Caring for People with Rare Diseases: A Systematic Review of the Challenges of, and Strategies for Dealing with, COVID-19
Abstract
:1. Introduction
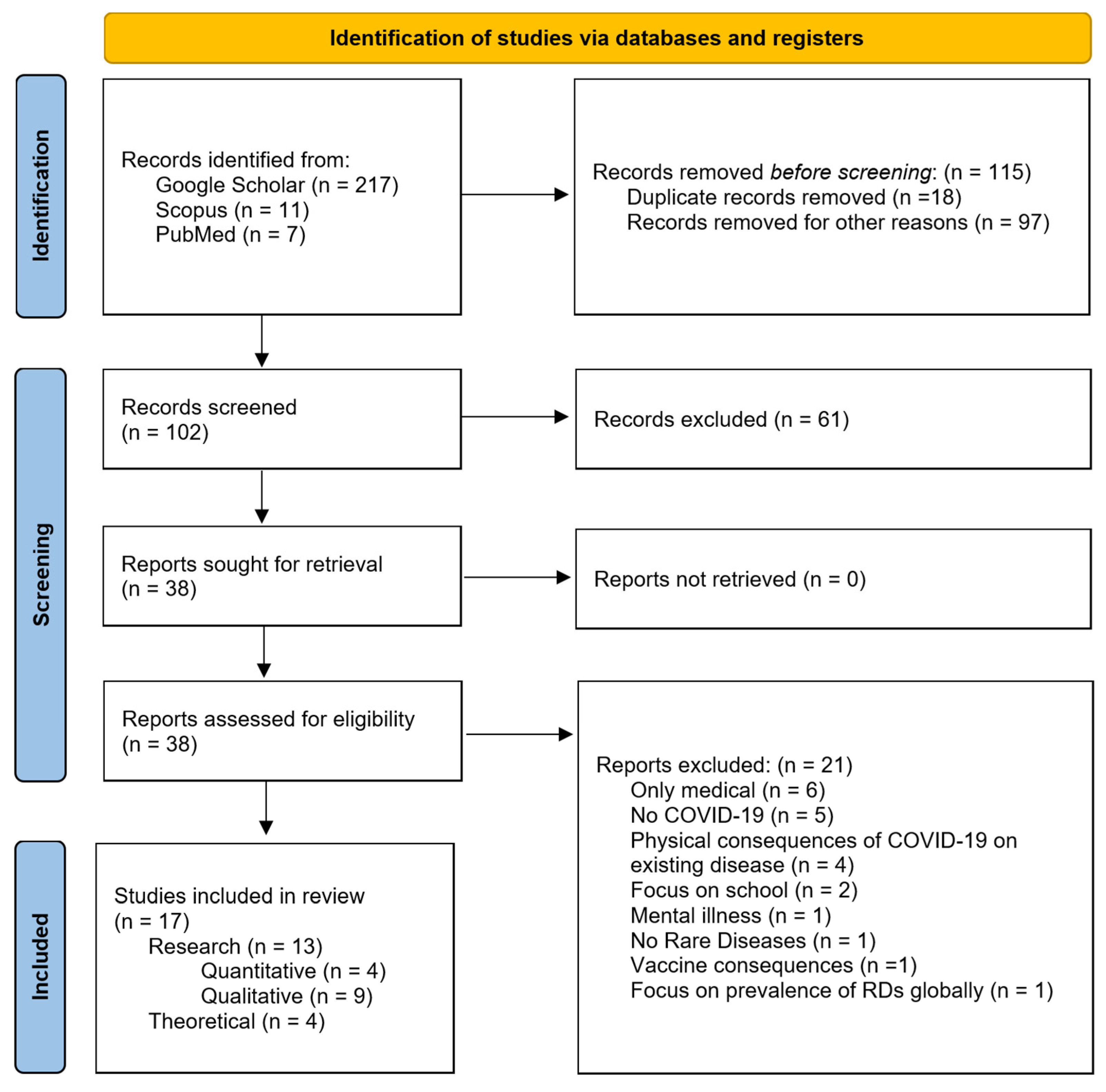
2. Materials and Methods
3. Results
3.1. Psychological and Social Points of View
3.1.1. Stress and Distress
3.1.2. Anxiety
3.1.3. Loneliness
3.1.4. Social Isolation
3.1.5. Depressive Moods
3.1.6. Psychosocial Burden
3.2. Points of View of People with RDs, FRCs, and RD Organisations
3.2.1. Experiences of People with RDs
3.2.2. Families, Relatives, and Caregivers
3.2.3. Organisations
3.3. Interventions
3.4. Coping with the Pandemic
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Aknin, L.B.; De Neve, J.-E.; Dunn, E.W.; Fancourt, D.E.; Goldberg, E.; Helliwell, J.F.; Jones, S.P.; Karam, E.; Layard, R.; Lyubomirsky, S.; et al. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect. Psychol. Sci. J. Assoc. Psychol. Sci. 2022, 17, 915–936. [Google Scholar] [CrossRef] [PubMed]
- Richter, T.; Nestler-Parr, S.; Babela, R.; Khan, Z.M.; Tesoro, T.; Molsen, E.; Hughes, D.A. Rare Disease Terminology and Definitions—A Systematic Global Review: Report of the ISPOR Rare Disease Special Interest Group. Value Health 2015, 18, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Nguengang Wakap, S.; Lambert, D.M.; Olry, A.; Rodwell, C.; Gueydan, C.; Lanneau, V.; Murphy, D.; Le Cam, Y.; Rath, A. Estimating Cumulative Point Prevalence of Rare Diseases: Analysis of the Orphanet Database. Eur. J. Hum. Genet. 2020, 28, 165–173. [Google Scholar] [CrossRef]
- Fatti e Cifre, Demografia dell’UE|Unione Europea. Available online: https://european-union.europa.eu/principles-countries-history/key-facts-and-figures/life-eu_it (accessed on 24 May 2023).
- Marano, G.; Gaetani, E.; Gasbarrini, A.; Janiri, L.; Sani, G.; Mazza, M.; Multidisciplinary Gemelli Group for HHT. Mental Health and Counseling Intervention for Hereditary Hemorrhagic Telangiectasia (HHT) during the COVID-19 Pandemic: Perspectives from Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 10225–10227. [Google Scholar] [CrossRef]
- Schwartz, I.V.D.; Randon, D.N.; Monsores, N.; Moura de Souza, C.F.; Horovitz, D.D.G.; Wilke, M.V.M.B.; Brunoni, D. SARS-CoV-2 Pandemic in the Brazilian Community of Rare Diseases: A Patient Reported Survey. Am. J. Med. Genet. C Semin. Med. Genet. 2021, 187, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Fiumara, A.; Lanzafame, G.; Arena, A.; Sapuppo, A.; Raudino, F.; Praticò, A.; Pavone, P.; Barone, R. COVID-19 Pandemic Outbreak and Its Psychological Impact on Patients with Rare Lysosomal Diseases. J. Clin. Med. 2020, 9, 2716. [Google Scholar] [CrossRef]
- Rihm, L.; Dreier, M.; Rezvani, F.; Wiegand-Grefe, S.; Dirmaier, J. The Psychosocial Situation of Families Caring for Children with Rare Diseases during the COVID-19 Pandemic: Results of a Cross-Sectional Online Survey. Orphanet J. Rare Dis. 2022, 17, 449. [Google Scholar] [CrossRef]
- Stewart, A.; Smith, C.H.; Eaton, S.; De Coppi, P.; Wray, J. COVID-19 Pandemic Experiences of Parents Caring for Children with Oesophageal Atresia/Tracheo-Oesophageal Fistula. BMJ Paediatr. Open 2021, 5, e001077. [Google Scholar] [CrossRef]
- Smyth, D.; Hytiris, M.; Kelday, C.; McDonnell, C.; Burren, C.; Gardner, A.; Mills, L.; Parekh, S.; Semler, O.; Stewart, A.; et al. Patient-Reported Experience of Clinical Care of Osteogenesis Imperfecta (OI) during the COVID-19 Pandemic. Front. Public Health 2023, 10, 951569. [Google Scholar] [CrossRef]
- Marano, G.; Gaetani, E.; Marturano, M.; Sani, G.; Gasbarrini, A.; Scambia, G.; Mazza, M. Web-Mediated Counseling to Counteract the Emotional Impact of COVID-19 for Women with Interstitial Cystitis/Bladder Pain Syndrome. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2109–2113. [Google Scholar] [CrossRef]
- Hartinger, A.V. The Rare Covid Experience: Systemic and Health Factors, Coping, and Support Among Adults with Rare Diseases During COVID-19. Honors Baccalurate of Sience in History, Oregon State University, Corvallis, OR, USA, 2022. [Google Scholar]
- Fjermestad, K.W.; Orm, S.; Silverman, W.K.; Cogo-Moreira, H. Short Report: COVID-19-Related Anxiety Is Associated with Mental Health Problems among Adults with Rare Disorders. Res. Dev. Disabil. 2022, 123, 104181. [Google Scholar] [CrossRef] [PubMed]
- McMullan, J.; Crowe, A.; Santin, O.; Quinn, S.; McShane, C.; Anderson, L.; McKnight, A.J. Investigating the Impact of COVID-19 on caregivers for Those with a Rare Disease. In Proceedings of the Joint Public Health Conference 2020, Online, 17 November 2020. [Google Scholar]
- Hwang, T.-J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and Social Isolation during the COVID-19 Pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Lakhan, R.; Agrawal, A.; Sharma, M. Prevalence of Depression, Anxiety, and Stress during COVID-19 Pandemic. J. Neurosci. Rural Pract. 2020, 11, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.C.Y.; Ng, Y.N.C.; Jain, R.; Chung, B.H.Y. A Thematic Study: Impact of COVID-19 Pandemic on Rare Disease Organisations and Patients across Ten Jurisdictions in the Asia Pacific Region. Orphanet J. Rare Dis. 2021, 16, 119. [Google Scholar] [CrossRef]
- Scherr, J.F.; Albright, C.; de los Reyes, E. Utilizing Telehealth to Create a Clinical Model of Care for Patients with Batten Disease and Other Rare Diseases. Ther. Adv. Rare Dis. 2021, 2, 26330040211038564. [Google Scholar] [CrossRef]
- Chowdhury, S.F.; Sium, S.M.A.; Anwar, S. Research and Management of Rare Diseases in the COVID-19 Pandemic Era: Challenges and Countermeasures. Front. Public Health 2021, 9, 640282. [Google Scholar] [CrossRef]
- Ward, A.J.; Murphy, D.; Marron, R.; McGrath, V.; Bolz-Johnson, M.; Cullen, W.; Daly, A.; Hardiman, O.; Lawlor, A.; Lynch, S.A.; et al. Designing Rare Disease Care Pathways in the Republic of Ireland: A Co-Operative Model. Orphanet J. Rare Dis. 2022, 17, 162. [Google Scholar] [CrossRef]
- Li, L.; Taeihagh, A.; Tan, S.Y. A Scoping Review of the Impacts of COVID-19 Physical Distancing Measures on Vulnerable Population Groups. Nat. Commun. 2023, 14, 599. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Chaplin, C. Unmasked: An Insight into Three Patients’ Rare Disease Experiences during the COVID-19 Pandemic. Orphanet J. Rare Dis. 2021, 16, 88. [Google Scholar] [CrossRef]
- Martin, J.; Robertson, K.; Richards, C.; Scerif, G.; Baker, K.; Tye, C. Experiences of Parents of Children with Rare Neurogenetic Conditions during the COVID-19 Pandemic: An Interpretative Phenomenological Analysis. BMC Psychol. 2022, 11, 179. [Google Scholar] [CrossRef] [PubMed]
- Boettcher, J.; Nazarian, R.; Fuerboeter, M.; Liedtke, A.; Wiegand-Grefe, S.; Reinshagen, K.; Boettcher, M. Mental Health of Siblings of Children with Rare Congenital Surgical Diseases during the COVID-19 Pandemic. Eur. J. Pediatr. Surg. 2021, 32, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.C.; Wong, W.H.; Fung, J.L.; Hong Kong, R.D.; Chung, B.H. Impact of COVID-19 Pandemic on Patients with Rare Disease in Hong Kong. Eur. J. Med. Genet. 2020, 63, 104062. [Google Scholar] [CrossRef]
- Ridner, S.H. Psychological Distress: Concept Analysis. J. Adv. Nurs. 2004, 45, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Thaller, M.; Tsermoulas, G.; Sun, R.; Mollan, S.; Sinclair, A. Negative Impact of COVID-19 Lockdown on Papilloedema and Idiopathic Intracranial Hypertension. J. Neurol. Neurosurg. Psychiatry 2022, 93, A121. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Norman, G.J.; Berntson, G.G. Social Isolation. Ann. N. Y. Acad. Sci. 2011, 1231, 17–22. [Google Scholar] [CrossRef]
- Nilsson, B.; Lindström, U.Å.; Nåden, D. Is Loneliness a Psychological Dysfunction? A Literary Study of the Phenomenon of Loneliness. Scand. J. Caring Sci. 2006, 20, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Killeen, C. Loneliness: An Epidemic in Modern Society. J. Adv. Nurs. 1998, 28, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Zavaleta, D.; Samuel, K.; Mills, C.T. Measures of Social Isolation. Soc. Indic. Res. 2017, 131, 367–391. [Google Scholar] [CrossRef]
- ICD-11 for Mortality and Morbidity Statistics. Available online: https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1563440232 (accessed on 9 September 2023).
- American Psychiatric Association. Depressive Disorders. In Diagnostic and Statistical Manual of Mental Disorders; DSM Library; American Psychiatric Association Publishing: Washington, DC, USA, 2022; ISBN 978-0-89042-575-6. [Google Scholar]
- Essue, B.M.; Iragorri, N.; Fitzgerald, N.; de Oliveira, C. The Psychosocial Cost Burden of Cancer: A Systematic Literature Review. Psychooncology 2020, 29, 1746–1760. [Google Scholar] [CrossRef]
- Graf, J.; Stengel, A. Psychological Burden and Psycho-Oncological Interventions for Patients with Hepatobiliary Cancers—A Systematic Review. Front. Psychol. 2021, 12, 662777. [Google Scholar] [CrossRef] [PubMed]
- Van Bunnik, B.A.D.; Morgan, A.L.K.; Bessell, P.R.; Calder-Gerver, G.; Zhang, F.; Haynes, S.; Ashworth, J.; Zhao, S.; Cave, R.N.R.; Perry, M.R.; et al. Segmentation and Shielding of the Most Vulnerable Members of the Population as Elements of an Exit Strategy from COVID-19 Lockdown. Philos. Trans. R. Soc. B Biol. Sci. 2021, 376, 20200275. [Google Scholar] [CrossRef] [PubMed]
- Ramaswami, U.; D’Amore, S.; Finnegan, N.; Hughes, D.; Kazemi, M.; Lysosomal Disorders Team, R.F.L.N.F.T. Impact of SARS-CoV-2 (COVID-19) Pandemic on Patients with Lysosomal Storage Disorders and Restoration of Services: Experience from a Specialist Centre. Intern. Med. J. 2021, 51, 1580–1593. [Google Scholar] [CrossRef] [PubMed]
- Rajmil, L.; Perestelo-Pérez, L.; Herdman, M. Quality of Life and Rare Diseases. In Rare Diseases Epidemiology; Advances in Experimental Medicine and Biology; Posada de la Paz, M., Groft, S.C., Eds.; Springer Netherlands: Dordrecht, The Netherlands, 2010; pp. 251–272. ISBN 978-90-481-9485-8. [Google Scholar]
- Nguyen, C.Q.; Kariyawasam, D.; Alba-Concepcion, K.; Grattan, S.; Hetherington, K.; Wakefield, C.E.; Woolfenden, S.; Dale, R.C.; Palmer, E.E.; Farrar, M.A. ‘Advocacy Groups Are the Connectors’: Experiences and Contributions of Rare Disease Patient Organization Leaders in Advanced Neurotherapeutics. Health Expect. 2022, 25, 3175–3191. [Google Scholar] [CrossRef]
- Dovigo, L.; Caprì, T.; Iannizzotto, G.; Nucita, A.; Semino, M.; Giannatiempo, S.; Zocca, L.; Fabio, R.A. Social and Cognitive Interactions Through an Interactive School Service for RTT Patients at the COVID-19 Time. Front. Psychol. 2021, 12, 676238. [Google Scholar] [CrossRef]
- BMJ Rare Diseases in the Time of COVID-19: Once Forgotten, Always Forgotten? Available online: https://blogs.bmj.com/bmj/2020/09/20/rare-diseases-in-the-time-of-covid-19-once-forgotten-always-forgotten/ (accessed on 30 May 2023).
- Roser, M.; Ritchie, H. Cancer. Our World Data 2015. [Google Scholar]
- Jones, K.; Mallon, S.; Schnitzler, K. A Scoping Review of the Psychological and Emotional Impact of the COVID-19 Pandemic on Children and Young People. Illn. Crisis Loss 2023, 31, 175–199. [Google Scholar] [CrossRef]
- Mahmud, S.; Mohsin, M.; Dewan, M.N.; Muyeed, A. The Global Prevalence of Depression, Anxiety, Stress, and Insomnia Among General Population During COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Trends Psychol. 2023, 31, 143–170. [Google Scholar] [CrossRef]
- Khan, M.; Khan, N.; Begum, S.; Qureshi, M.I. Digital Future beyond Pandemic Outbreak: Systematic Review of the Impact of COVID-19 Outbreak on Digital Psychology. Foresight 2023, ahead-of-print. [Google Scholar] [CrossRef]
- Coca, J.R.; Esteban-Bueno, G.; Manuel-Guerra, J. Investigación cualitativa sobre el impacto del confinamiento estricto en las entidades del tercer sector españolas relacionadas con las enfermedades raras. Saúde Soc. 2022, 31, e210378es. [Google Scholar] [CrossRef]
- Vara Graña, C.G. Impacto de la Pandemia por COVID-19 en las Personas que Padecen Enfermedades Raras del Perú Durante el Año 2021. Bachelor Degree, Universidad Privada San Juan Baut, Lima, Perú, 2022. [Google Scholar]
- Meyer, D.; Slone, S.E.; Ogungbe, O.; Duroseau, B.; Farley, J.E. Impact of the COVID-19 Pandemic on HIV Healthcare Service Engagement, Treatment Adherence, and Viral Suppression in the United States: A Systematic Literature Review. AIDS Behav. 2023, 27, 344–357. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, E.; Dey, D.; Grainger, R.; Li, M.; Machado, P.M.; Ugarte-Gil, M.F.; Yazdany, J. Global Perspective on the Impact of the COVID-19 Pandemic on Rheumatology and Health Equity. Arthritis Care Res. 2023, online version of record before inclusion in an issue. [Google Scholar] [CrossRef]
- Angelini, M.; Teglia, F.; Casolari, G.; Astolfi, L.; Boffetta, P. Decrease of Visits and Hospital Admissions for Cancer Patients during the COVID-19 Pandemic. A Systematic Review and Meta-Analysis. J. Public Health 2023. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, Country | Research Focus, Number of Participants, Control Group (Y/N) Findings | Document Nature, Researcher Background |
|---|---|---|
| Marano, G.; Gaetani, E.; et.al, 2020 [5]; Italy | Interventions for hereditary haemorrhagic telangiectasia patients during COVID-19 Telehealth and multidisciplinary approach needed for effective interventions | Paper, review, psychology, medicine |
| Schwartz, I.V.D.; Randon, D.N.; et.al, 2021 [6], Brazil | COVID-19 impact on RD patients, n = 1466, Y Isolation helped contain mortality; telemedicine was an essential tool to face healthcare system flaws | Paper, research, medicine |
| Fiumara, A.; Lanzafame, G.; et.al, 2020 [7], Italy | COVID-19 impact on lysosomal storage disorder patients, n = 15, Y LSD patients’ needs to adhere to therapy schedule; the pandemic strengthened familiar relationships and worsened social ones | Paper, research, medicine |
| Rihm, L.; Dreier, M.; et.al, 2022 [8], Germany | COVID-19 impact on families of RD children, n = 149, N Caregivers of RD children endured great distress during the pandemic; family-centred psychological support is needed to help caregivers coping with emergency situations | Paper, research, psychology |
| Stewart, A.; Smith, C.H.; et.al, 2021 [9], England | COVID-19 impact on parents of oesophageal atresia/tracheo-oesophageal fistula patients, n = 65 + 6, N Telehealth, as necessary as it is, needs improvement to address specific needs; caregivers’ experiences were varied and, as such, so should be the institutions’ responses | Paper, research, medicine, language therapy |
| Smyth, D.; Hytiris, M.; et.al, 2023 [10], England | COVID-19 impact on osteogenesis imperfecta patients, n1 = 110, n2 = 124, N Remote consultation played an important role in managing the emergency and should be implemented in the healthcare system; there were differences in results between T1 and T2 of the research, highlighting differences in patients’ perceptions and needs during the pandemic | Paper, research, medicine |
| Marano, G.; Gaetani, E.; et.al, 2021 [11], Italy | Interventions for interstitial cystitis/bladder pain syndrome patients during COVID-19 Web-mediated counselling could help patients and their caregivers to alleviate distress with a tailor-made approach; a multidisciplinary approach is advised | Paper, review, psychology, medicine |
| Hartinger, A.V., 2022 [12], USA | COVID-19 impact on RD patients, n = 759, N COVID-19 pandemic had a great impact on RD patients, who were demonstrated to be resilient, and it strengthened familiar relationships; hope for needed changes grew thanks to the pandemic highlighting healthcare system flaws | Thesis dissertation, research, psychology |
| Fjermestad, K.W.; Orm, S.; et.al, 2022 [13], Norway | COVID-19 impact on RD patients, n = 58, Y RD patients showed worse indexes in SLC-5 and CAS scale compared with non-RD people; anxiety management is advised for professionals working with RD patients | Paper, short report, psychology |
| McMullan, J.; Crowe, A.; et.al, 2020 [14], England | COVID-19 impact on caregivers, n = 165, N Caregivers experienced high psychological burden during the COVID-19 pandemic; a tailored approach is advised to better help alleviate the burden on this population | Conference, research, psychology |
| Chung, C.C.Y.; Ng, Y.N.C.; et.al, 2021 [17], Asia–Pacific region | COVID-19 impact on RD-related organisations RD-related organisations experienced decrease in manpower and funding; digitalization was needed to cope with the situation and manage to help those in need | Paper, research, medicine |
| Scherr, J.F.; Albright, C.; et.al, 2021 [18], U.S.A. | Interventions for Batten disease during COVID-19 Telehealth is an important tool to address special needs of RD patients; a tailor-made approach should be implemented for better results | Paper, review, medicine |
| Chowdhury, S.F.; Sium, S.M.A.; et.al, 2021 [19], Global | Interventions for patients and research during COVID-19 RD people endured a worsening of an already difficult situation; institutions should focus on RD people’s special needs and provide adequate care and access to therapy | Paper, review, medicine |
| Chaplin, C., 2021 [23], England | COVID-19 impact on mastocytosis patients, n = 3, N Telemedicine was one of the only aids for patients enduring new challenges and isolation during the pandemic; resilience emerged as an important aspect to adjust to a new normality; a lack in non-RD people’s understanding of the challenges is highlighted | Paper, research, medicine |
| Martin, J.; Robertson, K.; et.al, 2022 [24], England | COVID-19 impact on parents of rare neurogenetic conditions children, n = 11, N COVID-19 pandemic highlighted some flaws in the healthcare system, giving insight into how to improve the services; a multidisciplinary approach is suggested to offer appropriate support; children with neurogenetic disorders were negatively impacted by the pandemic | Paper (peer review pending), research, psychology |
| Boettcher, J.; Nazarian, R.; et.al, 2021 [25], Germany | COVID-19 impact on siblings of children with rare congenital surgical diseases, n = 81, Y Not only patients but also siblings of RD children have been largely impacted by the COVID-19 pandemic; healthy siblings could have experienced a lack of attention to their needs; greater attention from professionals and families alike is advised | Paper, research, medicine |
| Chung, C.CY.; Wong, W.HS.; et.al, 2020 [26], China | COVID-19 impact on RD patients RD patients suffered from both higher risk of COVID-19 infection and difficulties in accessing healthcare services, increasing psychological burden | Paper, research, medicine |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faccio, E.; Bottecchia, M.; Rocelli, M. Caring for People with Rare Diseases: A Systematic Review of the Challenges of, and Strategies for Dealing with, COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 6863. https://doi.org/10.3390/ijerph20196863
Faccio E, Bottecchia M, Rocelli M. Caring for People with Rare Diseases: A Systematic Review of the Challenges of, and Strategies for Dealing with, COVID-19. International Journal of Environmental Research and Public Health. 2023; 20(19):6863. https://doi.org/10.3390/ijerph20196863
Chicago/Turabian StyleFaccio, Elena, Matteo Bottecchia, and Michele Rocelli. 2023. "Caring for People with Rare Diseases: A Systematic Review of the Challenges of, and Strategies for Dealing with, COVID-19" International Journal of Environmental Research and Public Health 20, no. 19: 6863. https://doi.org/10.3390/ijerph20196863
APA StyleFaccio, E., Bottecchia, M., & Rocelli, M. (2023). Caring for People with Rare Diseases: A Systematic Review of the Challenges of, and Strategies for Dealing with, COVID-19. International Journal of Environmental Research and Public Health, 20(19), 6863. https://doi.org/10.3390/ijerph20196863








