Knowledge and Attitudes towards HIV and HCV among the Population Attending the Fast-Track Cities Mobile Unit in Brescia, Italy
Abstract
1. Background
2. Methods
2.1. Study Design
2.2. Participants and Settings Population
2.3. Questionnaire
2.4. Analysis
3. Results
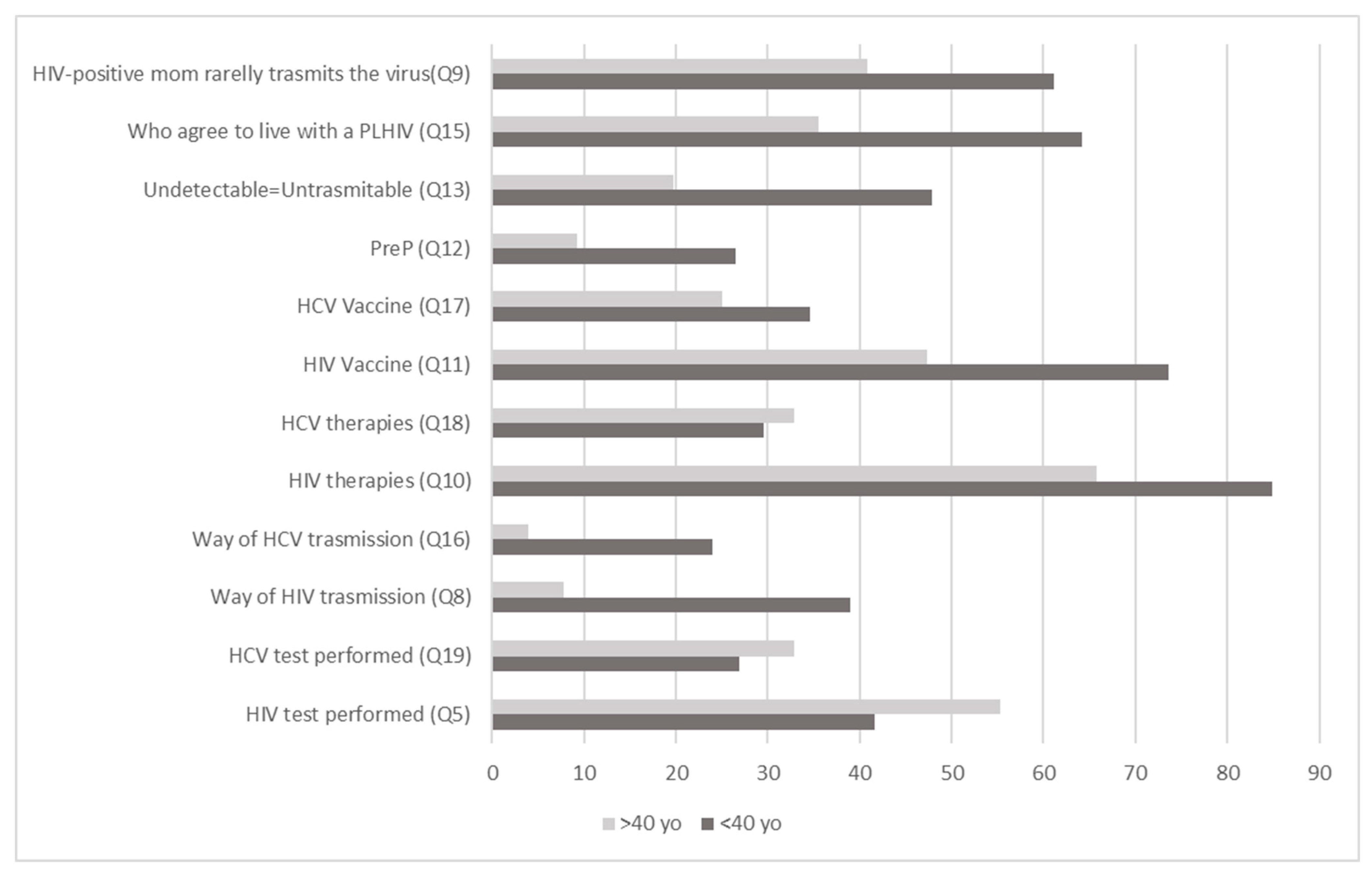
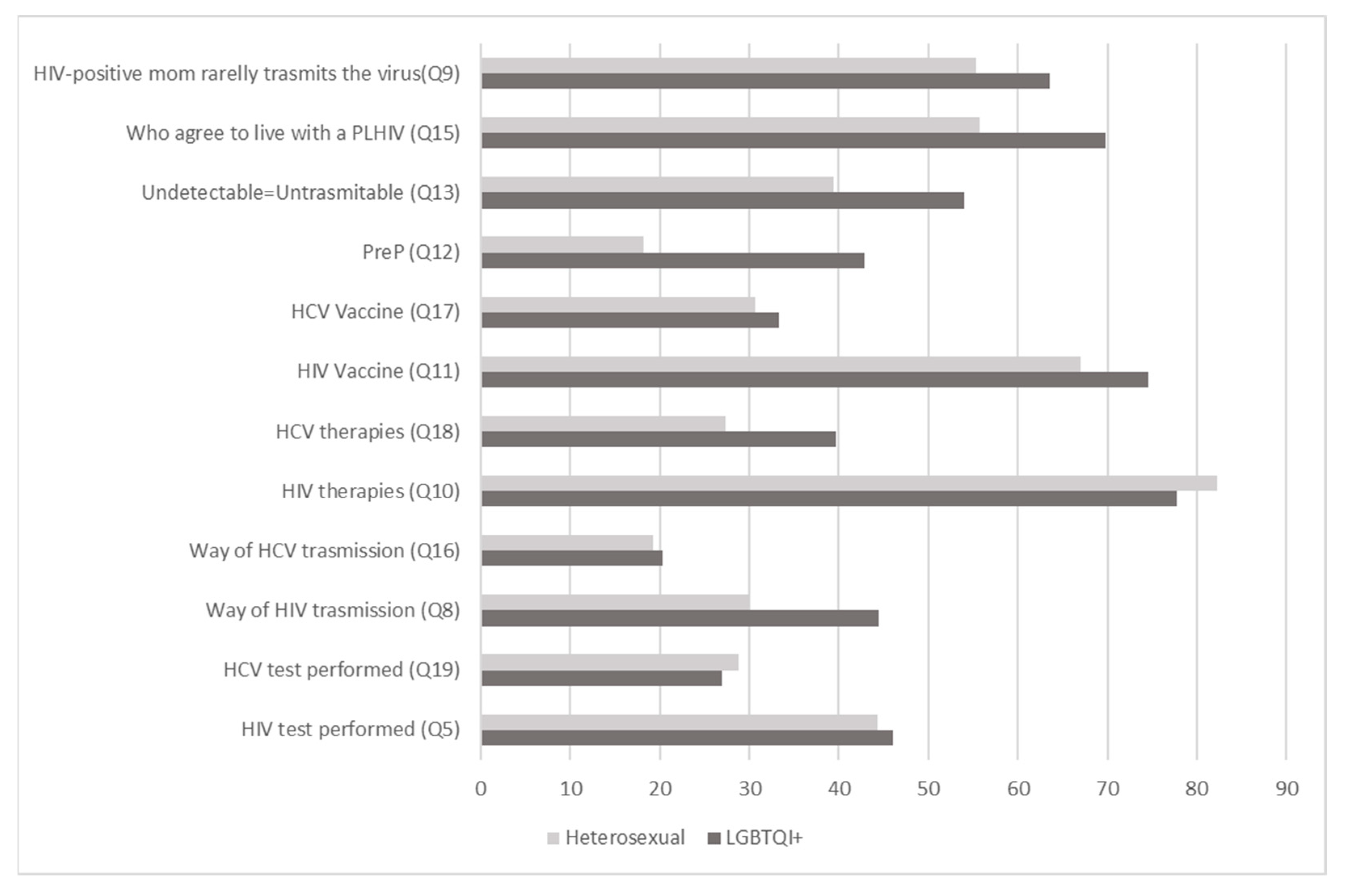
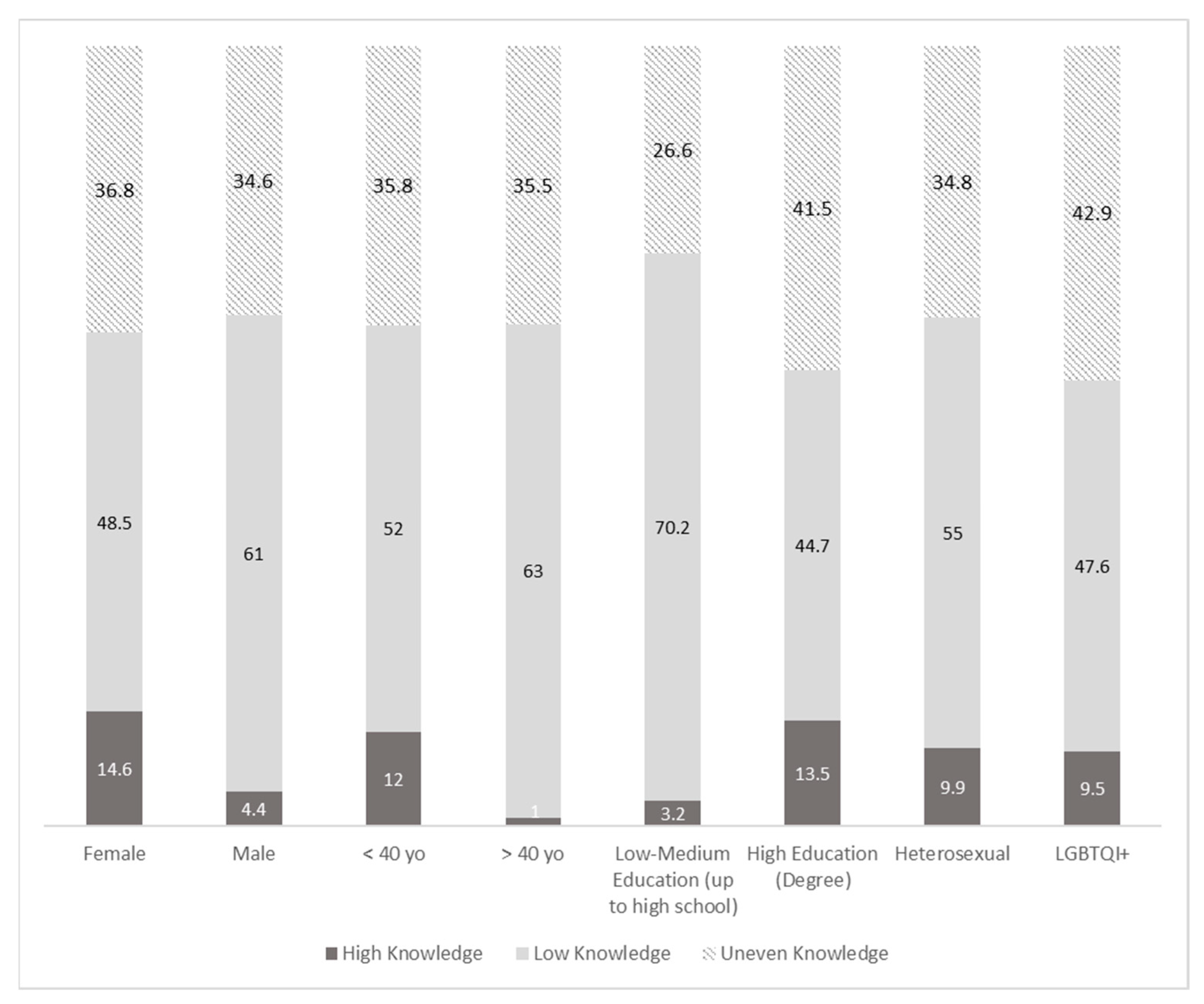
3.1. HIV Knowledge and Attitudes
3.2. Hepatitis C Virus Knowledge
3.3. Comparing HIV and HCV Knowledge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Welcome to Fast-Track Cities|Fast-Track Cities. Available online: https://www.fast-trackcities.org/ (accessed on 12 April 2023).
- ATS Brescia, Banca Dati Assistiti Integrata: Presa in Carico Nel 2020. Available online: https://www.ats-brescia.it/documents/3432658/8478812/BDA2020B.pdf/45e31d1b-38e8-67f7-35ba-452ed9887a58 (accessed on 1 August 2023).
- About European Testing Week. Available online: https://www.testingweek.eu/about-european-testing-week/ (accessed on 12 April 2023).
- Fonner, V.A.; Denison, J.; Kennedy, C.E.; O’Reilly, K.; Sweat, M. Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane Database Syst. Rev. 2012, 9, CD001224. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Sessa, A.; Mollo, S.; Corbisiero, N.; Angelillo, I.F.; Collaborative Working Group. Knowledge, attitudes, and behaviors regarding HIV among first time attenders of voluntary counseling and testing services in Italy. BMC Infect. Dis. 2013, 13, 277. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mazzitelli, M.; Caridà, G.; Scigliano, C.; Vallone, M.C.; Pirrò, F.; Lombardo, M.R.; Clemente, G.; Bernaudo, F.; Postorino, M.C.; Strazzulla, A.; et al. Knowledge of HIV infection and transmission: A knowledge, attitudes, beliefs and practices (KABP) survey among a sample of students at the “Magna Graecia”, University of Catanzaro. Ann. Dell’istituto Super. Sanità 2016, 52, 530–535. [Google Scholar] [CrossRef]
- Loconsole, D.; Metallo, A.; Bruno, V.; De Robertis, A.L.; Morea, A.; Quarto, M.; Chironna, M. HIV awareness: A kap study among students in Italy reveals that preventive campaigns still represent a public health priority. Ann Ig. 2020, 32, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Licata, F.; Angelillo, S.; Oliverio, A.; Di Gennaro, G.; Bianco, A. How to Safeguard University Students Against HIV Transmission? Results of a Cross-Sectional Study in Southern Italy. Front. Med. 2022, 9, 903596. [Google Scholar] [CrossRef] [PubMed]
- ISTAT Resident Population by Gender, Age, and Marital Status as of 1 January 2021. Available online: http://dati-censimentopopolazione.istat.it/ (accessed on 1 August 2023).
- Jun, S.P.; Yoo, H.S.; Lee, J.S. The impact of the pandemic declaration on public awareness and behavior: Focusing on COVID-19 google searches. Technol. Forecast Soc. Chang. 2021, 166, 120592. [Google Scholar] [CrossRef]
- Sallam, M.; Alabbadi, A.M.; Abdel-Razeq, S.; Battah, K.; Malkawi, L.; Al-Abbadi, M.A.; Mahafzah, A. HIV Knowledge and Stigmatizing Attitude towards People Living with HIV/AIDS among Medical Students in Jordan. Int. J. Environ. Res. Public Health 2022, 19, 745. [Google Scholar] [CrossRef]
- Li, X.; Yuan, L.; Li, X.; Shi, J.; Jiang, L.; Zhang, C.; Yang, X.; Zhang, Y.; Zhao, D.; Zhao, Y. Factors associated with stigma attitude towards people living with HIV among general individuals in Heilongjiang, Northeast China. BMC Infect. Dis. 2017, 17, 154. [Google Scholar] [CrossRef]
- Qashqari, F.S.; Alsafi, R.T.; Kabrah, S.M.; AlGary, R.A.; Naeem, S.A.; Alsulami, M.S.; Makhdoom, H. Knowledge of HIV/AIDS transmission modes and attitudes toward HIV/AIDS infected people and the level of HIV/AIDS awareness among the general population in the kingdom of Saudi Arabia: A cross-sectional study. Front. Public Health 2022, 10, 955458. [Google Scholar] [CrossRef]
- Walters, S.M.; Rivera, A.V.; Starbuck, L.; Reilly, K.H.; Boldon, N.; Anderson, B.J.; Braunstein, S. Differences in Awareness of Pre-exposure Prophylaxis and Post-exposure Prophylaxis Among Groups At-Risk for HIV in New York State: New York City and Long Island, NY, 2011–2013. JAIDS J. Acquir. Immune Defic. Syndr. 2017, 75 (Suppl. S3), S383–S391. [Google Scholar] [CrossRef]
- Mereu, A.; Liori, A.; Fadda, L.; Puddu, M.; Chessa, L.; Contu, P.; Sardu, C. What do young people know about HIV? Results of a cross sectional study on 18–24-year-old students. J. Prev. Med. Hyg. 2022, 63, E541–E548. [Google Scholar] [CrossRef] [PubMed]
- Arifin, H.; Ibrahim, K.; Rahayuwati, L.; Herliani, Y.K.; Kurniawati, Y.; Pradipta, R.O.; Sari, G.M.; Ko, N.Y.; Wiratama, B.S. HIV-related knowledge, information, and their contribution to stigmatization attitudes among females aged 15–24 years: Regional disparities in Indonesia. BMC Public Health 2022, 22, 637. [Google Scholar] [CrossRef] [PubMed]
- Merakou, K.; Costopoulos, C.; Marcopoulou, J.; Kourea-Kremastinou, J. Knowledge, attitudes and behaviour after 15 years of HIV/AIDS prevention in schools. Eur. J. Public Health 2002, 12, 90–93. [Google Scholar] [CrossRef]
- EpiCentro Aids—Aspetti Epidemiologici in Italia. Available online: https://www.epicentro.iss.it/aids/epidemiologia-italia (accessed on 13 April 2023).
- Hebo, H.J.; Gemeda, D.H.; Abdusemed, K.A. Hepatitis B and C Viral Infection: Prevalence, Knowledge, Attitude, Practice, and Occupational Exposure among Healthcare Workers of Jimma University Medical Center, Southwest Ethiopia. Sci. World J. 2019, 2019, 9482607. [Google Scholar] [CrossRef]
- Sultan, N.Y.; YacoobMayet, A.; Alaqeel, S.A.; Al-Omar, H.A. Assessing the level of knowledge and available sources of information about hepatitis C infection among HCV-infected Egyptians. BMC Public Health 2018, 18, 747. [Google Scholar] [CrossRef]
- Alzahrani, M.S.; Ayn Aldeen, A.; Almalki, R.S.; Algethami, M.B.; Altowairqi, N.F.; Alzahrani, A.; Almalki, A.S.; Alzhrani, R.M.; Algarni, M.A. Knowledge of and Testing Rate for Hepatitis C Infection among the General Public of Saudi Arabia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 2080. [Google Scholar] [CrossRef] [PubMed]
- Mtengezo, J.; Lee, H.; Ngoma, J.; Kim, S.; Aronowitz, T.; DeMarco, R.; Shi, L. Knowledge and Attitudes toward HIV, Hepatitis B Virus, and Hepatitis C Virus Infection among Health-care Workers in Malawi. Asia Pac. J. Oncol. Nurs. 2016, 3, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Camoni, L.; Regine, V.; Stanecki, K.; Salfa, M.C.; Raimondo, M.; Suligoi, B. Estimates of the number of people living with HIV in Italy. Biomed. Res. Int. 2014, 2014, 209619. [Google Scholar] [CrossRef]
- Adoba, P.; Boadu, S.K.; Agbodzakey, H.; Somuah, D.; Ephraim, R.K.; Odame, E.A. High prevalence of hepatitis B and poor knowledge on hepatitis B and C viral infections among barbers: A cross-sectional study of the Obuasi municipality, Ghana. BMC Public Health 2015, 15, 1041. [Google Scholar] [CrossRef]
- Chaquisse, E.; Meireles, P.; Fraga, S.; Mbofana, F.; Barros, H. Knowledge about HIV, HBV and HCV modes of transmission among pregnant women in Nampula—Mozambique. AIDS Care 2018, 30, 1161–1167. [Google Scholar] [CrossRef]
- Screening Gratuito per l’Epatite C. Available online: https://www.regione.lombardia.it/wps/portal/istituzionale/HP/DettaglioRedazionale/servizi-e-informazioni/cittadini/salute-e-prevenzione/Prevenzione-e-benessere/screening-gratuito-epatite-c/screening-gratuito-epatite-c (accessed on 13 April 2023).
- Liu, H.; Li, M.; Jin, M.; Jing, F.; Wang, H.; Chen, K. Public awareness of three major infectious diseases in rural Zhejiang province, China: A cross-sectional study. BMC Infect. Dis. 2013, 13, 192. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Health Days and Campaigns. Available online: https://www.who.int/campaigns (accessed on 17 April 2023).

| Biological Sex Q1 | F | M | Other | |||
| Age Q2 | 18–25 | 25–30 | 30–40 | 40–50 | 50–60 | >60 |
| Educational level Q3 | Primary School Diploma | Middle School Diploma | High School Diploma | High School Student | University Student | University Diploma |
| Sexual Orientation Q4 | Heterosexual | Homosexual | Bisexual | Fluid | Other | |
| HIV | ||||||
| Have you ever performed an HIV test before? Q5 | Yes | No | ||||
| Do you know where to perform the HIV test in your city? Q6 | Yes | No | ||||
| Do you know people living with HIV? Q7 | Yes, my partner | Yes, a relative | No | |||
| How HIV can be transmitted Q8 * more than one correct answer | Sharing cutlery | Mosquito bites | Infected blood | Saliva | Unprotected sex | Pregnancy |
| A mom living with HIV, regularly taking antiretroviral therapy can transmit the HIV virus during pregnancy: Q9 | Yes, in 90% of cases | Yes, in 50% of cases | In less than 1% of cases | |||
| With the current drug therapies, People living with HIV could have a quality of life similar to HIV-negative people Q10 | Yes | No | I do not know | |||
| Do you think there is a vaccine against HIV? Q11 | Yes | No | I do not know | |||
| Do you know what’s the PreP? Q12 | Yes | No | I do not know | |||
| People living with HIV, regularly taking antiretroviral therapy and having “viremia 0” can transmit the HIV virus Q13 | Yes | No | I do not know | |||
| Do you know the meaning of “Undetectable”? Q14 | Yes | No | I do not know | |||
| Do you agree to live with People living with HIV? Q15 | Yes | No | I do not know | |||
| HCV | ||||||
| HCV virus can be transmitted through * more than one correct answer Q16 | Mosquito bites | By air (cough or sneeze) | Unprotected sex | Infected blood | During the pregnancy | |
| There is a vaccine that prevents HCV Q17 | Yes | No | I do not know | |||
| The current therapies are able to treat the infection and eliminate the hepatitis virus HCV Q18 | Yes | No | I do not know | |||
| Have you ever performed an HCV test before? Q19 | Yes | No | I do not know |
| Overall | <40 | >40 | Heterosexual | LGBTQ+ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| TOT | 333 | 100.0 | 257 | 77.2 | 76 | 22.8 | 264 | 79.3 | 63 | 18.9 | |
| Biological Sex Q1 | F | 171 | 51.4 | 145 | 43.5 | 26 | 7.8 | 142 | 42.6 | 28 | 8.4 |
| M | 159 | 47.7 | 111 | 33.3 | 48 | 14.4 | 120 | 36.0 | 34 | 10.2 | |
| other | 3 | 0.9 | 1 | 0.3 | 2 | 0.6 | 2 | 0.6 | 1 | 0.3 | |
| Age Q2 | 18–25 | 170 | 51.1 | 170 | 51.0 | - | - | 136 | 40.8 | 34 | 10.2 |
| 25–30 | 57 | 17.1 | 57 | 17.1 | - | - | 43 | 12.9 | 13 | 3.9 | |
| 30–40 | 30 | 9.0 | 30 | 9.0 | - | - | 21 | 6.3 | 8 | 2.4 | |
| 40–50 | 19 | 5.7 | - | - | 19 | 5.7 | 17 | 5.1 | 0 | 0.0 | |
| 50–60 | 28 | 8.4 | - | - | 28 | 8.4 | 23 | 6.9 | 5 | 1.5 | |
| >60 | 29 | 8.7 | - | - | 29 | 8.7 | 24 | 7.2 | 3 | 0.9 | |
| Educational level Q3 | Primary School Diploma | 5 | 1.5 | 1 | 0.3 | 4 | 1.2 | 2 | 0.6 | 1 | 0.3 |
| Middle School Diploma | 27 | 8.1 | 7 | 2.1 | 20 | 6.0 | 22 | 6.6 | 3 | 0.9 | |
| High School Diploma | 58 | 17.4 | 32 | 9.6 | 26 | 7.8 | 51 | 15.3 | 7 | 2.1 | |
| High School Student | 34 | 10.2 | 28 | 8.4 | 6 | 1.8 | 22 | 6.6 | 11 | 3.3 | |
| University Student | 139 | 41.7 | 137 | 41.1 | 2 | 0.6 | 112 | 33.6 | 27 | 8.1 | |
| University Diploma | 68 | 20.4 | 50 | 15.0 | 18 | 5.4 | 53 | 15.9 | 14 | 4.2 | |
| NA | 2 | 0.6 | 2 | 0.6 | 0 | 0.0 | 2 | 0.6 | 0 | 0.0 | |
| Sexual Orientation Q | Heterosexual | 264 | 79.3 | 200 | 60.1 | 64 | 19.2 | 264 | 79.3 | - | - |
| Homosexual | 18 | 5.4 | 16 | 4.8 | 2 | 0.6 | - | - | 18 | 5.4 | |
| Bisexual | 35 | 10.5 | 32 | 9.6 | 3 | 0.9 | - | - | 35 | 10.5 | |
| Fluid | 4 | 1.2 | 4 | 1.2 | 0 | 0.0 | - | - | 4 | 1.2 | |
| Other | 6 | 1.8 | 3 | 0.9 | 3 | 0.9 | - | - | 6 | 1.8 | |
| NA | 6 | 1.8 | 2 | 0.6 | 4 | 1.2 | 6 | 1.8 | - | - | |
| High Knowledge of HIV | High Knowledge of HCV | |||||
|---|---|---|---|---|---|---|
| Log likelihood = −213.05 | Odds Ratio | p-Value | 95% CI | Odds Ratio | p-Value | 95% CI |
| Years of age—Ref. Category: < 40 | ||||||
| > 40 | 1.10 | 0.760 | 0.58–2.09 | 0.63 | 0.452 | 0.19–2.07 |
| Sex—Ref. Category: Female | ||||||
| Male | 0.71 | 0.162 | 0.44–1.14 | 0.52 | 0.099 | 0.24–1.13 |
| Sexual Orientation—Ref. Category: Heterosexual | ||||||
| LGBTQ+ | 1.19 | 0.562 | 0.65–2.17 | 1.10 | 0.825 | 0.44–2.74 |
| Education—Ref. Category: Primary and Middle school diploma | ||||||
| High School students and diploma | 2.38 | 0.119 | 0.79–7.12 | 1.72 | 0.640 | 0.17–17.16 |
| University students and diploma | 5.30 | 0.003 * | 1.77–15.89 | 54.44 | 0.189 | 1.48–41.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viola, F.; Formenti, B.; Arsuffi, S.; Polesini, I.; Focà, E.; Castelli, F.; Quiros-Roldan, E. Knowledge and Attitudes towards HIV and HCV among the Population Attending the Fast-Track Cities Mobile Unit in Brescia, Italy. Int. J. Environ. Res. Public Health 2023, 20, 6878. https://doi.org/10.3390/ijerph20196878
Viola F, Formenti B, Arsuffi S, Polesini I, Focà E, Castelli F, Quiros-Roldan E. Knowledge and Attitudes towards HIV and HCV among the Population Attending the Fast-Track Cities Mobile Unit in Brescia, Italy. International Journal of Environmental Research and Public Health. 2023; 20(19):6878. https://doi.org/10.3390/ijerph20196878
Chicago/Turabian StyleViola, Francesca, Beatrice Formenti, Stefania Arsuffi, Itala Polesini, Emanuele Focà, Francesco Castelli, and Eugenia Quiros-Roldan. 2023. "Knowledge and Attitudes towards HIV and HCV among the Population Attending the Fast-Track Cities Mobile Unit in Brescia, Italy" International Journal of Environmental Research and Public Health 20, no. 19: 6878. https://doi.org/10.3390/ijerph20196878
APA StyleViola, F., Formenti, B., Arsuffi, S., Polesini, I., Focà, E., Castelli, F., & Quiros-Roldan, E. (2023). Knowledge and Attitudes towards HIV and HCV among the Population Attending the Fast-Track Cities Mobile Unit in Brescia, Italy. International Journal of Environmental Research and Public Health, 20(19), 6878. https://doi.org/10.3390/ijerph20196878








