Polyvictimization and Adolescent Health and Well-Being in Ethiopia: The Mediating Role of Resilience
Abstract
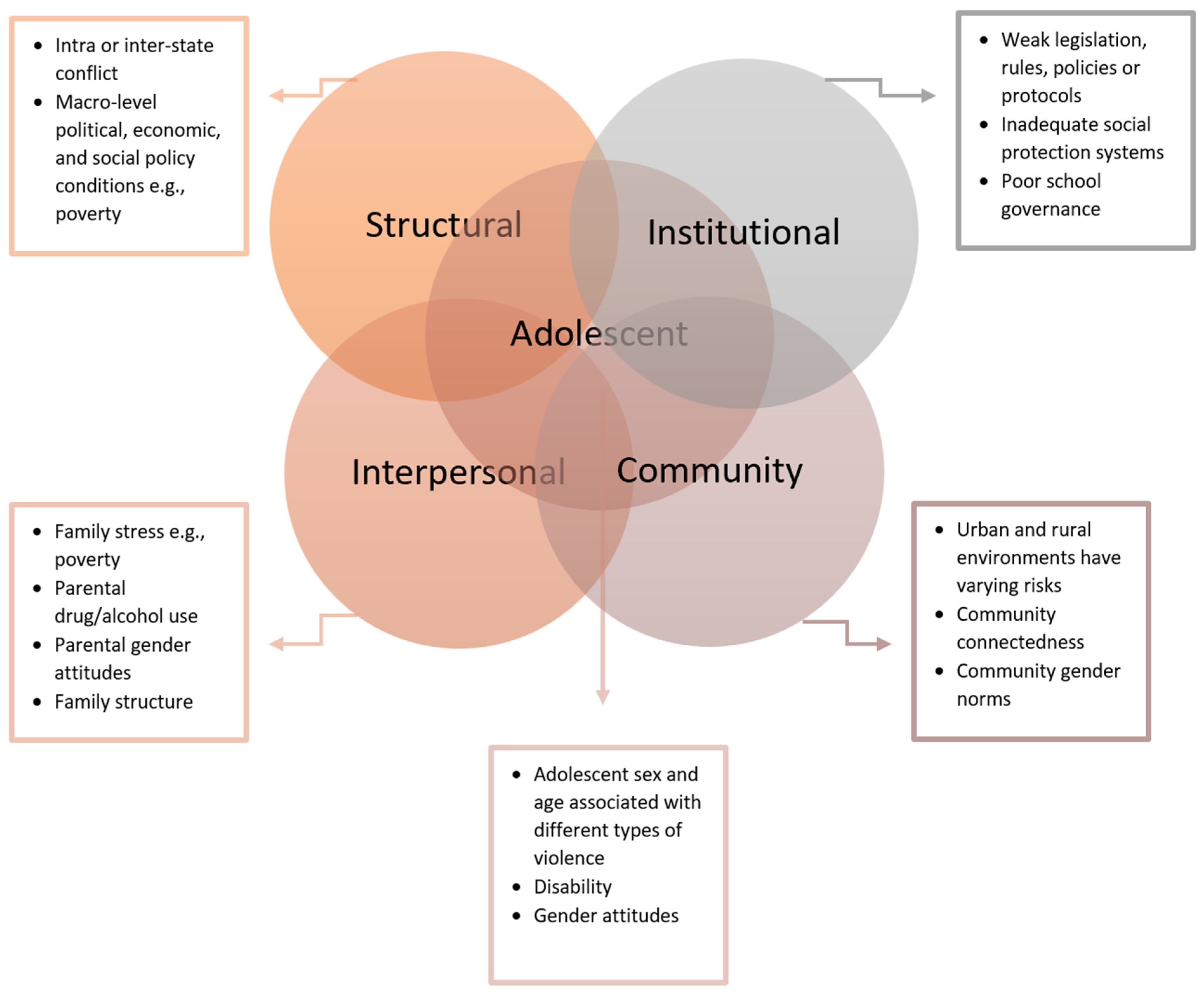
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Measures
2.4. Data Analyses
3. Results
3.1. Descriptive Statistics
3.2. Regression Analyses
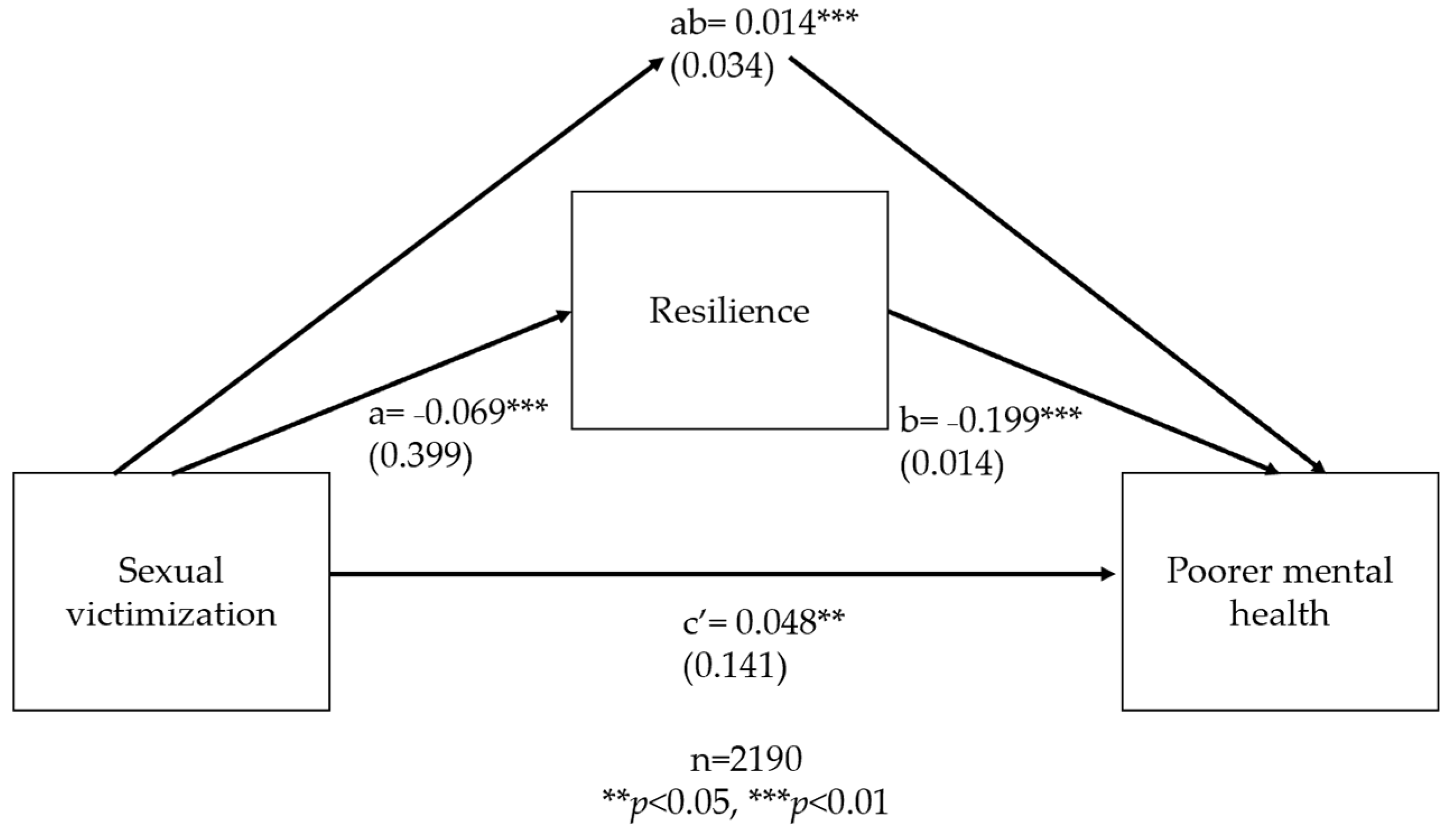
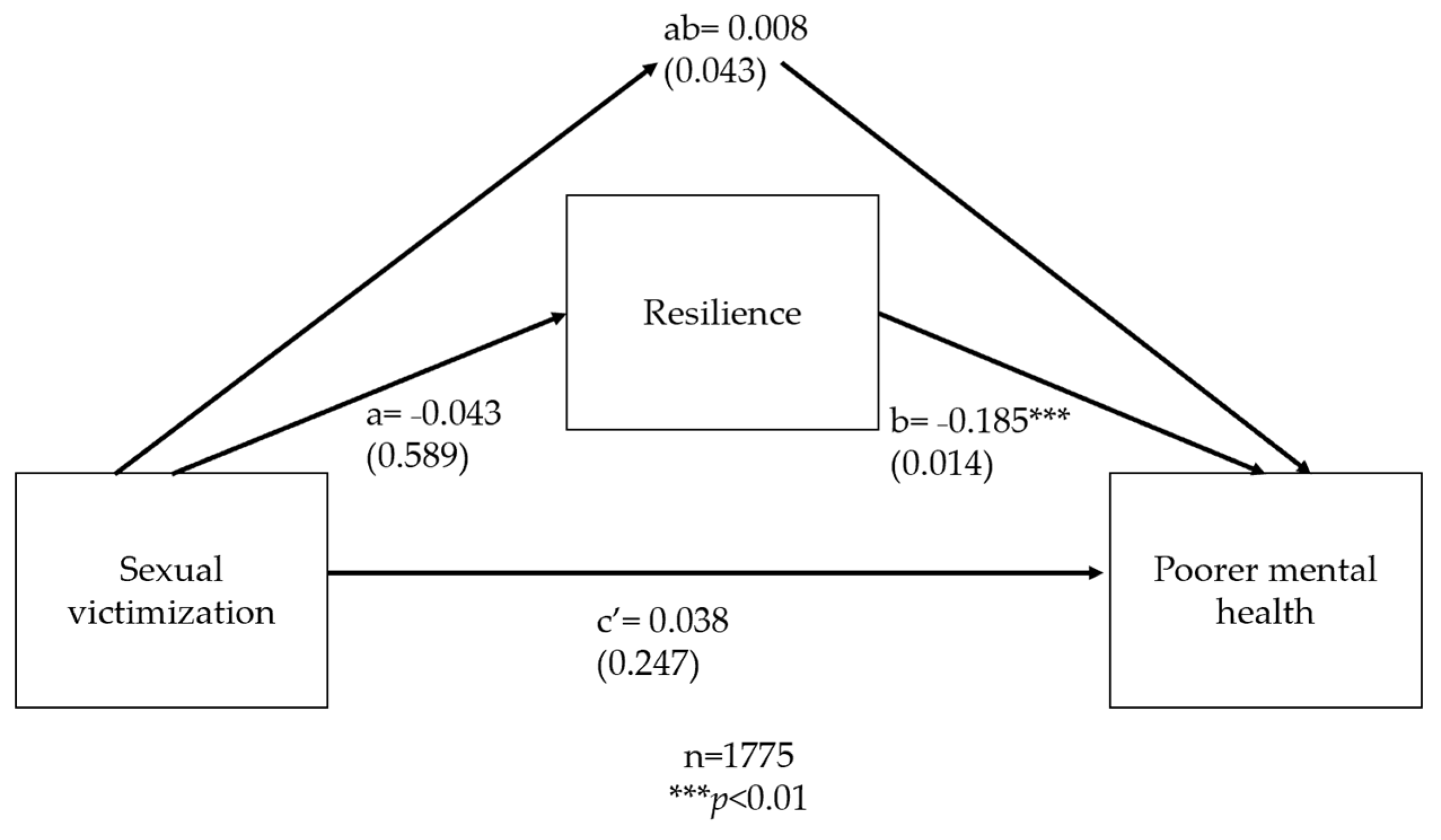
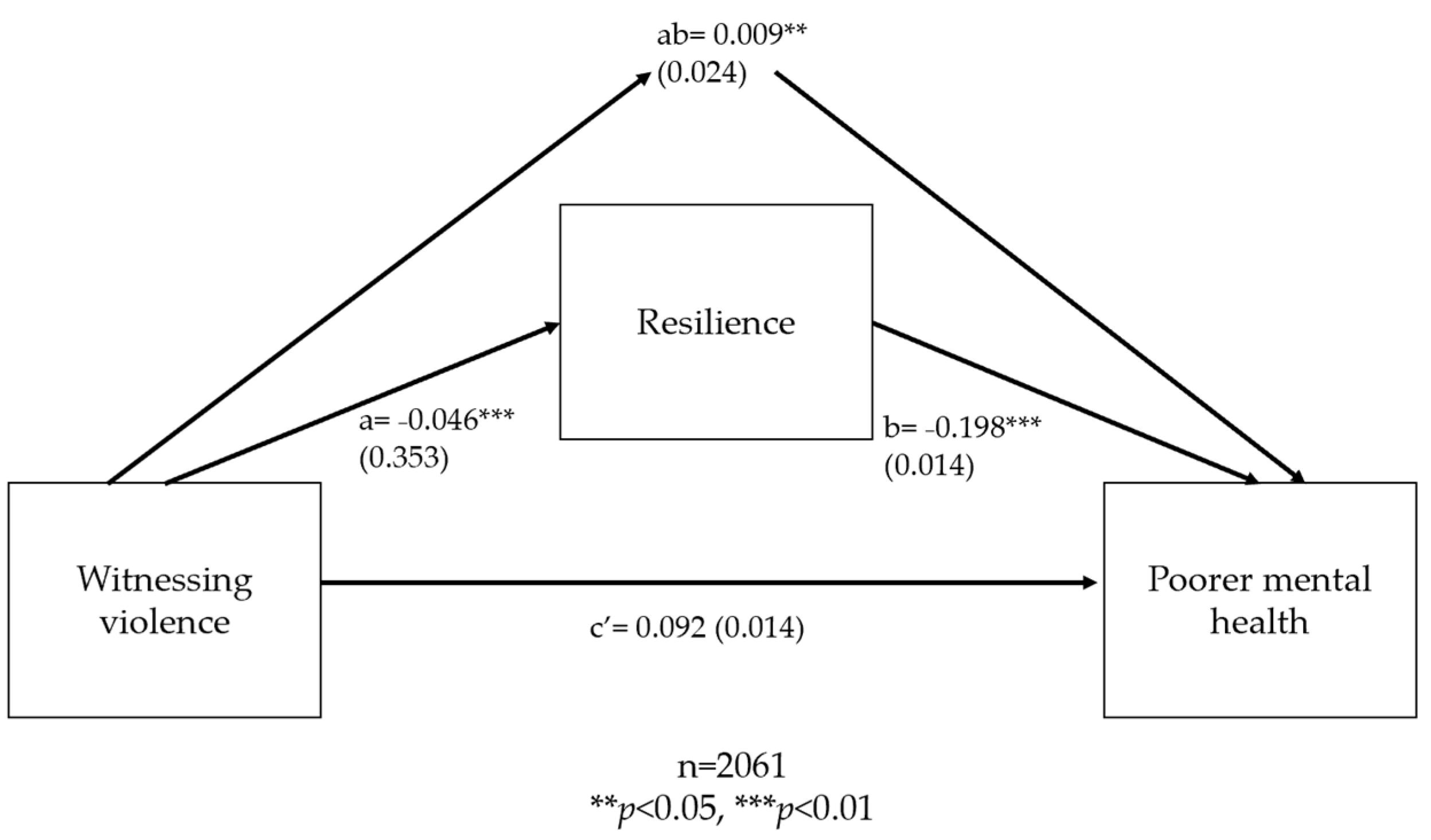
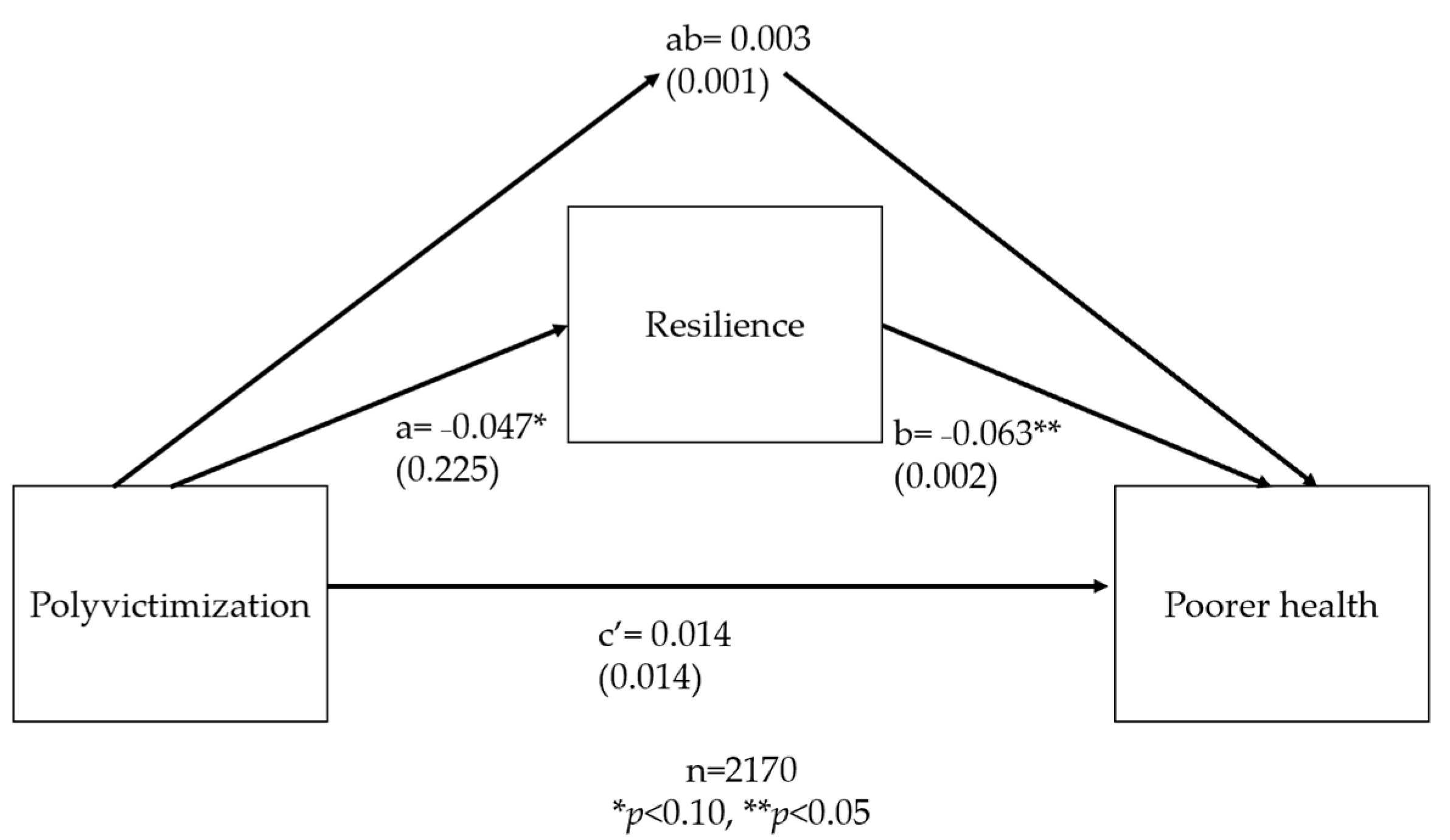
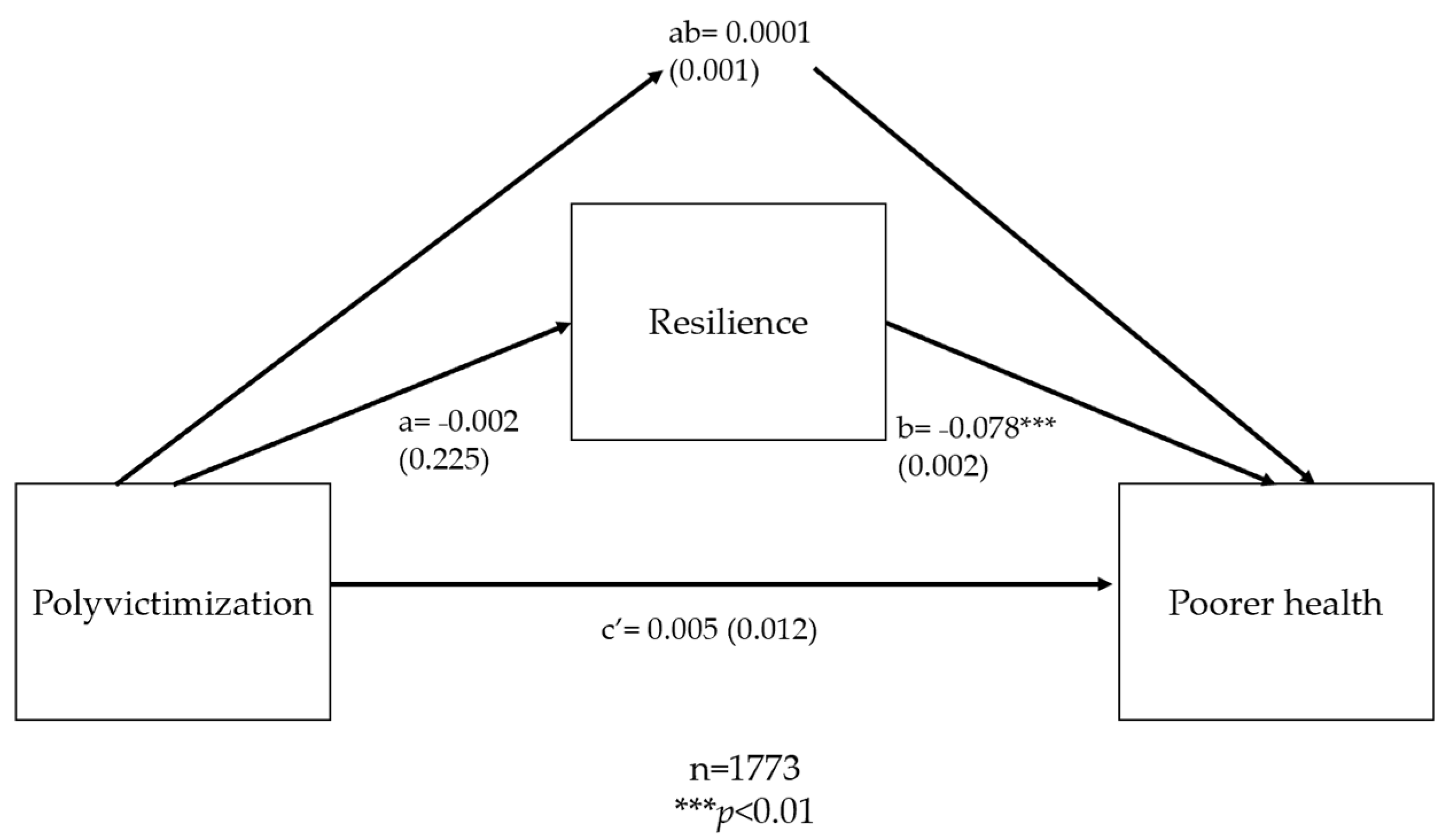
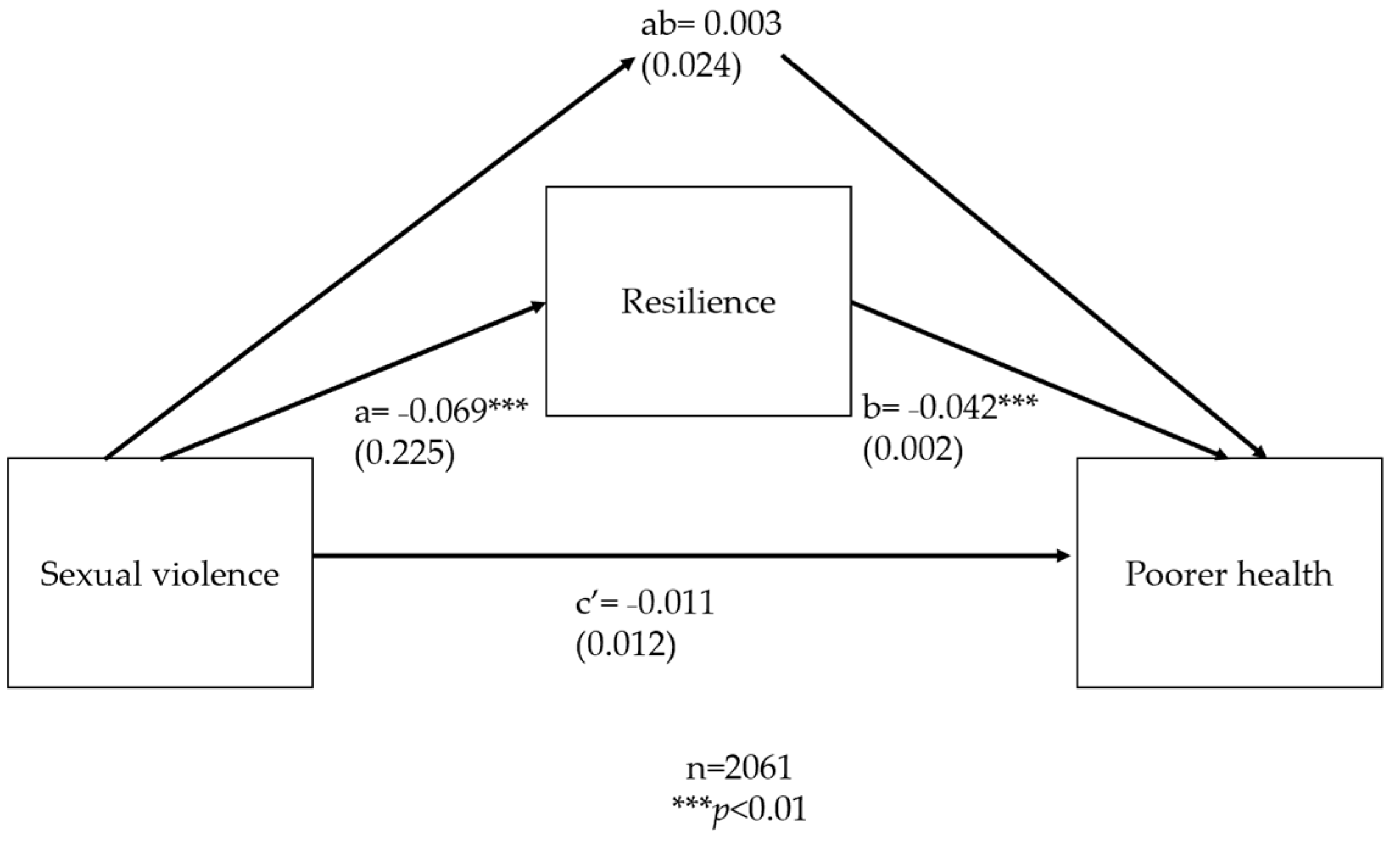
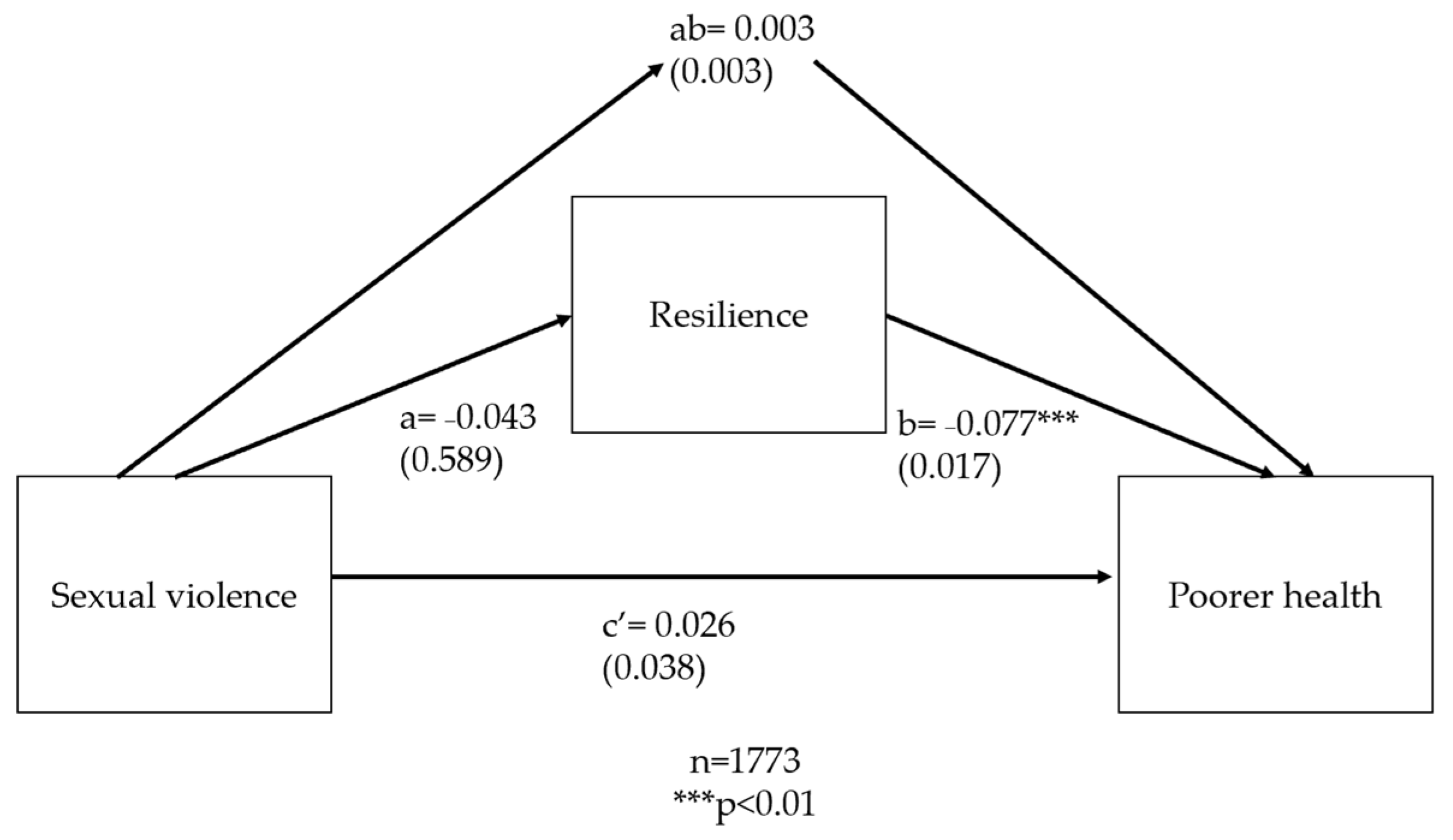
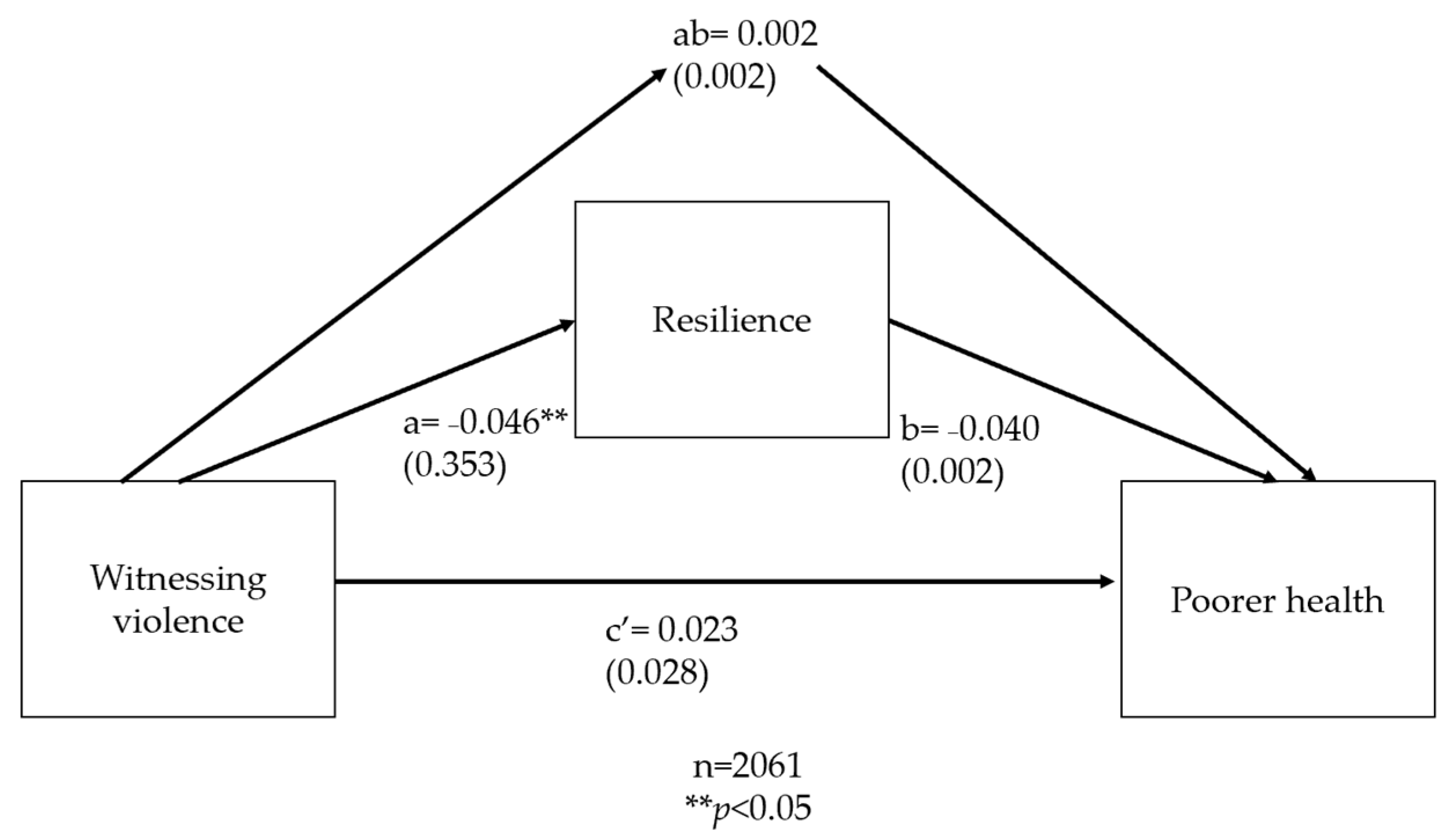
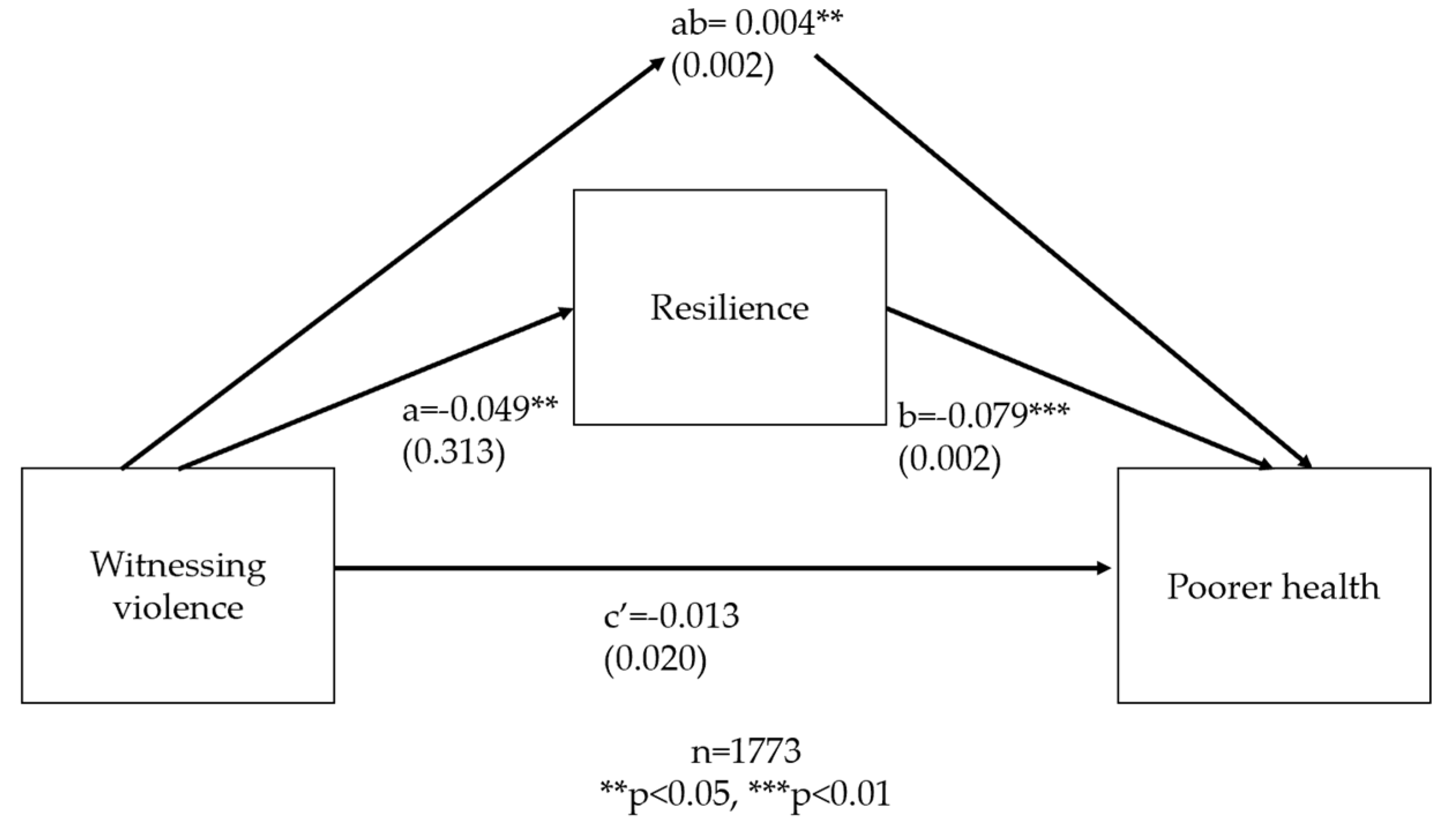
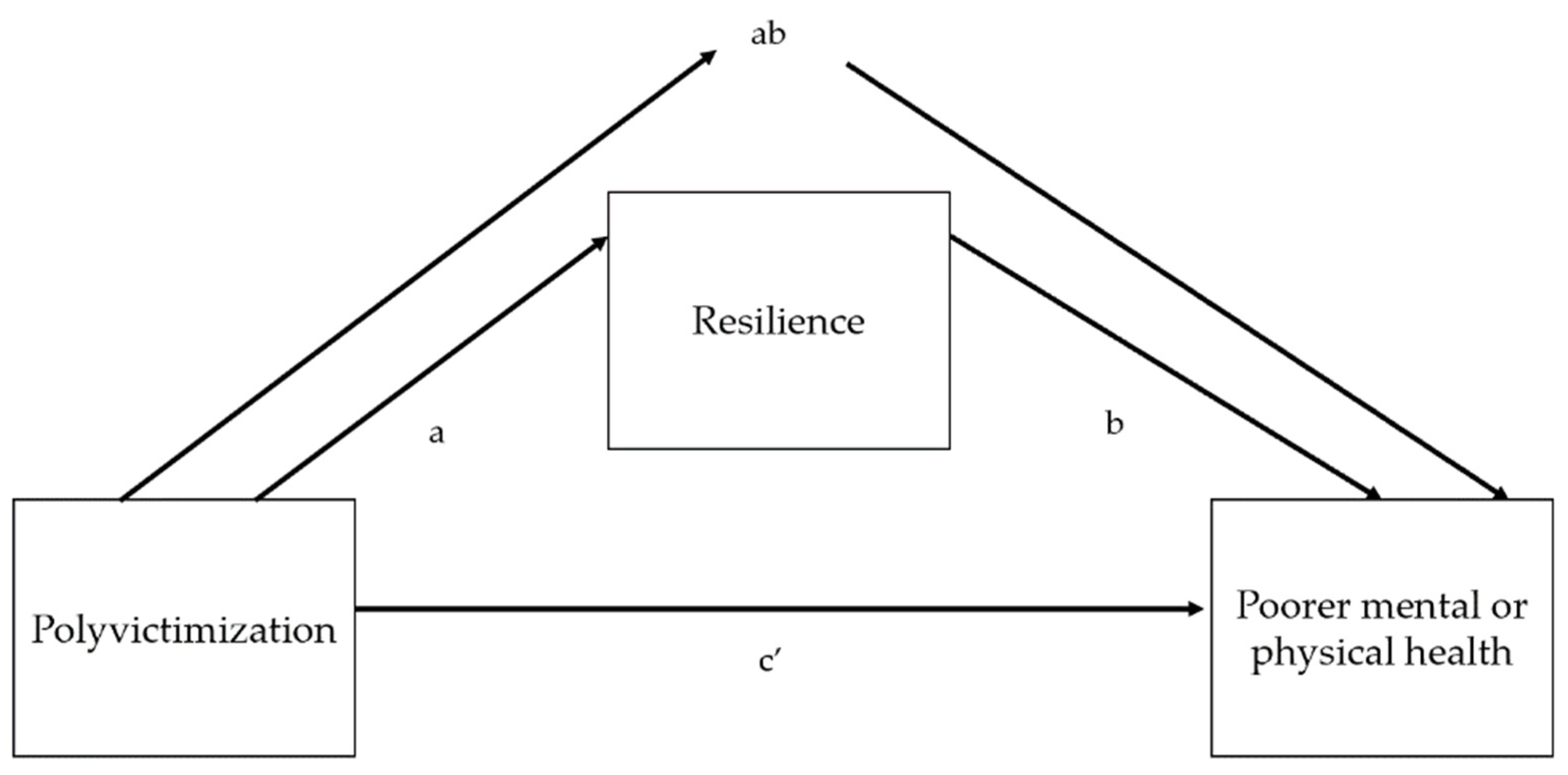
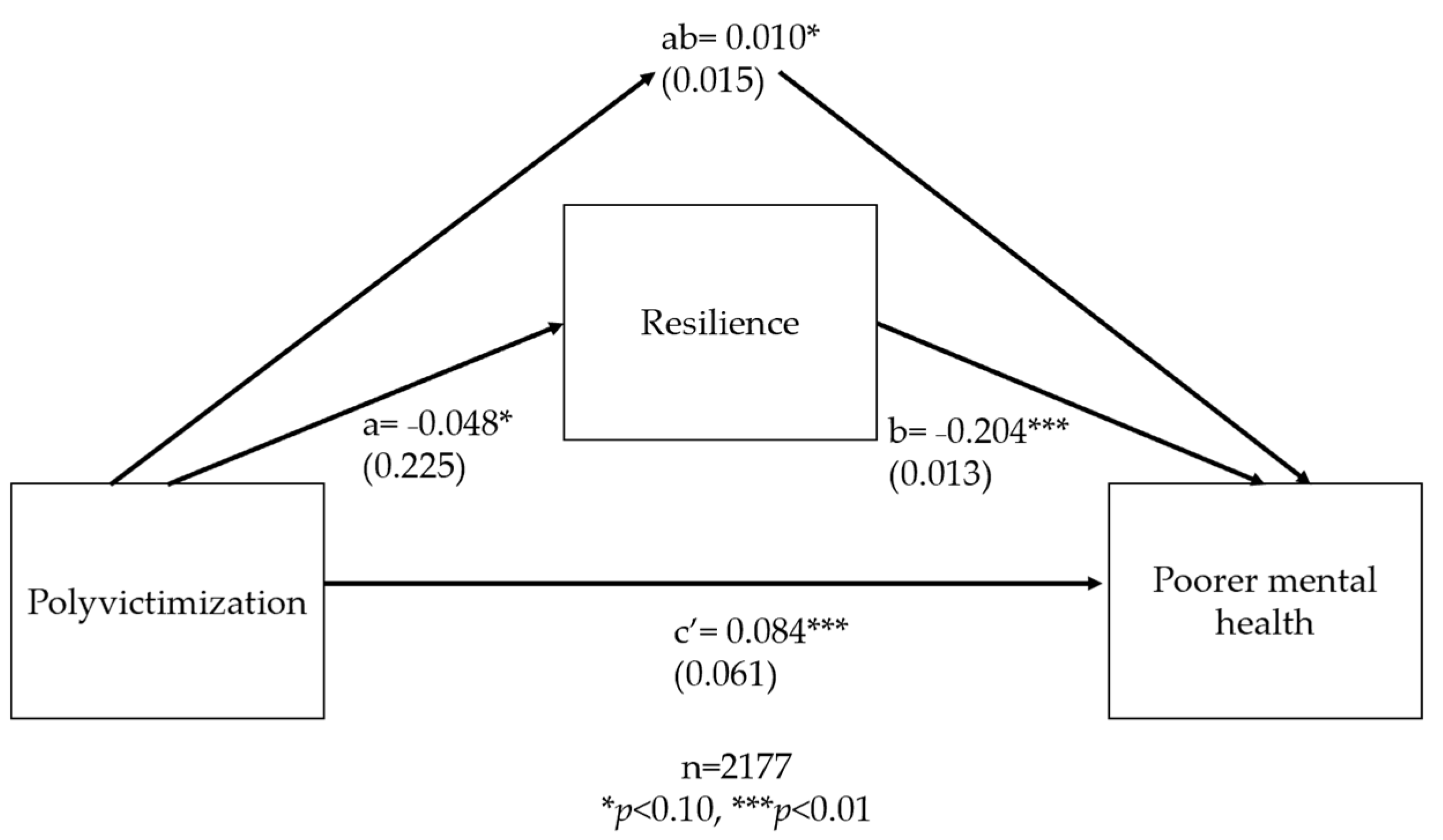
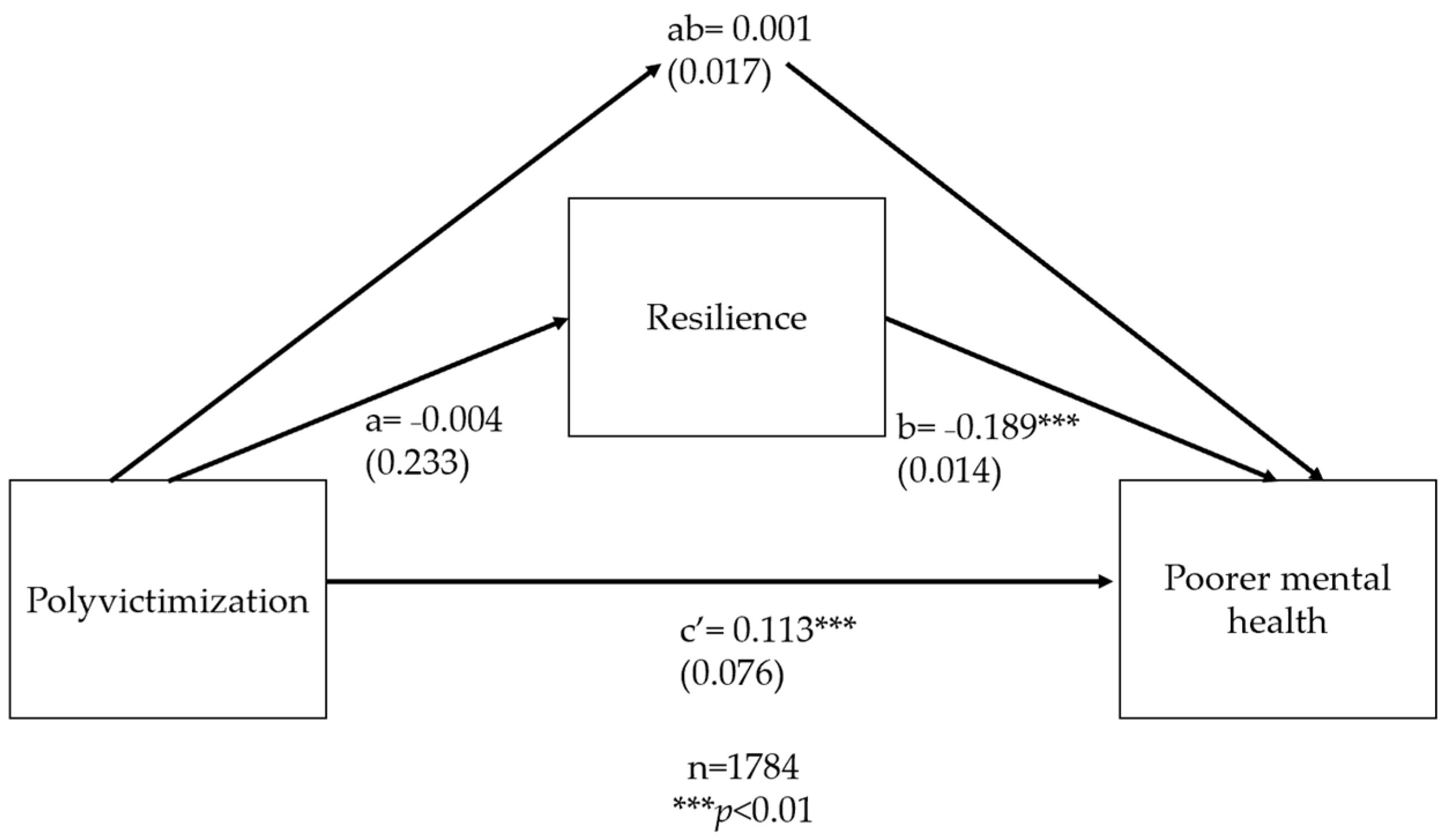
3.3. Mediation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. GAGE Survey Questions on Experiences of Violence
| Type of Violence | Survey Question(s) |
|---|---|
| Household physical violence | How often in the past 12 months were you pushed, slapped, hit beaten, or otherwise physically hurt by a parent or other adult in your household? |
| Household emotional violence | How often in the past 12 months did a parent or other adult in your household treat you poorly in another way, such as withholding food from you when others in the family were fed? How often in the past 12 months did a parent or other adult in the household yell at you or call you names? |
| Witnessing violence against mother/female guardian | How often in the past 12 months have you seen or heard your father/male guardian hit or beat your mother/female guardian? How often in the past 12 months have you seen or heard your mother/female guardian being hit by any family member other than your father/male guardian? |
| Sexual violence | In the past 12 months: Has any male person ever forced you or attempted to force you into sexual intercourse when you did not want to, for example by threatening you, holding you down, or putting you in a situation where you could not say no. Remember to include people you have known as well as strangers. (Only female participants asked) Has anyone touched you sexually when you did not want them to (this includes touching your breasts or private parts) or made you touch them sexually when you did not want them to? (Only female participants asked) Female and male participants given a card and were read: I would now like to give you a card. On this card are two pictures. No other information is written on the card. The first picture is of a sad face, the second is of a happy face. No matter what you have already told me, I would like you to put a mark below the sad face if someone has ever touched you sexually against your will, or made you do something sexual that you didn’t want to. This could have been a boyfriend or girlfriend, family member, teacher, friend, or any other person. Please put a mark below the happy face if this has never happened to you. |
| School violence | In the past 12 months: Have you ever been beaten, hit, whipped, or caned by a teacher at your school, or physically punished by a teacher in some other way? Have you ever been punished at school in another way, like being forced to run around, stand on a bench, or kneel? Have you ever been made fun of, belittled, humiliated, threatened, or scared by a teacher or other authority figure at school? (This question not included in baseline survey, only round two) |
| Peer violence | How many times in the past 12 months did you experience: teasing/name calling, being left out or ignored, having something stolen or damaged, being physically hurt, being made to do things, or being threatened with harm. |
| FGM/C | Have you yourself ever been circumcised? (Asked in adolescent female survey) Was [adolescent name] circumcised? (Asked of primary female decision-makers in adult female survey) |
Appendix B. Supplemental Path Analyses

References
- Hillis, S.; Mercy, J.; Amobi, A.; Kress, H. Global prevalence of past-year violence against children: A systematic review and minimum estimates. Pediatrics 2016, 137, e20154079. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Hidden in Plain Sight: A Statistical Analysis of Violence against Children; UNICEF: New York, NY, USA, 2014. [Google Scholar]
- African Child Policy Forum. Save the Children Sweden Violence Against Children in Ethiopia: In Their Words; African Child Policy Forum: Addis Ababa, Ethiopia, 2006. [Google Scholar]
- Hamby, S.; Finkelhor, D.; Turner, H.; Ormrod, R. The overlap of witnessing partner violence with child maltreatment and other victimizations in a nationally representative survey of youth. Child Abus. Negl. 2010, 34, 734–741. [Google Scholar] [CrossRef] [PubMed]
- United Nations Declaration on the Elimination of Violence against Women. Available online: https://www.ohchr.org/en/instruments-mechanisms/instruments/declaration-elimination-violence-against-women (accessed on 12 February 2023).
- United Nations Promotion and Protection of the Rights of Children. Available online: https://documents-dds-ny.un.org/doc/UNDOC/LTD/N22/683/04/PDF/N2268304.pdf?OpenElement (accessed on 12 February 2023).
- Gershon, A.; Minor, K.; Hayward, C. Gender, victimization, and psychiatric outcomes. Psychol. Med. 2008, 38, 1377–1391. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, D.; Ormrod, R.K.; Turner, H.A.; Hamby, S.L. Measuring poly-victimization using the Juvenile Victimization Questionnaire. Child Abus. Negl. 2005, 29, 1297–1312. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, D.; Turner, H.; Ormrod, R.; Hamby, S.L. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics 2009, 124, 1411–1423. [Google Scholar] [CrossRef]
- Le, M.T.; Holton, S.; Romero, L.; Fisher, J. Polyvictimization among children and adolescents in low-and lower-middle-income countries: A systematic review and meta-analysis. Trauma Violence Abus. 2018, 19, 323–342. [Google Scholar] [CrossRef]
- Unicef. Know Violence in Childhood Ending Violence in Childhood: Global Report 2017; Know Violence in Childhood: New Dehli, India, 2017. [Google Scholar]
- Haahr-Pedersen, I.; Ershadi, A.; Hyland, P.; Hansen, M.; Perera, C.; Sheaf, G.; Bramsen, R.H.; Spitz, P.; Vallières, F. Polyvictimization and psychopathology among children and adolescents: A systematic review of studies using the Juvenile Victimization Questionnaire. Child Abus. Negl. 2020, 107, 104589. [Google Scholar] [CrossRef]
- Ellonen, N.; Salmi, V. Poly-victimization as a life condition: Correlates of poly-victimization among Finnish children. J. Scand. Stud. Criminol. Crime Prev. 2011, 12, 20–44. [Google Scholar] [CrossRef]
- Turner, H.A.; Finkelhor, D.; Ormrod, R. Poly-victimization in a national sample of children and youth. Am. J. Prev. Med. 2010, 38, 323–330. [Google Scholar] [CrossRef]
- Finkelhor, D.; Ormrod, R.K.; Turner, H.A. Polyvictimization and trauma in a national longitudinal cohort. Dev. Psychopathol. 2007, 19, 149–166. [Google Scholar] [CrossRef]
- Charak, R.; Byllesby, B.M.; Roley, M.E.; Claycomb, M.A.; Durham, T.A.; Ross, J.; Armour, C.; Elhai, J.D. Latent classes of childhood poly-victimization and associations with suicidal behavior among adult trauma victims: Moderating role of anger. Child Abus. Negl. 2016, 62, 19–28. [Google Scholar] [CrossRef]
- Klein, H.J. Adverse Childhood Experiences and Adolescent Gang Membership: Utilizing Latent Class Analysis to Understand the Relationship. Ph.D. Thesis, Temple University, Philadelphia, PA, USA, 2020. [Google Scholar]
- Ugarte, E.; Narea, M.; Aldoney, D.; Weissman, D.G.; Hastings, P.D. Family Risk and Externalizing Problems in Chilean Children: Mediation by Harsh Parenting and Emotional Support. Child Dev. 2021, 92, 871–888. [Google Scholar] [CrossRef]
- Guedes, A.; Bott, S.; Garcia-Moreno, C.; Colombini, M. Bridging the gaps: A global review of intersections of violence against women and violence against children. Glob. Health Action 2016, 9, 31516. [Google Scholar] [CrossRef] [PubMed]
- Meier, J.S.; Dickson, S.; O’Sullivan, C.; Rosen, L.; Hayes, J. Child Custody Outcomes in Cases Involving Parental Alienation and Abuse Allegations. GWU Law School Public Law Research Paper 2019. No. 2019-56; GWU Legal Studies Research Paper No. 2019-56. Available online: https://ssrn.com/abstract=3448062 (accessed on 12 February 2023).
- Kantor, G.K.; Little, L. Defining the boundaries of child neglect: When does domestic violence equate with parental failure to protect? J. Interpers. Violence 2003, 18, 338–355. [Google Scholar] [CrossRef]
- Stanziani, M.; Cox, J. The failure of all mothers or the mother of all failures? Juror perceptions of failure to protect laws. J. Interpers. Violence 2021, 36, NP690–NP711. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. World Report on Violence against Children; UNICEF: New York, NY, USA, 2006. [Google Scholar]
- Im, H.; Swan, L.E.; Heaton, L. Polyvictimization and mental health consequences of female genital mutilation/circumcision (FGM/C) among Somali refugees in Kenya. Women Health 2020, 60, 636–651. [Google Scholar] [CrossRef] [PubMed]
- Landis, D.; Falb, K.; Michelis, I.; Bakomere, T.; Stark, L. Violence, well-being and level of participation in formal education among adolescent girls in eastern Democratic Republic of the Congo: The role of child marriage. Stud. Soc. Justice 2018, 12, 273–290. [Google Scholar] [CrossRef]
- Clarke, K.; Patalay, P.; Allen, E.; Knight, L.; Naker, D.; Devries, K. Patterns and predictors of violence against children in Uganda: A latent class analysis. BMJ Open 2016, 6, e010443. [Google Scholar] [CrossRef]
- Devries, K.M.; Child, J.C.; Allen, E.; Walakira, E.; Parkes, J.; Naker, D. School violence, mental health, and educational performance in Uganda. Pediatrics 2014, 133, e129–e137. [Google Scholar] [CrossRef]
- Heekes, S.; Kruger, C.B.; Lester, S.N.; Ward, C.L. A systematic review of corporal punishment in schools: Global prevalence and correlates. Trauma Violence Abus. 2022, 23, 52–72. [Google Scholar] [CrossRef]
- Farouki, L.; El-Dirani, Z.; Abdulrahim, S.; Akl, C.; Akik, C.; McCall, S.J. The global prevalence of female genital mutilation/cutting: A systematic review and meta-analysis of national, regional, facility, and school-based studies. PLoS Med. 2022, 19, e1004061. [Google Scholar] [CrossRef] [PubMed]
- Presler-Marshall, E.; Jones, N.; Dutton, R.; Baird, S.; Yadete, W.; Woldehanna, T.; Emirie, G.; Gezaghne, K. ‘Girls Don’t Shout If They Are Raped… That Is Taboo’: Exploring Barriers to Ethiopian Adolescents’ Freedom from Age-And Gender-Based Violence; Gender and Adolescence, Global Evidence: London, UK, 2020. [Google Scholar]
- Palermo, T.; Pereira, A.; Neijhoft, N.; Bello, G.; Buluma, R.; Diem, P.; Daban, R.A.; Kaloga, I.F.; Islam, A.; Kheam, T. Risk factors for childhood violence and polyvictimization: A cross-country analysis from three regions. Child Abus. Negl. 2019, 88, 348–361. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.; Hares, S.; Holland, P.; Acosta, A.M. Adolescent Girls’ Safety in and out of School: Evidence on Physical and Sexual Violence from across Sub-Saharan Africa. J. Dev. Stud. 2023, 59, 739–757. [Google Scholar] [CrossRef]
- Seppälä, P.; Vornanen, R.; Toikko, T. Multimorbidity and polyvictimization in children—An analysis on the association of children’s disabilities and long-term illnesses with mental violence and physical violence. Child Abus. Negl. 2021, 122, 105350. [Google Scholar] [CrossRef]
- Meinck, F.; Cluver, L.D.; Boyes, M.E.; Ndhlovu, L.D. Risk and protective factors for physical and emotional abuse victimisation amongst vulnerable children in South Africa. Child Abuse Rev. 2015, 24, 182–197. [Google Scholar] [CrossRef]
- Nace, A.; Maternowska, C.; Fernandez, B.; Cravero, K. The Violence Against Children Surveys (VACS): Using VACS data to drive programmes and policies. Glob. Public Health 2022, 17, 2807–2825. [Google Scholar] [CrossRef]
- Dahl, R.E.; Allen, N.B.; Wilbrecht, L.; Suleiman, A.B. Importance of investing in adolescence from a developmental science perspective. Nature 2018, 554, 441–450. [Google Scholar] [CrossRef]
- Murphy, M.; Jones, N.; Yadete, W.; Baird, S. Gender-norms, violence and adolescence: Exploring how gender norms are associated with experiences of childhood violence among young adolescents in Ethiopia. Glob. Public Health 2021, 16, 842–855. [Google Scholar] [CrossRef]
- Wilkins, N.; Tsao, B.; Hertz, M.F.; Davis, R.; Klevens, J. Connecting the Dots: An Overview of the Links among Multiple Forms of Violence; National Center for Injury Prevention and Control, Center for Disease Control and Prevention: Atlanta, GA, USA, 2014. [Google Scholar]
- Finkelhor, D.; Ormrod, R.K.; Turner, H.A. Poly-victimization: A neglected component in child victimization. Child Abus. Negl. 2007, 31, 7–26. [Google Scholar] [CrossRef]
- Aho, N.; Gren-Landell, M.; Svedin, C.G. The prevalence of potentially victimizing events, poly-victimization, and its association to sociodemographic factors: A Swedish youth survey. J. Interpers. Violence 2016, 31, 620–651. [Google Scholar] [CrossRef]
- Pires, A.R.; Almeida, T.C. Risk Factors of Poly-Victimization and the Impact on Delinquency in Youth: A Systematic Review. Crime Delinq. 2023, 1–19. [Google Scholar] [CrossRef]
- Maguire-Jack, K.; Font, S.A. Community and individual risk factors for physical child abuse and child neglect: Variations by poverty status. Child Maltreat. 2017, 22, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Maternowska, C.; Fry, D.; Potts, A.; Casey, T. Beyond risk factors: Structural drivers of violence affecting children. In Children and Peace; Springer: New York, NY, USA, 2020. [Google Scholar]
- WHO. Constitution of the World Health Organization; WHO: Geneva, Switzerland, 1948. [Google Scholar]
- Turner, H.A.; Shattuck, A.; Finkelhor, D.; Hamby, S. Effects of poly-victimization on adolescent social support, self-concept, and psychological distress. J. Interpers. Violence 2017, 32, 755–780. [Google Scholar] [CrossRef] [PubMed]
- Samms-Vaughan, M.; Lambert, M. The impact of polyvictimisation on children in LMICs: The case of Jamaica. Psychol. Health Med. 2017, 22, 67–80. [Google Scholar] [CrossRef] [PubMed]
- Sherr, L.; Hensels, I.S.; Skeen, S.; Tomlinson, M.; Roberts, K.J.; Macedo, A. Exposure to violence predicts poor educational outcomes in young children in South Africa and Malawi. Int. Health 2016, 8, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Villaveces, A.; Shankar, V.; Palomeque, F.; Padilla, M.; Kress, H. Association between violence and mental distress, self-harm and suicidal ideation and attempts among young people in Malawi. Inj. Prev. 2022, 28, 446–452. [Google Scholar] [CrossRef]
- La Flair, L.N.; Reboussin, B.A.; Storr, C.L.; Letourneau, E.; Green, K.M.; Mojtabai, R.; Pacek, L.R.; Alvanzo, A.A.; Cullen, B.; Crum, R.M. Childhood abuse and neglect and transitions in stages of alcohol involvement among women: A latent transition analysis approach. Drug Alcohol Depend. 2013, 132, 491–498. [Google Scholar] [CrossRef]
- Gómez-Baya, D.; López-Gaviño, F.; Ibáñez-Alfonso, J.A. Mental Health, Quality of Life and Violence Exposure in Low-Socioeconomic Status Children and Adolescents of Guatemala. Int. J. Environ. Res. Public Health 2020, 17, 7620. [Google Scholar] [CrossRef]
- Sui, X.; Massar, K.; Kessels, L.T.; Reddy, P.S.; Ruiter, R.A.; Sanders-Phillips, K. Violence exposure in south African adolescents: Differential and cumulative effects on psychological functioning. J. Interpers. Violence 2021, 36, 4084–4110. [Google Scholar] [CrossRef]
- Kamndaya, M.; Pisa, P.T.; Chersich, M.F.; Decker, M.R.; Olumide, A.; Acharya, R.; Cheng, Y.; Brahmbhatt, H.; Delany-Moretlwe, S. Intersections between polyvictimisation and mental health among adolescents in five urban disadvantaged settings: The role of gender. BMC Public Health 2017, 17, 41–50. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Kegler, S.R.; Chiang, L.; Kress, H. Effects of poly-victimization before age 18 on health outcomes in young Kenyan adults: Violence against children survey. Violence Vict. 2019, 34, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Pigott, T.D.; Watson, A.; Reuben, K.; O’Hara, K.; Massetti, G.; Fang, X.; Self-Brown, S. Childhood polyvictimization and associated health outcomes: A systematic scoping review. Trauma Violence Abus. 2023, 24, 1579–1592. [Google Scholar] [CrossRef] [PubMed]
- Nath, P.; Pradhan, R.K. Influence of positive affect on physical health and psychological well-being: Examining the mediating role of psychological resilience. J. Health Manag. 2012, 14, 161–174. [Google Scholar] [CrossRef]
- Mitrani, N. Examining the Relationship between Victimization History, Resiliency Factors, and Trauma-Related Symptoms Using Structural Equation Modeling. Ph.D. Thesis, University of Central Arkansas, Conway, AR, USA, 2017. [Google Scholar]
- Karatzias, T.; Jowett, S.; Yan, E.; Raeside, R.; Howard, R. Depression and resilience mediate the relationship between traumatic life events and ill physical health: Results from a population study. Psychol. Health Med. 2017, 22, 1021–1031. [Google Scholar] [CrossRef]
- Kelifa, M.O.; Yang, Y.; Herbert, C.; He, Q.; Wang, P. Psychological resilience and current stressful events as potential mediators between adverse childhood experiences and depression among college students in Eritrea. Child Abus. Negl. 2020, 106, 104480. [Google Scholar] [CrossRef]
- Ran, H.; Cai, L.; He, X.; Jiang, L.; Wang, T.; Yang, R.; Xu, X.; Lu, J.; Xiao, Y. Resilience mediates the association between school bullying victimization and self-harm in Chinese adolescents. J. Affect. Disord. 2020, 277, 115–120. [Google Scholar] [CrossRef]
- Ross, N.; Gilbert, R.; Torres, S.; Dugas, K.; Jefferies, P.; McDonald, S.; Savage, S.; Ungar, M. Adverse childhood experiences: Assessing the impact on physical and psychosocial health in adulthood and the mitigating role of resilience. Child Abus. Negl. 2020, 103, 104440. [Google Scholar] [CrossRef]
- GAGE. Gender and Adolescence: Global Evidence. Available online: https://www.gage.odi.org/ (accessed on 23 August 2020).
- GAGE. Consortium Gender and Adolescence: Why Understanding Adolescent Capabilities, Change Strategies, and Context Matters; Gender and Adolescence, Global Evidence: London, UK, 2019. [Google Scholar]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Maternowska, M.C.; Potts, A. The Multi-Country Study on the Drivers of Violence Affecting Children: A Child-Centred Integrated Framework for Violence Prevention; UNICEF Office of Research: Florence, Italy, 2017. [Google Scholar]
- Jones, K.J. Measuring Polyvictimization among Vulnerable Children: A Confirmatory Factor Analysis. Ph.D. Thesis, Marquette University, Milwaukee, WI, USA, 2019. [Google Scholar]
- Maternowska, M.C.; Potts, A.; Fry, D.; Casey, T. Research That Drives Change: Conceptualizing and Conducting Nationally Led Violence Prevention Research; UNICEF Office of Research: Florence, Italy, 2018. [Google Scholar]
- Jones, N.; Baird, S.; Lunin, L. GAGE Research Design, Sample and Methodology; Gender and Adolescence, Global Evidence: London, UK, 2018. [Google Scholar]
- Hicks, J.; Jones, N.; Woldehanna, T.; Baird, S. GAGE Ethiopia Baseline Quantitative Research Design and Sample; Quantitative Research Manual Series; Gender and Adolescence, Global Evidence: London, UK, 2019. [Google Scholar]
- Jones, N.; Baird, S.; Hicks, J.; Presler-Marshall, E.; Woldehanna, T.; Yadete, W. Adolescent Well-Being in Ethiopia: Exploring Gendered Capabilities, Contexts and Change Strategies; Gender and Adolescence, Global Evidence: London, UK, 2019. [Google Scholar]
- Central Statistical Agency/Ethiopia; ICF. Ethiopia Demographic and Health Survey 2016; CSA and ICF: Addis Ababa, Ethiopia; Rockville, MD, USA, 2016. [Google Scholar]
- World Bank. Ethiopia Poverty Assessment: Harnessing Continued Growth for Accelerated Poverty Reduction; The World Bank: Washington, DC, USA, 2020. [Google Scholar]
- UN News. Tigray’s Children in Crisis and Beyond Reach, after Months of Conflict: UNICEF. Available online: https://news.un.org/en/story/2021/01/1083102 (accessed on 7 March 2021).
- UN Women Africa. Supporting Development of a National Policy and Strategy on GBV Prevention and Response in Ethiopia. Available online: https://africa.unwomen.org/en/stories/news/2022/11/supporting-development-of-a-national-policy-and-strategy-on-gbv-prevention-and-response-in-ethiopia (accessed on 12 August 2023).
- Kebede, E.; Collins, M.E. Policy development for children in Ethiopia: Progress and next steps. Child. Geogr. 2023, 21, 235–241. [Google Scholar] [CrossRef]
- Girls Not Brides. Ethiopia. Available online: https://www.girlsnotbrides.org/learning-resources/child-marriage-atlas/regions-and-countries/ethiopia/ (accessed on 13 August 2023).
- Federal Democratic Republic of Ethiopia, Ministry of Women, Children, and Youth. National Costed Roadmap to End Child Marriage and FGM/C 2020–2024; Federal Democratic Republic of Ethiopia: Addis Ababa, Ethiopia, 2019. [Google Scholar]
- Worku, D.; Gebremariam, A.; Jayalakshmi, S. Child sexual abuse and its outcomes among high school students in southwest Ethiopia. Trop. Doct. 2006, 36, 137–140. [Google Scholar] [CrossRef]
- Wondie, Y.; Zemene, W.; Tafesse, B.; Reschke, K.; Schröder, H. The psychosocial consequences of child sexual abuse in Ethiopia: A case-control comparative analysis. J. Interpers. Violence 2011, 26, 2025–2041. [Google Scholar] [CrossRef]
- Baird, S.; Bhutta, Z.A.; Hamad, B.A.; Hicks, J.H.; Jones, N.; Muz, J. Do restrictive gender attitudes and norms influence physical and mental health during very young adolescence? Evidence from Bangladesh and Ethiopia. SSM-Pop Health 2019, 9, 100480. [Google Scholar] [CrossRef] [PubMed]
- GAGE Toolkits and Survey Instruments. Available online: https://www.gage.odi.org/types/method-tools-and-guides/ (accessed on 3 August 2020).
- Foy, P.; Olson, J. TIMSS 2015 User Guide for the International Database. Supplement 1. International Version of the TIMSS 2015 Context Questionnaires; TIMSS & PIRLS International Study Center, Boston College: Chestnut Hill, MA, USA, 2017. [Google Scholar]
- Filmer, D.; Pritchett, L.H. Estimating wealth effects without expenditure data—Or tears: An application to educational enrollments in states of India. Demography 2001, 38, 115–132. [Google Scholar]
- Washington Group on Disability Statistics. The Washington Group Short Set on Functioning (WG-SS). Available online: https://www.washingtongroup-disability.com/ (accessed on 7 March 2021).
- World Bank. The Living Standards Measurement Study. Available online: https://www.worldbank.org/en/programs/lsms (accessed on 5 March 2021).
- Oxford Poverty & Human Development Initiative. Global Multidimensional Poverty Index Questionnaire. Available online: https://ophi.org.uk/multidimensional-poverty-index/ (accessed on 5 March 2021).
- Zheng, X.; Fang, Z.; Shangguan, S.; Fang, X. Associations between childhood maltreatment and educational, health and economic outcomes among middle-aged Chinese: The moderating role of relative poverty. Child Abus. Negl. 2022, 130, 105162. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M.; Liebenberg, L. Assessing resilience across cultures using mixed methods: Construction of the child and youth resilience measure. J. Mix. Methods Res. 2011, 5, 126–149. [Google Scholar] [CrossRef]
- Liebenberg, L.; Ungar, M.; LeBlanc, J.C. The CYRM-12: A brief measure of resilience. Can. J. Public Health 2013, 104, e131–e135. [Google Scholar] [CrossRef] [PubMed]
- Russell, B.S.; Collins, C.M.; Tomkunas, A.J.; Hutchison, M. Exploring the factor structure of the child and youth resilience measure (CYRM-12) for young children in a disadvantaged community. Child. Youth Serv. Rev. 2021, 120, 105746. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Williams, P. User’s Guide to the General Health Questionnaire; NFER-NELSON, Windsor: Berkshire, UK, 1988. [Google Scholar]
- GL Assessment General Health Questionnaire. Available online: https://www.gl-assessment.co.uk/products/general-health-questionnaire-ghq/ (accessed on 14 March 2021).
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting anxiety and depression in general medical settings. Br. Med. J. 1988, 297, 897–899. [Google Scholar] [CrossRef]
- National Institutes of Health. Health Information National Trends Survey. Available online: https://hints.cancer.gov/docs/Instruments/HINTS5_Cycle2_Annotated_Instrument_English.pdf (accessed on 3 August 2020).
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 17; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Feng, J.; Hsieh, Y.; Hwa, H.; Huang, C.; Wei, H.; Shen, A.C. Childhood poly-victimization and children’s health: A nationally representative study. Child Abus. Negl. 2019, 91, 88–94. [Google Scholar] [CrossRef]
- Vaillancourt, T.; Hymel, S.; McDougall, P. The biological underpinnings of peer victimization: Understanding why and how the effects of bullying can last a lifetime. Theory Pract. 2013, 52, 241–248. [Google Scholar] [CrossRef]
- Knack, J.M.; Jensen-Campbell, L.A.; Baum, A. Worse than sticks and stones? Bullying is associated with altered HPA axis functioning and poorer health. Brain Cogn. 2011, 77, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Abebe, S.; Dessalegn, M.; Hailu, Y.; Makonnen, M. Prevalence and barriers to ending female genital cutting: The case of Afar and Amhara Regions of Ethiopia. Int. J. Environ. Res. Public Health 2020, 17, 7960. [Google Scholar] [CrossRef] [PubMed]
- Hodes, G.E.; Epperson, C.N. Sex differences in vulnerability and resilience to stress across the life span. Biol. Psychiatry 2019, 86, 421–432. [Google Scholar] [CrossRef]
- Epperson, C.N.; Sammel, M.D.; Bale, T.L.; Kim, D.R.; Conlin, S.; Scalice, S.; Freeman, K.; Freeman, E.W. Adverse childhood experiences and risk for first-episode major depression during the menopause transition. J. Clin. Psychiatry 2017, 78, 2557. [Google Scholar] [CrossRef]
- Abdullah, A.; Cudjoe, E.; Jordan, L.P.; Emery, C.R. Child polyvictimization in Zongo communities in Ghana: Young people’s reflections on systemic resilience enablers. Child Abus. Negl. 2021, 119, 105075. [Google Scholar] [CrossRef]
- Stoltzfus, J.C. Logistic regression: A brief primer. Acad. Emerg. Med. 2011, 18, 1099–1104. [Google Scholar] [CrossRef]
- Shamu, S.; Gevers, A.; Mahlangu, B.P.; Jama Shai, P.N.; Chirwa, E.D.; Jewkes, R.K. Prevalence and risk factors for intimate partner violence among Grade 8 learners in urban South Africa: Baseline analysis from the Skhokho Supporting Success cluster randomised controlled trial. Int. Health 2016, 8, 18–26. [Google Scholar] [CrossRef]
- Wood, S.L.; Sommers, M.S. Consequences of intimate partner violence on child witnesses: A systematic review of the literature. J. Child Adolesc. Psychiatr. Nurs. 2011, 24, 223–236. [Google Scholar] [CrossRef]
- Moylan, C.A.; Herrenkohl, T.I.; Sousa, C.; Tajima, E.A.; Herrenkohl, R.C.; Russo, M.J. The effects of child abuse and exposure to domestic violence on adolescent internalizing and externalizing behavior problems. J. Fam. Violence 2010, 25, 53–63. [Google Scholar] [CrossRef]
- Karlsson, M.E.; Temple, J.R.; Weston, R.; Le, V.D. Witnessing interparental violence and acceptance of dating violence as predictors for teen dating violence victimization. Violence Women 2016, 22, 625–646. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.; Howard, A.; Gleckel, J.; Ogoti, C.; Karlsson, J.; Hynes, M.; Mwangi, M. Cycle of violence among young Kenyan women: The link between childhood violence and adult physical intimate partner violence in a population-based survey. Child Abus. Negl. 2018, 84, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Tenkorang, E.Y. A survey analysis of barriers to help-seeking at the Ghana domestic violence and victim support unit (DOVVSU). J. Fam. Violence 2022, 37, 601–611. [Google Scholar] [CrossRef]
- Abramsky, T.; Devries, K.; Kiss, L.; Nakuti, J.; Kyegombe, N.; Starmann, E.; Cundill, B.; Francisco, L.; Kaye, D.; Musuya, T. Findings from the SASA! Study: A cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med. 2014, 12, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Kyegombe, N.; Abramsky, T.; Devries, K.M.; Michau, L.; Nakuti, J.; Starmann, E.; Musuya, T.; Heise, L.; Watts, C. What is the potential for interventions designed to prevent violence against women to reduce children’s exposure to violence? Findings from the SASA! study, Kampala, Uganda. Child Abus. Negl. 2015, 50, 128–140. [Google Scholar] [CrossRef]
- Toska, E.; Gittings, L.; Hodes, R.; Cluver, L.D.; Govender, K.; Chademana, K.E.; Gutiérrez, V.E. Resourcing resilience: Social protection for HIV prevention amongst children and adolescents in Eastern and Southern Africa. Afr. J. AIDS Res. 2016, 15, 123–140. [Google Scholar] [CrossRef]
- Singla, D.R.; Waqas, A.; Hamdani, S.U.; Suleman, N.; Zafar, S.W.; Saeed, K.; Servili, C.; Rahman, A. Implementation and effectiveness of adolescent life skills programs in low-and middle-income countries: A critical review and meta-analysis. Behav. Res. Ther. 2020, 130, 103402. [Google Scholar] [CrossRef]
- Howarth, E.; Moore, T.H.; Welton, N.J.; Lewis, N.; Stanley, N.; MacMillan, H.; Shaw, A.; Hester, M.; Bryden, P.; Feder, G. IMPRoving Outcomes for children exposed to domestic ViolencE (IMPROVE): An evidence synthesis. Public Health Res. 2016, 4, 1–342. [Google Scholar] [CrossRef]
- Graham-Bermann, S.A.; Miller-Graff, L. Community-based intervention for women exposed to intimate partner violence: A randomized control trial. J. Fam. Psychol. 2015, 29, 537. [Google Scholar] [CrossRef]
- Anderson, K.; Van Ee, E. Mothers and children exposed to intimate partner violence: A review of treatment interventions. Int. J. Environ. Res. Public Health. 2018, 15, 1955. [Google Scholar] [CrossRef]
- Jamieson, L.; Mathews, S.; Röhrs, S. Stopping Family Violence: Integrated Approaches to Address Violence against Women and Children; Children’s Institute, University of Cape Town: Cape Town, South African, 2018. [Google Scholar]
- de Vries, T.R.; Arends, I.; Oldehinkel, A.J.; Bültmann, U. Associations between type of childhood adversities and labour market participation and employment conditions in young adults. J. Epidemiol. Community Health 2023, 77, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Rodwell, L.; Romaniuk, H.; Nilsen, W.; Carlin, J.B.; Lee, K.J.; Patton, G.C. Adolescent mental health and behavioural predictors of being NEET: A prospective study of young adults not in employment, education, or training. Psychol. Med. 2018, 48, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.; Reiss, F.; Voss, C.; Wüstner, A.; Meyrose, A.; Hölling, H.; Ravens-Sieberer, U. Mental health and well-being from childhood to adulthood: Design, methods and results of the 11-year follow-up of the BELLA study. Eur. Child Adolesc. Psychiatry 2021, 30, 1559–1577. [Google Scholar] [CrossRef] [PubMed]

| Type of Violence | Survey Response Options | Variable Construction | Number of Survey Items Used to Construct Variable |
|---|---|---|---|
| Household physical violence | Never happened, happened once, and happened more than once | Dichotomized to 1 if happened once or more than once reported or 0 if never happened | One |
| Household emotional violence | Never happened, happened once, and happened more than once | Dichotomized to 1 if happened once or more than once reported on either item or 0 if never happened on all items | Two |
| Sexual violence | Yes, no, refused, or don’t know Happy face, sad face, or no image chosen | Dichotomized to 1 if yes reported on either item or 0 if no, refused, or don’t know on all items Dichotomized to 1 if sad face chosen or 0 if happy face or no image chosen | Two 2 One 3 |
| Witnessing violence against mother/female guardian | Never happened, happened once, and happened more than once | Dichotomized to 1 if happened once, more than once, or refused reported on either item or 0 if never happened on all items | Two |
| Peer violence | Never, once, or more than once | Dichotomized to 1 if happened once or more than once or 0 if never | Six |
| School violence | Yes, no, refused, or don’t know | Dichotomized to 1 if yes or 0 if no, refused, or don’t know | Three |
| FGM/C | Yes, no, refused, or don’t know | Dichotomized to 1 if yes or refused, or 0 if no or don’t know | Two |
| Level | Covariate | Survey Response Options | Variable Construction |
|---|---|---|---|
| Individual level | Adolescent age | Numeric | Continuous |
| Biological sex | Female or male | Female = 1, male = 0 | |
| Disability status | Either yes, no, refused, or don’t know options or no difficulty, some difficulty, a lot of difficulty, or cannot do at all. | Questions covered six domains of functioning including seeing, hearing, walking, self-care, cognition, and communication (understanding and being understood). Adolescents who responded with no, refused, don’t know, or some difficulty in all six domains were 0, no disability. Adolescents who responded with either a lot of difficulty or cannot do at all to at least one of the six domains were 1, have a disability. | |
| Orphan status (one or both parents deceased) | Yes, no, refused, or don’t know | 0 (no, refused, or don’t know) indicating that neither the biological father or biological mother were reported to have died and 1 (yes) if either the biological father or mother were reported to have died. | |
| Gender attitudes | Agree, partially agree, disagree, refused, or don’t know | 32 gender attitude questions covering domains of education, time use, financial inclusion and economic empowerment, relationships and marriage, and sexual and reproductive health. 1 = agree or partially agree, 0 = refused, or don’t know, or disagree, where agreement represents a gendered response and is reverse coded for items for which agreements suggests a nongendered response). Gender attitude scores were summed and standardized; higher scores reflect more inequitable gender attitudes and norms. | |
| Household level | Household size | Numeric | Continuous variable for household size was calculated from the household roster of the adult female module by adding the number of adults and the number of children who were reported to typically live in the household. |
| Living in a female-headed household | Male, female, refused, don’t know | Female = 1, male = 0, refused, or don’t know. | |
| Household head literacy | Yes, no, refused, or don’t know | Cannot read or write = 1, can read or write = 0, refused, or don’t know | |
| Household poverty | Whether the household owns a given item (yes, no, refused, or don’t know) | Asset deciles created using principal component analysis to capture material assets using an asset list from the adult female module [79,82]. Yes = 1, no = 0, refused, or don’t know. | |
| Parental alcohol or drug use | Yes, no, refused, not applicable, or don’t know | Dichotomized to yes = 1, no = 0, refused, or don’t know. | |
| Community level | Gender norms | Agree, partially agree, disagree | Fourteen norms-related questions (Domains and scoring same as in gender attitudes). |
| Type of location | Rural or urban | 0 = rural, 1 = urban |
| Sex | Polyvictimized N (%) | Non-Polyvictimized N (%) | Household Physical Violence N (%) | Household Emotional Violence N (%) | Sexual Violence N (%) | Witnessing Violence N (%) | Peer Violence N (%) | School-Based Violence N (%) | FGC/M N (%) |
|---|---|---|---|---|---|---|---|---|---|
| Male | 959 (53.49) | 854 (47.10) | 591 (32.60) | 842 (46.62) | 70 (3.86) | 177 (9.76) | 690 (38.48) | 911 (50.44) | n/a |
| Female | 1094 (50.00) | 1094 (50.00) | 493 (22.27) | 775 (35.08) | 158 (7.15) | 199 (8.99) | 491 (22.44) | 715 (32.37) | 1031 (46.57) |
| Overall | 2053 (51.57) | 1948 (48.93) | 1084 (26.92) | 1617 (40.27) | 228 (5.67) | 376 (9.34) | 1181 (29.67) | 1626 (40.50) | n/a |
| Panel A: Females | Female, Overall | Female, Non-Polyvictimized | Female, Polyvictimized | ||||||
| N | Mean | sd | N | Mean | sd | N | Mean | sd | |
| Resilience Score (higher scores = more resilient, max = 48) | 2213 | 31.82 | 4.28 | 1094 | 32.21 | 4.11 | 1094 | 31.45 | 4.40 |
| Poor health | 2214 | 0.11 | 0.32 | 1094 | 0.11 | 0.31 | 1094 | 0.12 | 0.32 |
| Score on GHQ-12 (0–12, higher = more distress) | 2214 | 0.90 | 1.50 | 1094 | 0.71 | 1.30 | 1094 | 1.10 | 1.67 |
| Age at R2 survey | 2214 | 12.89 | 0.90 | 1094 | 12.93 | 0.89 | 1094 | 12.86 | 0.90 |
| Has a disability | 2213 | 0.05 | 0.21 | 1093 | 0.04 | 0.20 | 1094 | 0.05 | 0.22 |
| 1 or both parents are deceased | 2214 | 0.09 | 0.29 | 1094 | 0.08 | 0.28 | 1094 | 0.10 | 0.29 |
| Household head is female | 2214 | 0.18 | 0.39 | 1094 | 0.17 | 0.37 | 1094 | 0.20 | 0.40 |
| Household head illiterate | 2214 | 0.63 | 0.48 | 1094 | 0.60 | 0.49 | 1094 | 0.65 | 0.48 |
| Standardized gender attitudes index | 2214 | 0.37 | 0.66 | 1094 | 0.30 | 0.66 | 1094 | 0.44 | 0.65 |
| Standardized gender norms index | 2214 | 0.10 | 1.00 | 1094 | 0.10 | 1.00 | 1094 | 0.11 | 1.01 |
| Household size | 2207 | 6.31 | 2.30 | 1089 | 6.24 | 2.34 | 1093 | 6.38 | 2.26 |
| Either parent/guardian drinks alcohol or uses chat | 2214 | 0.54 | 0.50 | 1094 | 0.48 | 0.50 | 1094 | 0.59 | 0.49 |
| Standardized index of household assets (decile) | 2203 | 5.19 | 2.99 | 1087 | 5.24 | 3.04 | 1091 | 5.14 | 2.95 |
| Lives in urban area | 2214 | 0.13 | 0.33 | 1094 | 0.11 | 0.32 | 1094 | 0.14 | 0.35 |
| Panel B: Males | Male, Overall | Male, Non-Polyvictimized | Male, Polyvictimized | ||||||
| N | Mean | sd | N | Mean | sd | N | Mean | sd | |
| Resilience Score (higher = more resilient, max = 48) | 1809 | 32.33 | 3.79 | 343 | 31.53 | 4.64 | 959 | 32.24 | 3.56 |
| Poor health | 1807 | 0.08 | 0.27 | 343 | 0.08 | 0.27 | 959 | 0.08 | 0.27 |
| Score on GHQ-12 (0–12, higher = more distress) | 1810 | 1.02 | 1.55 | 343 | 0.80 | 1.30 | 959 | 1.20 | 1.71 |
| Age at R2 survey | 1813 | 12.98 | 0.90 | 343 | 13.05 | 0.94 | 959 | 12.95 | 0.91 |
| Has a disability | 1810 | 0.07 | 0.25 | 343 | 0.08 | 0.27 | 959 | 0.07 | 0.26 |
| 1 or both parents are deceased | 1812 | 0.09 | 0.29 | 343 | 0.09 | 0.28 | 959 | 0.10 | 0.30 |
| Household head is female | 1813 | 0.16 | 0.36 | 343 | 0.19 | 0.39 | 959 | 0.16 | 0.37 |
| Household head illiterate | 1813 | 0.59 | 0.49 | 343 | 0.64 | 0.48 | 959 | 0.59 | 0.49 |
| Standardized gender attitudes index | 1813 | 0.49 | 0.62 | 343 | 0.59 | 0.64 | 959 | 0.49 | 0.61 |
| Standardized gender norms index | 1813 | 0.04 | 0.98 | 343 | 0.08 | 0.99 | 959 | 0.06 | 1.01 |
| Household size | 1804 | 6.11 | 2.21 | 341 | 5.74 | 2.44 | 954 | 6.20 | 2.19 |
| Either parent/guardian drinks alcohol or uses chat | 1813 | 0.50 | 0.50 | 343 | 0.38 | 0.49 | 959 | 0.56 | 0.50 |
| Standardized index of household assets (decile) | 1804 | 5.41 | 2.84 | 341 | 5.40 | 2.78 | 954 | 5.29 | 2.87 |
| Lives in urban area | 1813 | 0.17 | 0.38 | 343 | 0.11 | 0.31 | 959 | 0.20 | 0.40 |
| Score on GHQ-12 (0–12, Higher = More Mental Distress) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Panel A: Females | Panel B: Males | |||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Polyvictimized | 0.386 *** (0.067) | 0.338 *** (0.067) | 0.301 *** (0.066) | 0.298 *** (0.066) | 0.284 *** (0.064) | 0.377 *** (0.079) | 0.359 *** (0.077) | 0.367 *** (0.079) | 0.361 *** (0.078) | 0.357 *** (0.079) |
| Sample size | 2188 | 2177 | 2177 | 2177 | 2177 | 1793 | 1784 | 1784 | 1784 | 1784 |
| Score on GHQ-12 (0–12, Higher = More Mental Distress) | ||||
|---|---|---|---|---|
| Panel A: Females | Panel B: Males | |||
| Unadjusted Coefficient | Adjusted Coefficient | Unadjusted Coefficient | Adjusted Coefficient | |
| Sexually victimized | 0.450 *** (0.158) | 0.439 *** (0.146) | 0.390 (0.278) | 0.351 (0.254) |
| Witnessed violence against mother/female guardian | 0.530 *** (0.152) | 0.507 *** (0.146) | 0.803 *** (0.189) | 0.695 *** (0.178) |
| Experienced school violence | 0.076 (0.072) | 0.189** (0.084) | −0.113 (0.087) | 1793 |
| Experienced household physical violence | 0.252 *** (0.091) | 0.123 (0.081) | 0.392 *** (0.105) | 0.347 *** (0.097) |
| Experienced household emotional violence | 0.149 * (0.086) | 0.070 (0.063) | 0.225 ** (0.095) | 0.204 ** (0.094) |
| Experienced FGM/C | 0.147 ** (0.073) | 0.345 *** (0.087) | ||
| Experienced peer violence | 0.378 *** (0.089) | 0.439 *** (0.146) | 0.216 ** (0.102) | 0.233 ** (0.099) |
| =1 if Physical Health is Poor or Very Poor | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Panel A: Females | Panel B: Males | |||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Polyvictimized | 0.009 (0.015) | 0.010 (0.015) | 0.013 (0.014) | 0.016 (0.014) | 0.014 (0.014) | −0.023 (0.019) | −0.0157 (0.018) | −0.013 (0.018) | −0.013 (0.018) | −0.001 (0.020) |
| Sample size | 2215 | 2204 | 2204 | 2204 | 2204 | 2215 | 1789 | 1789 | 1789 | 1789 |
| =1 if Physical Health is Poor or Very Poor | ||||
|---|---|---|---|---|
| Panel A: Females | Panel B: Males | |||
| Unadjusted Coefficient | Adjusted Coefficient | Unadjusted Coefficient | Adjusted Coefficient | |
| Sexually victimized | −0.004 (0.025) | −0.005 (0.023) | 0.035 (0.038) | 0.037 (0.036) |
| Witnessed domestic violence | 0.022 (0.028) | 0.029 (0.027) | −0.013 (0.021) | −0.010 (0.021) |
| Experienced school violence | −0.013 (0.015) | 0.021 (0.015) | −0.008 (0.010) | −0.010 (0.012) |
| Experienced household physical violence | 0.028 (0.018) | 0.035 (0.018) | −0.007 (0.013) | 0.007 (0.012) |
| Experienced household emotional violence | −0.011 (0.018) | −0.012 (0.016) | 0.007 (0.013) | 0.011 (0.013) |
| Experienced FGM/C | −0.024 (0.015) | −0.016 (0.014) | ||
| Experienced peer violence | 0.082 *** (0.021) | 0.071 *** (0.020) | 0.045 *** (0.013) | 0.039 *** (0.013) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, L.; Butera, N.M.; Ellsberg, M.; Baird, S. Polyvictimization and Adolescent Health and Well-Being in Ethiopia: The Mediating Role of Resilience. Int. J. Environ. Res. Public Health 2023, 20, 6755. https://doi.org/10.3390/ijerph20186755
Miller L, Butera NM, Ellsberg M, Baird S. Polyvictimization and Adolescent Health and Well-Being in Ethiopia: The Mediating Role of Resilience. International Journal of Environmental Research and Public Health. 2023; 20(18):6755. https://doi.org/10.3390/ijerph20186755
Chicago/Turabian StyleMiller, Lior, Nicole M. Butera, Mary Ellsberg, and Sarah Baird. 2023. "Polyvictimization and Adolescent Health and Well-Being in Ethiopia: The Mediating Role of Resilience" International Journal of Environmental Research and Public Health 20, no. 18: 6755. https://doi.org/10.3390/ijerph20186755
APA StyleMiller, L., Butera, N. M., Ellsberg, M., & Baird, S. (2023). Polyvictimization and Adolescent Health and Well-Being in Ethiopia: The Mediating Role of Resilience. International Journal of Environmental Research and Public Health, 20(18), 6755. https://doi.org/10.3390/ijerph20186755





