 | Median: 0.11 Range: 0.00–69.44 | p = 0.739 U = 55.00 |
| Facial Measures | TBI Participants (n = 10) | Control Participants (n = 10) | Statistical Significance |
|---|---|---|---|
| Engagement time percentage | Median: 54.73 Range: 1.83–92.31 | Median: 5.98 Range: 0.38–29.59 | p ≤ 0.001 * U = 93.00 |
| Smile time percentage | Median: 18.23 Range: 0.41–83.20 | Median: 0.32 Range: 0.00–13.64 | p = 0.015 * U = 82.00 |
| Brow furrow time percentage | Median: 2.69 Range: 0.00–26.41 | Median: 0.44 Range: 0.00–13.44 | p = 0.052 U = 76.00 |
| Facial Measures | Personal Event Story | Cinderella Story | Statistical Significance |
|---|---|---|---|
| Engagement time percentage | Median: 47.53 Range: 0.00–85.75 | Median: 54.73 Range: 1.83–92.31 | p = 0.386 Z = 0.866 |
| Smile time percentage | Median: 9.61 Range: 0.00–87.89 | Median: 18.23 Range: 0.41–83.20 | p = 0.799 Z = 0.255 |
| Brow furrow time percentage | Median: 2.45 Range: 0.00–12.70 | Median: 2.69 Range: 0.00–26.41 | p = 0.767 Z = 0.296 |
| Facial Measures | Personal Event Story | Cinderella Story | Statistical Significance |
|---|---|---|---|
| Engagement time percentage | Median: 1.96 Range: 0.00–51.93 | Median: 5.98 Range: 0.38–29.59 | p = 0.878 Z = −0.153 |
| Smile time percentage | Median: 0.67 Range: 0.00–3.58 | Median: 0.32 Range: 0.00–13.64 | p = 0.386 Z = 0.866 |
| Brow furrow time percentage | Median: 0.11 Range: 0.00–69.44 | Median: 0.44 Range: 0.00–13.44 | p = 0.678 Z = −0.415 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yiew, K.; Togher, L.; Power, E.; Brunner, M.; Rietdijk, R. Differentiating Use of Facial Expression between Individuals with and without Traumatic Brain Injury Using Affectiva Software: A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 1169. https://doi.org/10.3390/ijerph20021169
Yiew K, Togher L, Power E, Brunner M, Rietdijk R. Differentiating Use of Facial Expression between Individuals with and without Traumatic Brain Injury Using Affectiva Software: A Pilot Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1169. https://doi.org/10.3390/ijerph20021169
Chicago/Turabian StyleYiew, Kelly, Leanne Togher, Emma Power, Melissa Brunner, and Rachael Rietdijk. 2023. "Differentiating Use of Facial Expression between Individuals with and without Traumatic Brain Injury Using Affectiva Software: A Pilot Study" International Journal of Environmental Research and Public Health 20, no. 2: 1169. https://doi.org/10.3390/ijerph20021169
APA StyleYiew, K., Togher, L., Power, E., Brunner, M., & Rietdijk, R. (2023). Differentiating Use of Facial Expression between Individuals with and without Traumatic Brain Injury Using Affectiva Software: A Pilot Study. International Journal of Environmental Research and Public Health, 20(2), 1169. https://doi.org/10.3390/ijerph20021169





