Abstract
Cognitive insight refers to the ability to question one’s judgments and cognitive biases and is underpinned by specific metacognitive processes. The Beck Cognitive Insight Scale was developed to assess cognitive insight and includes two subscales, Self-Reflectiveness and Self-Certainty (SC). The present study aimed to investigate the underlying factor structure of the Italian version of the BCIS in patients with schizophrenia (SZ) and in the general population (GP) for the first time. A cross-sectional design was adopted and a GP sample of 624 subjects and an SZ sample of 130 patients were enrolled. In the SZ group, a two-factor solution was supported. The internal reliability of each factor was satisfactory. Two items were eliminated and one item moved from the SC to the SR subscale. In the GP group, a two-factor solution was highlighted. The internal reliability of each factor was satisfactory. However, four items of the SR subscale were deleted. The Italian-validated version of the BCIS shows different structures for the SZ and the GP and is characterized by different features concerning previous studies. This evidence suggests new interpretations of metacognitive processes in the two populations and implies specific therapeutic approaches.
1. Introduction
The concept of cognitive insight [1] was introduced concerning patients with schizophrenia and indicated the ability to monitor, question, and correct one’s erroneous convictions, distorted beliefs, and delusional thinking. In this perspective, cognitive insight is originally strictly related to the insight of illness.
To assess the construct of cognitive insight, Beck and colleagues [1] developed the Beck Cognitive Insight Scale (BCIS), which investigates two sub-dimensions, Self-Reflectiveness (SR) and Self-Certainty (SC). The former concerns the subject’s capacity to appraise cognitive biases, consider alternative explanations, and trust in external feedback; the latter concerns an overconfidence in the validity of one’s beliefs and the unwillingness to modify and correct one’s own opinions and interpretations.
Eventually, the construct of cognitive insight showed to be independent of, although representing a prerequisite of, insight into illness [2,3]. Nowadays, it concerns autonoetic consciousness or the capacity to mentally represent, and consequently become aware of, our continuous subjective life experience as related to specific memories [4,5]. Autonoetic consciousness is strictly underpinned by metacognitive function—that is, the knowledge and reflective capacities an individual has concerning their cognitive emotional and behavioral processes, or, more generally, the ability to think about thinking [6,7,8,9].
This broader interpretation of cognitive insight not only raised a remarkable interest and widespread use of the BCIS for clinical studies, but also showed its potential in the non-clinical general population (GP) [3,10,11,12].
Validation and Translations of the BCIS
The BCIS has been translated into several languages and administered in different cultural contexts, including European [13,14,15,16], Asian [17,18,19,20,21], and American [22,23] countries.
Furthermore, the BCIS has been validated in several different psychiatric conditions, such as schizophrenia, schizoaffective disorder, major depression with or without psychotic symptoms, bipolar disorder, anxiety disorders, and substance abuse [1,13,14,24,25,26], but also in non-psychiatric medical disorders [27,28]. Finally, an attempt to fix cut-off scores was carried out for clinical purposes [29].
The BCIS has also been widely administered to healthy subjects. So far, a similar factor structure of the BCIS in the GP and in psychiatric patients was found, and the two-factor structure has been confirmed in both populations [23,30].
Despite this, a discrete variability in reliability results, statistical procedures, and pragmatical considerations emerges in the literature [31]. A point deserving attention is a controversy about the appropriateness of some items, which in some cases led to the depletion of some statements in both the psychiatric population and the healthy subject validation procedures [13,32,33].
Orfei and colleagues [16] published an Italian translation of the scale, validated by both a back translation with an English mother-tongue expert in the field and an evaluation of the items by two judges regarding semantic congruence, content validity, and theoretical relevance. Assessment of interrater reliability for raters was in the excellent to good range for all the items, with intraclass correlations ranging from 0.80 to 0.93.
However, the psychometric properties of this version of the BCIS have yet to be tested. The main aim of this study was to investigate the underlying factor structure of the Italian version of the BCIS both in patients with schizophrenia (SZ) and in the GP.
2. Materials and Methods
2.1. Study Design and Setting
A cross-sectional design was adopted. All participants were provided with a detailed description of the experimental procedures and required consent before participating in the study. Participation was anonymous, voluntary, and not rewarded in any form. Each subject could fill out the questionnaire only once. The study was conducted in accordance with the Declaration of Helsinki and under research protocols approved by local Ethical Committees (Scuola Normale Superiore and Scuola Superiore Sant’Anna Joint Ethical Committee: Protocol No. 04/2021).
The General Population sample was recruited by two different modalities: partly by an online survey and partly by in-person recruitment. The online survey was carried out in the months of November and December 2021. The in-person recruitment of healthy volunteers was carried out at the Neuropsychiatry Lab of the IRCCS Santa Lucia Foundation from November 2021 to March 2022. The sample of patients with a diagnosis of schizophrenia was fully recruited from June 2021 to December 2022 at the Neuropsychiatry Lab of the IRCCS Santa Lucia Foundation (see below for further details).
2.2. Participants
2.2.1. General Population (GP)
For all the GP groups, the research participation was voluntary and the inclusion criteria were: (a) age greater than or equal to 18 years, (b) Italian mother tongue or high-level knowledge of the Italian language, (c) at least 8 years of education.
For the online survey, an initial sample of 2367 employees of a large Italian banking group was invited. The survey was anonymous, as each participant was assigned an alphanumeric code to ensure the confidentiality of information. Questionnaires were evenly distributed across the national territory. Given the online distribution, no anamnestic information about mental health was collected for these subjects.
Regarding the in-person recruitment, 150 healthy volunteers were recruited at the Neuropsychiatry Lab of the IRCCS Santa Lucia of Rome. These subjects were assessed by one senior clinical psychiatrist. For the in-person GP sample, for whom the collection of anamnestic data was possible, additional exclusion criteria were past or present major medical or neurological illnesses, psychiatric disorders, or mental retardation [34,35].
2.2.2. Patients with Schizophrenia (SZ)
One hundred and fifty consecutive SZ outpatients according to DSM-VI [34,35] were preliminarily recruited at the IRCCS S. Lucia of Rome. All patients were diagnosed by one senior clinical psychiatrist. Inclusion criteria were: (1) age between 18 and 65 years, (2) at least 8 years of education, (3) no dementia or cognitive deterioration according to the DSM V- criteria or Mini-Mental State Examination (MMSE) [36] scores lower than 24, which is consistent with normative data in the Italian population [37]. This criterion was selected to exclude patients with cognitive deterioration, which could represent a confounding variable in the interpretation of results. Exclusion criteria were: history of alcohol or drug dependence or traumatic head injury, any past or present major medical or neurological illness, any additional psychiatric disorder, mental retardation, or dementia.
The Positive and Negative Syndrome Scale (PANSS) [38] was administered by a senior clinical psychiatrist (G.S.) to rate the severity of psychopathological symptoms. PANSS ratings were obtained considering the last week’s period from the assessment.
Extrapyramidal side effects due to current treatment were assessed by the Simpson-Angus Rating Scale (SARS) [39], and the Abnormal Involuntary Movements Scale [40] was administered to assess the presence of tardive dyskinesias. No patient suffered from tardive dyskinesias.
All patients were receiving stable oral doses of one or more atypical antipsychotic drugs such as risperidone, quetiapine, and olanzapine. Antipsychotic dosages were converted to estimated equivalent dosages of olanzapine by use of a standard table [41]. All patients were in their phase of stable clinical compensation.
2.3. Beck Cognitive Insight Scale (BCIS)
The BCIS is a standardized, self-rated instrument composed of 15 items that rely on two sub-factors, SR and SC. SR expresses the willingness to acknowledge fallibility, self-appraise, and consider external feedback, while SC expresses firm confidence in one’s judgments and opinions. A subscale of nine items assesses SR (e.g., “If somebody points out that my beliefs are wrong, I am willing to consider it”), while a subscale of six items assesses SC (e.g., “I can trust my judgment at all times”). A third index, R-C, resulting from the SR score minus the SC score, reflects the balance between the two components.
2.4. Statistical Analyses
All analyses were performed using IBM SPSS v.27. Descriptive statistics were conducted on sociodemographic variables, with the chi-squared test for the nominal variable (gender) and independent sample t-test for the continuous variable (age). An independent sample t-test was also performed to compare SZ and GP on BCIS scores. The significance of these comparisons was set at p < 0.05.
The Cronbach’s alpha, the McDonald’s omega tests, and the inter-item correlation were performed to test questionnaire reliability. Keiser-Meyer-Olkin (KMO) and Bartlett’s sphericity tests were used to evaluate the adequacy and suitability of the samples (SZ and GP) before performing the factor analysis. A principal components analysis (PCA) was performed to extract factors with eigenvalues greater than or equal to 1.0. To clarify the interpretation, exploratory factor analyses (EFA) with orthogonal rotation (varimax) were performed; the acceptable factor loading index was set at ≥|0.40|.
3. Results
From the initial online panel, 487 subjects accepted to participate in the study and completed the online survey; from the initial sample who underwent the in-person psychiatric screening at the IRCCS Santa Lucia Foundation, three subjects were excluded because of a dementia diagnosis or an MMSE score lower than 27, four were excluded because they were diagnosed with comorbid substance use disorders (including the use of cannabis), five were excluded because of a major medical illness or a neuropsychiatric disorder, and one was excluded because of previous traumatic brain injury. Thus, 137 subjects were considered eligible. Summing up the two GP groups, the actual final GP sample was composed of 624 subjects.
About the SZ group, from the initial sample, 11 were excluded because they were diagnosed with comorbid substance use disorders, 5 were excluded because they were cognitively deteriorated, 3 were excluded because of comorbid medical or neurological illness, and 1 was excluded because of previous traumatic brain injury. Thus, 130 consecutive outpatients were included in the final SZ sample.
The size of both samples is adequate to support EFA results [42,43,44].
Descriptive statistics of sociodemographic variables (age and gender), BCIS indexes, and clinical data (PANSS scores and illness duration) are shown in Table 1.

Table 1.
Descriptive statistics of socio-demographic variables, BCIS indexes, and clinical data.
3.1. Reliability of the BCIS in the SZ and the GP Groups
The Italian translation of the BCIS, in its original formulation, showed slightly acceptable internal consistency in SZ, both in the SR (Cronbach’s alpha = 0.583, McDonald’s omega = 0.587) and SC subscales (Cronbach’s alpha = 0.608, McDonald’s omega = 0.616). In the GP group, slightly acceptable reliability values were found for SR (Cronbach’s alpha = 0.564, McDonald’s omega = 0.566) and SC (Cronbach’s alpha = 0.628, McDonald’s omega = 0.630) (Table S1). Furthermore, no threshold inter-item correlations (≥0.800) were found in SZ and GP (Tables S2 and S3).
3.2. PCA and EFA in the SZ Group
The KMO (0.609) and Bartlett’s sphericity test results (χ2 = 268.656 p = 0.000) showed that the data were suitable for factor analysis. The PCA showed six eigenvalues greater than or equal to 1.0, accounting for 62% of the total variance explained (Figure 1).
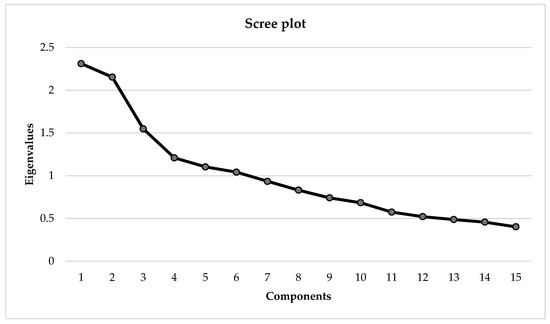
Figure 1.
PCA Scree plot with eigenvalues greater than or equal to 1.0 in the SZ group. PCA = Principal components analysis; SZ = Patients with schizophrenia.
To explore the factorial structure of the BCIS, all 15 items of the instrument were subjected to EFA with orthogonal rotation (varimax).
The first solution according to the scree plot showed 12 items and six factors, where two factors (4 and 6) were composed of 1 item only. The internal consistency was calculated for factors with several items greater than or equal to 2: factor 1 (2 items; Cronbach’s alpha = 0.521, McDonald’s omega = 0.521), factor 2 (3 items; Cronbach’s alpha = 0.534, McDonald’s omega = 0.570), factor 3 (3 items, Cronbach’s alpha = 0.500, McDonald’s omega = 0.511), and factor 5 (2 items; Cronbach’s alpha = 0.470, McDonald’s omega = 0.470) (Table S4). Due to this questionable factor solution, the EFAs with four, three, and two forced factors were conducted (Tables S5–S7, Figure S1).
The four forced factors solution showed 12 items and the following internal consistency indexes for each factor: factor 1 (3 items; Cronbach’s alpha = 0.573, McDonald’s omega = 0.534), factor 2 (4 items; Cronbach’s alpha = 0.521, McDonald’s omega = 0.506), factor 3 (3 items; Cronbach’s alpha = 0.455, McDonald’s omega = 0.444), and factor 4 (2 items; Cronbach’s alpha = 0.000, McDonald’s omega = −0.373).
Then EFA with three forced factors solution was performed reporting 13 items distributed in three factors with the following internal consistency indexes: factor 1 (5 items; Cronbach’s alpha = 0.624, McDonald’s omega = 0.618), factor 2 (4 items; Cronbach’s alpha = 0.521, McDonald’s omega = 0.506), and factor 3 (4 items; Cronbach’s alpha = 0.509, McDonald’s omega = 0.487).
Lastly, the EFA with two forced factors showed 13 items and the following reliability indexes: factor 1 (8 items; Cronbach’s alpha = 0.610, McDonald’s omega = 0.607) and factor 2 (5 items; Cronbach’s alpha = 0.624, McDonald’s omega = 0.618) (Table S7). The two factors were respectively renamed: Self-unreliability, i.e., the metacognitive belief of poor trust in the self; Self-certainty, consisting of part of the same items of the SC subscale of Beck’s original version (Figure 2).
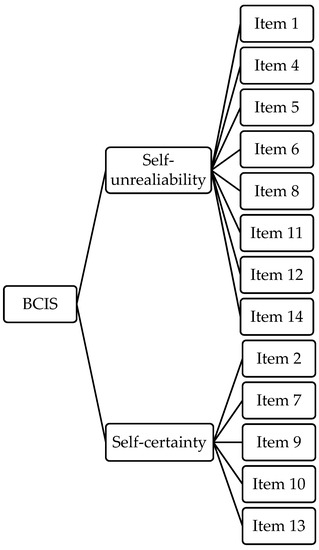
Figure 2.
The path diagram of the two-factor model of the BCIS in SZ. Survivor item distribution after the EFA in the SZ group. BCIS = Beck Cognitive Insight Scale; SZ = Patients with schizophrenia.
3.3. PCA and EFA in the GP Group
The KMO (0.717) and Bartlett’s sphericity test results (χ2 = 1331.186 p = 0.000) showed the adequacy of the GP sample. The PCA showed four eigenvalues greater than or equal to 1.0, accounting for 50% of the total variance explained (Figure 3).
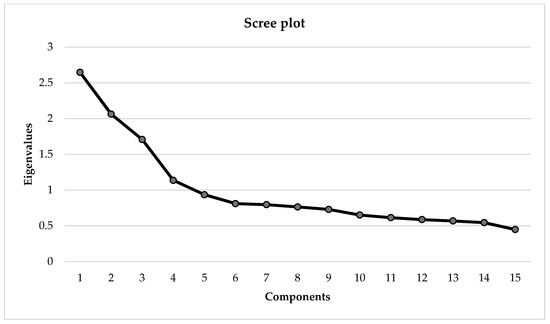
Figure 3.
PCA Scree plot with eigenvalues greater than or equal to 1.0 in the GP group. PCA = Principal components analysis; GP = General population.
To explore the factorial structure of the BCIS in the GP sample, all 15 items of the instrument were subjected to EFA with orthogonal rotation (varimax).
The first solution according to the scree plot showed 14 items and four factors, whereas the fourth factor was composed of only one item. The internal consistency was calculated for factors with several items greater than or equal to 2: factor 1 (5 items; Cronbach’s alpha = 0.500, McDonald’s omega = 0.414), factor 2 (5 items; Cronbach’s alpha = 0.641, McDonald’s omega = 0.636), and factor 3 (3 items, Cronbach’s alpha = 0.526, McDonald’s omega = 0.511) (Table S8). Given this questionable factor structure, an EFA with three and two forced factors was performed (Tables S9 and S10, Figure S2).
The three forced factors solution showed 14 items and the following factors internal consistency: factor 1 (5 items; Cronbach’s alpha = 0.666, McDonald’s omega = 0.667), factor 2 (6 items; Cronbach’s alpha = 0.630, McDonald’s omega = 0.628), and factor 3 (3 items; Cronbach’s alpha = 0.526, McDonald’s omega = 0.511).
The EFA with two forced factors obtained 10 items and the reliability of the following factors: factor 1 (5 items; Cronbach’s alpha = 0.666, McDonald’s omega = 0.667) and factor 2 (5 items; Cronbach’s alpha = 0.641, McDonald’s omega = 0.636). Factors 1 and 2 were respectively named: Self-doubt, i.e., a critical inspection of own beliefs; Self-certainty, overlapping the SC subscale of Beck’s original version (Figure 4).
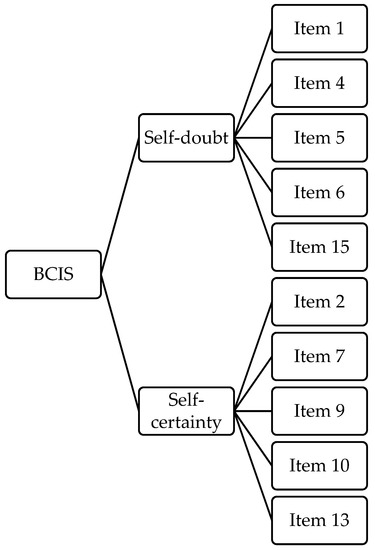
Figure 4.
The path diagram of the two-factor model of the BCIS in GP. Survivor item distribution after the EFA in the General Population. BCIS = Beck Cognitive Insight Scale; GP = General population.
4. Discussion
The main aim of the study was to examine the underlying factor structure of the Italian version of the BCIS both in SZ patients and the GP. We obtained two main results: (a) in the SZ group, the analyses supported the efficiency of a two-factor model, which was similar—although not fully comparable—to Beck’s original structure of the scale; and (b) in the GP group, a two-factor model best fitted the data, although it implied a remarkably different structure concerning Beck’s original version.
4.1. Results in the SZ Group
In the SZ group, the two-factor solution turned out to be the best fitting for the data because it was supported by an acceptable internal reliability level, and the data were consistent with previous evidence.
Despite the exclusion of two items from the SR subscale, our two-factor model mostly resembled the original Beck description of the questionnaire. To note, the EFA showed that the first factor included seven original SR items along with an item drawn from the SC subscale (“I cannot trust other people’s opinion about my experiences”). This statement originally aimed to elicit an attitude of mistrust in other people. This apparent incongruence might cast light on the peculiar metacognitive process explored by the SR subscale in our model. In fact, in SZ patients, it might mirror a deep feeling of unreliability of one’s judgment, to the extent that even one’s understanding of other peoples’ opinions is doubtful. Thus, in SZ patients, high scores on this factor would indicate a radical mistrust in one’s judgment ability, rather than a healthy openness to external feedback. In this perspective, this dimension would be better renamed as “Self-Unreliability”. This would be consistent with several previous studies that highlighted that in psychotic patients, SR may be healthy to a point, after which high levels may be associated with depressive thinking and self-stigma [45,46,47,48,49] and even jeopardize the quality of life [46,50,51].
Indeed, our study not only provided results partially different from previous evidence in terms of internal reliability [31] and data interpretation, it also showed that the reliability values—as defined by Cronbach’s alpha or McDonald’s omega—were not very high, although they were still fairly acceptable. However, we would like to bring attention to some data. Regarding the SZ sample, the alpha values of our final 2-factor structure were 0.610 and 0.624, respectively. Indeed, previous studies showed a fair variability in results, and any case obtained not much higher values. Beck and colleagues [1] reported an alpha of 0.68 for SR and 0.60 for SC; Favrod [14] described a French translation with an alpha of 0.73 (SR) and 0.62 (SC); Greenberger [2] obtained an SR characterized by alpha = 0.61 and 0.84, respectively. Among confirmatory analyses, Saguem [19] provided reliability scores of 0.60 for Sr and 0.53 for SC, and Pedrelli [25] of 0.70 and 0.55, respectively. This difference in results is attributable to the features of the samples recruited, namely psychiatric diagnosis and duration of illness. Most of the studies enrolled psychiatric patients with different diagnoses, ranging from schizophrenia to schizoaffective, bipolar, and major depressive disorders, with or without psychotic features, and even not otherwise specified psychotic features [1,13,14,17,47]. Conversely, we selected a sample that was highly homogeneous in terms of diagnosis, clinical picture, and medical treatment in order to not to blur results. Interestingly, Gutierrez and colleagues [15], different from the aforementioned studies and similar to ours, included only patients with a diagnosis of schizophrenia and reported alpha values of 0.59 for SR and 0.62 for SC and had to delete three items from the original version; thus, they showed evidence consistent with our results.
Finally, our two-factor structure required the depletion of two items, which was a not entirely new solution. Some items of the original Beck’s version have been previously debated. For instance, Pedrelli and colleagues [25], in their study on patients with schizophrenia and schizoaffective disorder, slightly modified the phrasing of an item from the original version, which referred to “unusual experiences” as “unpleasant experiences”. The suitability of the original version of this item for the GP is also questioned by Martin and colleagues [32]. Furthermore, in Pedrelli’s study, although item 14 is lower than the cutoff loading of 0.30 used for determining whether an item contributed significantly to a specific factor, it was nonetheless saved.
4.2. Results in the GP Group
In the GP group, the forced two-factor solution was characterized by the good internal reliability level of each factor. However, this higher consistency was obtained by the elimination of five SR items, which significantly altered the original structure of the scale. Notably, most of the SR factors deleted by the EFA concerned external feedback. We might speculate that the cognitive insight in the GP is underpinned by a metacognitive process that is drastically different from that of the SZ. In fact, in SZ patients, external feedback, up to a certain point, can represent a benchmark due to the untrustworthiness of one’s judgment function. Conversely, GP self-reflection would mostly pertain to a critical attitude toward one’s judgment biases, similar to the metacognitive construct of private self-consciousness or the inspection and evaluation of our thinking and feelings [51,52]. Different neuropsychological correlations of SR in the SZ and the GP highlighted in previous studies [17,53,54,55] would support this different role of self-reflection in the two populations.
This is the first validation study pointing out this structure of the SR in the GP. The few previous studies suggested a depletion of items, and were merely focused on the sentences implicitly concerning psychotic experiences [13,25,32], which was deemed inappropriate for healthy subjects. Engh [13] raised doubts about the suitability of items 3, 5, 6, and 15 because in his control group, they were left out to a large degree, possibly because referring to psychotic experiences was difficult to answer for this group. Thus, he concluded that in the case of comparison between controls and other clinical samples, the four items referring to psychotic experiences should not be used. Uchida [20] decided to keep item 15, although it did not reach the loading threshold, in order to guarantee consistency with Beck’s original results. One of the most different interpretations of the BCIS, when applied to healthy subjects, is described by Kao and colleagues [17]. The authors’ factorial analysis pointed out that two items originally of the SC subscale (items 10 and 11) were now included in the SR subscale, and that two items originally about the SR subscale were now better loaded on the SC subscale. Moreover, the factorial structure is quite different from Beck’s description, to the extent that the authors suggest renaming SR and SC as “reflective attitude” and “certain attitude”, respectively. Thus, although their principal components analysis supported a two-factor solution, the pattern of intercorrelation suggested that cognitive insight comprises two or even more related yet partially independent components.
Our evidence can be traced back to the characteristics of the samples enrolled because our GP group was, on average, older and better balanced for gender than in other studies [23,32]. In particular, older subjects can benefit from greater self-experience and consequently be more aware of one’s judgment biases; thus, they are less concerned with external feedback. This is not to say that the different statistical approaches adopted may play a role, as some authors performed a confirmatory factor analysis rather than a validation procedure [32].
As for the SZ group, for the GP group, we also obtained reliability indices that are of moderate magnitude at first glance. Our final two-factor structure was characterized by alpha scores of 0.666 for the first factor (renamed as Self-doubt) and 0.641 for the second factor (SC). As debated for the SZ group, our values are not very unlike those reported in previous studies. Warman [30] showed that, in a population of undergraduate students, the alpha values of the BCIS were 0.62 for SR and 0.61 for SC. Engh [13], in a much smaller sample of subjects that were supposed to not have psychiatric disorders, described the Norwegian translation of the BCIS as characterized by 0.73 (SR) and 0.63 (SC). A wider healthy sample was enrolled by Buchy and colleagues [23] to validate the BCIS in the Canadian community, and alpha scores of 0.68 for SR and 0.65 for SC emerged. Other studies reported higher reliability indices. Among others, Kao and colleagues first reported Cronbach’s values of 0.70 (SR) and 0.69 (SC) [17] and later of 0.75 and 0.78, respectively. Also, Martin [32] highlighted alpha values of 0.74 for SR and 0.75 for SC in a sample of undergraduate students. However, we cannot help but note that most of the previous studies are underpinned by very young subjects, and by samples frequently unbalanced for gender. This evidence allows us to suppose that our data are fairly consistent with the literature and underpinned by a reliable sampling approach.
4.3. Limitations
Some limitations must be considered when interpreting the results of the present study. First, our main concern is selection bias. As the majority of our GP group was constituted by employees of a single Italian banking group, the results may not represent the general Italian population. Moreover, the difference between the figures of the online panel and those of the actual sample may seem impressive at first glance. To note, those who have accepted our invitation to participate in the study as volunteers may be more sensitive toward psychological issues. However, some points have to be considered. The participation was completely voluntary and anonymous. Consequently, no data are available about the characteristics of the panel invited and much less about those of the subjects who rejected to get involved in the online survey. To address these potential sources of bias, we also included an additional GP group external from the bank to increase the representativeness of results and to cautiously speculate about the possibility of extending our results to wider segments of the Italian population.
Second, the premorbid cognitive and psychiatric status was not documented for the online-recruited GP subsample; thus, we cannot exclude the presence of psychological discomfort symptoms. This is why we opted for the “GP” denomination of the group, rather than “healthy participants”. However, the inclusion of volunteers who underwent a psychiatric screening in the GP group, which excluded any present or past psychiatric issues, is expected to counterbalance the missing information on the other part of the sample.
Third, on one side, the strict inclusion criteria defined for the SZ group ensured the validity of our results; on the other side, it limited their generalizability to other psychotic disorders. Future studies would cast light on this point, enrolling patients with different diagnoses.
Fourth, our study aimed to specifically explore the underlying factor structure of the Italian version of the BCIS, but did not include the investigation of additional psychometric properties, such as test–retest stability and discriminant validity. Further studies to deepen these psychometric properties are required to provide a fully exhaustive perspective on the issue.
5. Conclusions
The BCIS is an efficient tool to assess general metacognitive processes underpinning autonoetic consciousness in diverse psychiatric disorders as well as non-clinical subjects [17].
The results presented here provide a benchmark for cognitive insight in Italian GP and SZ patients, allowing us to speculate on different metacognitive processes. Notably, treatments for patients with psychosis, and in particular the Metacognitive Training [56], frequently aim to improve cognitive insight because this seems to affect overall treatment outcomes and recovery [10,57]. The dimension that we named Self-Unreliability may orient the therapeutic approach for SZ patients to improve insight into illness, supporting patients to consider external feedback as sources of information to integrate into one’s cognitive schemata, consequently reinforcing confidence in managing information and evidence. On the other hand, in the GP, the management of autonoetic knowledge highlighted in our study may suggest a psychotherapeutic approach toward encouraging to take external feedback into greater consideration, as well as a realistic self-evaluation.
Nonetheless, the evidence highlighted in our study poses a pragmatic problem for research. We may wonder whether two different forms of the same questionnaire can be administered in a unique study to assess the same construct in GP and SZ patients. In particular, the depletion of some items from the original form of the scale cannot be disregarded. We may wonder what factors led to this evidence. It might be traced back to the translation into the Italian language, but we are not inclined to consider this hypothesis because the translation process was supported by good results. Notably, we recommend to not interpret the evidence that emerged from our study as questioning the purposefulness of the BCIS per se. Rather, the partly controversial debate of the underlying factor structure of the scale, with the contribution of our additional data, would require further deepening and clarification in future studies. In waiting for further definitive evidence, we suggest administering the classical form of the BCIS.
Interestingly, our study points out that the most unstable dimension of cognitive insight is SR. This is possibly due to the multifactorial nature of this construct.
Different from SR, we confirm the consistency of the SC dimension across different studies, samples, cultural contexts, and statistical approaches, which consequently seems to investigate a more stable construct than SR.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20176634/s1, Table S1: Internal consistency of BCIS in the GP and SZ groups; Table S2: Inter-item correlation of the BCIS in the SZ group; Table S3: Inter-item correlation of the BCIS in the GP group; Table S4: EFA with orthogonal rotation (varimax) of 6 factors solution and internal consistency of 6 factors solution in the SZ group; Table S5: EFA with orthogonal rotation (varimax) and internal consistency of 4 factors solutions in SZ; Table S6: EFA with orthogonal rotation (varimax) and internal consistency of the 3 factors solution in SZ; Table S7: EFA with orthogonal rotation (varimax) and internal consistency of 2 factors solution in SZ; Table S8: EFA with orthogonal rotation (varimax) and internal consistency of 4 factors solutions in GP; Table S9: EFA with orthogonal rotation (varimax) and internal consistency of 3 factors solutions in GP; Table S10: EFA with orthogonal rotation (varimax) and internal consistency of 2 factors solutions in GP; Figure S1: EFAs path diagram of BCIS in SZ; Figure S2: EFAs path diagram of BCIS in GP.
Author Contributions
Conceptualization, M.D.O. and D.E.P.; methodology, M.D.O. and D.E.P.; validation, M.D.O.; formal analysis, D.E.P.; investigation, M.D.O. and D.E.P.; resources, E.R., F.A., N.B., F.P. and G.S.; data curation, M.D.O., D.E.P., F.A. and N.B.; writing—original draft preparation, M.D.O. and D.E.P.; writing—review and editing, M.D.O., E.R., F.A., N.B., F.P. and G.S.; visualization, M.D.O. and D.E.P.; supervision, E.R.; project administration, E.R.; funding acquisition, E.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Intesa Sanpaolo Innovation Center S.p.A. and by the DM n. 289/2021—Programmazione Triennale (PRO3) project: ‘Neurocognitive, sensory-motor, and emotional outcomes following the pandemic in populations at risk’. The research was conducted under a cooperative agreement between IMT School for Advanced Studies Lucca, Intesa Sanpaolo Innovation Center S.p.A., and Intesa Sanpaolo S.p.A. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Institutional Review Board Statement
The study was conducted following the Declaration of Helsinki and under research protocols approved by local Ethical Committees (Scuola Normale Superiore and Scuola Superiore Sant’Anna Joint Ethical Committee: Protocol n. 04/2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We sincerely thank Dario Russignaga of Intesa Sanpaolo Group and Francesca Maggi and Sonia D’Arcangelo of Intesa Sanpaolo Innovation Centre Spa (society of Intesa Sanpaolo) for the fundamental organizational support and operative contribution.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Beck, A.; Baruch, E.; Balter, J.M.; Steer, R.A.; Warman, D.M. A new instrument for measuring insight: The Beck Cognitive Insight Scale. Schizophr. Res. 2004, 68, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Greenberger, C.; Serper, M.R. Examination of Clinical and Cognitive Insight in Acute Schizophrenia Patients. J. Nerv. Ment. Dis. 2010, 198, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Tranulis, C.; Lepage, M.; Malla, A. Insight in first episode psychosis: Who is measuring what? Early Interv. Psychiatry 2008, 2, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Vandekerckhove, M.; Bulnes, L.C.; Panksepp, J. The Emergence of Primary Anoetic Consciousness in Episodic Memory. Front. Behav. Neurosci. 2014, 7, 210. [Google Scholar] [CrossRef]
- Wheeler, M.A.; Stuss, D.T.; Tulving, E. Toward a theory of episodic memory: The frontal lobes and autonoetic consciousness. Psychol. Bull. 1997, 121, 331–354. [Google Scholar] [CrossRef]
- Flavell, J.H. Metacognition and cognitive monitoring: A new area of cognitive–developmental inquiry. Am. Psychol. 1979, 34, 906–911. [Google Scholar] [CrossRef]
- Newen, A.; Vogeley, K. Self-representation: Searching for a neural signature of self-consciousness. Conscious Cogn. 2003, 12, 529–543. [Google Scholar] [CrossRef]
- Wells, A.; Purdon, C. Metacognition and cognitive-behaviour therapy: A special issue. Clin. Psychol. Psychother. 1999, 6, 71–72. [Google Scholar] [CrossRef]
- Zeman, A. What do we mean by “conscious” and “aware”? Neuropsychol. Rehabil. 2006, 16, 356–376. [Google Scholar] [CrossRef]
- Birulés, I.; López-Carrilero, R.; Cuadras, D.; Pousa, E.; Barrigón, M.; Barajas, A.; Lorente-Rovira, E.; González-Higueras, F.; Grasa, E.; Ruiz-Delgado, I.; et al. Cognitive Insight in First-Episode Psychosis: Changes during Metacognitive Training. J. Pers. Med. 2020, 10, 253. [Google Scholar] [CrossRef]
- Capdevielle, D.; Norton, J.; Aouizerate, B.; Berna, F.; Chereau, I.; D’Amato, T.; Dubertret, C.; Dubreucq, J.; Fond, G.; C, L.; et al. Comparison of three scales (BIS, SUMD and BCIS) for measuring insight dimensions and their evolution after one-year of follow-up: Findings from the FACE-SZ Cohort. Psychiatry Res. 2021, 303, 114044. [Google Scholar] [CrossRef] [PubMed]
- Tastet, H.; Verdoux, H.; Bergua, V.; Destaillats, J.M.; Prouteau, A. Cognitive Insight in Schizophrenia: The Missing Link between Insight and Neurocognitive Complaint? J. Nerv. Ment. Dis. 2012, 200, 908–910. [Google Scholar] [CrossRef] [PubMed]
- Engh, J.A.; Friis, S.; Birkenaes, A.B.; Jónsdóttir, H.; Ringen, P.A.; Ruud, T.; Sundet, K.S.; Opjordsmoen, S.; Andreassen, O.A. Measuring cognitive insight in schizophrenia and bipolar disorder: A comparative study. BMC Psychiatry 2007, 7, 71. [Google Scholar] [CrossRef]
- Favrod, J.; Zimmermann, G.; Raffard, S.; Pomini, V.; Khazaal, Y. The Beck Cognitive Insight Scale in Outpatients with Psychotic Disorders: Further Evidence from a French-Speaking Sample. Can. J. Psychiatry 2008, 53, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Zotes, J.A.; Valero, J.; Cortés, M.J.; Labad, A.; Ochoa, S.; Ahuir, M.; Carlson, J.; Bernardo, M.; Cañizares, S.; Escartin, G.; et al. Spanish adaptation of the Beck Cognitive Insight Scale (BCIS) for schizophrenia. Actas Esp. Psiquiatr. 2012, 40, 2–9. [Google Scholar] [PubMed]
- Orfei, M.D.; Caltagirone, C.; Spalletta, G. I Disturbi Della Consapevolezza Nelle Malattie Neuropsichiatriche; Metodologie Riabilitative in Logopedia; Springer: Milan, Italy, 2007. [Google Scholar]
- Kao, Y.C.; Liu, Y.P. The Beck Cognitive Insight Scale (BCIS): Translation and validation of the Taiwanese version. BMC Psychiatry 2010, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Othman, Z. Validation of Malay Beck Cognitive Insight Scale (BCIS). 1 August 2017. Available online: https://zenodo.org/record/2588052 (accessed on 16 November 2022).
- Saguem, B.N.; Braham, A.; Ines, M.K.; Mtiraoui, A.; Nakhli, J.; Nasr, S.B. Validation of Beck Cognitive Insight Scale—Arabic version in a Tunisian sample. L’Encéphale 2023, 49, 234–240. [Google Scholar] [CrossRef]
- Uchida, T.; Matsumoto, K.; Kikuchi, A.; Miyakoshi, T.; Ito, F.; Ueno, T.; Matsuoka, H. Psychometric properties of the Japanese version of the Beck Cognitive Insight Scale: Relation of cognitive insight to clinical insight: Cognitive insight in schizophrenia. Psychiatry Clin. Neurosci. 2009, 63, 291–297. [Google Scholar] [CrossRef]
- Wong, A.W.S.; Chen, E.Y.H. Psychometric properties of translated outcome measures of cognitive behavioural therapy for psychosis in the Chinese context. Asian J. Psychiatry 2015, 13, 62–65. [Google Scholar] [CrossRef]
- Alvarenga, M.A.S.; Hastenreiter, F.; Salgado, J.V.; Rego, M.F.G.; Pereira, K.I.R.; Guilhermino, C.S.; Azevedo, T.G.; de Portela, D.D.N. Evidências de Validade de Conteúdo da Beck Cognitive Insight Scale, Versão Brasileira (BCIS-BR). Estud. Pesqui. Psicol. 2022, 22, 872–895. [Google Scholar] [CrossRef]
- Buchy, L.; Brodeur, M.B.; Lepage, M. The Beck Cognitive Insight Scale: Psychometric properties in a Canadian community sample. Schizophr. Res. 2012, 137, 254–255. [Google Scholar] [CrossRef] [PubMed]
- Fatahi, F.; Ramezani Farani, A. Cognitive Insight as the Differentiating Feature of Psychosis and Anxiety. Pract. Clin. Psychol. 2021, 9, 103–110. [Google Scholar] [CrossRef]
- Pedrelli, P.; McQuaid, J.R.; Granholm, E.; Patterson, T.L.; McClure, F.; Beck, A.T.; Jeste, D.V. Measuring cognitive insight in middle-aged and older patients with psychotic disorders. Schizophr. Res. 2004, 71, 297–305. [Google Scholar] [CrossRef]
- Raftery, D.; Kelly, P.J.; Deane, F.P.; Mcketin, R.; Baker, A.L.; Turner, A.; Dean, O.M. Measuring cognitive insight in people with problematic substance use: An exploration of the factor validity of the Beck Cognitive Insight Scale. Drug Alcohol. Rev. 2019, 38, 622–629. [Google Scholar] [CrossRef]
- Degirmenci, E.; Degirmenci, T.; Dügüncü, Y.; Yılmaz, G. Cognitive Insight in Alzheimer’s Disease. Am. J. Alzheimers Dis. Dementiasr. 2013, 28, 263–268. [Google Scholar] [CrossRef]
- Innamorati, M.; Chetta, A.; Antonucci, C.; Bettini, E.; Aiello, M.; Montali, A.; Parisoli, C.; Murri, M.B.; Brugnoli, R.; Pisi, R.; et al. Alexithymia and self-reflectiveness in bronchial asthma. Riv. Psichiatr. 2015, 50, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Penney, D.; Sauvé, G.; Joober, R.; Malla, A.K.; Lepage, M. Establishing Clinical Cutoff Values for the Beck Cognitive Insight Scale. Cogn. Ther. Res. 2019, 43, 324–334. [Google Scholar] [CrossRef]
- Warman, D.B.; Dunahue, S.; Martin, J.M.; Beck, A.T. An Investigation of the Beck Cognitive Insight Scale in the General Population; Poster presentation: New Orleans, LA, USA, 2004. [Google Scholar]
- Riggs, S.E.; Grant, P.M.; Perivoliotis, D.; Beck, A.T. Assessment of Cognitive Insight: A Qualitative Review. Schizophr. Bull. 2012, 38, 338–350. [Google Scholar] [CrossRef]
- Martin, J.M.; Warman, D.M.; Lysaker, P.H. Cognitive insight in non-psychiatric individuals and individuals with psychosis: An examination using the Beck Cognitive Insight Scale. Schizophr. Res. 2010, 121, 39–45. [Google Scholar] [CrossRef]
- Warman, D.M.; Martin, J.M. Cognitive insight and delusion proneness: An investigation using the Beck Cognitive Insight Scale. Schizophr. Res. 2006, 84, 297–304. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-5: Manuale Diagnostico e Statistico dei Disturbi Mentali, 5th ed.; R. Cortina: Milan, Italy, 2014. [Google Scholar]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; 947p. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Measso, G.; Cavarzeran, F.; Zappalà, G.; Lebowitz, B.D.; Crook, T.H.; Pirozzolo, F.J.; Amaducci, L.A.; Massari, D.; Grigoletto, F. The mini-mental state examination: Normative study of an Italian random sample. Dev. Neuropsychol. 1993, 9, 77–85. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The Positive and Negative Syndrome Scale (PANSS) for Schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.M.; Angus, J.W. A Rating Scale for Extrapyramidal Side Effects. Acta Psychiatr. Scand. 1970, 45, 11–19. [Google Scholar] [CrossRef]
- Kane, J.M.; Correll, C.U.; Nierenberg, A.A.; Caroff, S.N.; Sajatovic, M.; on behalf of the Tardive Dyskinesia Assessment Working Group. Revisiting the Abnormal Involuntary Movement Scale: Proceedings from the Tardive Dyskinesia Assessment Workshop. J. Clin. Psychiatry 2018, 79, 17cs11959. Available online: http://www.psychiatrist.com/JCP/article/Pages/2018/v79n03/17cs11959.aspx (accessed on 30 November 2022). [CrossRef]
- Oquendo, M.A.; Baca-Garcia, E.; Kartachov, A.; Khait, V.; Campbell, C.E.; Richards, M.; Sackeim, H.A.; Prudic, J.; Mann, J.J. A Computer Algorithm for Calculating the Adequacy of Antidepressant Treatment in Unipolar and Bipolar Depression. J. Clin. Psychiatry 2003, 64, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Geweke, J.F.; Singleton, K.J. Interpreting the Likelihood Ratio Statistic in Factor Models When Sample Size is Small. J. Am. Stat. Assoc. 1980, 75, 133–137. [Google Scholar] [CrossRef]
- Bearden, W.O.; Sharma, S.; Teel, J.E. Sample Size Effects on Chi Square and Other Statistics Used in Evaluating Causal Models. J. Mark. Res. 1982, 19, 425. [Google Scholar] [CrossRef]
- De Winter, J.C.F.; Dodou, D.; Wieringa, P.A. Exploratory Factor Analysis with Small Sample Sizes. Multivar. Behav. Res. 2009, 44, 147–181. [Google Scholar] [CrossRef]
- Ekinci, O.; Ugurlu, G.K.; Albayrak, Y.; Arslan, M.; Caykoylu, A. The relationship between cognitive insight, clinical insight, and depression in patients with schizophrenia. Compr. Psychiatry 2012, 53, 195–200. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, S.; Han, A.Y.; Kim, K.; Lee, J. Relationship between cognitive insight and subjective quality of life in outpatients with schizophrenia. Neuropsychiatr. Dis. Treat. 2015, ume 11, 2041–2048. [Google Scholar] [CrossRef]
- Mak, W.W.S.; Wu, C.F.M. Cognitive Insight and Causal Attribution in the Development of Self-Stigma among Individuals with Schizophrenia. Psychiatr. Serv. 2006, 57, 1800–1802. [Google Scholar] [CrossRef]
- Misdrahi, D.; Denard, S.; Swendsen, J.; Jaussent, I.; Courtet, P. Depression in schizophrenia: The influence of the different dimensions of insight. Psychiatry Res. 2014, 216, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Warman, D.; Lysaker, P.; Martin, J. Cognitive insight and psychotic disorder: The impact of active delusions. Schizophr. Res. 2007, 90, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Phalen, P.L.; Viswanadhan, K.; Lysaker, P.H.; Warman, D.M. The relationship between cognitive insight and quality of life in schizophrenia spectrum disorders: Symptom severity as potential moderator. Psychiatry Res. 2015, 230, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Van Camp, L.S.C.; Sabbe, B.G.C.; Oldenburg, J.F.E. Cognitive insight: A systematic review. Clin. Psychol. Rev. 2017, 55, 12–24. [Google Scholar] [CrossRef]
- Grant, A.M.; Franklin, J.; Langford, P. The Self-Reflection and Insight Scale: A New Measure of Private Self-Consciousness. Soc. Behav. Pers. Int. J. 2002, 30, 821–835. [Google Scholar] [CrossRef]
- Lepage, M.; Buchy, L.; Bodnar, M.; Bertrand, M.C.; Joober, R.; Malla, A. Cognitive insight and verbal memory in first episode of psychosis. Eur. Psychiatry 2008, 23, 368–374. [Google Scholar] [CrossRef]
- Orfei, M.D.; Spoletini, I.; Banfi, G.; Caltagirone, C.; Spalletta, G. Neuropsychological correlates of cognitive insight in schizophrenia. Psychiatry Res. 2010, 178, 51–56. [Google Scholar] [CrossRef]
- Orfei, M.D.; Caltagirone, C.; Cacciari, C.; Assogna, F.; Spalletta, G. The neuropsychological correlates of cognitive insight in healthy participants. Appl. Cogn. Psychol. 2011, 25, 927–932. [Google Scholar] [CrossRef]
- Aghotor, J.; Pfueller, U.; Moritz, S.; Weisbrod, M.; Roesch-Ely, D. Metacognitive training for patients with schizophrenia (MCT): Feasibility and preliminary evidence for its efficacy. J. Behav. Ther. Exp. Psychiatry 2010, 41, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Penzenstadler, L.; Chatton, A.; Lecomte, T.; Huguelet, P.; Lecardeur, L.; Azoulay, S.; Bartolomei, J.; Brazo, P.; Murys, E.; Poupart, F.; et al. Does the Beck Cognitive Insight Scale predict change in delusional beliefs? Psychol. Psychother. Theory Res. Pract. 2020, 93, 690–704. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).