Exploring the Role of Birth Environment on Italian Mothers’ Emotional Experience during Childbirth
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection Tools
2.3. Data Analysis
2.3.1. Spatial Analysis
2.3.2. Statistical Analysis
3. Results
3.1. Identifying the Study Sites
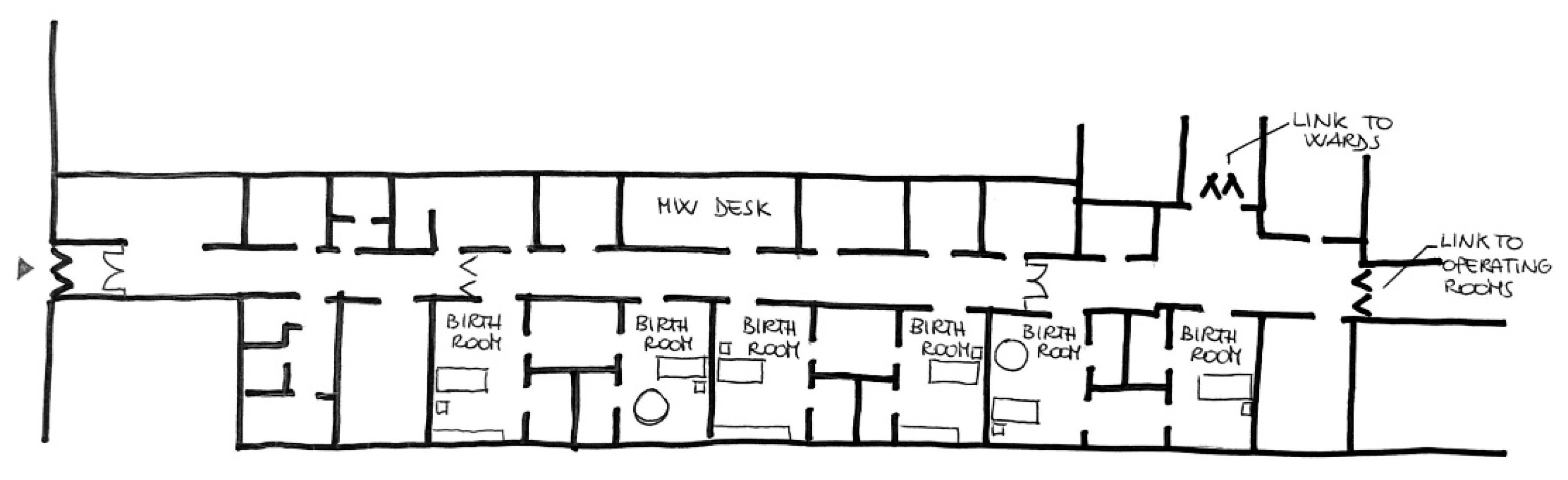
- Case 1—Hospital setting (low degree of spatial-physical humanization setting)
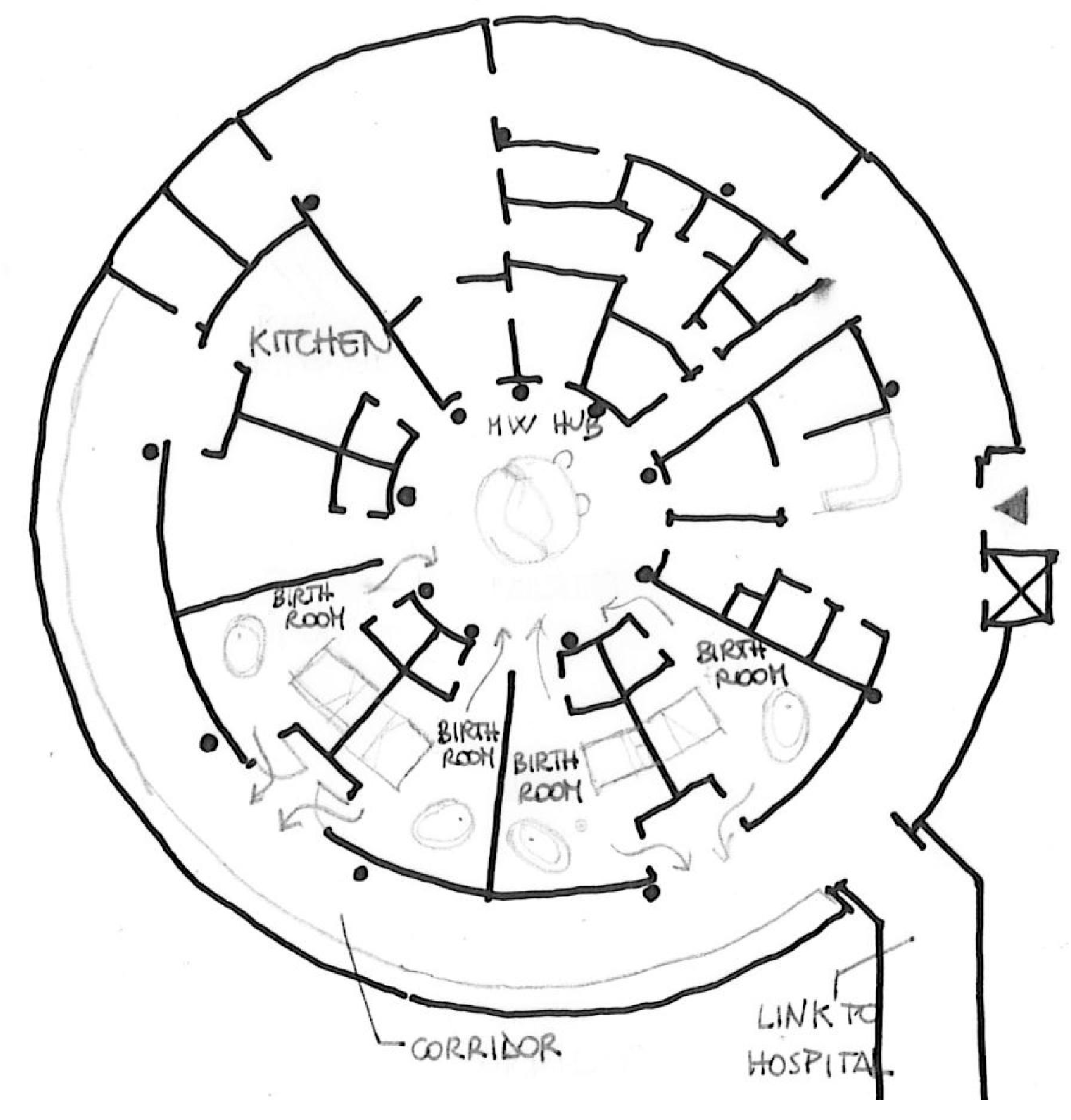
- Case 2—Birth Centre setting (high degree of spatial-physical humanization setting)
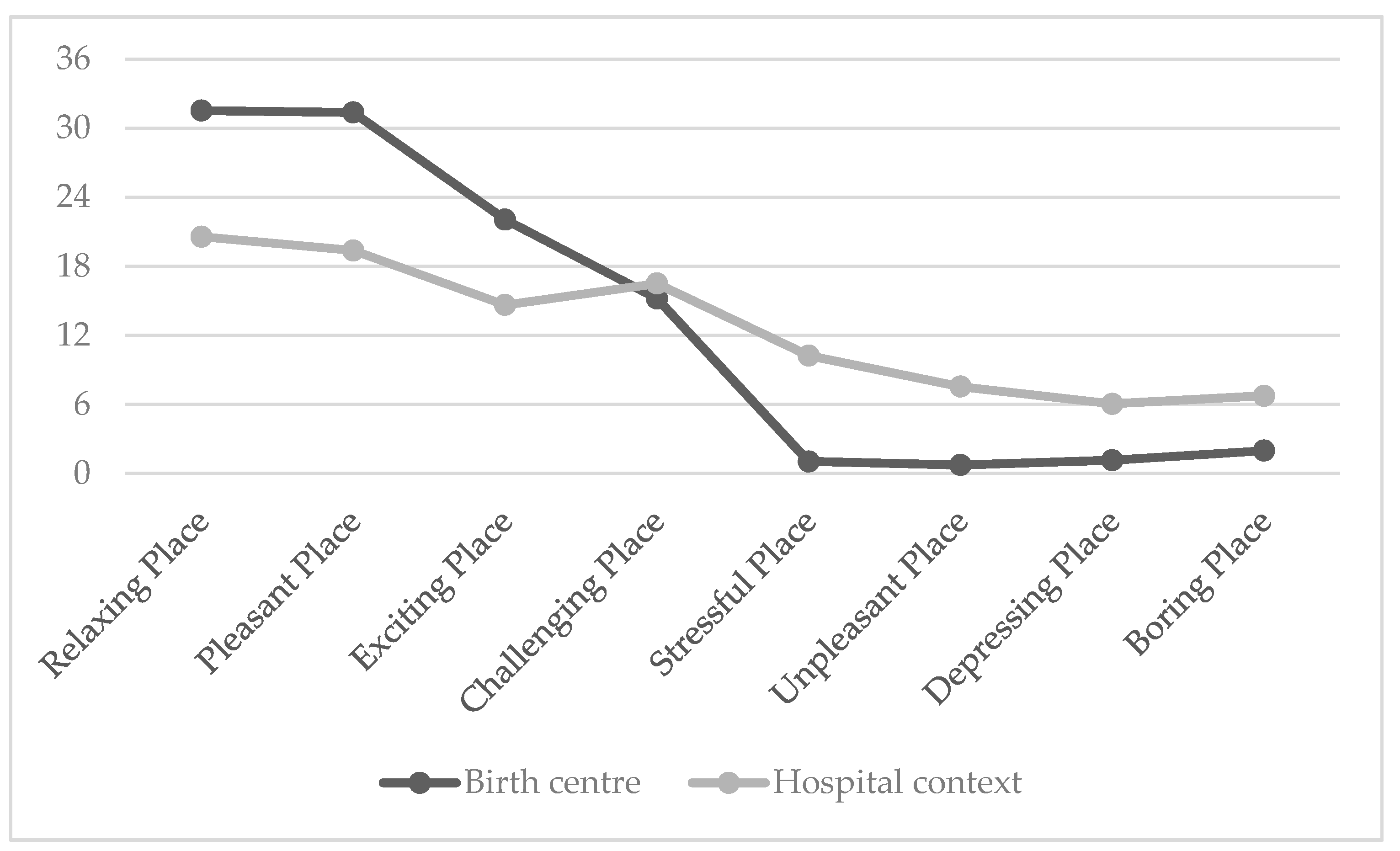
3.2. Mothers’ Perceptions
4. Discussion
5. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andrade, C.C.; Lima, M.L.; Devlin, A.S.; Hernández, B. Is it the place or the people? Disentangling the effects of hospitals’ physical and social environments on well-being. Environ. Behav. 2016, 48, 299–323. [Google Scholar] [CrossRef]
- Becker, F.D.; Sweeney, B.; Parsons, K. Ambulatory facility design and patients’ perceptions of healthcare quality. Health Environ. Res. Des. J. 2008, 1, 35–54. [Google Scholar] [CrossRef]
- Andrade, C.C.; Lima, M.L.; Pereira, C.R.; Fornara, F.; Bonaiuto, M. Inpatients’, and outpatients’ satisfaction: The mediating role of perceived quality of physical and social environment. Health Place 2013, 21, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S. Effects of interior design on wellness: Theory and recent scientific research. J. Health Care Inter. Des. 1991, 3, 97–109. [Google Scholar]
- Manca, S.; Bonaiuto, M.; Fornara, F. Perceived Hospital Environment Quality Indicators: The Case of Healthcare Places for Terminal Patients. Buildings 2023, 13, 57. [Google Scholar] [CrossRef]
- Bates, V. ‘Humanizing’ healthcare environments: Architecture, art and design in modern hospitals. Des. Health 2018, 2, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Sadek, A.H.; Willis, J. Ways to harness the built environment of ambulatory cancer facilities for comprehensive patient support: A review of the literature. Int. J. Nurs. Stud. 2020, 101, 103356. [Google Scholar] [CrossRef] [PubMed]
- Mandato, C.; Siano, M.A.; De Anseris, A.G.E.; Tripodi, M.; Massa, G.; De Rosa, R.; Buffoli, M.; Lamanna, A.; Siani, P.; Vajro, P. Humanization of care in pediatric wards: Differences between perceptions of users and staff according to department type. Riv. Ital. Pediatr. 2020, 46, 65. [Google Scholar] [CrossRef]
- Buriola, A.A.; Pinho, L.B.; Kantorski, L.P.; Matsuda, L.M. Assessment of the physical and human resource structure of a psychiatric emergency service. Avaliação da estrutura física e de recursos humanos de um serviço de emergência psiquiátrical. Texto E Contexto Enferm. 2017, 26, e3240016. [Google Scholar]
- Fornara, F.; Bonnes, M.; Bonaiuto, M. Indicatori di umanizzazione ospedaliera percepita: Un’analisi comparativa tra reparti di Chirurgia Generale. Psicol. Della Salut. 2012, 1, 39–60. [Google Scholar] [CrossRef]
- Jovanović, N.; Miglietta, E.; Podlesek, A.; Malekzadeh, A.; Lasalvia, A.; Campbell, J.; Priebe, S. Impact of the hospital built environment on treatment satisfaction of psychiatric in-patients. Psychol. Med. 2022, 52, 1969–1980. [Google Scholar] [CrossRef]
- Fleming, S.E.; Donovan-Batson, C.; Burduli, E.; Barbosa-Leiker, C.; Hollins Martin, C.J.; Martin, C.R. Birth Satisfaction Scale/Birth Satisfaction Scale-Revised (BSS/BSS-R): A large scale United States planned home birth and birth centre survey. Midwifery 2016, 41, 9–15. [Google Scholar] [CrossRef]
- Soet, J.E.; Brack, G.A.; Dilorio, C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth 2003, 30, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Kwee, J.L.; McBride, H.L. Working together for women’s empowerment: Strategies for interdisciplinary collaboration in perinatal care. J. Health Psychol. 2015, 21, 2742–2752. [Google Scholar] [CrossRef]
- Rink, E.; Anastario, M.; Reimer, G.A.; Peterson, M. An ecological approach to understanding Women’s reproductive health and pregnancy decision making in Greenland. Health Place 2022, 77, 102868. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S.; Zimring, C.; Barch, X.Z.; Dubose, J.; Seo, H.-B.; Choi, Y.-S.; Joseph, A. A review of the research literature on evidencebased healthcare design. HERD Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef] [PubMed]
- Jouhki, M.R.; Suominen, T.; Åstedt-Kurki, P. Giving birth on our own terms-Women’s experience of childbirth at home. Midwifery 2017, 53, 35–41. [Google Scholar] [CrossRef]
- Romoli, V.; Cardinali, P.; Ferrari, J.R.; Migliorini, L. Migrant perceptions of psychological home: A scoping review. Int. J. Intercult. Relat. 2022, 86, 14–25. [Google Scholar] [CrossRef]
- Hodnett, E.D.; Downe, S.; Walsh, D. Alternative versus conventional institutional settings for birth. Cochrane Database Syst. Rev. 2012, 8, CD000012. [Google Scholar] [CrossRef]
- Aburas, R.; Pati, D.; Casanova, R.; Adams, N.G. The Influence of nature stimulus in enhancing the birth experience. HERD Health Environ. Res. Des. J. 2017, 10, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Foureur, M.; Davis, D.; Fenwick, J.; Leap, N.; Iedema, R.; Forbes, I.; Homer, C. The relationship between birth unit design and safe, satisfying birth: Developing a hypotheticalmodel. Midwifery 2010, 26, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Mondy, T.; Fenwick, J.; Leap, N.; Foureur, M. How domesticity dictates behaviour in the birth space: Lessons for designing birth environments in institutions wanting to promote a positive experience of birth. Midwifery 2016, 43, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Menke, S.; Jenkinson, B.; Foureur, M.; Kildea, S. Is the Birthing Unit Design Spatial Evaluation Tool valid for diverse groups? Women Birth 2019, 32, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Setola, N.; Naldi, E.; Cardinali, P.; Migliorini, L. A Broad Study to Develop Maternity Units Design Knowledge Combining Spatial Analysis and Mothers’ and Midwives’ Perception of the Birth Environment. HERD Health Environ. Res. Des. J. 2022, 15, 204–232. [Google Scholar]
- Borrelli, S.; Walsh, D.; Spiby, H. First-time mothers’ choice of birthplace: Influencing factors, expectations of the midwife’s role and perceived safety. J. Adv. Nurs. 2017, 73, 1937–1946. [Google Scholar] [CrossRef]
- Holten, L.; de Miranda, E. Women’s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery 2016, 38, 55–62. [Google Scholar] [CrossRef]
- Hauck, Y.; Nathan, E.; Ball, C.; Hutchinson, M.; Somerville, S.; Hornbuckle, J.; Doherty, D. Women’s reasons and perceptions around planning a homebirth with a registered midwife in Western Australia. Women Birth 2018, 33, e39–e47. [Google Scholar] [CrossRef]
- Witteveen, A.B.; De Cock, P.; Huizink, A.C.; De Jonge, A.; Klomp, T.; Westerneng, M.; Geerts, C.C. Pregnancy related anxiety and general anxious or depressed mood and the choice for birth setting: A secondary data-analysis of the DELIVER study. BMC Pregnancy Childbirth 2016, 16, 363. [Google Scholar] [CrossRef]
- Gldkuhnl, L.; Dellenborg, L.; Berg, M.; Wijk, H.; Nilsson, C. The influence and meaning of the birth environment for nulliparous women at a hospital-based labour ward in Sweden: An ethnographic study. Women Birth 2022, 35, e337–e347. [Google Scholar] [CrossRef]
- AusHFG Part B. Health Facility Briefing and Planning HPU 510 Maternity Unit. 2017. Available online: https://www.healthfacilityguidelines.com.au/health-planning-units (accessed on 26 June 2021).
- Department of Health. Health Building Note 09-02: Maternity Care Facilities. 2013. Available online: https://www.gov.uk/government/publications/guidance-for-the-planning-and-design-ofmaternity-care-facilities (accessed on 27 July 2021).
- Aguilera-Martín, Á.; Gálvez-Lara, M.; Blanco-Ruiz, M.; García-Torres, F. Psychological, educational, and alternative interventions for reducing fear of childbirth in pregnant women: A systematic review. J. Clin. Psychol. 2021, 77, 525–555. [Google Scholar] [CrossRef]
- Hofberg, K.; Brockington, I. Tokophobia: An unreasoning dread of childbirth. A series of 26 cases. Br. J. Psychiatry 2000, 176, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Dencker, A.; Nilsson, C.; Begley, C.; Jangsten, E.; Mollberg, M.; Patel, H.; Wigert, H.; Hessman, E.; Sjöblom, H.; Sparud-Lundin, C. Causes and outcomes in studies of fear of childbirth: A systematic review. Women Birth 2019, 32, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Foureur, M.; Harte, J.D. Salutogenic Design for Birth. In Health and Well-Being for Interior Architecture; Kopec, D., Ed.; Taylor & Francis: New York, NY, USA, 2017; pp. 108–122. [Google Scholar]
- France, G.; Taroni, F.; Donatini, A. The Italian Health-Care System, Health Economics; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2005; Volume 14, pp. 187–202. [Google Scholar]
- Setola, N.; Iannuzzi, L.; Santini, M.; Cocina, G.G.; Naldi, E.; Branchini, L.; Morano, S.; Escuriet Peirò, R.; Downe, S. Optimal settings for childbirth. Minerva Ginecol. 2018, 70, 687–699. [Google Scholar] [CrossRef] [PubMed]
- Perun, M.B. Maternal identity of women in the postpartum period. J. Educ. Cult. Soc. 2020, 4, 95–105. [Google Scholar] [CrossRef]
- Mazzoni, G. Psicologia Della Testimonianza; Carocci Editore: Roma, Italy, 2011. [Google Scholar]
- Russell, J.A.; Ward, L.; Pratt, G. A description of the affective quality attributed to environments. J. Pers. Soc. Psychol. 1980, 38, 311–322. [Google Scholar] [CrossRef]
- Perugini, M.; Bonnes, M.; Aiello, A.; Ercolani, A.P. Il modello circonflesso delle qualità affettive dei luoghi: Sviluppo di uno strumento valutativo italiano. TPM-Test. Psychom. Methodol. 2002, 9, 131–152. [Google Scholar]
- Fenaroli, V.; Saita, E. Fear of childbirth: A contribution to the validation of the Italian version of the Wijma Delivery Expectancy/Experience Questionnaire (WDEQ). TPM-Test. Psychom. Methodol. 2013, 20, 131–154. [Google Scholar]
- Setola, N.; Naldi, E.; Cocina, G.G.; Eide, L.B.; Iannuzzi, L.; Daly, D. The Impact of the Physical Environment on Intrapartum Maternity Care: Identification of Eight Crucial Building Spaces. HERD Health Environ. Res. Des. J. 2019, 12, 67–98. [Google Scholar] [CrossRef]
- Nilsson, C.; Wijk, H.; Höglund, L.; Sjöblom, H.; Hessman, E.; Berg, M. Effects of birthing room design on maternal and neonate outcomes: A systematic review. HERD Health Environ. Res. Des. J. 2020, 13, 198–214. [Google Scholar] [CrossRef]
- Cho, M. Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 1540. [Google Scholar] [CrossRef]
- Rashid, M.; Zimring, C. A review of the empirical literature on the relationships between indoor environment and stress in health care and office settings: Problems and prospects of sharing evidence. Environ. Behav. 2008, 40, 151–190. [Google Scholar] [CrossRef]
- Gharaveis, A.; Hamilton, D.K.; Pati, D. The impact of environmental design on teamwork and communication in healthcarefacilities: A systematic literature review. Health Environ. Res. Des. J. 2018, 11, 119–137. [Google Scholar]
- McBain, K.A. Adult Attachment Theory and Attachment to Place: Exploring Relationships between People and Places. Ph.D. Thesis, James Cook University, Douglas, QLD, Australia, 2010. [Google Scholar]
- Low, S.M.; Altman, I. Place attachment. In Place Attachment; Springer: Boston, MA, USA, 1992; pp. 1–12. [Google Scholar]
- Wood, R.J.; Mignone, J.; Heaman, M.I.; Robinson, K.J.; Roger, K.S. Choosing an out-of-hospital birth centre: Exploring women’s decision-making experiences. Midwifery 2016, 39, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Schaming, C.; Wendland, J. Postnatal mental health during the COVID-19 pandemic: Impact on mothers’ postnatal sense of security and on mother-to-infant bonding. Midwifery 2023, 117, 103557. [Google Scholar] [CrossRef]
- Ahmad Tajudin, N.F.S.; Che Amat, R. The COVID-19 Pandemic: Impacts on the Hospital Environment and Spatial Design. Int. J. Built Environ. Sustain. 2022, 9, 5–14. [Google Scholar] [CrossRef]


| Indicators | Setting | N | Mean | SD | Student’s t | Sig. |
|---|---|---|---|---|---|---|
| Building aesthetics (Alpha 0.88) | Hospital | 30 | 4.04 | 0.80 | ||
| BC | 36 | 4.62 | 0.59 | 3.35 | 0.001 | |
| Acustic comfort (Alpha 0.82) | Hospital | 30 | 3.75 | 1.27 | ||
| BC | 36 | 4.55 | 0.71 | 3.09 | 0.003 | |
| Climate comfort (Alpha 0.83) | Hospital | 30 | 3.52 | 1.07 | ||
| BC | 36 | 3.65 | 1.09 | 0.51 | 0.612 | |
| Care for waiting or meeting rooms (Alpha 0.86) | Hospital | 30 | 2.38 | 0.88 | ||
| BC | 36 | 4.38 | 0.80 | 9.65 | 0.000 | |
| Views (Alpha 0.69) | Hospital | 30 | 2.22 | 0.68 | ||
| BC | 36 | 2.67 | 1.22 | 1.86 | 0.068 | |
| Orientation and reception (Alpha 0.87) | Hospital | 30 | 3.40 | 1.11 | ||
| BC | 36 | 4.30 | 0.80 | 3.74 | 0.000 | |
| Organisation clarity (Alpha 0.88) | Hospital | 30 | 3.48 | 1.06 | ||
| BC | 36 | 4.54 | 0.66 | 4.76 | 0.000 | |
| Privacy (Alpha 0.45) | Hospital | 30 | 4.52 | 0.67 | ||
| BC | 36 | 4.81 | 0.39 | 2.11 | 0.041 | |
| Availability and professionalism of operators (Alpha 0.85) | Hospital | 30 | 3.91 | 0.67 | ||
| BC | 36 | 4.80 | 0.32 | 4.85 | 0.000 | |
| Spatial physical aspects of the care unit (includes first six dimensions) | Hospital | 30 | 3.22 | 0.57 | ||
| BC | 36 | 4.03 | 0.60 | 5.55 | 0.000 | |
| Social and functional aspects of the care unit (includes last three dimensions) | Hospital | 30 | 3.97 | 0.74 | ||
| BC | 36 | 4.72 | 0.35185 | 5.05 | 0.000 |
| Group | N | Mean | SD | Student’s t | p | |
|---|---|---|---|---|---|---|
| Low Self efficacy (Alpha 0.86) | Hospital | 30 | 31.17 | 5.97 | −3.50 | 0.001 |
| Birth Center | 36 | 25.44 | 7.34 | |||
| Loneliness (Alpha 0.79) | Hospital | 30 | 21.53 | 5.21 | −4.52 | <0.001 |
| Birth Center | 36 | 15.22 | 5.98 | |||
| Negative appraisal (Alpha 0.72) | Hospital | 30 | 12.17 | 3.51 | −1.99 | 0.095 |
| Birth Center | 36 | 10.56 | 4.10 | |||
| Lack of positive anticipation (Alpha 0.45) | Hospital | 30 | 10.83 | 3.14 | −3.37 | 0.001 |
| Birth Center | 36 | 8.25 | 3.07 | |||
| Fear (Alpha 0.67) | Hospital | 30 | 16.10 | 3.56 | −4.07 | <0.001 |
| Birth Center | 36 | 12.42 | 3.74 | |||
| Concern for the baby (Alpha 0.72) | Hospital | 30 | 4.37 | 2.30 | −2.84 | 0.006 |
| Birth Center | 36 | 3.00 | 1.60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migliorini, L.; Setola, N.; Naldi, E.; Rompianesi, M.C.; Iannuzzi, L.; Cardinali, P. Exploring the Role of Birth Environment on Italian Mothers’ Emotional Experience during Childbirth. Int. J. Environ. Res. Public Health 2023, 20, 6529. https://doi.org/10.3390/ijerph20156529
Migliorini L, Setola N, Naldi E, Rompianesi MC, Iannuzzi L, Cardinali P. Exploring the Role of Birth Environment on Italian Mothers’ Emotional Experience during Childbirth. International Journal of Environmental Research and Public Health. 2023; 20(15):6529. https://doi.org/10.3390/ijerph20156529
Chicago/Turabian StyleMigliorini, Laura, Nicoletta Setola, Eletta Naldi, Maria Chiara Rompianesi, Laura Iannuzzi, and Paola Cardinali. 2023. "Exploring the Role of Birth Environment on Italian Mothers’ Emotional Experience during Childbirth" International Journal of Environmental Research and Public Health 20, no. 15: 6529. https://doi.org/10.3390/ijerph20156529
APA StyleMigliorini, L., Setola, N., Naldi, E., Rompianesi, M. C., Iannuzzi, L., & Cardinali, P. (2023). Exploring the Role of Birth Environment on Italian Mothers’ Emotional Experience during Childbirth. International Journal of Environmental Research and Public Health, 20(15), 6529. https://doi.org/10.3390/ijerph20156529










