Associations among Food Systems, Food Environments, Food Choices, Food Security, and Nutrition Transition in Limpopo Province, South Africa: A Cross-Sectional Study
Abstract
1. Introduction
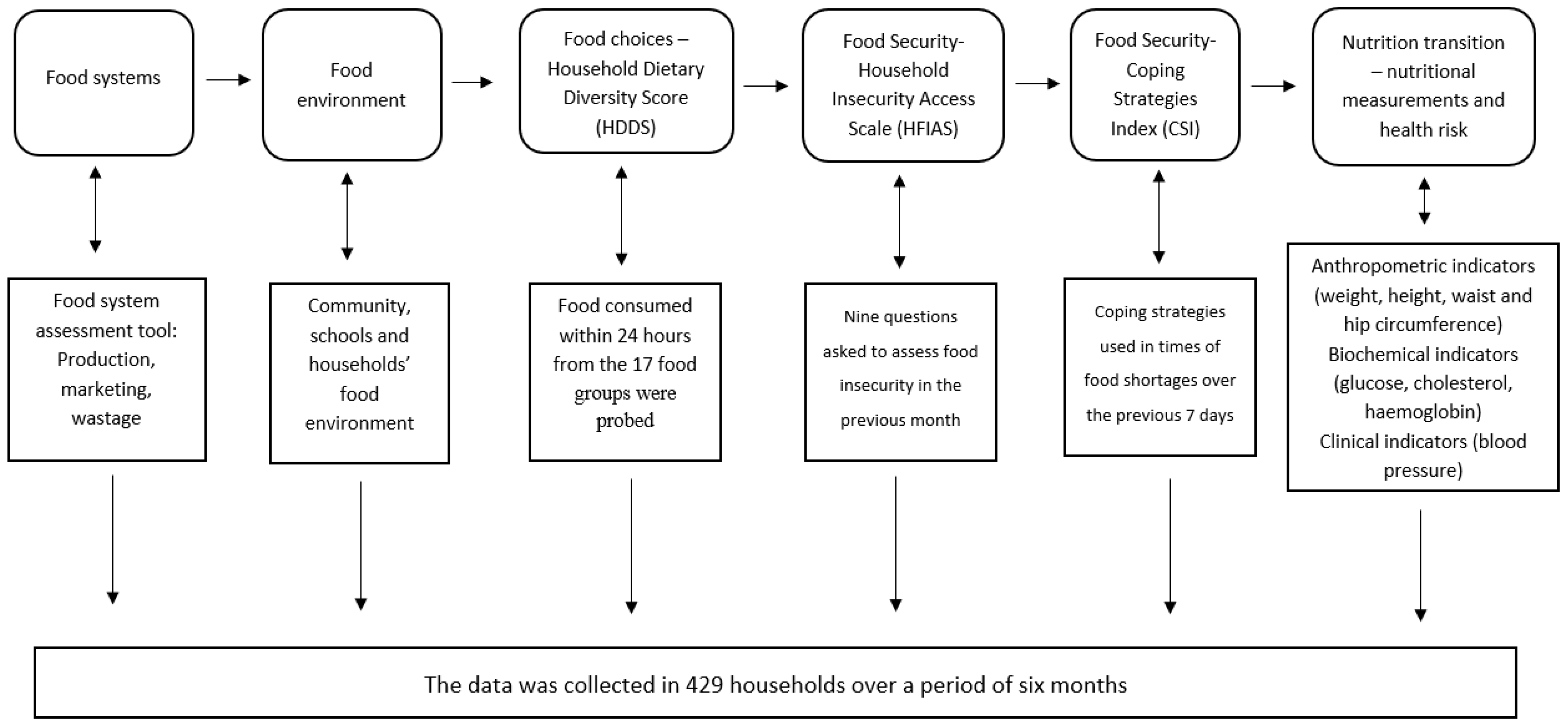
2. Materials and Methods
2.1. Study Design and Setting
2.2. Target Population, Sample Size Calculation, and Sampling Technique
2.3. Data Collection Tool and Procedure
2.4. Ethical Clearance
2.5. Data Analysis
3. Results
3.1. Socio-Demographic Information and Biophysical Environment
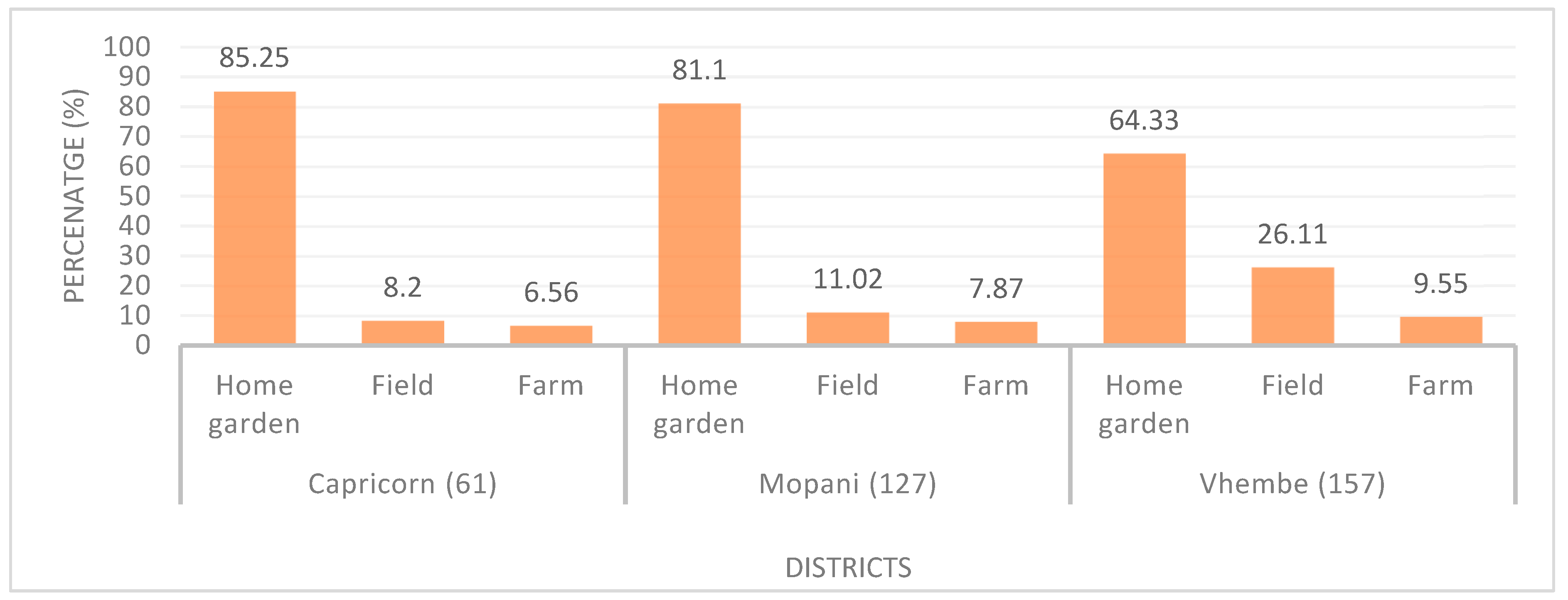
3.2. Food Systems Assessment
3.3. Food Environment Assessment
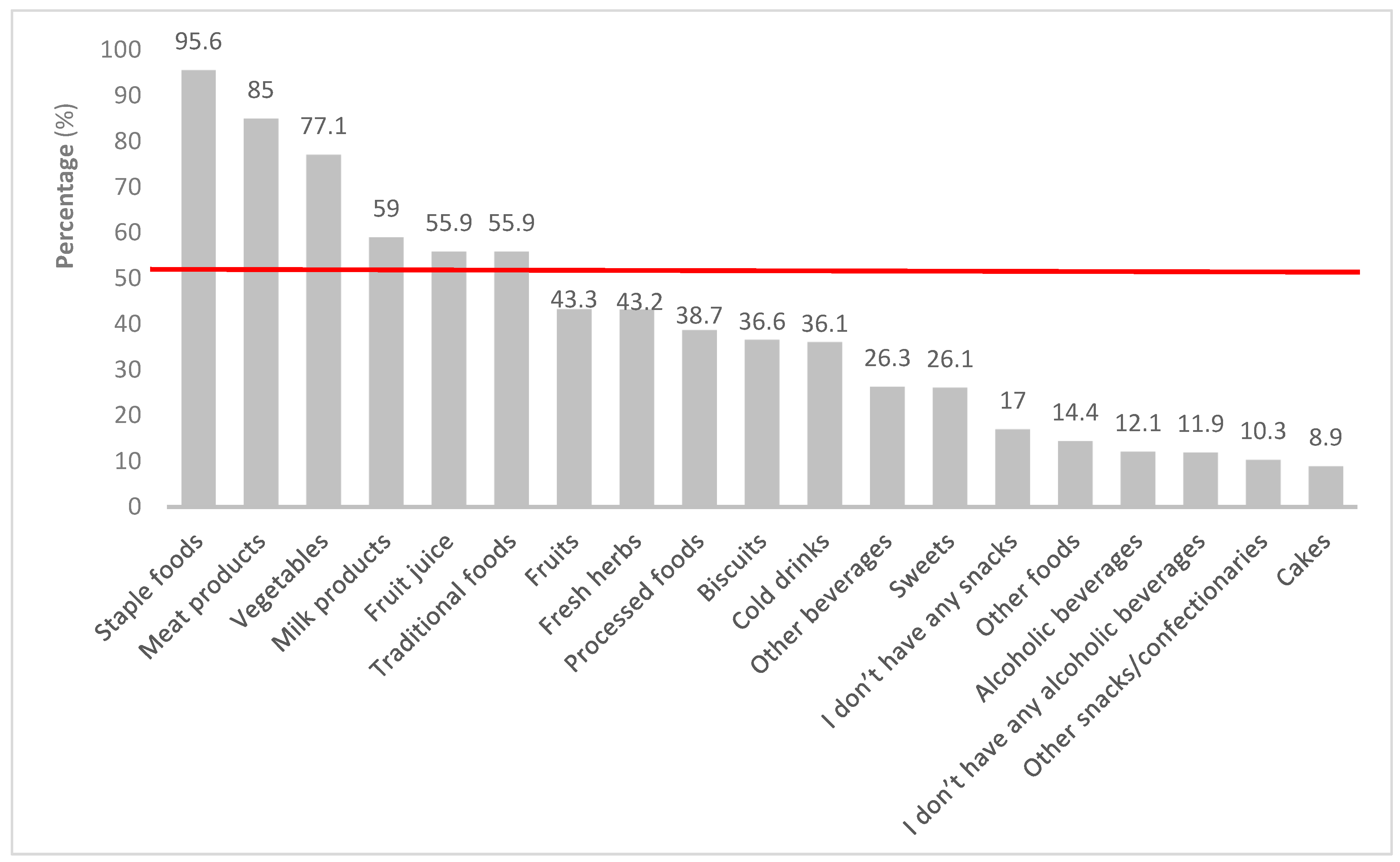
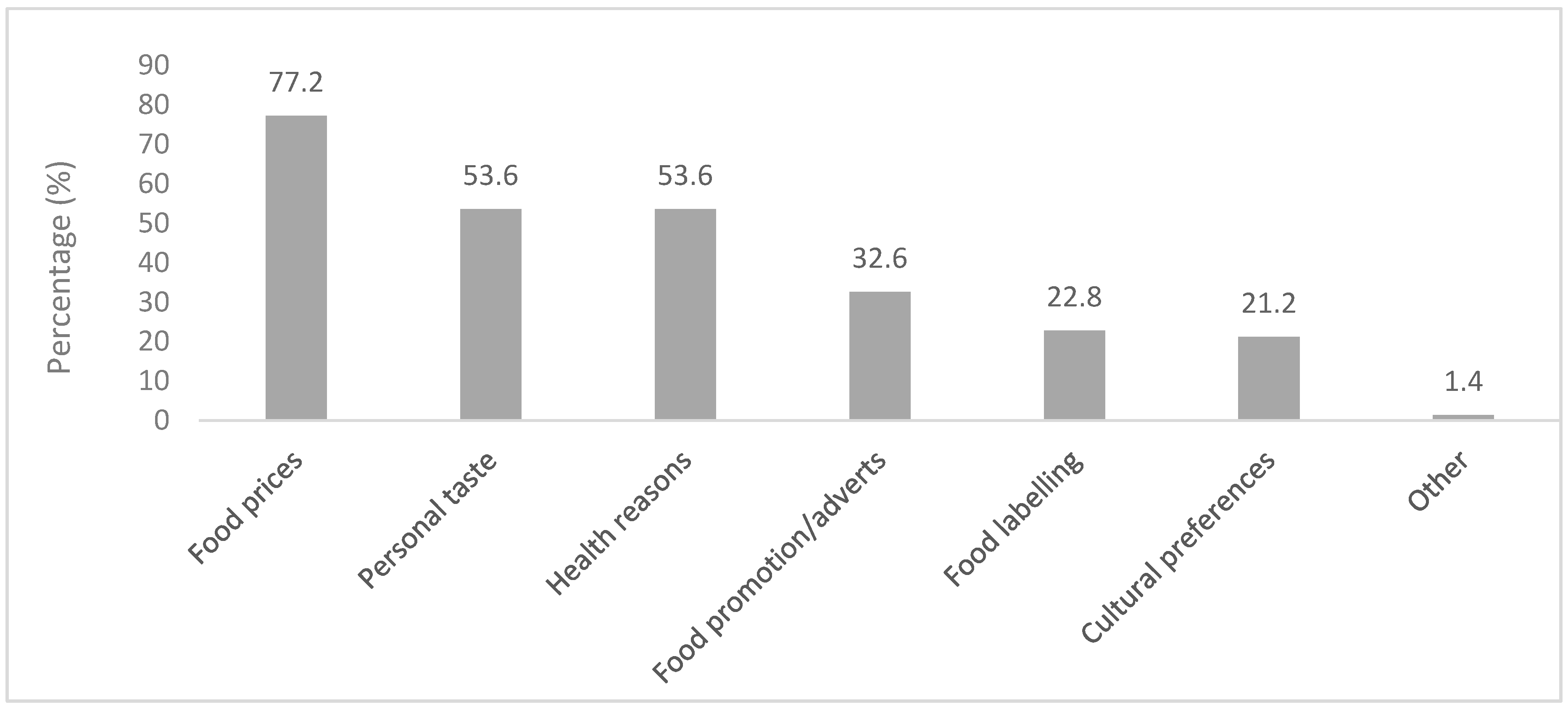
3.4. Food Choices
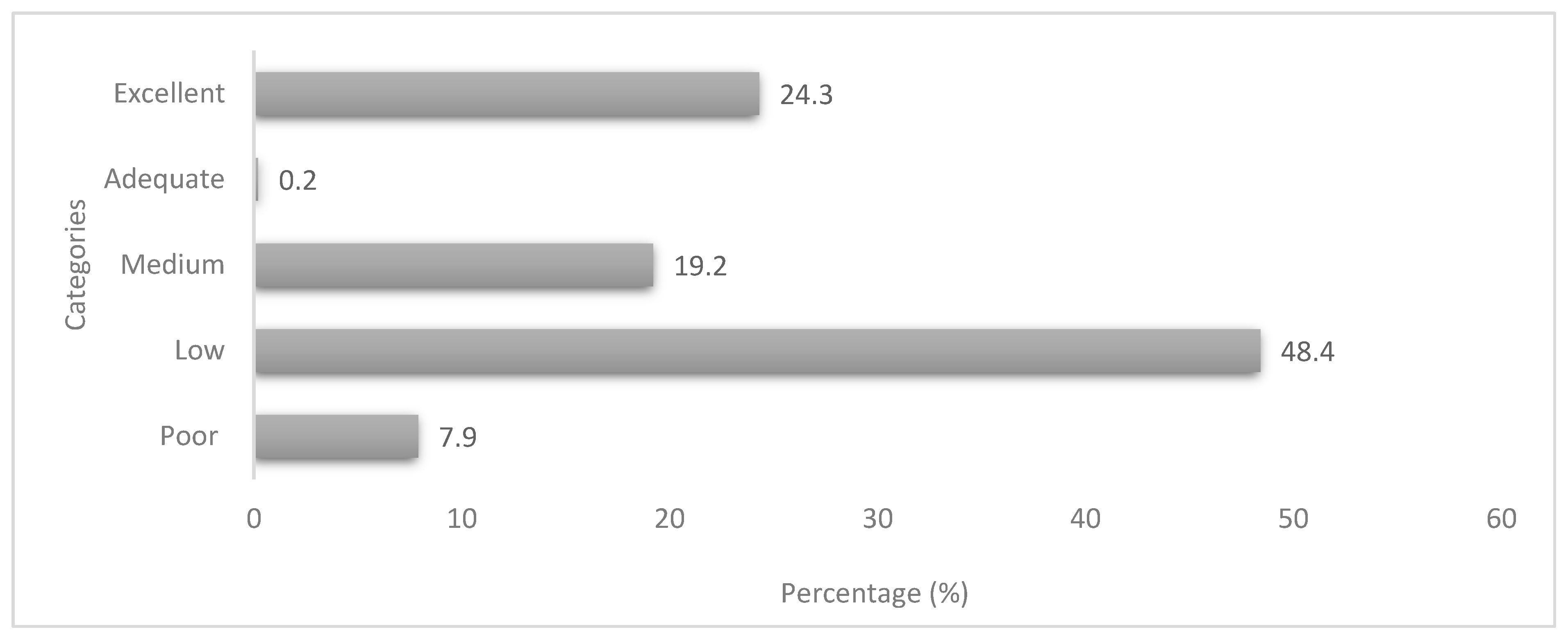
3.5. Household Food Security Status
3.6. Nutritional Status and Health Risk
3.6.1. Anthropometric Indicators of the Respondents
3.6.2. Biochemical Indicators of the Respondents
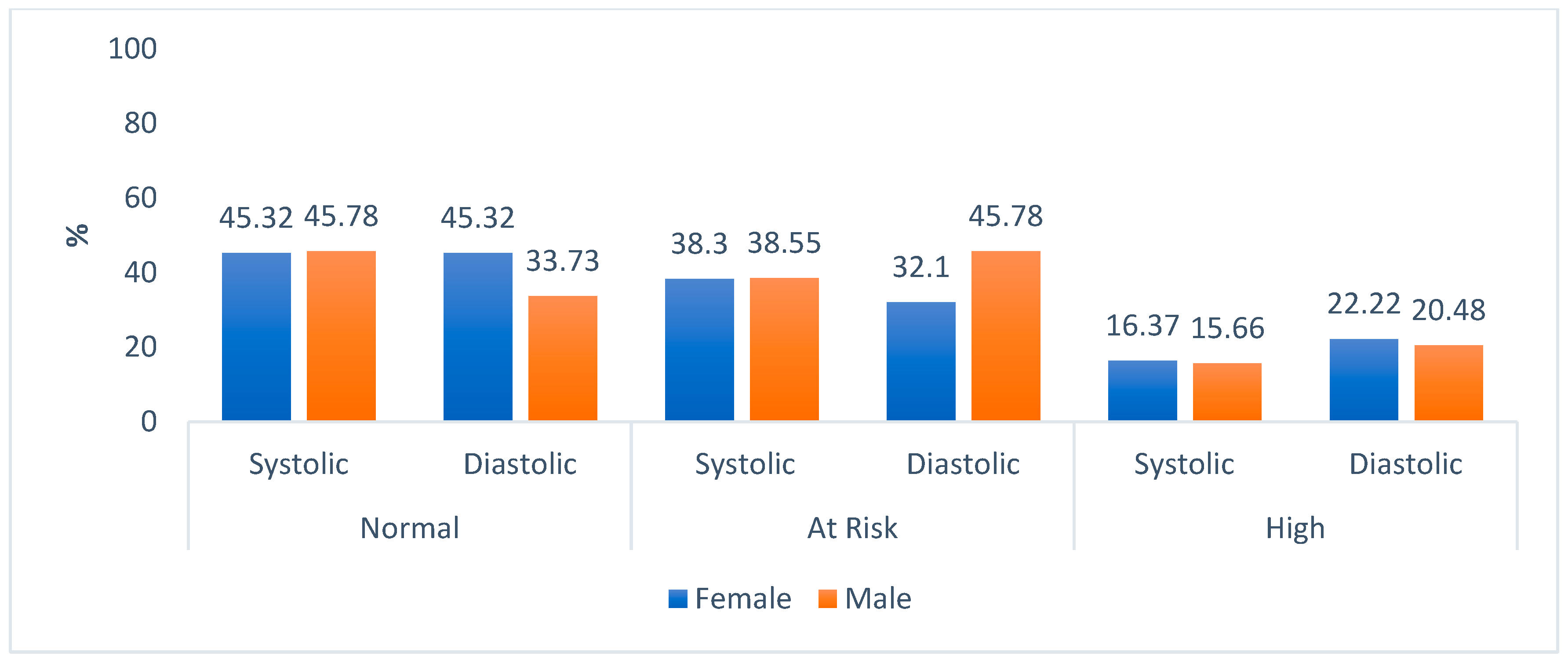
3.6.3. Clinical Indicators of Respondents
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Wildlife Fund-WWF. Food: Agri-Food Systems: Facts and Futures. Available online: https://dtnac4dfluyw8.cloudfront.net/downloads/wwf_food_report_facts_and_futures_2019.pdf?27341/agri-food-systems-facts-and-futures (accessed on 17 September 2022).
- Downs, S.M.; Ahmed, S.; Fanzo, J.; Herforth, A. Food Environment Typology: Advancing an Expanded Definition, Framework, and Methodological Approach for Improved Characterization of Wild, Cultivated, and Built Food Environments toward Sustainable Diets. Foods 2020, 9, 532. [Google Scholar] [CrossRef]
- Girard, A.W.; Little, P.; Yount, K.; Dominguez-Salas, P.; Kinabo, J.; Mwanri, A. Understanding the Drivers of Diet Change and Food Choice among Tanzanian Pastoralists to Inform Policy and Practice; Drivers of Food Choice Research Brief; University of South Carolina: Columbia, SC, USA, 2020. [Google Scholar]
- Nyiwul, L. Climate change adaptation and inequality in Africa: Case of water, energy and food insecurity. J. Clean. Prod. 2021, 278, 123393. [Google Scholar] [CrossRef]
- Food and Agriculture Organisation—FAO. The State of Food and Agriculture: Food Systems for Better Nutrition. Available online: www.fao.org/docrep/018/i3300e/i3300e00.htm (accessed on 26 June 2021).
- Turner, C.; Kadiyala, S.; Aggarwal, A.; Coates, J.; Drewnowski, A.; Hawkes, C.; Walls, H. Concepts and Methods for Food Environment Research in Low- and Middle-Income Countries; Agriculture, Nutrition and Health Academy Food Environments Working Group (ANH-FEWG), Innovative Methods and Metrics for Agriculture and Nutrition Actions (IMMANA) Programme: London, UK, 2017. [Google Scholar]
- Swinburn, B.; Vandevijvere, S.; Kraak, V.; Sacks, G.; Snowdon, W.; Hawkes, C.; Walker, C. Monitoring and benchmarking government policies and actions to improve the healthiness of food environments: A proposed Government Healthy Food Environment Policy Index. Obes. Rev. 2013, 14, 24–37. [Google Scholar] [CrossRef]
- Herforth, A.; Ahmed, S. The food environment, its effects on dietary consumption, and potential for measurement within agriculture-nutrition interventions. Food Secur. 2015, 7, 505–520. [Google Scholar] [CrossRef]
- Food and Agriculture Organisation—FAO. Influencing Food Environments for Healthy Diets. Available online: www.fao.org/3/a-i6484e.pdf (accessed on 13 May 2020).
- Global Panel on Agriculture and Food Systems for Nutrition—GLOPAN. Food Systems and diets: Facing the Challenges of the 21st Century. Available online: www.glopan.org/sites/default/files/ForesightReport.pdf (accessed on 13 May 2019).
- Popkin, B.M.; Adair, L.S.; Ng, S.W. NOW AND THEN: The Global nutrition transition: The pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef] [PubMed]
- Taruvinga, A.; Muchenje, V.; Mushunje, A. Determinants of rural household dietary diversity: The case of Amatole and Nyandeni districts, South Africa. Int. J. Sustain. Dev. Plan. 2013, 2, 2233–2247. Available online: https://isdsnet.com/ijds-v2n4-4.pdf (accessed on 1 July 2021).
- Ochieng, J.; Afari-Sefa, V.; Lukumay, P.J.; Dubois, T. Determinants of dietary diversity and the potential role of men in improving household nutrition in Tanzania. PLoS ONE 2017, 12, e0189022. [Google Scholar] [CrossRef]
- Morseth, M.; Grewal, N.K.; Kaasa, I.S.; Hatloy, A.; Barikmo, I.; Henjum, S. Dietary diversity is related to socioeconomic status among adult Saharawi refugees living in Algeria. BMC Public Health 2017, 17, 621. [Google Scholar] [CrossRef]
- Battersby, J. Food System transformation in the Absence of Food System Planning: The Case of Supermarket and Shopping Mall Retail Expansion in Cape Town, South Africa. Built Environ. 2017, 43, 417–430. [Google Scholar] [CrossRef]
- Haggblade, S.; Duodu, K.G.; Kabasa, J.D.; Minnaar, A.; Ojijo, N.K.O.; Taylor, J.R.N. Emerging Early Actions to Bend the Curve in Sub-Saharan Africa’s Nutrition Transition. Food Nutr. Bull. 2016, 37, 219–241. [Google Scholar] [CrossRef] [PubMed]
- Van Zyl, M.; Steyn, N.; Marais, M. Characteristics and factors influencing fast food intake of young adult consumers in Johannesburg, South Africa. S. Afr. J. Clin. Nutr. 2010, 23, 124–130. [Google Scholar] [CrossRef]
- Pillay-van Wyk, V.; Msemburi, W.; Laubscher, R.; Dorrington, R.E.; Groenewald, P.; Glass, T.; Nojilana, B.; Joubert, J.D.; Matzopoulos, R.; Prinsloo, M.; et al. Mortality trends and differentials in South Africa from 1997 to 2012: Second National Burden of Disease Study. Lancet Glob. Health 2016, 4, e642–e653. [Google Scholar] [CrossRef]
- Bradshaw, D.; Norman, R.; Pieterse, D.; Levitt, N.S.; The South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to diabetes in South Africa in 2000. S. Afr. Med. J. 2007, 97, 700–706. Available online: http://samj.org.za/index.php/samj/article/view/664/159 (accessed on 25 September 2020). [CrossRef] [PubMed]
- World Health Organization-WHO. “The Double Burden of Malnutrition: Policy Brief”. Geneva. Available online: https://apps.who.int/iris/handle/10665/255413 (accessed on 9 July 2019).
- De Cock, N.; D’haese, M.; Vink, N.; van Rooyen, C.J.; Staelens, L.; Schönfeldt, H.C.; D’haese, L. Food security in rural areas of Limpopo province, South Africa. Food Secur. 2013, 5, 269–282. [Google Scholar] [CrossRef]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. South African National Health and Nutrition Examination Survey (SANHANES-1). Available online: http://repository.hsrc.ac.za/bitstream/handle/20.500.11910/2864/7844.pdf?sequence=1&isAllowed=y (accessed on 23 October 2019).
- Chase, L.; Grubinger, V.P. Food, Farms and Community: Exploring Food Systems; University of New Hampshire: Durham, UK, 2014. [Google Scholar]
- Harris, J.; Chisanga, B.; Drimie, S.; Kennedy, G. Nutrition transition in Zambia: Changing food supply, food prices, household consumption, diet and nutrition outcomes. Food Secur. 2019, 11, 371–387. [Google Scholar] [CrossRef]
- Holdsworth, M.; Landais, E. Urban food environments in Africa: Implications for policy and research. Proc. Nutr. Soc. 2019, 78, 513–525. [Google Scholar] [CrossRef]
- Constantinides, S.V.; Turner, C.; Frongillo, E.A.; Bhandari, S.; Reyes, L.I.; Blake, C.E. Using a global food environment framework to understand relationships with food choice in diverse low- and middle-income countries. Glob. Food Secur. 2021, 29, 100511. [Google Scholar] [CrossRef]
- Chen, P.-J.; Antonelli, M. Conceptual Models of Food Choice: Influential Factors Related to Foods, Individual Differences, and Society. Foods 2020, 9, 1898. [Google Scholar] [CrossRef]
- Rosenzweig, C.; Mbow, C.; Barioni, L.G.; Benton, T.G.; Herrero, M.; Krishnapillai, M.; Liwenga, E.T.; Pradhan, P.; Rivera-Ferre, M.G.; Sapkota, T.; et al. Climate change responses benefit from a global food system approach. Nat. Food 2020, 1, 94–97. Available online: https://www.fao.org/3/ca7824en/ca7824en.pdf (accessed on 20 June 2023). [CrossRef]
- Noort, M.W.J.; Renzetti, S.; Linderhof, V.; du Rand, G.E.; Marx-Pienaar, N.J.M.M.; de Kock, H.L.; Magano, N.; Taylor, J.R.N. Towards Sustainable Shifts to Healthy Diets and Food Security in Sub-Saharan Africa with Climate-Resilient Crops in Bread-Type Products: A Food System Analysis. Foods 2022, 11, 135. [Google Scholar] [CrossRef] [PubMed]
- Granheim, S.I.; Løvhaug, A.L.; Terragni, L.; Torheim, L.E.; Thurston, M. Mapping the digital food environment: A systematic scoping review. Obes. Rev. 2022, 23, e13356. [Google Scholar] [CrossRef] [PubMed]
- Zurek, M.; Hebinck, A.; Selomane, O. Climate change and the urgency to transform food systems. Science 2022, 376, 1416–1421. [Google Scholar] [CrossRef] [PubMed]
- Nicolétis, É.; Caron, P.; El Solh, M.; Cole, M.; Fresco, L.O.; Godoy-Faúndez, A.; Kadleciková, M.; Kennedy, E.; Khan, M.; Li, X.; et al. Agroecological and Other Innovative Approaches for Sustainable Agriculture and Food Systems That Enhance Food Security and Nutrition. A Report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Available online: https://www.fao.org/3/ca5602en/ca5602en.pdf (accessed on 18 June 2023).
- Valentini, R.; Sievenpiper, J.L.; Antonelli, M.; Dembska, K. (Eds.) Achieving the Sustainable Development Goals through Sustainable Food Systems; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Laar, A.K.; Addo, P.; Aryeetey, R.; Agyemang, C.; Zotor, F.; Asiki, G.; Rampalli, K.K.; Amevinya, G.S.; Tandoh, A.; Nanema, S.; et al. Perspective: Food Environment Research Priorities for Africa—Lessons from the Africa Food Environment Research Network. Adv. Nutr. 2022, 13, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Batal, M.; Deaconu, A.; Steinhouse, L. The nutrition transition and the double burden of malnutrition. In Nutritional Health: Strategies for Disease Prevention; Springer: Cham, Switzerland, 2023; Volume 28, pp. 345–350. [Google Scholar] [CrossRef]
- Rolls, B.J.; Keller, K.L.; Hayes, J.E.; Masterson, T.D. Food choice: Behavioral aspects. Encycl. Hum. Nutr. 2023, 1–4, 62–69. [Google Scholar] [CrossRef]
- Statistics South Africa—Stats SA. 2020 Mid-Year Population Estimates. Available online: http://www.statssa.gov.za/publications/P0302/P03022020.pdf (accessed on 2 June 2021).
- Green, S.H.; Glanz, K. Development of the Perceived Nutrition Environment Measures Survey. Am. J. Prev. Med. 2015, 49, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Saelens, B.E.; Glanz, K.; Sallis, J.F.; Frank, L.D. Nutrition Environment Measures Study in Restaurants (NEMS-R): Development and evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition Environment Measures Survey in Stores (NEMS-S): Development and Evaluation. Am. J. Prev. Med. 2007, 32, 273–281. [Google Scholar] [CrossRef]
- Food and Agriculture Organisation—FAO. Dietary Diversity Questionnaire. Available online: http://www.fao.org/fileadmin/user_upload/eufao-fsi4dm/doc-training/hdd.pdf (accessed on 23 July 2021).
- Food and Agriculture Organisation—FAO. “The Coping Strategies Index: A Tool for Rapid Measurement of Household Food Security and the Impact of Food Aid Programs in Humanitarian Emergencies: Field Methods Manual”. 2nd ed. Available online: www.fao.org/3/a-ae513e.pdf (accessed on 19 May 2019).
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v3). Washington DC. FHI 360/FANTA. Available online: https://www.fantaproject.org/sites/default/files/resources/HFIAS_ENG_v3_Aug07.pdf (accessed on 16 July 2021).
- Food and Agriculture Organisation—FAO. Guidelines for Measuring Household and Individual Dietary Diversity. Available online: https://www.fao.org/3/i1983e/i1983e.pdf (accessed on 9 February 2022).
- Del Ninno, C.; Dorosh, P.A.; Smith, L.C. Public Policy, Market and Household Coping Strategies in Bangladesh: Avoiding Food Security Crisis Following the 1998 Floods. World Dev. 2003, 31, 1221–1238. [Google Scholar] [CrossRef]
- World Health Organization—WHO. Non-Communicable Diseases Global Monitoring Framework: Indicator Definitions and Specifications. Available online: https://www.who.int/nmh/ncd-tools/indicators/GMF_Indicator_Definitions_Version_NOV2014.pdf (accessed on 16 July 2019).
- World Health Organisation—WHO; International Federation on Diabetes—IDF. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation. Available online: https://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf (accessed on 9 February 2022).
- The Heart and Stroke Foundation South Africa. Cholesterol. Available online: https://www.heartfoundation.co.za/cholesterol/ (accessed on 11 October 2021).
- World Health Organization–WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Available online: https://apps.who.int/iris/handle/10665/85839 (accessed on 9 February 2022).
- American College of Cardiology. High Blood Pressure Guidelines. Available online: https://www.cardiosmart.org/news/2017/11/high-blood-pressure-guidelines-2017#:~:text=For%20example%2C%20blood%20pressure%20between,at%20130%2F80%20mm%20Hg (accessed on 9 February 2022).
- Statistics South Africa—Stats SA. General Household Survey. Available online: https://www.statssa.gov.za/publications/P0318/P03182018.pdf (accessed on 3 August 2021).
- Mkhawani, K.; Motadi, S.A.; Mabapa, N.S.; Mbhenyane, X.G.; Blaauw, R. Effects of rising food prices on household food security on female-headed households in Runnymede Village, Mopani District, South Africa. S. Afr. J. Clin. Nutr. 2016, 29, 69–74. Available online: http://www.sajcn.co.za/index.php/SAJCN/article/view/994 (accessed on 8 November 2019).
- Statistics South Africa—Stats SA. South Africa Demographic and Health Survey: Key Indicator Report. Available online: https://www.statssa.gov.za/publications/Report%2003-00-09/Report%2003-00092016.pdf (accessed on 6 October 2021).
- Mbhenyane, X.G.; Tambe, B.A.; Phooko-Rabodiba, D.A.; Nesamvuni, C.N. The relationship between employment status of the mother, household hunger and nutritional status of children in Sekhukhune district, Limpopo province. Afr. J. Food Agric. Nutr. Dev. 2020, 20, 15821–15836. [Google Scholar] [CrossRef]
- Cheteni, P. Youth Participation in Agriculture in the Nkonkobe District Municipality, South Africa. J. Hum. Ecol. 2016, 55, 207–213. Available online: https://www.econstor.eu/bitstream/10419/162735/1/Youth%20Participation%20in%20Agriculture%20in%20the%20Nkonkobe%20District%20Municipality.pdf (accessed on 1 July 2021). [CrossRef]
- Cheteni, P.; Khamfula, Y.; Mah, G. Exploring Food Security and Household Dietary Diversity in the Eastern Cape Province, South Africa. Sustainability 2020, 12, 1851. [Google Scholar] [CrossRef]
- Ward, P.R.; Coveney, J.; Verity, F.; Carter, P.; Schilling, M. Cost and affordability of healthy food in rural South Australia. Rural Remote Health 2012, 12, 1938. [Google Scholar] [CrossRef]
- Pietermaritzburg Economic Justice & Dignity Group—PMBEJD. Household Affordability Index. Available online: https://pmbejd.org.za/wp-content/uploads/2023/01/January-2023-Household-Affordability-Index-PMBEJD_25012023.pdf (accessed on 18 February 2023).
- Department of Employment and Labour. Government Gazette on National Minimum Wage Act: Annual Review and Adjustment of the National Minimum Wage for 2021. Available online: https://www.gov.za/sites/default/files/gcis_document/202102/44136gon76.pdf (accessed on 2 July 2021).
- Beyene, M.; Worku, A.G.; Wassie, M.M. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: A cross- sectional study. BMC Public Health 2015, 3, 1007. [Google Scholar] [CrossRef] [PubMed]
- Harris-Fry, H.; Azad, K.; Kuddus, A.; Shaha, S.; Nahar, B.; Hossen, M.; Younes, L.; Costello, A.; Fottrell, E. Socio-economic determinants of household food security and women’s dietary diversity in rural Bangladesh: A cross-sectional study. J. Health Popul. Nutr. 2015, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Mullins, L.; Charlebois, S.; Finch, E.; Music, J. Home Food Gardening in Canada in Response to the COVID-19 Pandemic. Sustainability 2021, 13, 3056. [Google Scholar] [CrossRef]
- Ogundiran, O.A.; Monde, N.; Agholor, I.; Odeyemi, A.S. The Role of Home Gardens in Household Food Security in Eastern Cape: A Case Study of Three Villages in Nkonkobe Municipality. J. Agric. Sci. 2013, 6, 129–136. [Google Scholar] [CrossRef]
- Bettencourt, E.M.V.; Tilman, M.; Narciso, V.; Da Silva Carvalho, M.L.; de Sousa Henriques, P.D. The Livestock Roles in the Wellbeing of Rural Communities of Timor-Leste. Rev. Econ. Sociol. Rural 2015, 53, S63–S80. [Google Scholar] [CrossRef]
- Roberto, C.A.; Swinburn, B.; Hawkes, C.; Huang, T.T.-K.; Costa, S.A.; Ashe, M.; Zwicker, L.; Cawley, J.H.; Brownell, K.D. Patchy progress on obesity prevention: Emerging examples, entrenched barriers, and new thinking. Lancet 2015, 385, 2400–2409. [Google Scholar] [CrossRef]
- Lang, T. Reshaping the Food System for Ecological Public Health. J. Hunger. Environ. Nutr. 2009, 4, 315–335. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Emergency Fund—UNICEF. The State of Food Security and Nutrition in the World: Safeguarding against Economic Slowdowns and Downturns. Available online: https://www.unicef.org/media/55921/file/SOFI-2019-full-report.pdf (accessed on 13 July 2021).
- O’halloran, S.A.; Eksteen, G.; Polayya, N.; Ropertz, M.; Senekal, M. The Food Environment of Primary School Learners in a Low-to-Middle-Income Area in Cape Town, South Africa. Nutrients 2021, 13, 2043. [Google Scholar] [CrossRef] [PubMed]
- Marraccini, T.; Meltzer, S.; Bourne, L.; Draper, C.E.; Johnston, C.A.; Moreno, J.P.; El-Mubasher, A.; Woehler, D.; Isoldi, K.K.; Dalton, S.; et al. A Qualitative Evaluation of Exposure to and Perceptions of the Woolworths Healthy Tuck Shop Guide in Cape Town, South Africa. Child. Obes. 2012, 8, 369–377. [Google Scholar] [CrossRef]
- de Villiers, A.; Steyn, N.P.; Draper, C.E.; Fourie, J.M.; Barkhuizen, G.; Lombard, C.J.; Dalais, L.; Abrahams, Z.; Lambert, E.V. “HealthKick”: Formative assessment of the health environment in low-resource primary schools in the Western Cape Province of South Africa. BMC Public Health 2012, 12, 794. [Google Scholar] [CrossRef]
- Temple, N.J.; Steyn, N.P.; Myburgh, N.G.; Nel, J.H. Food items consumed by students attending schools in different socioeconomic areas in Cape Town, South Africa. Nutrition 2006, 22, 252–258. [Google Scholar] [CrossRef]
- Kroll, F.; Swart, E.C.; Annan, R.A.; Thow, A.M.; Neves, D.; Apprey, C.; Aduku, L.N.E.; Agyapong, N.A.F.; Moubarac, J.-C.; Du Toit, A.; et al. Mapping Obesogenic Food Environments in South Africa and Ghana: Correlations and Contradictions. Sustainability 2019, 11, 3924. [Google Scholar] [CrossRef]
- Chai, W.; Fan, J.X.; Wen, M. Association of Individual and Neighborhood Factors with Home Food Availability: Evidence from the National Health and Nutrition Examination Survey. J. Acad. Nutr. Diet. 2018, 118, 815–823. [Google Scholar] [CrossRef]
- National Agricultural Marketing Council—NAMC. Food Price Monitor: August Issue. Available online: https://www.namc.co.za/wp-content/uploads/2017/09/NAMC-Food-Price-Monitor-31-Aug-2016.pdf (accessed on 2 July 2021).
- Castro, I.A.; Majmundar, A.; Williams, C.B.; Baquero, B. Customer Purchase Intentions and Choice in Food Retail Environments: A Scoping Review. Int. J. Environ. Res. Public Health 2018, 15, 2493. [Google Scholar] [CrossRef]
- Faber, M.; Witten, C.; Drimie, S. Community-based agricultural interventions in the context of food and nutrition security in South Africa. S. Afr. J. Clin. Nutr. 2011, 24, 21–30. [Google Scholar] [CrossRef]
- Tambe, B.A.; Tchuenchieu, A.K.; Tchuente, B.T.; Edoun, F.E.; Mouafo, H.T.; Kesa, H.; Medou, G.N. The state of food security and dietary diversity during the COVID-19 pandemic in Cameroon. J. Health Res. 2021, 6, 1–11. Available online: https://www.ikprress.org/index.php/JOMAHR/article/view/6216 (accessed on 16 July 2022).
- Chakona, G.; Shackleton, C. Minimum Dietary Diversity Scores for Women Indicate Micronutrient Adequacy and Food Insecurity Status in South African Towns. Nutrients 2017, 9, 812. [Google Scholar] [CrossRef] [PubMed]
- Nabuuma, D.; Ekesa, B.; Faber, M.; Mbhenyane, X. Food security and food sources linked to dietary diversity in rural smallholder farming households in central Uganda. AIMS Agric. Food 2021, 6, 644–662. [Google Scholar] [CrossRef]
- World Food Programme—WFP. Comprehensive Food Security and Vulnerability Analysis (CFSVA): Democratic Republic of Congo. Available online: https://documents.wfp.org/stellent/groups/public/documents/ena/wfp266329.pdf (accessed on 13 July 2021).
- Sharma, J.R.; Mabhida, S.E.; Myers, B.; Apalata, T.; Nicol, E.; Benjeddou, M.; Muller, C.; Johnson, R. Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa. Int. J. Environ. Res. Public Health 2021, 18, 1215. [Google Scholar] [CrossRef] [PubMed]
- Crush, J.; Caesar, M. City Without Choice: Urban Food Insecurity in Msunduzi, South Africa. Urban Forum 2014, 25, 165–175. [Google Scholar] [CrossRef]
- World Health Organisation—WHO. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 October 2021).
- Cois, A.; Day, C. Obesity trends and risk factors in the South African adult population. BMC Obes. 2015, 2, 42. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation—WHO. Global Report on Diabetes. Available online: https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf (accessed on 7 October 2021).
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence—NICE. Hypertension in Adults: Diagnosis and Management. Available online: https://www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-management-pdf-66141722710213 (accessed on 7 October 2021).

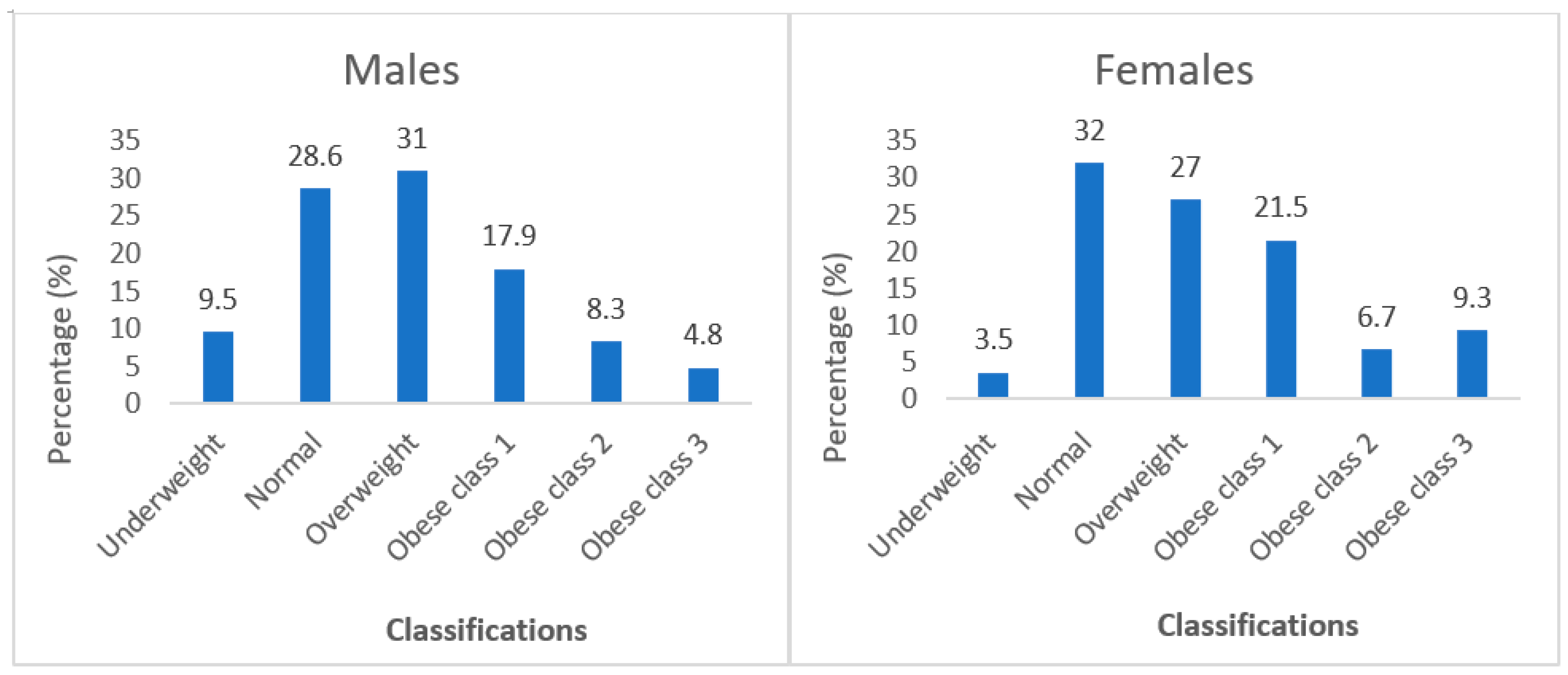
| Interpretation | Classifications (kg/m2) |
|---|---|
| Underweight | <18.5 |
| Normal | 18.5–24.99 |
| Overweight | 25–29.99 |
| Obese class 1 | 30–34.99 |
| Obese class 2 | 35–39.99 |
| Obese class 3 | >40 |
| Categories | Frequency (n) | Percentage (%) | p Values |
|---|---|---|---|
| Age (years) * | |||
| 18–35 | 210 | 49.2 | |
| 36–55 | 156 | 36.5 | <0.001 |
| >55 | 61 | 14.3 | |
| Marital Status | |||
| Single | 248 | 57.8 | |
| Married | 119 | 27.7 | <0.001 |
| Divorced | 13 | 3.0 | |
| Widowed | 25 | 5.8 | |
| Cohabitation | 22 | 5.1 | |
| Other | 2 | 0.5 | |
| Gender | |||
| Female | 345 | 80.4 | <0.001 |
| Male | 84 | 19.6 | |
| Education | |||
| Never attended school | 21 | 4.9 | |
| Primary education (grade 1–7) | 26 | 6.1 | |
| Secondary education (grade 8–12) | 232 | 54.1 | <0.001 |
| Tertiary education (degree, diploma, etc.) | 146 | 34.0 | |
| Other | 4 | 0.9 | |
| Usage | No of Days | |||||||
|---|---|---|---|---|---|---|---|---|
| Behaviours | % (n) | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Rely on less preferred and less expensive foods | 31.3 (134) | 4.7 (20) | 8.4 (36) | 5.1 (22) | 2.8 (12) | 2.1 (9) | 0.7 (3) | 7.5 (32) |
| Reduce portion sizes | 23.1 (99) | 4.7 (20) | 6.3 (27) | 4.0 (17) | 3.5 (15) | 0.2 (1) | 0.0 (0) | 4.4 (19) |
| Limit portion size at mealtimes | 22.4 (96) | 4.0 (17) | 6.8 (29) | 3.7 (16) | 2.8 (12) | 0.9 (4) | 0.0 (0) | 4.2 (18) |
| Borrow food, or rely on help from a friend or relative | 18.0 (80) | 8.4 (36) | 4.4 (19) | 2.1 (9) | 1.4 (6) | 0.5 (2) | 0.0 (0) | 1.2 (5) |
| Reduce the number of meals eaten in a day | 17.7 (76) | 4.7 (20) | 6.3 (27) | 2.1 (9) | 0.9 (4) | 0.9 (4) | 0.2 (1) | 2.6 (11) |
| Not having enough food or money to buy food | 15.1 (65) | 3.7 (16) | 3.5 (15) | 3.3 (14) | 1.4 (6) | 0.2 (1) | 0.0 (0) | 3.0 (13) |
| Purchase food on credit | 13.7 (59) | 6.8 (29) | 3.0 (13) | 1.6 (7) | 1.2 (5) | 0.2 (1) | 0.2 (1) | 0.7 (3) |
| Skip meals | 13.6 (59) | 3.7 (16) | 5.1 (22) | 2.1 (9) | 0.9 (4) | 0.0 (0) | 0.2 (1) | 1.6 (7) |
| Borrow money to buy food from neighbours | 12.6 (54) | 7.5 (32) | 2.6 (11) | 0.9 (4) | 0.2 (1) | 0.9 (4) | 0.0 (0) | 0.5 (2) |
| Take other measures | 13.3 (51) | 4.0 (17) | 2.7 (11) | 3.7 (10) | 0.6 (3) | 0.2 (1) | 0.0 (0) | 2.1 (9) |
| Drink tea only | 11.3 (48) | 2.6 (11) | 4.7 (20) | 1.9 (8) | 0.2 (1) | 1.9 (8) | 0.0 (0) | 0.0 (0) |
| Restrict consumption by adults in order for small children to eat | 7.4 (32) | 2.8 (12) | 2.3 (10) | 1.2 (5) | 0.2 (1) | 0.0 (0) | 0.0 (0) | 0.9 (4) |
| Borrow food from neighbours | 6.9 (29) | 1.9 (8) | 2.6 (11) | 0.7 (3) | 0.7 (3) | 0.5 (2) | 0.0 (0) | 0.5 (2) |
| Sleep without food | 5.5 (24) | 3.0 (13) | 0.9 (4) | 1.2 (5) | 0.0 (0) | 0.2 (1) | 0.0 (0) | 0.2 (1) |
| Send household members to beg | 5.1 (22) | 1.4 (6) | 1.6 (7) | 1.2 (5) | 0.2 (1) | 0.5 (2) | 0.2 (1) | 0.0 (0) |
| Send children to neighbours or relatives | 5.1 (22) | 2.1 (9) | 1.9 (8) | 0.5 (2) | 0.2 (1) | 0.2 (1) | 0.0 (0) | 0.2 (1) |
| Send household members to eat elsewhere | 4.4 (19) | 1.2 (5) | 1.9 (8) | 0.2 (1) | 0.2 (1) | 0.0 (0) | 0.0 (0) | 0.9 (4) |
| Feed female members of HH at the expense of male members | 2.5 (11) | 1.4 (6) | 0.5 (2) | 0.2 (1) | 0.0 (0) | 0.2 (1) | 0.0 (0) | 0.2 (1) |
| Exchange sorghum/green mealies for white mealie meals from local shops or mobile vendors | 2.5 (11) | 1.4 (6) | 0.9 (4) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.2 (1) |
| Sell traditional beer and buy food with profit | 2.3 (10) | 0.7 (3) | 1.4 (6) | 0.2 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Gather wild food, hunt, or harvest immature crops | 2.1 (9) | 1.4 (6) | 0.5 (2) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.2 (1) |
| Consume seed stock held for next season | 2.1 (9) | 0.9 (4) | 0.5 (2) | 0.5 (2) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.2 (1) |
| Feed working members of HH at the expense of non-working members | 2.1 (9) | 1.2 (5) | 0.5 (2) | 0.2 (1) | 0.2 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Feed adult members of HH at the expense of children members | 2.1 (9) | 0.5 (2) | 0.2 (1) | 1.2 (5) | 0.2 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Feed male members of HH at the expense of female members | 2.1 (9) | 0.0 (0) | 0.5 (2) | 0.2 (1) | 1.4 (6) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Food Security Characteristics | % |
|---|---|
| HFIAS domains | |
| Anxiety and uncertainty over food | 45.2 |
| Insufficient food quality | 40.2 |
| Insufficient food intake | 46.0 |
| HFIAS conditions | |
| Worrying about food intake | 43.7 |
| Not able to eat preferred food | 40.6 |
| Limited variety of food | 39.5 |
| Eating unwanted foods | 38.9 |
| Eating smaller meals | 33.1 |
| Eating fewer meals | 26.8 |
| No food in the house | 15.6 |
| Sleeping hungry | 8.2 |
| The whole day and night without food | 6.5 |
| HFIAS categories | |
| Food secure | 46.0 |
| Mildly food insecure | 23.8 |
| Moderately food insecure | 26.3 |
| Severe food insecurity | 4.0 |
| Variables | Bivariate | Multivariate | |||||
|---|---|---|---|---|---|---|---|
| Characteristics | N | HFI (%) | OR (CI) | p Value | AOR (CI) | p Value | |
| Gender | Male | 345 | 82.83 | 0.716 (0.444–1.155) | 0.181 | 1.048 (0.561–1.957) | 0.884 |
| Female | 84 | 1.17 | |||||
| Education | Illiterate | 21 | 5.15 | 0.886 (0.365–2.150) | 0.826 | 0.827 (0.259–2.642) | 0.748 |
| Literate | 408 | 94.85 | |||||
| Farm ownership | Yes | 29 | 7.30 | 0.829 (.386–1.780) | 0.702 | 0.987 (0.410–2.379) | 0.977 |
| No | 400 | 92.70 | |||||
| Field ownership | Yes | 60 | 12.45 | 1.322 (0.765–2.282) | 0.331 | 1.709 (0.866–3.374) | 0.122 |
| No | 369 | 87.55 | |||||
| Home garden ownership | Yes | 256 | 63.95 | 0.685 (0.465–1.011) | 0.035 | 0.670 (0.405–1.110) | 0.120 |
| No | 172 | 36.05 | |||||
| DDS | Poor dietary intake | 240 | 53.65 | 1.227 (0.836–1.800) | 0.329 | 1.370 (0.841–2.233) | 0.206 |
| Good dietary intake | 189 | 46.35 | |||||
| Nutritional knowledge | Yes | 363 | 81.97 | 1.576 (0.916–2.710) | 0.064 | ||
| No | 66 | 18.03 | |||||
| BMI | ≤Normal | 20 | 5.15 | 0.773 (0.309–1.931) | 0.651 | 0.788 (0.269–2.309) | 0.664 |
| >Normal | 406 | 93.56 | |||||
| Variables | % | Mean | Std. Deviation | p Value |
|---|---|---|---|---|
| Random blood glucose (mmol/L) | 9.7386 | 3.4863 | <0.001 | |
| Normal (<11.1) | 67.5 | |||
| Diabetes (>11.1) | 32.5 | |||
| Total blood cholesterol (mmol/L) | 3.6893 | 0.7421 | <0.001 | |
| Normal (<5.0) | 93.2 | |||
| At risk (<7.5) | 6.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nedzingahe, V.; Tambe, B.A.; Zuma, M.K.; Mbhenyane, X.G. Associations among Food Systems, Food Environments, Food Choices, Food Security, and Nutrition Transition in Limpopo Province, South Africa: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 6557. https://doi.org/10.3390/ijerph20166557
Nedzingahe V, Tambe BA, Zuma MK, Mbhenyane XG. Associations among Food Systems, Food Environments, Food Choices, Food Security, and Nutrition Transition in Limpopo Province, South Africa: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(16):6557. https://doi.org/10.3390/ijerph20166557
Chicago/Turabian StyleNedzingahe, Vhushavhelo, Betrand Ayuk Tambe, Mthokozisi Kwazi Zuma, and Xikombiso Gertrude Mbhenyane. 2023. "Associations among Food Systems, Food Environments, Food Choices, Food Security, and Nutrition Transition in Limpopo Province, South Africa: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 16: 6557. https://doi.org/10.3390/ijerph20166557
APA StyleNedzingahe, V., Tambe, B. A., Zuma, M. K., & Mbhenyane, X. G. (2023). Associations among Food Systems, Food Environments, Food Choices, Food Security, and Nutrition Transition in Limpopo Province, South Africa: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(16), 6557. https://doi.org/10.3390/ijerph20166557







