A Single Center Observational Study on Clinical Manifestations and Associated Factors of Pediatric Long COVID
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Weekly Epidemiological Update on COVID-19, 50th ed.; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Ortiz-Prado, E.; Simbaña-Rivera, K.; Gómez-Barreno, L.; Rubio-Neira, M.; Guaman, L.P.; Kyriakidis, N.C.; Muslin, C.; Jaramillo, A.M.G.; Barba-Ostria, C.; Cevallos-Robalino, D.; et al. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn. Microbiol. Infect. Dis. 2020, 98, 115094. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_3-maggio-2023.pdf (accessed on 6 May 2023).
- Howard-Jones, A.R.; Burgner, D.P.; Crawford, N.W.; Goeman, E.; E Gray, P.; Hsu, P.; Kuek, S.; McMullan, B.J.; Tosif, S.; Wurzel, D.; et al. COVID-19 in children. II: Pathogenesis, disease spectrum and management. J. Paediatr. Child Health 2022, 58, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Li, X.; Xiao, Y.; Yang, R.; Wang, Y.; Wei, X. Distinct Characteristics of COVID-19 Infection in Children. Front. Pediatr. 2021, 9, 619738. [Google Scholar] [CrossRef] [PubMed]
- Liguoro, I.; Pilotto, C.; Bonanni, M.; Ferrari, M.E.; Pusiol, A.; Nocerino, A.; Vidal, E.; Cogo, P. SARS-CoV-2 infection in children and newborns: A systematic review. Eur. J. Pediatr. 2021, 179, 1029–1046. [Google Scholar] [CrossRef]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M.; Bonanomi, E.; D’Antiga, L. An outbreak of severe Kawasaki- like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An obser-vational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Levin, M. Childhood multisystem inflammatory syndrome—A new chal- lenge in the pandemic. N. Engl. J. Med. 2020, 383, 393–395. [Google Scholar] [CrossRef]
- Available online: https://apps.who.int/iris/bitstream/handle/10665/345824/WHO-2019-nCoV-Post-COVID-19-condition-Clinical-case-definition-2021.1-eng.pdf (accessed on 20 March 2023).
- Buonsenso, D.; Munblit, D.; De Rose, C.; Sinatti, D.; Ricchiuto, A.; Carfi, A.; Valentini, P. Preliminary evidence on long COVID in children. Acta Paediatr. 2021, 110, 2208–2211. [Google Scholar] [CrossRef]
- Buonsenso, D.; Espuny Pujol, F.; Munblit, D.; Mcfarland, S.; Simpson, F. Clinical Characteristics, Activity Levels and Mental Health Problems in Children with Long COVID: A Survey of 510 Children. Future Microbiol. 2021, 17, 577–588. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021, 110, 914–921. [Google Scholar] [CrossRef]
- Selvakumar, J.; Havdal, L.B.; Drevvatne, M.; Brodwall, E.M.; Berven, L.L.; Stiansen-Sonerud, T.; Einvik, G.; Leegaard, T.M.; Tjade, T.; Michelsen, A.E.; et al. Prevalence and Characteristics Associated With Post-COVID-19 Condition Among Nonhospitalized Adolescents and Young Adults. JAMA Netw. Open 2023, 6, e235763. [Google Scholar] [CrossRef]
- Barlow, S.E.; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120 (Suppl. S4), S164–S192. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.K.; Guevara-Coto, J.; Yogendra, R.; Francisco, E.B.; Long, E.; Pise, A.; Rodrigues, H.; Parikh, P.; Mora, J.; Mora-Rodríguez, R.A. Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. Front. Immunol. 2021, 12, 700782. [Google Scholar] [CrossRef] [PubMed]
- King, J.A.; Whitten, T.A.; Bakal, J.A.; McAlister, F.A. Symptoms associated with a positive result for a swab for SARS-CoV-2 infection among children in Alberta. CMAJ 2021, 193, E1–E9. [Google Scholar] [CrossRef] [PubMed]
- Hoste, L.; Van Paemel, R.; Haerynck, F. Multisystem inflammatory syndrome in children related to COVID-19: A systematic review. Eur. J. Pediatr. 2021, 180, 2019–2034. [Google Scholar] [CrossRef]
- Götzinger, F.; Santiago-García, B.; Noguera-Julián, A.; Lanaspa, M.; Lancella, L.; Carducci, F.I.C.; Gabrovska, N.; Velizarova, S.; Prunk, P.; Osterman, V.; et al. COVID-19 in children and adolescents in Europe: A multinational, multicentre cohort study. Lancet Child Adolesc. Health 2020, 4, 653–661. [Google Scholar] [CrossRef]
- Cristiani, L.; Mancino, E.; Matera, L.; Nenna, R.; Pierangeli, A.; Scagnolari, C.; Midulla, F. Will children reveal their secret? The coronavirus dilemma. Eur. Respir. J. 2020, 55, 2000749. [Google Scholar] [CrossRef]
- Vezir, E.; Hizal, M.; Yayla, B.C.; Aykac, K.; Yilmaz, A.; Kaya, G.; Oygar, P.D.; Ozsurekci, Y.; Ceyhan, M. Does aeroallergen sensitivity and allergic rhinitis in children cause milder COVID-19 infection? Allergy Asthma Proc. 2021, 42, 522–529. [Google Scholar] [CrossRef]
- Brough, H.A.; Kalayci, O.; Sediva, A.; Untersmayr, E.; Munblit, D.; Rodriguez del Rio, P.; Vazquez-Ortiz, M.; Arasi, S.; Alvaro-Lozano, M.; Tsabouri, S.; et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics—The 2020 COVID-19 pandemic. Pediatr. Allergy Immunol. 2020, 31, 442–448. [Google Scholar] [CrossRef]
- Longo, D.L.; Fauci, A.S.; Kasper, D.L.; Hausen, S.L.; Jameson, J.; Loscalzo, J. (Eds.) . Harrison’s Principles of Internal Medicine, 18th ed.; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- Ahmed, H.; Patel, K.; Greenwood, D.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00063. [Google Scholar] [CrossRef]
- Lam, M.H.B.; Wing, Y.K.; Yu, M.W.M.; Leung, C.M.; Ma, R.C.; Kong, A.P.; So, W.Y.; Fong, S.Y.Y.; Lam, S.P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
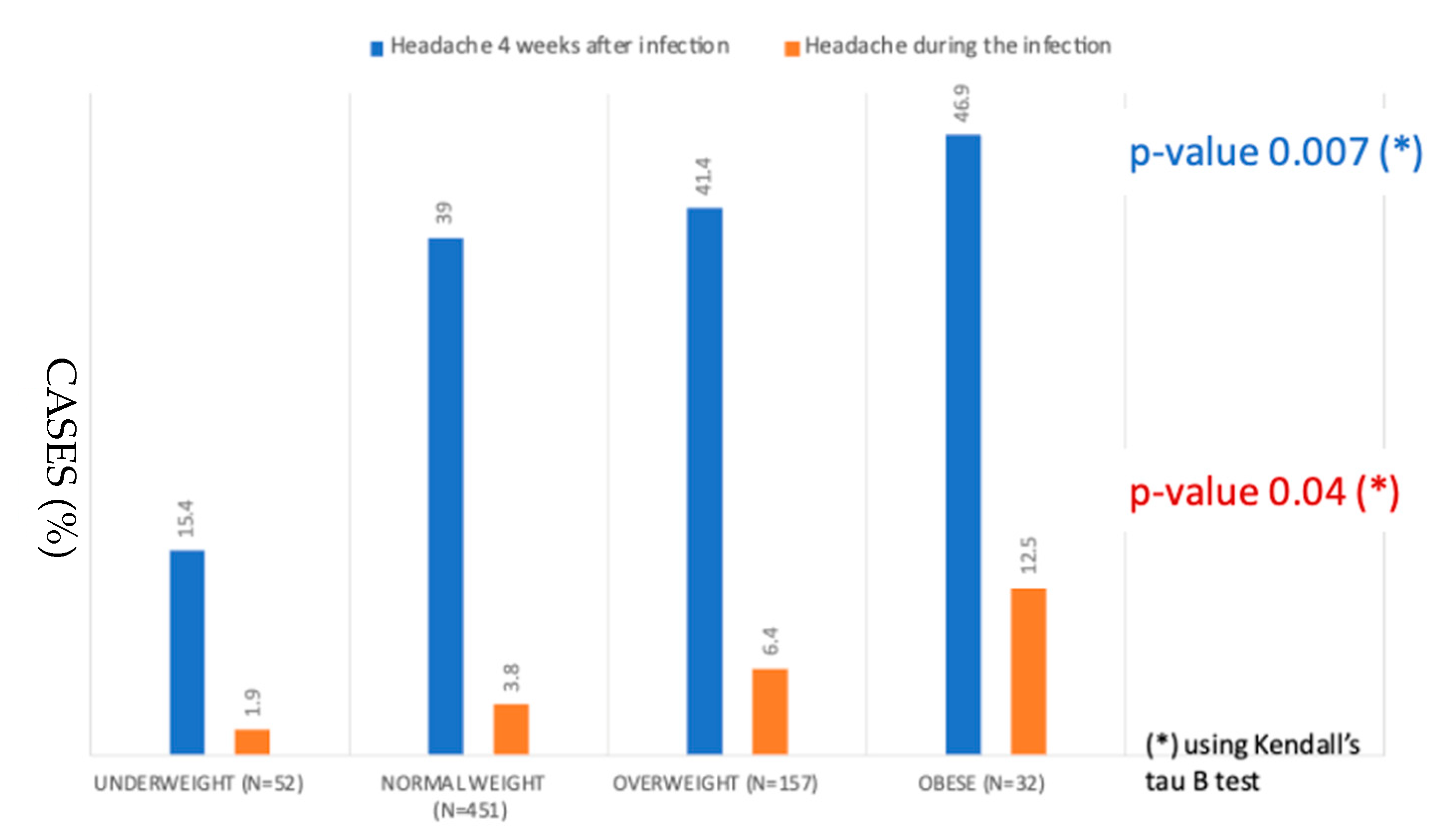
- Oakley, C.B.; Scher, A.I.; Recober, A.; Peterlin, B.L. Headache and obesity in the pediatric population. Curr. Pain Headache Rep. 2014, 18, 416. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, L.D.; Zuelch, M.L.; Dimitratos, S.M.; Scherr, R.E. Adolescent Obesity: Diet Quality, Psychosocial Health, and Cardiometabolic Risk Factors. Nutrients 2019, 12, 43. [Google Scholar] [CrossRef] [PubMed]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631, Erratum in Nat. Med. 2021, 27, 1116. [Google Scholar] [CrossRef] [PubMed]
- Brusaferri, L.; Alshelh, Z.; Martins, D.; Kim, M.; Weerasekera, A.; Housman, H.; Morrissey, E.J.; Knight, P.C.; Castro-Blanco, K.A.; Albrecht, D.S.; et al. The pandemic brain: Neuroinflammation in non-infected individuals during the COVID-19 pandemic. Brain Behav. Immun. 2022, 102, 89–97. [Google Scholar] [CrossRef]
- Borch, L.; Holm, M.; Knudsen, M.; Ellermann-Eriksen, S.; Hagstroem, S. Long COVID symptoms and duration in SARS-CoV-2 positive children—A nationwide cohort study. Eur. J. Pediatr. 2022, 181, 1597–1607. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
| 354 Males | 342 Females | 697 Children | p- Value | |
|---|---|---|---|---|
| Age, years (median, range) | 9.6 (0.1–18.6) | |||
| 65 (18) | 45 (13) | 110 (16) | |
| 152 (43) | 156 (46) | 306 (44) | 0.314 |
| 117 (33) | 121 (35) | 236 (34) | |
| 20 (5.8) | 20 (5.6) | 40 (5.7) | |
| Preterm (<37 weeks) (no, %) | 41 (55) | 33 (45) | 74 (11) | 0.395 |
| Gestational age, weeks (median, range) | 39 (29–42) | 39 (25–42) | 39 (25–42) | 0.539 |
| Breastfeeding (no, %) | 280 (51) | 271 (49) | 551 (79) | 0.779 |
| Smoking exposure (no, %) * | 119 (51) | 113 (49) | 232 (33) | 0.373 |
| Previous bronchiolitis | 73 (57) | 54 (43) | 127 (18) | 0.103 |
| Previous wheezing | 91 (56) | 71 (44) | 162 (23) | 0.133 |
| Atopy $ | 95 (55) | 79 (45) | 174 (25.0) | 0.284 |
| Body Mass Index (centile) | ||||
| 31 (60) 227 (50) 72 (46) 21 (66) | 21 (40%) 224 (50) 85 (54) 11 (34) | 52 (7.5) 451 (65) 157 (22) 32 (4.6) | 0.112 |
| Persistently positive COVID-19 patients (positive swab test > 21 days) | 151 (52) | 139 (48) | 290 (42) | 0.618 |
| Days elapsed between first positive SARS-CoV-2 test and outpatient consultation (median, range) | 174 (36–424) | 174 (25–669) | 174 (25–669) | 0.691 |
| Symptomatic Children during SARS-CoV-2 n = 697 | Symptomatic Children 30 Days after Infection n = 697 | Symptomatic Children 90 Days after Infection n = 697 | |
|---|---|---|---|
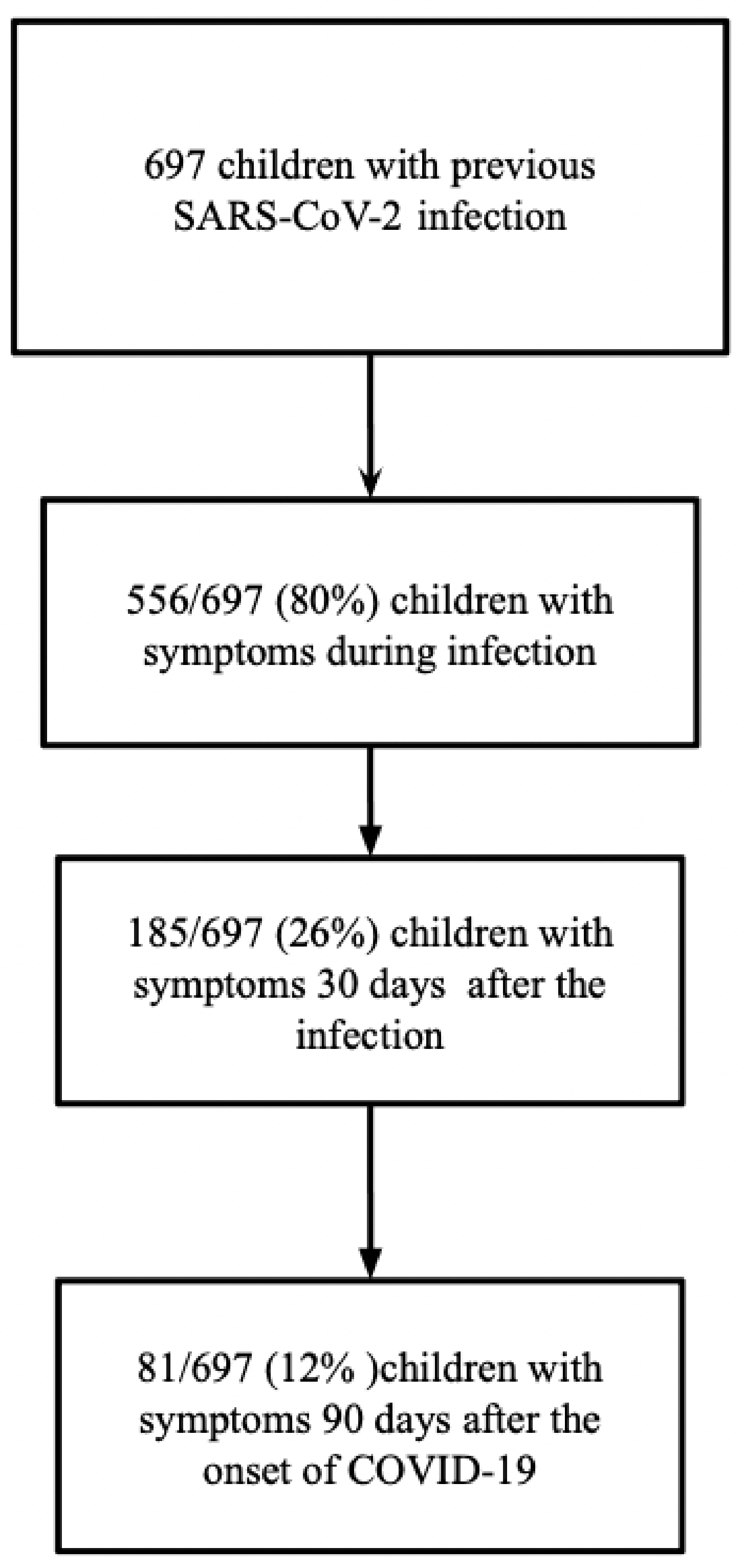
| Symptomatic patients | 556 (80%) | 185 (26%) | 81/697 (11.6%) |
| Fever # | 346 (50%) | 0 (0.0%) | 0 (0.0%) |
Respiratory Symptoms
| 281 (40%) 154 (22%) 120 (17%) 96 (14%) 47 (6.7%) 20 (2.9%) 0 (0.0%) 9 (1.3%) | 30 (4.3%) 10 (1.4%) 6 (0.9%) 1 (0.1%) 5 (0.7%) 0 (0.0%) 15 (2.2%) 15 (2.2%) | 13 (1.9%) 3 (0.4%) 5 (0.7%) 0 (0.0%) 11 (1.6%) 0 (0.0%) 0 (0.0%) 0 (0.0%) |
Gastrointestinal Symptoms
| 143 (20.5%) 102 (15%) 47 (6.7%) 17 (2.4%) 11 (1.6%) 10 (1.7%) 1 (0.1%) 0 (0%) | 16 (2.3%) 3 (0.4%) 0 (0.0%) 4 (0.6%) 0 (0.0%) 3 (0.4%) 7 (1.0%) 2 (0.3%) | 5 (0.7%) 0 (0.0%) 0 (0.0%) 3 (0.4%) 0 (0.0%) 2 (0.3%) 2 (0.3%) 2 (0.3%) |
Neurological Symptoms
| 339 (48.6%) 264 (38%) 142 (20%) 141 (20%) 1 (0.1%) 1 (0.1%) 1 (0.1%) 1 (0.1%) 0 (0%) 0 (0%) 0 (0%) 4 (0.6%) 17 (2.4%) | 94 (13.5%) 32 (4.6%) 34 (4.9%) 17 (2.4%) 11 (1.6%) 1 (0.1%) 8 (1.1%) 1 (0.1%) 12 (1.7%) 7 (1.0%) 1 (0.1%) 1 (0.1%) 0 (0.0%) | 47 (6.7%) 19 (2.7%) 16 (2.3%) 13 (1.9%) 1 (0.1%) 0 (0.0%) 14 (2.0%) 3 (0.4%) 9 (1.3%) 5 (0.7%) 0 (0%) 0 (0%) 9 (1.3%) |
Musculoskeletal symptoms
| 89 (13%) 67 (9.6%) | 17 (2.4%) 10 (1.4%) | 7 (1%) 7 (1%) |
| Asthenia | 180 (26%) | 86 (12.3%) | 39 (5.6%) |
| Skin rash | 28 (4.0%) | 4 (0.6%) | 3 (0.4%) |
| Chest pain | 6 (0.9%) | 3 (0.4%) | 3 (0.4%) |
| Palpitations | 1 (0.1%) | 2 (0.3%) | 1 (0.1%) |
| Other 3 | 17 (2.7%) | 3 (0.4%) | 0 (0.0%) |
| ≥5 symptoms during SARS-CoV-2 infection | 131 (19%) | -- | -- |
| MISC 4 | --- | 2 (0.3%) | --- |
| (a) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptomatic Children 30 Days after Infection n = 185 | Asymptomatic Children 30 Days after Infection n = 512 | p-Value | ||||||||
| Sex (male) | 88 (48%) | 267 (52%) | 0.33 | |||||||
| Preterm | 21 (11%) | 53 (10%) | 0.68 | |||||||
| Breastfeeding | 149 (82%) | 402 (79%) | 0.40 | |||||||
| Smoking exposure * | 66 (46%) | 166 (41%) | 0.28 | |||||||
| Persistently positive COVID-19 patients (positive swab test > 21 days) | 84 (47%) | 206 (41%) | 0.18 | |||||||
| Previous bronchiolitis | 31 (17%) | 96 (19%) | 0.56 | |||||||
| Previous wheezing | 50 (27%) | 112 (22%) | 0.15 | |||||||
| Atopy | 60 (31%) | 114 (22%) | 0.006 | |||||||
| Underweight | 7 (3.8%) | 45 (8.9%) | 0.03 | |||||||
| Overweight and obese | 57(30%) | 132 (26%) | 0.19 | |||||||
| Overweight and obese (female) | 34 (18%) | 62 (12%) | 0.03 | |||||||
| Overweight and obese (male) | 23 (12%) | 70 (14%) | 0.66 | |||||||
| Obesity | 21 (11%) | 35 (6.8%) | 0.07 | |||||||
| Symptoms during SARS-CoV-2 infection (No,%) | 172 (93%) | 384 (76%) | <0.001 | |||||||
| Fever during SARS-CoV-2 infection (No,%) | 106(58%) | 240 (47%) | 0.01 | |||||||
| ≥5 symptoms during SARS-CoV-2 infection | 69 (38%) | 64 (12%) | <0.001 | |||||||
| Asthenia (No,%) | 76 (41%) | 104 (20%) | <0.001 | |||||||
| (b) | ||||||||||
| Step 5a | B | S.E. | Wald | df | Score | OR | 95% C.I. for OR | p | ||
| Lower | Upper | |||||||||
| Anosmia | 0.864 | 0.210 | 16.952 | 1 | 2.373 | 1.573 | 3.581 | 0.001 | ||
| Atopy | 0.495 | 0.205 | 5.827 | 1 | 1.640 | 1.097 | 2.450 | 0.016 | ||
| Asthenia | 0.725 | 0.199 | 13.282 | 1 | 2.065 | 1.398 | 3.049 | 0.001 | ||
| Cough | 0.853 | 0.209 | 16.667 | 1 | 2.346 | 1.558 | 3.532 | 0.001 | ||
| Sex | 1 | 1.429 | 0.232 | |||||||
| Preterm | 1 | 0.518 | 0.472 | |||||||
| Previous bronchiolitis | 1 | 0.248 | 0.618 | |||||||
| Previous wheezing | 1 | 0.102 | 0.750 | |||||||
| Obese | 1 | 0.919 | 0.338 | |||||||
| Positive swab test >21 days | 1 | 1.280 | 0.258 | |||||||
| Fever | 1 | 0.383 | 0.536 | |||||||
| Symptomatic Children 90 Days after Infection n = 81 | Asymptomatic Children 90 Days after Infection n = 104 | p-Value | |
|---|---|---|---|
| Sex (male) | 40 (49%) | 22 (21%) | 0.75 |
| Preterm | 7 (8.6%) | 9 (8.6%) | 0.04 |
| Breastfeeding | 67 (83%) | 30 (29%) | 0.11 |
| Smoking exposure * | 24 (30%) | 22 (21%) | 0.02 |
| Persistently positive COVID-19 patients (positive swab test > 21 days) | 34 (42%) | 21 (20%) | 0.43 |
| Previous bronchiolitis | 12 (15%) | 7 (6.7%) | 0.78 |
| Previous wheezing | 22 (27%) | 10 (9.6%) | 0.68 |
| Atopy | 29 (36%) | 16 (15%) | 0.80 |
| Underweight | 1 (1.2%) | 4 (3.8%) | 0.03 |
| Overweight and obese | 29 (36%) | 12 (11%) | 0.42 |
| Overweight and obesity (males) | 13 (16.0%) | 7 (6.7%) | 0.93 |
| Overweight and obesity (female) | 16 (20%) | 5 (4.8%) | 0.27 |
| Symptoms during SARS-CoV-2 infection (N0,%) | 77 (95%) | 38 (36%) | 0.33 |
| Fever during SARS-CoV-2 infection (No,%) | 49 (60%) | 24 (23%) | 0.72 |
| ≥5 symptoms during SARS-CoV-2 infection | 34 (42%) | 15 (14%) | 0.50 |
| Asthenia (No,%) | 45 (56%) | 14 (13%) | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancino, E.; Nenna, R.; Matera, L.; La Regina, D.P.; Petrarca, L.; Iovine, E.; Di Mattia, G.; Frassanito, A.; Conti, M.G.; Bonci, E.; et al. A Single Center Observational Study on Clinical Manifestations and Associated Factors of Pediatric Long COVID. Int. J. Environ. Res. Public Health 2023, 20, 6799. https://doi.org/10.3390/ijerph20186799
Mancino E, Nenna R, Matera L, La Regina DP, Petrarca L, Iovine E, Di Mattia G, Frassanito A, Conti MG, Bonci E, et al. A Single Center Observational Study on Clinical Manifestations and Associated Factors of Pediatric Long COVID. International Journal of Environmental Research and Public Health. 2023; 20(18):6799. https://doi.org/10.3390/ijerph20186799
Chicago/Turabian StyleMancino, Enrica, Raffaella Nenna, Luigi Matera, Domenico Paolo La Regina, Laura Petrarca, Elio Iovine, Greta Di Mattia, Antonella Frassanito, Maria Giulia Conti, Enea Bonci, and et al. 2023. "A Single Center Observational Study on Clinical Manifestations and Associated Factors of Pediatric Long COVID" International Journal of Environmental Research and Public Health 20, no. 18: 6799. https://doi.org/10.3390/ijerph20186799
APA StyleMancino, E., Nenna, R., Matera, L., La Regina, D. P., Petrarca, L., Iovine, E., Di Mattia, G., Frassanito, A., Conti, M. G., Bonci, E., Spatuzzo, M., Ialongo, S., Zicari, A. M., Spalice, A., Midulla, F., & on behalf of the Long COVID Research Group. (2023). A Single Center Observational Study on Clinical Manifestations and Associated Factors of Pediatric Long COVID. International Journal of Environmental Research and Public Health, 20(18), 6799. https://doi.org/10.3390/ijerph20186799






