Effectiveness of Family-Involved Interventions in Reducing Co-Occurring Alcohol Use and Mental Health Problems in Young People Aged 12–17: A Systematic Review and Meta-Analysis
Abstract
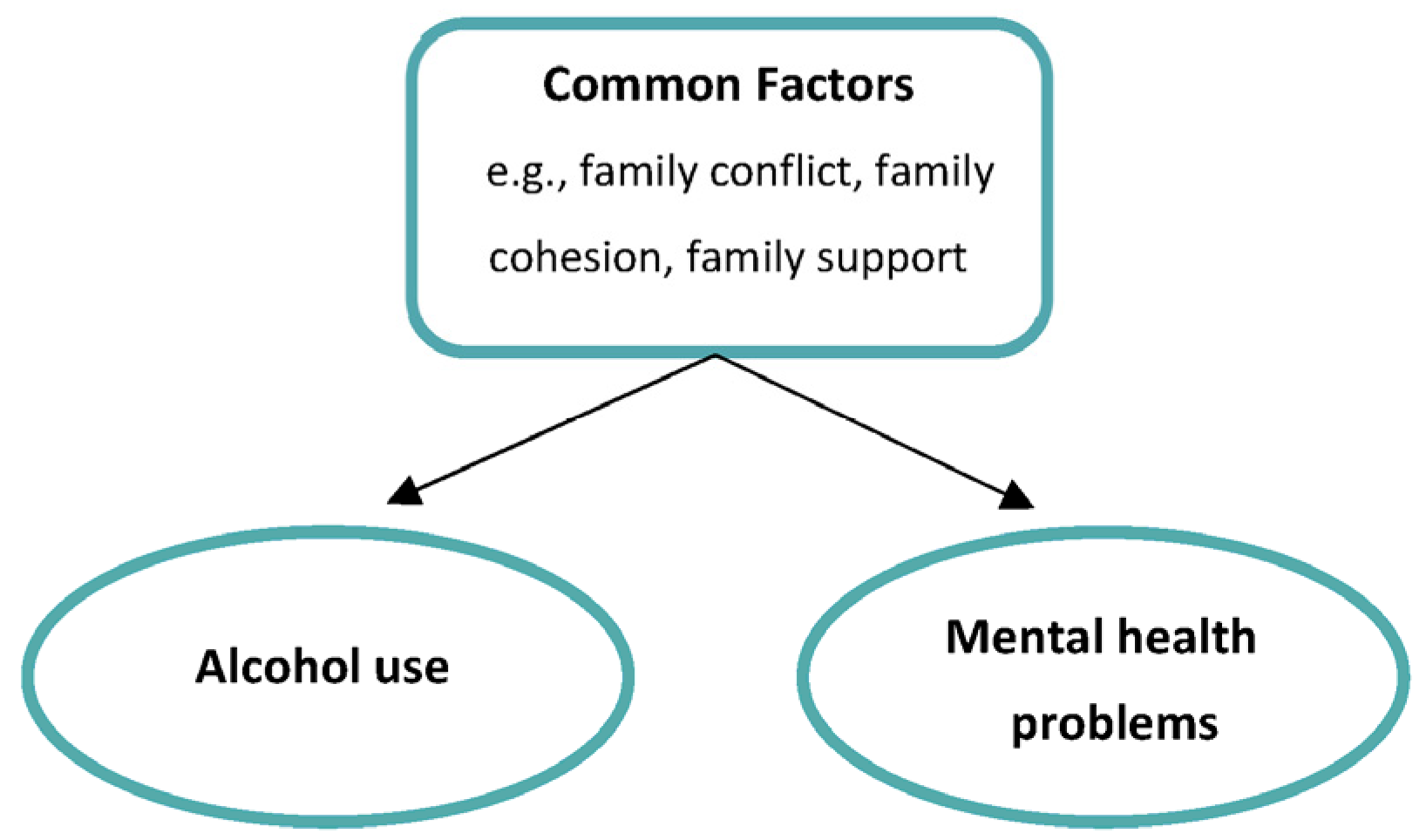
1. Introduction
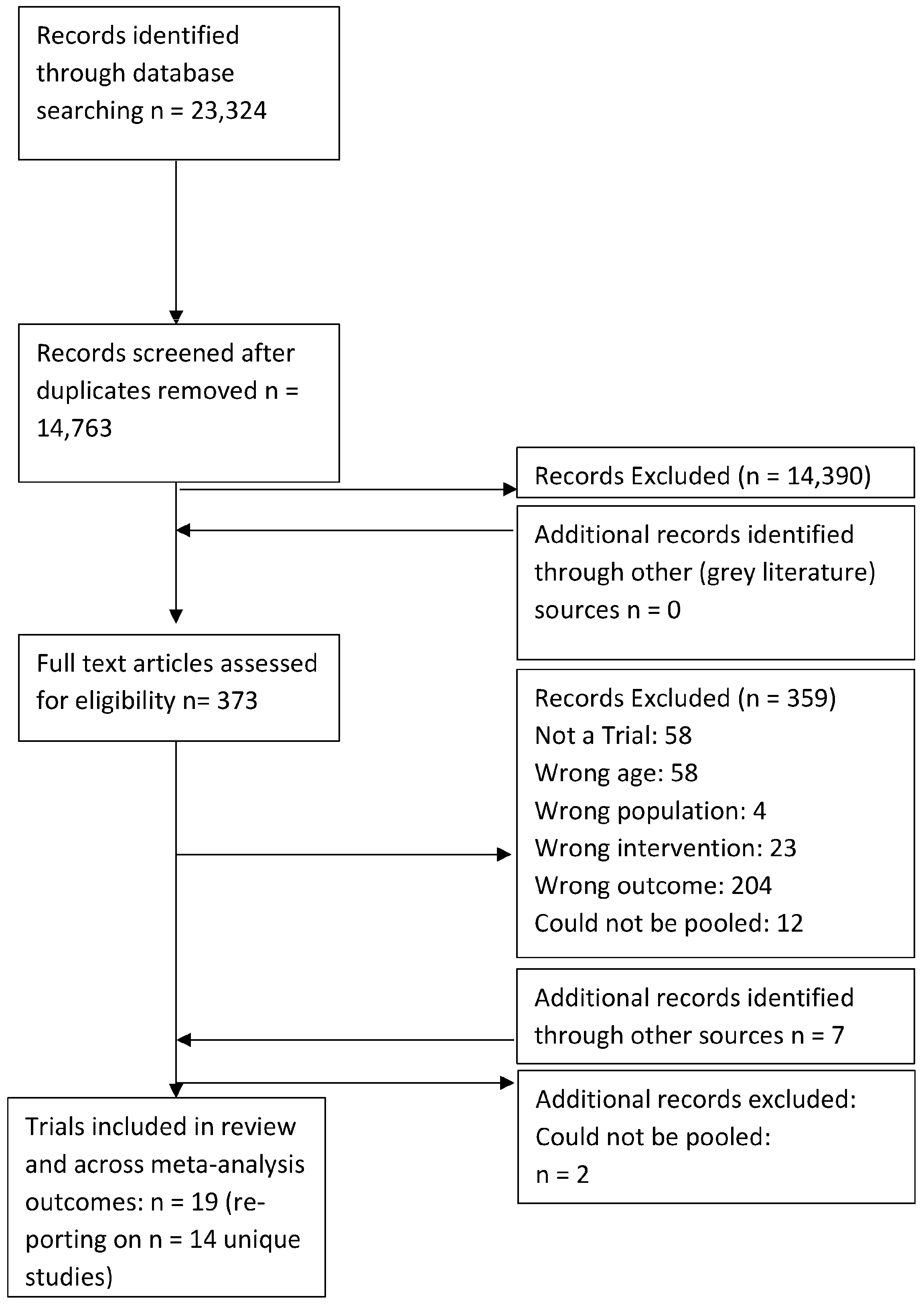
2. Materials and Methods
2.1. Eligibility Criteria
- Targeted young people aged 12–17 of any ethnicity or gender. Twelve years was selected as the lower cut-off as it is the common age of onset for both alcohol use and mental health problems [36,37]. Seventeen was selected as the upper age limit as family does not always remain a key influential context beyond this age. This is partly due to no longer having legislated age-related restrictions in the UK and other European countries [38]. Therefore, alcohol use may be less dependent on the family’s influence. Trials that had a broader age range were included if the mean age of participants fell between 12–17 years.
- Reported on a family-involved psycho-social intervention in which a young person and caregiver were included, either separately or together, in at least one session. A broad definition of family was employed to include parents, carers, grandparents, aunts, uncles and siblings. All levels of prevention and treatment were included to ensure a more thorough evaluation and to enable comparisons between these three levels of family-involved psycho-social interventions. These levels include: ‘universal prevention’ targets the entire population irrespective of risk [39]; ‘targeted prevention’ consists of ‘selective’ interventions [39]; targeting individuals at risk and ‘indicated’ interventions [39]; individuals with pre-existing symptoms or pre-clinical diagnoses, with the aim of reducing alcohol use and mental health problems before it reaches a diagnostic threshold [39] and ‘treatment’ is aimed at individuals with a diagnosis [13]. Levels of prevention can be considered to be on a continuum, with the levels merging into one another rather than occurring as distinct alternatives [40].
- Reported on both the primary outcomes: alcohol consumption (including frequency of drinking, binge drinking defined as drinking five or more drinks on any one occasion, regular or problem drinking) and common adolescent mental health problems including (a) internalizing problems such as anxiety and depression as well as (b) externalizing problems such as conduct problems and ADHD symptoms. Outcome measures could either report on the specific mental health problems or the overall internalizing or externalizing symptom score. Secondary outcomes included other substances and family functioning.
- Had a robust evaluation design, specifically randomized controlled trials (RCTs), controlled trials, randomized trials (RTs) and quasi-experimental trials. Trials that included active controls (such as a different variant of the same intervention or a different kind of therapy) were defined as RTs, and those employing inactive controls (such as no treatment, waitlist control and standard care) were defined as RCTs in this review [41].
2.2. Search Strategy
2.3. Study Selection, Risk of Bias Assessment and Extraction
2.4. Data Analysis
3. Results
3.1. Description of Included Trials
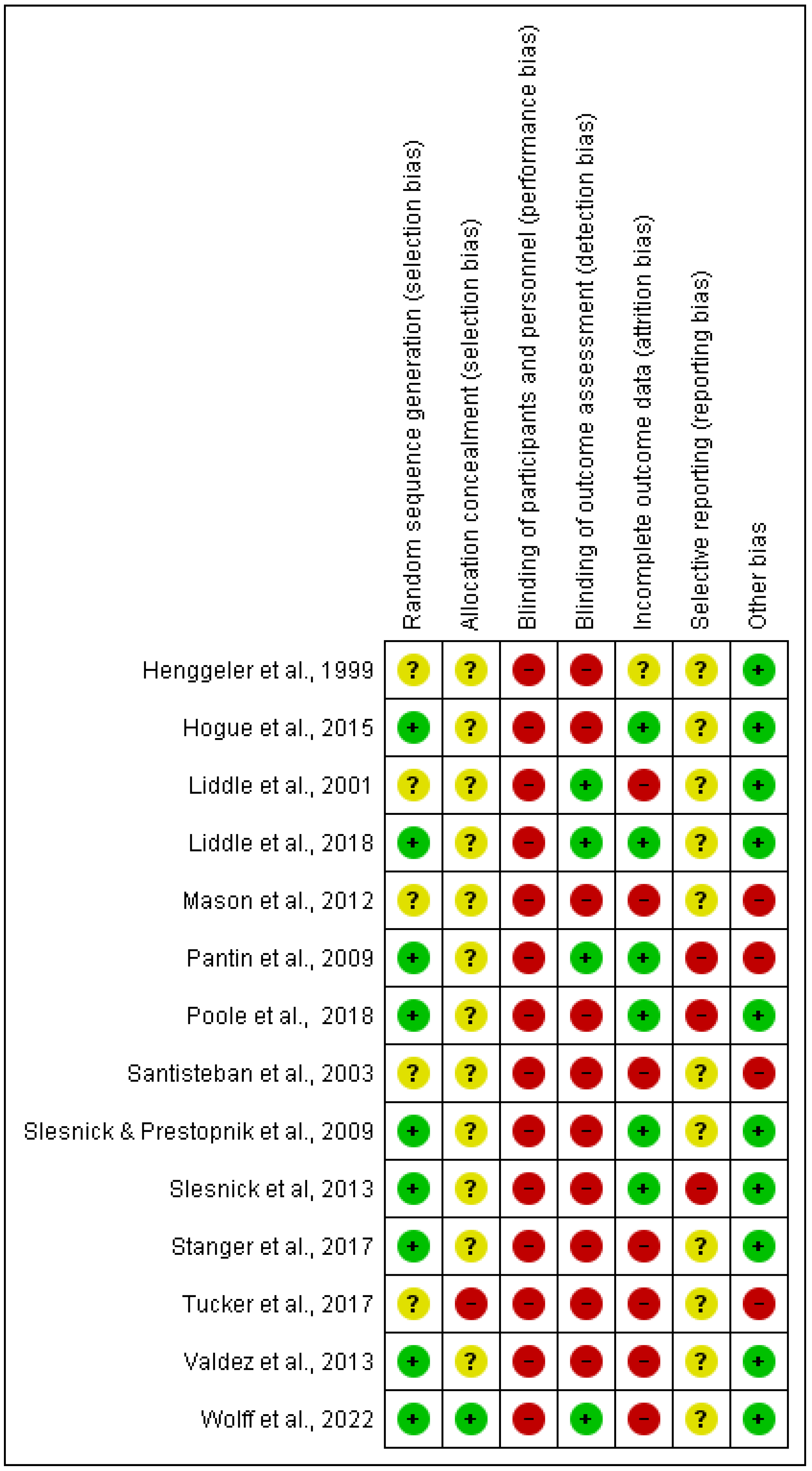
3.2. Risk of Bias
3.2.1. Random Sequence Generation
3.2.2. Allocation Concealment
3.2.3. Blinding of Participants and Outcome Assessment
3.2.4. Incomplete Outcome Data
3.2.5. Selective Reporting
3.2.6. Other Potential Sources of Bias
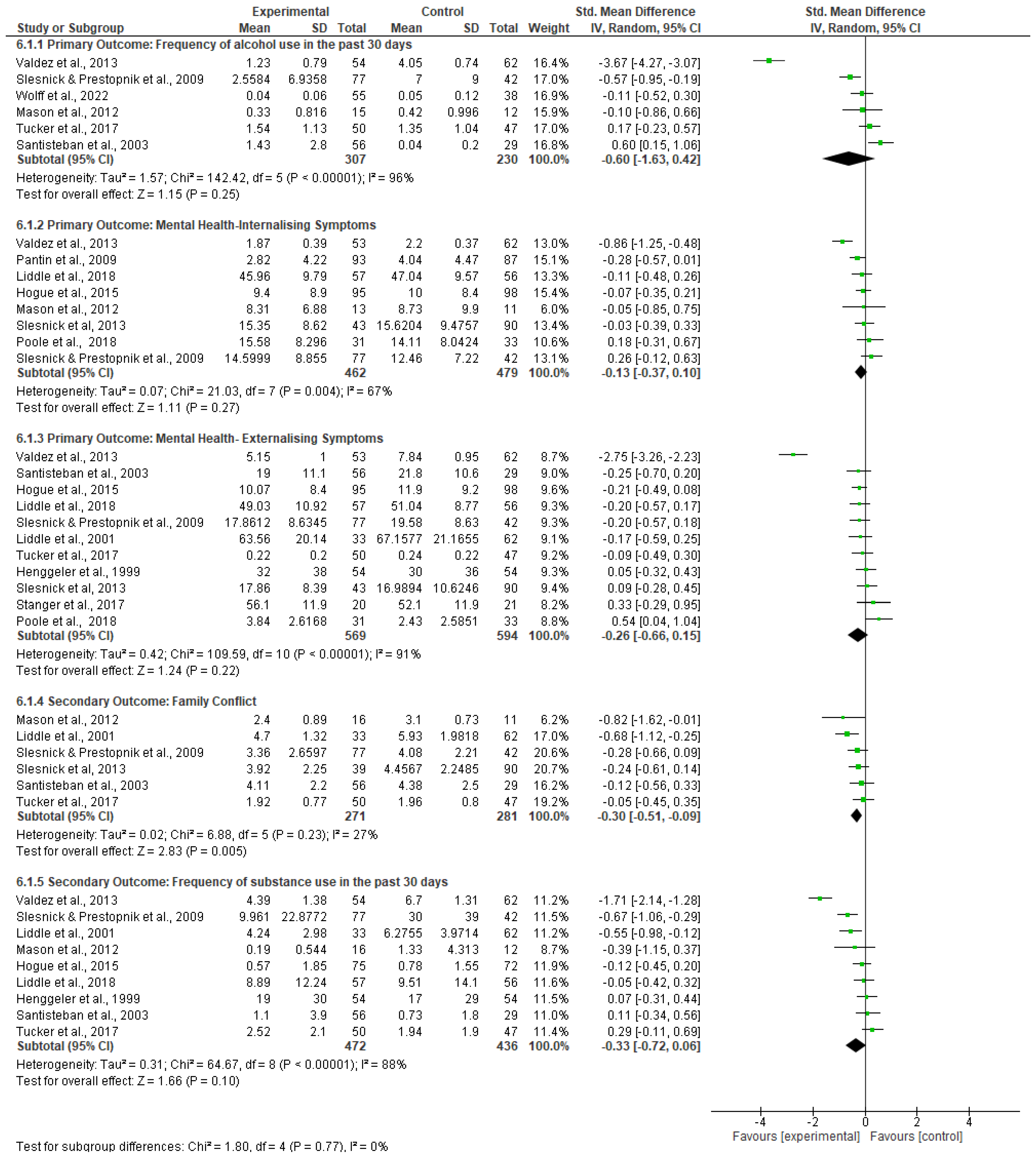
3.3. Meta-Analyses Findings
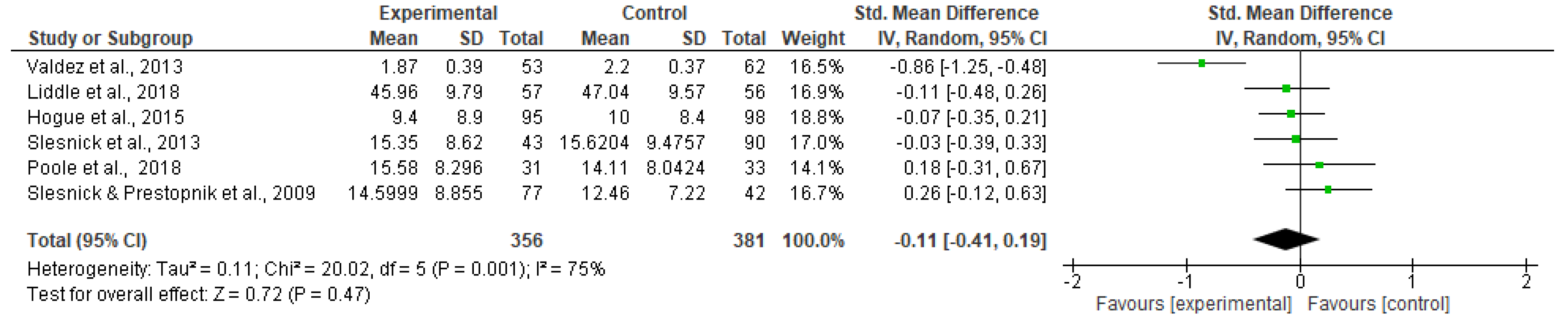
3.3.1. Primary Outcomes
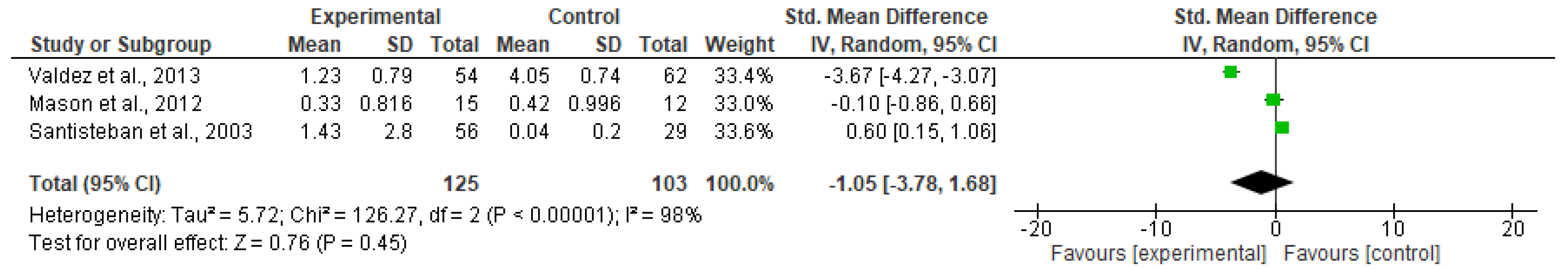
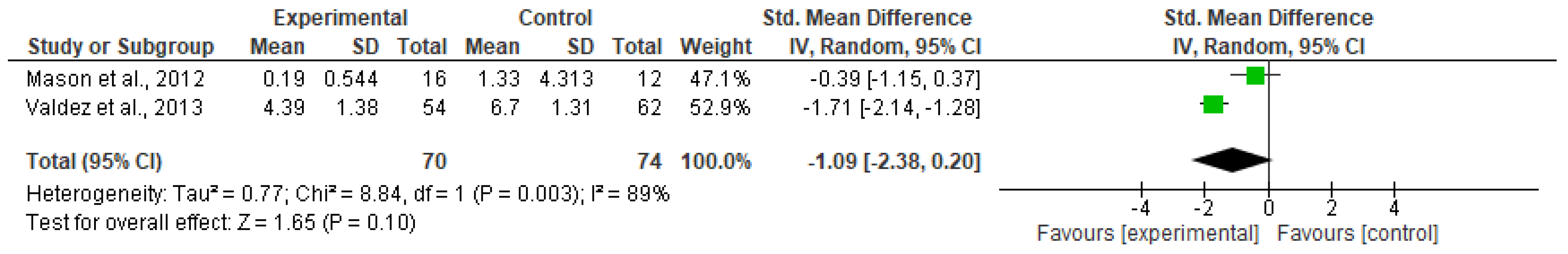
Effectiveness of Family-Involved Interventions
Impact of Prevention and Treatment
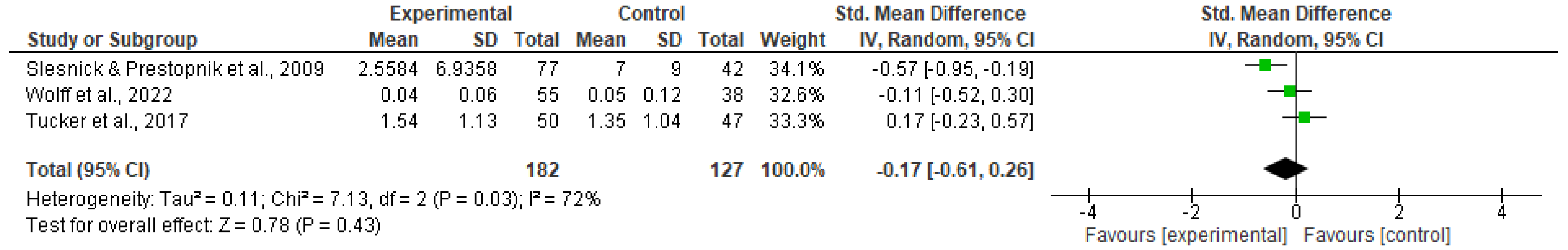
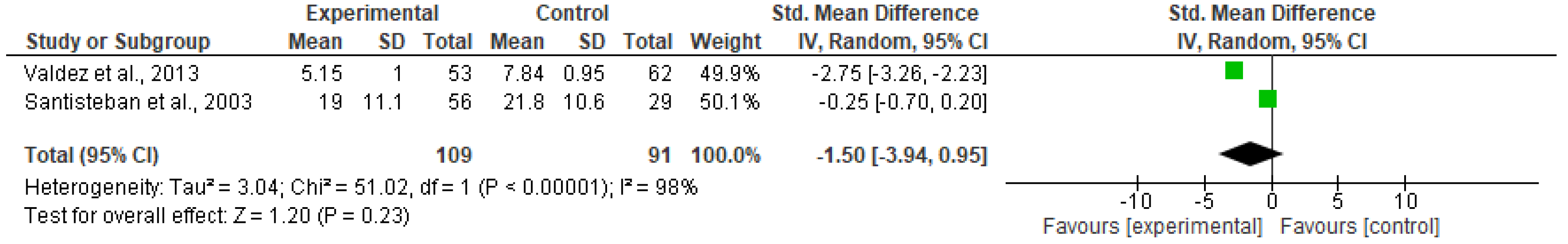
Effectiveness of Family-Involved Interventions
Impact of Prevention and Treatment
Impact of Young Person’s Age
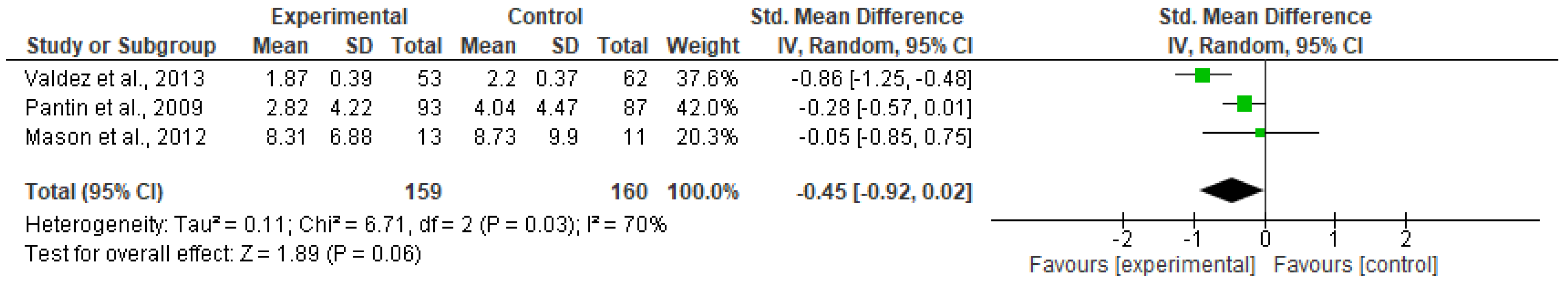
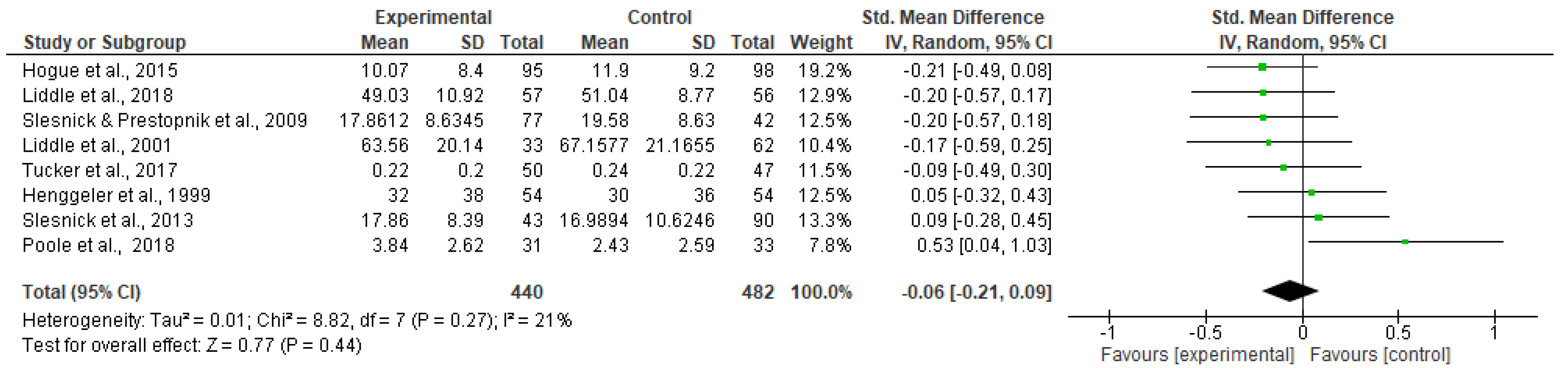
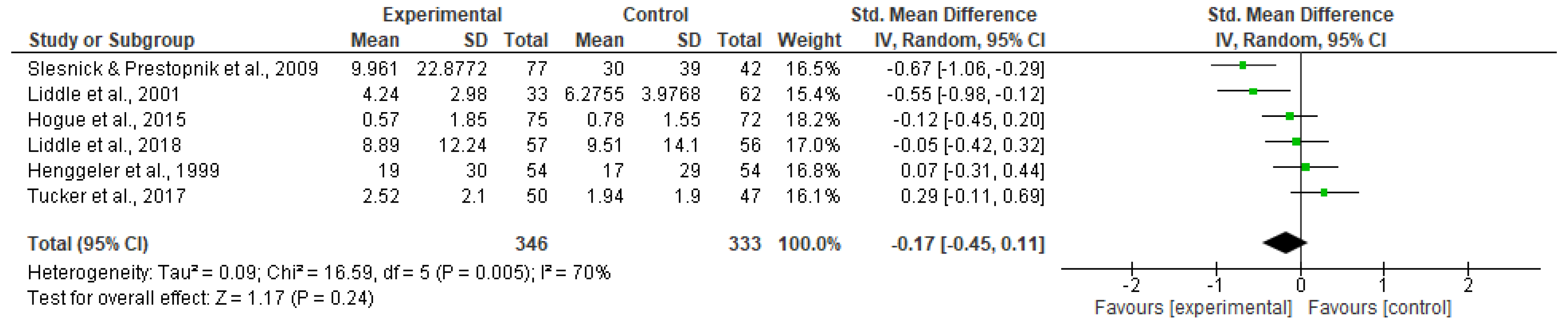
Effectiveness of Family-Involved Interventions
Impact of Prevention and Treatment
3.3.2. Secondary Outcomes
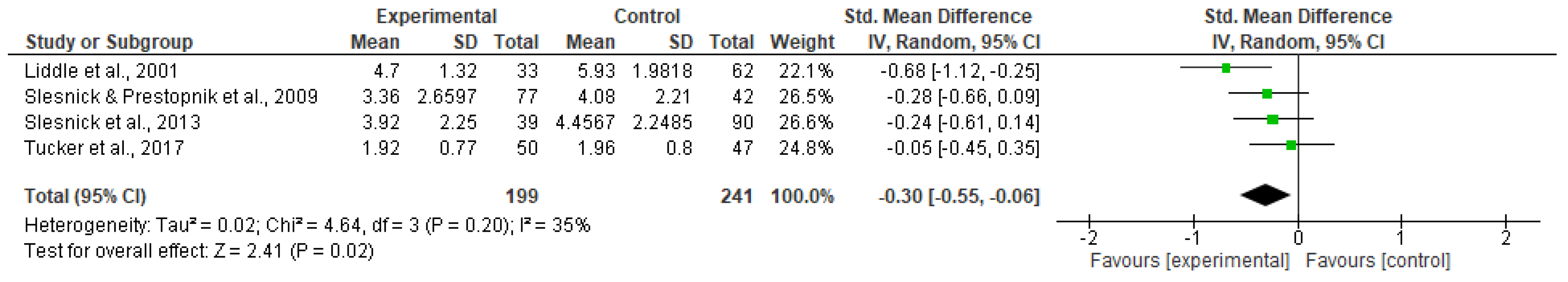
Effectiveness of Family-Involved Interventions
Impact of Prevention and Treatment
Effectiveness of Family-Involved Interventions
Impact of Prevention and Treatment
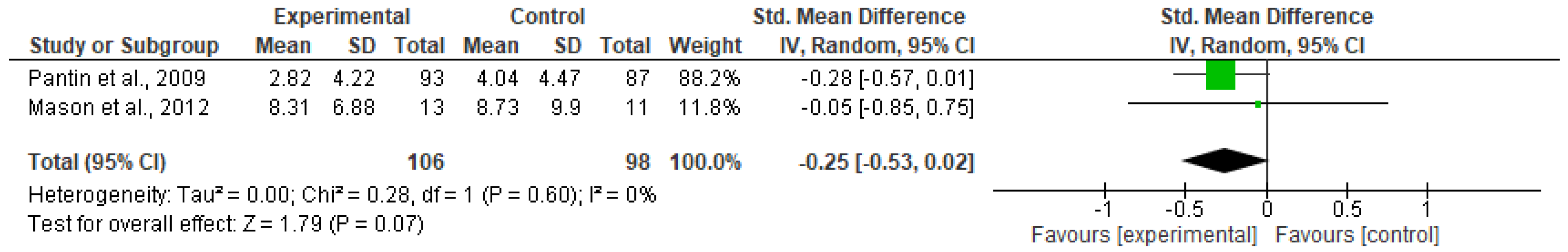
3.3.3. Sensitivity Analysis
Time Band of 3–12 Month Follow-Up
Outcome Measures
Outliers
3.3.4. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Erskine, H.E.; Moffitt, T.E.; Copeland, W.E.; Costello, E.J.; Ferrari, A.J.; Patton, G.; Degenhardt, L.; Vos, T.; Whiteford, H.A.; Scott, J.G. A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol. Med. 2015, 45, 1551–1563. [Google Scholar] [CrossRef]
- Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; Schulenberg, J.E. Monitoring the Future National Survey Results on Drug Use, 1975–2010; Institute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 2011; Volume 1. [Google Scholar]
- Degenhardt, L.; Stockings, E.; Patton, G.; Hall, W.D.; Lynksey, M. The increasing global health priority of substance use in young people. Lancet Psychiatry 2016, 3, 251–264. [Google Scholar] [CrossRef]
- Velleman, R.D.; Templeton, L.J.; Copello, A.G. The role of the family in preventing and intervening with substance use and misuse: A comprehensive review of family interventions, with a focus on young people. Drug Alcohol Rev. 2005, 24, 93–109. [Google Scholar] [CrossRef]
- Rowe, C.L.; Liddle, H.A.; Greenbaum, P.E.; Henderson, C.E. Impact of psychiatric comorbidity on treatment of adolescent drug abusers. J. Subst. Abus. Treat. 2004, 26, 129–140. [Google Scholar] [CrossRef]
- Armstrong, T.D.; Costello, E.J. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J. Consult. Clin. Psychol. 2002, 70, 1224. [Google Scholar] [CrossRef]
- Baker, K.D.; Lubman, D.I.; Cosgrave, E.M.; Killackey, E.J.; Yuen, H.P. Impact of co-occuring substance use on 6 month outcomes for young people seeking mental health treatment. Aust. N. Z. J. Psychiatry 2007, 41, 896–902. [Google Scholar] [CrossRef]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R. Adolescent psychopathology: III. The clinical consequences of comorbidity. J. Am. Acad. Child Adolesc. Psychiatry 1995, 34, 510–519. [Google Scholar] [CrossRef]
- Riggs, P.D.; Whitmore, E.A. Substance Use Disorders and Disruptive Behaviour Disorders. In Disruptive Behaviour Disorders in Children and Adolescents; Hendren, R.L., Ed.; APA Press: Washington, DC, USA, 1999; pp. 133–173. [Google Scholar]
- Lubman, D.I.; Allen, N.B.; Rogers, N.; Cementon, E.; Bonomo, Y. The impact of co-occurring mood and anxiety disorders among substance-abusing youth. J. Affect. Disord. 2007, 103, 105–112. [Google Scholar] [CrossRef]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clin. Psychol. Rev. 1998, 18, 765–794. [Google Scholar] [CrossRef]
- Marmorstein, N.R.; Iacono, W.G.; Malone, S.M. Longitudinal associations between depression and substance dependence from adolescence through early adulthood. Drug Alcohol Depend. 2010, 107, 154–160. [Google Scholar] [CrossRef]
- O’Connell, M.E.; Boat, T.; Warner, K.E. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities; The National Academic Press: Washington, DC, USA, 2009. [Google Scholar]
- Hawkins, E.H. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annu. Rev. Psychol. 2009, 60, 197–227. [Google Scholar] [CrossRef] [PubMed]
- Angold, A.; Costello, E.J.; Erkanli, A. Comorbidity. J. Child Psychol. Psychiatry 1999, 40, 57–87. [Google Scholar] [CrossRef]
- Department of Health. Future in Mind. Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing; NHS: Leeds, UK, 2015.
- Sadler, K.; Vizard, T.; Ford, T.; Goodman, A.; Goodman, R.; McManus, S. Mental Health of Children and Young People in England, 2017: Trends and Characteristics; NHS Digital: Leeds, UK, 2018. [Google Scholar]
- Lewinsohn, P.M.; Shankman, S.A.; Gau, J.M.; Klein, D.N. The prevalence and co-morbidity of subthreshold psychiatric conditions. Psychol. Med. 2004, 34, 613. [Google Scholar] [CrossRef]
- Sterling, S.; Weisner, C.; Hinman, A.; Parthasarathy, S. Access to Treatment for Adolescents With Substance Use and Co-Occurring Disorders:Challenges and Opportunities. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 637–726. [Google Scholar]
- Salom, C.L.; Kelly, A.B.; Alati, R.; Williams, G.M.; Patton, G.C.; Williams, J.W. Individual, school-related and family characteristics distinguish co-occurrence of drinking and depressive symptoms in very young adolescents. Drug Alcohol Rev. 2016, 35, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Edwards, A.C.; Shivola, E.; Korhonen, T.; Pulkkinen, L.; Moilanen, I.; Kaprio, J.; Rose, R.J.; Dick, D.M. Depressive Symptoms and Alcohol Use are Genetically and Environmentally Correlated Across Adolescence. Behav. Genet. 2010, 41, 476–487. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Treur, J.L.; Munafò, M.R.; Logtenberg, E.; Wiers, R.W.; Verweij, K.J. Using mendelian randomization analysis to better understand the relationship between mental health and substance use: A systematic review. Psychol. Med. 2021, 51, 1593–1624. [Google Scholar] [CrossRef]
- Mason, W.A.; Hawkins, J.D.; Kosterman, R.; Catalano, R.F. Alcohol use disorders and depression: Protective factors in the development of unique versus comorbid outcomes. J. Child Adolesc. Subst. Abus. 2010, 19, 309–323. [Google Scholar] [CrossRef]
- Monahan, K.C.; Oesterle, S.; Rhew, I.; Hawkins, J.D. The relation between risk and protective factors for problem behaviors and depressive symptoms, antisocial behavior, and alcohol use in adolescence. J. Community Psychol. 2014, 42, 621–638. [Google Scholar] [CrossRef]
- Windle, M.; Davies, P.T. Depression and heavy alcohol use among adolescents: Concurrent and prospective relations. Dev. Psychopathol. 1999, 11, 823–844. [Google Scholar] [CrossRef]
- Department for Education; Department of Health. Transforming Children and Young People’s Mental Health Provision: A Green Paper; APS Group: London, UK, 2017.
- Wahlbeck, K. Public mental health: The time is ripe for translation of evidence into practice. World Psychiatry 2015, 14, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Henderson, J.L.; Brownlie, E.; McMain, S.; Chaim, G.; Wolfe, D.A.; Rush, B.; Boritz, T.; Beitchman, J.H. Enhancing prevention and intervention for youth concurrent mental health and substance use disorders: The Research and Action for Teens study. Early Interv. Psychiatry 2019, 13, 110–119. [Google Scholar] [CrossRef]
- Bukstein, O.G.; Horner, M.S. Management of the adolescent with substance use disorders and comorbid psychopathology. Child Adolesc. Psychiatr. Clin. 2010, 19, 609–623. [Google Scholar] [CrossRef] [PubMed]
- Van Ryzin, M.J.; Roseth, C.J.; Fosco, G.; Lee, Y.K.; Chen, I. A component-centered meta-analysis of family-based prevention programs for adolescent substance use. Clin. Psychol. Rev. 2016, 45, 72–80. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence [CG115]. Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking (High-Risk Drinking) and Alcohol Dependence. Available online: https://www.nice.org.uk/guidance/cg115 (accessed on 29 June 2023).
- Smit, E.; Verdurmen, J.; Monshouwer, K.; Smit, F. Family interventions and their effect on adolescent alcohol use in general populations; a meta-analysis of randomized controlled trials. Drug Alcohol Depend. 2008, 97, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Foxcroft, D.R.; Tsertsvadze, A. Universal family-based prevention programs for alcohol misuse in young people (Review). Cochrane Database Syst. Rev. 2011, 9, CD009308. [Google Scholar] [CrossRef]
- Carr, A. The evidence base for family therapy and systemic interventions for child-focused problems. J. Fam. Ther. 2014, 36, 107–157. [Google Scholar] [CrossRef]
- Kaslow, N.J.; Broth, M.R.; Smith, C.O.; Collins, M.H. Family-based interventions for child and adolescent disorders. J. Marital Fam. Ther. 2012, 38, 82–100. [Google Scholar] [CrossRef]
- Patel, V.; Fisher, A.J.; Hetrick, S.; McGorry, P.D. Mental Health of young people: A global public-health challenge. Lancet 2007, 369, 1302–1313. [Google Scholar] [CrossRef]
- Currie, C.; Zanotti, C.; Morgan, A.; Currie, D.; de Looze, M.; Roberts, C. Social determinants of health and wellbeing among young people. In Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2009/2010 Survey, Health Policy for Children and Adolescents, No. 6; WHO Regional Office for Europe: Copenhagen, Denmark, 2012. [Google Scholar]
- Office of Public Sector Information. Children and Young Persons Act. Camb. Law J. 1934, 5, 283–285. [Google Scholar]
- Merry, S.N.; Hetrick, S.E.; Cox, G.R.; Brudevold-Iversen, T.; Bir, J.J.; McDowell, H. Cochrane Review: Psychological and educational interventions for preventing depression in children and adolescents. Evid.-Based Child Health Cochrane Rev. J. 2012, 7, 1409–1685. [Google Scholar] [CrossRef]
- Kumpfer, K.L.; Alexander, J.F.; McDonals, L.; Olds, D.L. Family-focused substance abuse prevention: What has been learned from other fields. In Drug Abuse Prevention through Family Intervention; Ashery, R.S., Robertson, E.B., Kumpfer, K.L., Eds.; National Institute of Drug Abuse: Rockville, MD, USA, 1998; pp. 78–102. [Google Scholar]
- Karlsson, P.; Bergmark, A. Compared with what? An analysis of control-group types in Cochrane and Campbell reviews of psychosocial treatment efficacy with substance use disorders. Addiction 2014, 110, 420–428. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Chapter 8: Assessing Risk of Bias in Included Studies. Available online: https://handbook-5-1.cochrane.org/ (accessed on 10 May 2023).
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Griffin, J.W.; Furukawa, T.A. The lack of statistical power of subgroup analyses in meta-analyses: A cautionary note. Epidemiol. Psychiatr. Sci. 2021, 30, e78. [Google Scholar] [CrossRef] [PubMed]
- Hogue, A.; Dauber, S.; Henderson, C.E.; Bobek, M.; Johnson, C.; Lichvar, E.; Morgenstern, J. Randomized trial of family therapy versus nonfamily treatment for adolescent behavior problems in usual care. J. Clin. Child Adolesc. Psychol. 2015, 44, 954–969. [Google Scholar] [CrossRef]
- Mason, W.A.; Haggerty, K.P.; Fleming, A.P.; Casey-Goldstein, M. Family Intervention to Prevent Depression and Substance Use among Adolescents of Depressed Parents. J. Child Fam. Stud. 2012, 21, 891–905. [Google Scholar] [CrossRef]
- Poole, L.A.; Knight, T.; Toumbourou, J.W.; Lubman, D.I.; Bertino, M.D.; Lewis, A.J. A randomized controlled trial of the impact of a family-based adolescent depression intervention on both youth and parent mental health outcomes. J. Abnorm. Child Psychol. 2018, 46, 169–181. [Google Scholar] [CrossRef]
- Slesnick, N.; Prestopnik, J.L. Comparison of family therapy outcome with alcohol-abusing, runaway adolescents. J. Marital Fam. Ther. 2009, 35, 255–277. [Google Scholar] [CrossRef]
- Slesnick, N.; Erdem, G.; Bartle-Haring, S.; Brigham, G.S. Intervention with substance-abusing runaway adolescents and their families: Results of a randomized clinical trial. J. Consult. Clin. Psychol. 2013, 81, 600. [Google Scholar] [CrossRef]
- The Cochrane Collaboration. Chapter 9: Analysing Data and Undertaking Meta-Analyses. Available online: https://handbook-5-1.cochrane.org/ (accessed on 10 May 2023).
- Pantin, H.; Prado, G.; Lopez, B.; Huang, S.; Tapia, M.I.; Schwartz, S.J.; Sabillon, E.; Brown, C.H.; Branchini, J. A randomized controlled trial of Familias Unidas for Hispanic adolescents with behavior problems. Psychosom. Med. 2009, 71, 987. [Google Scholar] [CrossRef]
- Perrino, T.; Brincks, A.; Howe, G.; Brown, C.H.; Prado, G.; Pantin, H. Reducing internalizing symptoms among high-risk, Hispanic adolescents: Mediators of a preventive family intervention. Prev. Sci. 2016, 17, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Prado, G.; Huang, S.; Cordova, D.; Malcolm, S.; Estrada, Y.; Cano, N.; Maldonado-Molina, M.; Bacio, G.; Rosen, A.; Pantin, H. Ecodevelopmental and intrapersonal moderators of a family based preventive intervention for Hispanic youth: A latent profile analysis. Prev. Sci. 2013, 14, 290–299. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Valdez, A.; Cepeda, A.; Parrish, D.; Horowitz, R.; Kaplan, C. An adapted brief strategic family therapy for gang-affiliated Mexican American adolescents. Res. Soc. Work Pract. 2013, 23, 383–396. [Google Scholar] [CrossRef]
- Stanger, C.; Scherer, E.A.; Babbin, S.F.; Ryan, S.R.; Budney, A.J. Abstinence based incentives plus parent training for adolescent alcohol and other substance misuse. Psychol. Addict. Behav. 2017, 31, 385. [Google Scholar] [CrossRef]
- Tucker, J.S.; Edelen, M.O.; Huang, W. Effectiveness of parent–child mediation in improving family functioning and reducing adolescent problem behavior: Results from a pilot randomized controlled trial. J. Youth Adolesc. 2017, 46, 505–515. [Google Scholar] [CrossRef]
- Henggeler, S.W.; Pickrel, S.G.; Brondino, M.J. Multisystemic treatment of substance-abusing and-dependent delinquents: Outcomes, treatment fidelity, and transportability. Ment. Health Serv. Res. 1999, 1, 171–184. [Google Scholar] [CrossRef]
- Liddle, H.A.; Dakof, G.A.; Rowe, C.L.; Henderson, C.; Greenbaum, P.; Wang, W.; Alberga, L. Multidimensional Family Therapy as a community-based alternative to residential treatment for adolescents with substance use and co-occurring mental health disorders. J. Subst. Abus. Treat. 2018, 90, 47–56. [Google Scholar] [CrossRef]
- Liddle, H.A.; Dakof, G.A.; Parker, K.; Diamond, G.S.; Barrett, K.; Tejeda, M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. Am. J. Drug Alcohol Abus. 2001, 27, 651–688. [Google Scholar] [CrossRef]
- Henggeler, S.W.; Pickrel, S.G.; Brondino, M.J.; Crouch, J.L. Eliminating (almost) treatment dropout of substance abusing or dependent delinquents through home-based multisystemic therapy. Am. J. Psychiatry 1996, 153, 427–428. [Google Scholar]
- Wolff, J.; Esposito-Smythers, C.; Frazier, E.; Stout, R.; Gomez, J.; Massing-Schaffer, M.; Nestor, B.; Cheek, S.; Graves, H.; Yen, S. A randomized trial of an integrated cognitive behavioral treatment protocol for adolescents receiving home-based services for co-occurring disorders. J. Subst. Abus. Treat. 2020, 116, 108055. [Google Scholar] [CrossRef]
- Slesnick, N.; Guo, X.; Feng, X. Change in parent-and child-reported internalizing and externalizing behaviors among substance abusing runaways: The effects of family and individual treatments. J. Youth Adolesc. 2013, 42, 980–993. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Slesnick, N.; Feng, X. Reductions in depressive symptoms among substance-abusing runaway adolescents and their primary caretakers: A randomized clinical trial. J. Fam. Psychol. 2014, 28, 98. [Google Scholar] [CrossRef] [PubMed]
- Santisteban, D.A.; Coatsworth, J.; Perez-Vidal, A.; Kurtines, W.M.; Schwartz, S.J.; LaPerriere, A.; Szapocznik, J. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. J. Fam. Psychol. 2003, 17, 121–133. [Google Scholar] [CrossRef]
- Slesnick, N.; Bartle-Haring, S.; Erdem, G.; Budde, H.; Letcher, A.; Bantchevska, D.; Patton, R. Troubled parents, motivated adolescents: Predicting motivation to change substance use among runaways. Addict. Behav. 2009, 34, 675–684. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gilligan, C.; Wolfenden, L.; Foxcroft, D.R.; Williams, A.J.; Kingsland, M.; Hodder, R.K.; Stockings, E.; McFadyen, T.R.; Tindall, J.; Sherker, S. Family-based prevention programmes for alcohol use in young people. Cochrane Database Syst. Rev. 2019, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- MacArthur, G.; Caldwell, D.M.; Redmore, J.; Watkins, S.H.; Kipping, R.; White, J.; Chittleborough, C.; Langford, R.; Er, V.; Lingam, R. Individual-, family-, and school-level interventions targeting multiple risk behaviours in young people. Cochrane Database Syst. Rev. 2018, 10, CD009927. [Google Scholar] [CrossRef]
- Lawrence, P.J.; Parkinson, M.; Jasper, B.; Creswell, C.; Halligan, S.L. Supporting the parents of children and young people with anxiety and depressive disorders is an opportunity not to be missed: A scoping review. Lancet Psychiatry 2021, 8, 909–918. [Google Scholar] [CrossRef]
- Honey, A.; Alchin, S.; Hancock, N. Promoting mental health and wellbeing for a young person with a mental illness: Parent occupations. Aust. Occup. Ther. J. 2014, 61, 194–203. [Google Scholar] [CrossRef]
- Arango, C.; Díaz-Caneja, C.M.; McGorry, P.D.; Rapoport, J.; Sommer, I.E.; Vorstman, J.A.; McDaid, D.; Marín, O.; Serrano-Drozdowskyj, E.; Freedman, R. Preventive strategies for mental health. Lancet Psychiatry 2018, 5, 591–604. [Google Scholar] [CrossRef]
- McGovern, R.; Smart, D.; Alderson, H.; Araújo-Soares, V.; Brown, J.; Buykx, P.; Evans, V.; Fleming, K.; Hickman, M.; Macleod, J. Psychosocial interventions to improve psychological, social and physical wellbeing in family members affected by an adult relative’s substance use: A systematic search and review of the evidence. Int. J. Environ. Res. Public Health 2021, 18, 1793. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed]
- Panter-Brick, C.; Burgess, A.; Eggerman, M.; McAllister, F.; Pruett, K.; Leckman, J.F. Practitioner review: Engaging fathers–recommendations for a game change in parenting interventions based on a systematic review of the global evidence. J. Child Psychol. Psychiatry 2014, 55, 1187–1212. [Google Scholar] [CrossRef] [PubMed]
- Bentley, G.R. Substitute Parents: Biological and Social Perspective on Alloparenting across Human Societies; Berghahn Books: New York, NY, USA, 2009; Volume 3. [Google Scholar]
- McGovern, R.; Gilivarry, E.; Addison, M.; Alderson, H.; Geijer-Simpson, E.; Lingam, R.; Smart, D.; Kaner, E. The association between adverse child health, psychological, educational and social outcomes, and nondependent parental substance: A rapid evidence assessment. Trauma Violence Abus. 2018, 21, 470–483. [Google Scholar] [CrossRef] [PubMed]
- Lieb, R.; Isensee, B.; Hofler, M.; Pfister, H.; Wittchen, H.U. Parental major depression and the risk of depression and other mental disorders in offspring. Arch. Gen. Psychiatry 2002, 59, 365–374. [Google Scholar] [CrossRef]
- Edwards, A.C.; Joinson, C.; Dick, D.M.; Kendler, K.S.; Macleod, J.; Munafo, M.; Hickman, M.; Lewis, G.; Heron, J. The association between depressive symptoms from early to late adolescence and later use and harmful use of alcohol. Eur. Child Adolesc. Psychiatry 2014, 23, 1219–1230. [Google Scholar] [CrossRef]
- Garey, L.; Olofsson, H.; Garza, T.; Rogers, A.H.; Kauffman, B.Y.; Zvolensky, M.J. Directional effects of anxiety and depressive disorders with substance use: A review of recent prospective research. Curr. Addict. Rep. 2020, 7, 344–355. [Google Scholar] [CrossRef]
- Salom, C.L.; Williams, G.M.; Najman, J.M.; Alati, R. Familial factors associated with development of alcohol and mental health comorbidity. Addiction 2015, 110, 248–257. [Google Scholar] [CrossRef]
- Allen, D.; Coombes, L.; Foxcroft, D.R. Cultural accommodation of the strenthening families programme 10-14: UK Phase I Study. Health Educ. Res. 2007, 22, 547–560. [Google Scholar] [CrossRef]


| Identifier | Recruitment | Sample | Sample Size | Interventions | Intervention Hours | Control | Outcomes | Follow-Up Time Points | Study Design |
|---|---|---|---|---|---|---|---|---|---|
| Targeted Interventions | |||||||||
| Mason et al., 2012 [46] USA | Healthcare clinics and therapeutic centres |
| 24 adolescents and their families | Project Hope Content: family functioning, parenting techniques and young people’s coping skills/substance refusal skills. Delivery: Separate adolescent and whole family sessions. | 10 × 90- min sessions | Waitlist control group |
| Post-test | Pilot feasibility Randomised controlled trials—2 arms |
| Pantin et al., 2009 [51] USA | Hispanic middle schools |
| 213 8th grade Hispanic adolescents and their families | Familias Unidas Content: Family functioning and parenting techniques Delivery: Adolescent involvement limited to family visits | 9 × 2 h group parent sessions, 10 × 1 h family visits and 4 × 1 h booster sessions | Community control: Referrals to agencies providing services behaviour problems. |
| 6,18 & 30 months post-baseline | Randomised controlled trial—2 arms |
| Santisteban et al., 2003 [64] USA | Self-referred or referred by a school counsellor |
| 126 Hispanic adolescents and families with | Brief Strategic Family Therapy Content: Family functioning Delivery: Whole family sessions | Approximately 20 × 1 h weekly sessions (amount dependent on the clinical severity) | The Group Control Condition: Participatory learning group. 6–16 sessions × 90 min. |
| Post-test | Randomised trial—2 arms |
| Valdez et al., 2013 [54] USA | Field-intensive outreach and street-based recruitment |
| 200 Mexican-American adolescents and their families. | Adapted Brief Strategic Family Therapy Content: Family functioning, school engagement, gang diversion and awareness. Delivery: Family, caregiver and adolescent sessions. | 12–16 × 1–1.5-h sessions | Social and Behavioural Health Services and Substance Abuse Counselling: Some family involvement. |
| Post-test & 6 months post-test | Randomised trial—2 arms |
| Treatment based interventions | |||||||||
| Henggeler Pickrel and Brondino, 1999 [57] USA | Department of Juvenile Justice |
| 118 adolescents and their families | Multisystemic Therapy Content: Family functioning and parenting techniques. Delivery: Family composition within sessions is not provided. Medication available | Length determined by clinical need. | Usual Community Services: Outpatient substance use services and/or mental health inpatient and outpatient services |
| Post-test and 6 months post-test | Randomised controlled trial |
| Hogue et al., 2015 [45] USA | Community referral network |
| 205 adolescents and their families. | Non-manualised Family Therapy Content: Family functioning and parenting techniques Delivery: Whole family sessions only. | Average of 9 sessions | Usual Care Other: Access to five outpatient clinics. Weekly treatment sessions and psychiatric support. |
| 3,6,9,12-months post-baseline | Randomised controlled trial—2 arms |
| Liddle, 2001 USA [59] | Juvenile justice systems, schools, health and mental health agencies |
| 182 adolescents and their families. | Multidimensional Family Therapy Content: Family functioning and parenting techniques Delivery: Family, caregiver, and adolescent sessions. | 14–16 weekly 90-min sessions | Adolescent Group Therapy: 14–16 weekly 90 min sessions. Included family sessions. Multifamily educational intervention 14–16 weekly 90 min group family sessions. Individual family crisis sessions |
| 12 months post-intervention | Randomised controlled trial |
| Liddle et al., 2018 [58] USA | Referred and approved by Department of Children and Families |
| 113 adolescents and their families. | Multidimensional Family Therapy Content: Family functioning and parenting techniques. Psychiatric care and medication management also available. Delivery: Family, caregiver and adolescent sessions. | 3.28 h of sessions per week | Residential Substance Use Treatment: Included monthly parental support groups. Psychiatric care and medication available |
| 2,4,12,18-month post-baseline | Randomised controlled trial |
| Poole et al., 2018 [47] USA | Public mental health service, schools, and community mental health service |
| 64 adolescents and their families | Best Mood-Behavior Exchange Systems Therapy for adolescent depression Content: Family functioning, parenting techniques and young people’s coping skills Delivery: Half of the sessions involved adolescents and siblings. | 8 × 2 h multifamily group sessions and 1 × 2 h follow-up session | PAST (treatment as usual): Aimed to represent treatment as usual in Victoria, Australia, parenting groups |
| 3 months post- treatment | Randomised trial—2 arms |
| Slesnick and Prestopnik., 2009 [48] USA | Runaway Shelters |
| 119 adolescents and their families | Ecologically-Based Family Therapy (EBFT) Content: Family functioning and parenting techniques Delivery: Home-based, Family, caregiver and adolescent sessions. Functional Family Therapy Content: Family functioning and parenting techniques. Delivery: Office-based. Whole family sessions only. | 16 × 50 minute sessions | Service As Usual: Mainly case management and informal meetings or therapy provided/arranged by shelter staff. |
| 3,9,15 months post-baseline | Randomised controlled trial—3 arms |
| Slesnick et al., 2013 [49] USA | Runaway shelter |
| 179 young people and their families | Ecologically-Based Family Therapy (EBFT) Content: Family functioning and parenting techniques. Delivery: Family, caregiver and adolescent sessions. | 14 sessions | Community Reinforcement Approach (skills training): 14 sessions Motivational Interviewing: 2 sessions |
| 3,6,9, 12,18,24 months post-baseline | Randomised trial—2 arms |
| Stanger et al., 2017 [55] USA | Schools, justice system, therapists, physicians, or parents. |
| 75 young people and their families | Abstinence-based Fishbowl Program, Home-based Incentives and Consequences Program Content: Parenting techniques, incentives, and consequences for young people’s substance use. All young people also received individual MET/CBT Delivery: Separate sessions with caregivers and young people only. | Number of sessions was not reported | Attendance Based Incentives: Number and duration not provided. All young people received additional individual MET/CBT |
| 36 week follow up | Randomised controlled trial—2 arms |
| Tucker et al., 2016 [56] USA | A community-based agency |
| 111 young people and their families | Parent-Child Mediation Content: Family functioning. Delivery: Family, caregiver, and adolescent sessions. | 3 mediation sessions | Waitlist Control Group |
| 1.5, 3 months post-baseline | Pilot feasibility randomised controlled trial—2 arms |
| Wolff et al., 2020 [61] USA | A community mental health clinic |
| 111 young people and their families | Integrated-Cognitive Behavioural Treatment Content: Family functioning, parenting techniques, coping skills and alcohol refusal skills in young people. Delivery: Family, caregiver, and adolescent sessions. | 30 min-3 h, up to 3 times a week. | Treatment as Usual: Could include eclectic, flexible treatment |
| 3,6,12 months post-baseline | Randomised controlled trial—2 arms |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geijer-Simpson, E.; Kaner, E.; Lingam, R.; McArdle, P.; McGovern, R. Effectiveness of Family-Involved Interventions in Reducing Co-Occurring Alcohol Use and Mental Health Problems in Young People Aged 12–17: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 6890. https://doi.org/10.3390/ijerph20196890
Geijer-Simpson E, Kaner E, Lingam R, McArdle P, McGovern R. Effectiveness of Family-Involved Interventions in Reducing Co-Occurring Alcohol Use and Mental Health Problems in Young People Aged 12–17: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(19):6890. https://doi.org/10.3390/ijerph20196890
Chicago/Turabian StyleGeijer-Simpson, Emma, Eileen Kaner, Raghu Lingam, Paul McArdle, and Ruth McGovern. 2023. "Effectiveness of Family-Involved Interventions in Reducing Co-Occurring Alcohol Use and Mental Health Problems in Young People Aged 12–17: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 19: 6890. https://doi.org/10.3390/ijerph20196890
APA StyleGeijer-Simpson, E., Kaner, E., Lingam, R., McArdle, P., & McGovern, R. (2023). Effectiveness of Family-Involved Interventions in Reducing Co-Occurring Alcohol Use and Mental Health Problems in Young People Aged 12–17: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(19), 6890. https://doi.org/10.3390/ijerph20196890





