Occupational COVID-19 Exposures and Illnesses among Workers in California—Analysis of a New Occupational COVID-19 Surveillance System
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Variables
2.2.1. Demographic Variables
2.2.2. Work-Related Variables
2.2.3. Exposure-Related Variables
2.2.4. Health Outcome Variables
2.3. Statistical Methods
3. Results
3.1. Worker Demographics
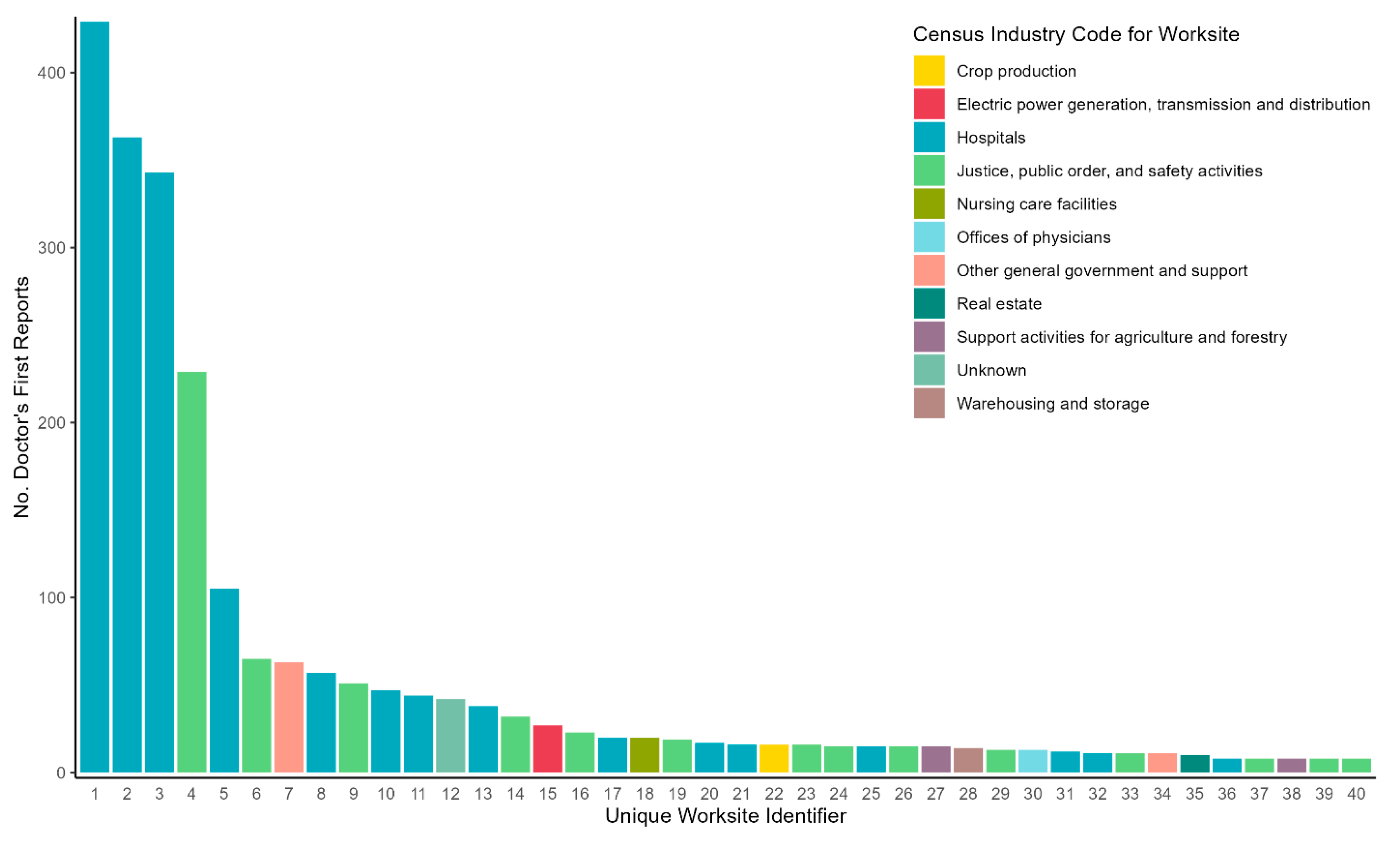
3.2. Reporting Rates
3.3. Reported Exposures
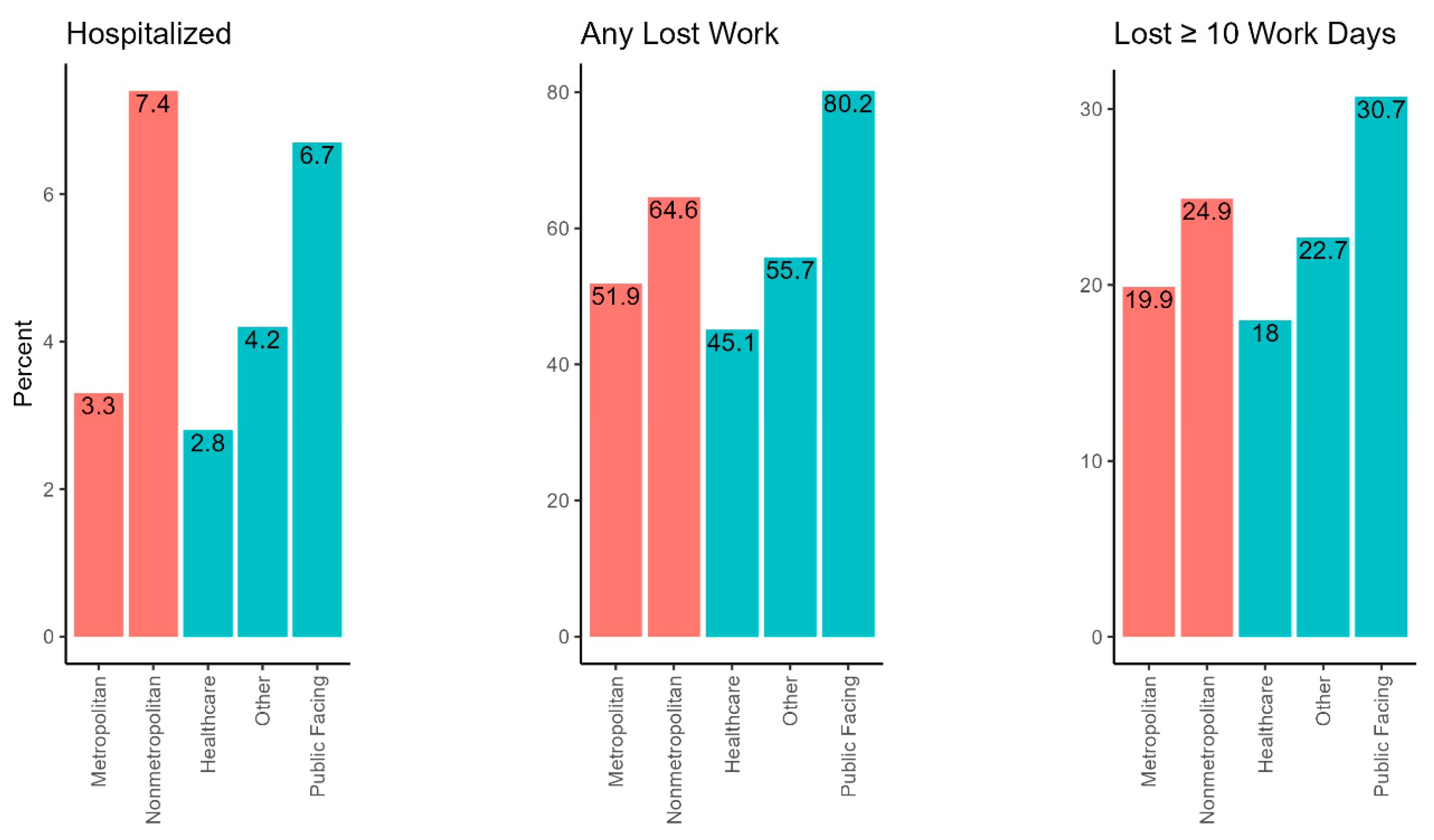
3.4. Reported Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Disclaimer
References
- McMichael, T.M.; Clark, S.; Pogosjans, S.; Kay, M.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; Ferro, J.; Brostrom-Smith, C.; et al. COVID-19 in a Long-Term Care Facility—King County, Washington, February 27–March 9, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Dyal, J.W.; Grant, M.P.; Broadwater, K.; Bjork, A.; Waltenburg, M.A.; Gibbins, J.D.; Hale, C.; Silver, M.; Fischer, M.; Steinberg, J.; et al. COVID-19 among Workers in Meat and Poultry Processing Facilities—19 States, April 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Bui, D.P.; McCaffrey, K.; Friedrichs, M.; LaCross, N.; Lewis, N.M.; Sage, K.; Barbeau, B.; Vilven, D.; Rose, C.; Braby, S.; et al. Racial and Ethnic Disparities Among COVID-19 Cases in Workplace Outbreaks by Industry Sector—Utah, March 6-June 5, 2020. MMWR Morb. Mortal. Wkly. 2020, 69, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Heinzerling, A.; Stuckey, M.J.; Scheuer, T.; Xu, K.; Perkins, K.M.; Resseger, H.; Magill, S.; Verani, J.R.; Jain, S.; Acosta, M.; et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient—Solano County, California, February 2020. MMWR Morb. Mortal. Wkly. 2020, 69, 472–476. [Google Scholar] [CrossRef]
- Heinzerling, A.; Nguyen, A.; Frederick, M.; Chan, E.; Gibb, K.; Rodriguez, A.; Wong, J.; Epson, E.; Watt, J.; Materna, B.; et al. Workplaces Most Affected by COVID-19 Outbreaks in California, January 2020–August 2021. Am. J. Public Health 2022, 112, 1180–1190. [Google Scholar] [CrossRef]
- Contreras, Z.; Ngo, V.; Pulido, M.; Washburn, F.; Meschyan, G.; Gluck, F.; Kuguru, K.; Reporter, R.; Curley, C.; Civen, R.; et al. Industry Sectors Highly Affected by Worksite Outbreaks of Coronavirus Disease, Los Angeles County, California, USA, March 19-September 30, 2020. Emerg. Infect. Dis. 2021, 27, 1769–1775. [Google Scholar] [CrossRef]
- Cummings, K.J.; Materna, B.L.; Vergara, X.; Beckman, J.; Espineli, C.; Harrison, R. COVID-19 in the Workplace: The View from California. Ann. Am. Thorac. Soc. 2022, 19, 1260–1264. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Riley, A.R.; A Duchowny, K.; E Aschmann, H.; Chen, R.; Kiang, M.V.; Mooney, A.C.; Stokes, A.C.; Glymour, M.M.; Bibbins-Domingo, K. COVID-19 mortality and excess mortality among working-age residents in California, USA, by occupational sector: A longitudinal cohort analysis of mortality surveillance data. Lancet Public Health 2022, 7, e744–e753. [Google Scholar] [CrossRef]
- Cummings, K.J.; Beckman, J.; Frederick, M.; Harrison, R.; Nguyen, A.; Snyder, R.; Chan, E.; Gibb, K.; Rodriguez, A.; Wong, J.; et al. Disparities in COVID-19 fatalities among working Californians. PLoS ONE 2022, 17, e0266058. [Google Scholar] [CrossRef]
- Asfaw, A. Cost of lost work hours associated with the COVID-19 pandemic-United States, March 2020 through February 2021. Am. J. Ind. Med. 2021, 65, 20–29. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Wiley, J.F.; Czeisler, C.A.; Howard, M.E.; Rajaratnam, S.M.W. Follow-up Survey of US Adult Reports of Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic, September 2020. JAMA Network Open 2021, 4, e2037665. [Google Scholar] [CrossRef] [PubMed]
- Burns, A. What Are the Implications of Long COVID for Employment and Health Coverage? Kaiser Family Foundation: San Francisco, CA, USA, 2022; Available online: https://www.kff.org/policy-watch/what-are-the-implications-of-long-covid-for-employment-and-health-coverage/ (accessed on 6 October 2022).
- Gibb, K.; Bui, D.P.; Vergara, X.P. Increases in Prevalent Depressed Mood and Suicidal Ideation among Workers during the COVID-19 Pandemic—Findings from the California Health Interview Survey. Int. J. Environ. Res. Public Health 2023, 20, 1253. [Google Scholar] [CrossRef]
- Pray, I.W.; Grajewski, B.; Morris, C.; Modji, K.; DeJonge, P.; McCoy, K.; Tomasallo, C.; DeSalvo, T.; Westergaard, R.P.; Meimanet, J. Measuring Work-related Risk of Coronavirus Disease 2019 (COVID-19): Comparison of COVID-19 Incidence by Occupation and Industry—Wisconsin, September 2020 to May 2021. Clin. Infect. Dis. 2022, 76, e163–e171. [Google Scholar] [CrossRef] [PubMed]
- Luckhaupt, S.B.S.; de Perio, M.; Haring Sweeney, M. NIOSH Science Blog [Internet]. Prevention CfDCa, editor: Centers for Disease Control and Prevention. 2020. Available online: https://blogs.cdc.gov/niosh-science-blog/2020/06/11/covid-surveillance/ (accessed on 6 October 2022).
- Ullrich, F.; Mueller, K. COVID-19 Cases and Deaths, Metropolitan and Nonmetropolitan Counties over Time (Update); RUPRI Center for Rural Health Policy Analysis: Iowa City, IA, USA, 2021. [Google Scholar]
- Hirko, K.A.; Kerver, J.M.; Ford, S.; Szafranski, C.; Beckett, J.; Kitchen, C.; Wendling, A.L. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J. Am. Med. Inform. Assoc. 2020, 27, 1816–1818. [Google Scholar] [CrossRef]
- Rader, B.; Astley, C.M.; Sewalk, K.; Delamater, P.L.; Cordiano, K.; Wronski, L.; Rivera, J.M.; Hallberg, K.; Pera, M.F.; Cantor, J.; et al. Spatial modeling of vaccine deserts as barriers to controlling SARS-CoV-2. Commun. Med. 2022, 2, 141. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.T.; McConnell, K.; Burow, P.B.; Pofahl, K.; Merdjanoff, A.A.; Farrell, J. Impacts of the COVID-19 pandemic on rural America. Am. Proc. Natl. Acad. Sci. USA 2021, 118, 2019378118. [Google Scholar] [CrossRef]
- Berkov, B.M.; Kleinman, G.D.; Powers, J.E.; Trasko, V.M. Evaluation of Occupational Disease Reporting in California. J. Occup. Med. 1961, 3, 449–456. [Google Scholar]
- Reinisch, F.; Harrison, R.J.; Cussler, S.; Athanasoulis, M.; Balmes, J.; Blanc, P.; Cone, J. Physician reports of work-related asthma in California, 1993-1996. Am. J. Ind. Med. 2001, 39, 72–83. [Google Scholar] [CrossRef]
- Vergara, X.; Espineli, C.; Martysh, E.; Gibb, K.; Wong, J.; Andrea, R.; Cummings, K.J. Workplace SARS-CoV-2 Exposure and COVID-19 Illness—Birth of a New California Surveillance System [abstract]. In Proceedings of the CSTE 2021 Annual Conference, Virtual, 13–17 June 2021. [Google Scholar]
- State of California Department of Industrial Relations Division of Workers’ Compensation. Physician’s Guide to Medical Practice in the California Workers’ Compensation System, 4th ed.; Relations DoI, Ed.; Department of Industrial Relations: San Francisco, CA, USA, 2016.
- US Department of Agriculture. Rural-Urban Commuting Area Codes; USDA: Washington, DC, USA, 2020. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed on 26 September 2022).
- Occupational Health Subcommittee Epidemiological Classification of COVID-19 Work-Relatedness and Documentation of Public-Facing Occupations [Internet]. Council of State and Territorial Epidemiologists. 2022. Available online: https://www.cste.org/resource/resmgr/occupationalhealth/publications/OH_docs_update12122.zip (accessed on 26 September 2022).
- United States Census Bureau. Current Population Survey. Available online: https://www.census.gov/programs-surveys/cps.html (accessed on 28 November 2022).
- Sarah Flood, M.K.; Rodgers, R.; Ruggles, S.; Robert Warren, J.; Westberry, M. Integrated Public Use Microdata Series, Current Population Survey: Version 10.0 [Dataset]. Minneapolis, MN, USA, 2022. Available online: https://cps.ipums.org/cps/ (accessed on 13 December 2022).
- Heinzerling, A.; Vergara, X.P.; Gebreegziabher, E.; Beckman, J.; Wong, J.; Nguyen, A.; Khan, S.; Frederick, M.; Bui, D.; Chan, E.; et al. COVID-19 Outbreaks and Mortality among Public Transportation Workers—California, January 2020-May 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1052–1056. [Google Scholar] [CrossRef]
- Azaroff, L.S.; Levenstein, C.; Wegman, D.H. Occupational injury and illness surveillance: Conceptual filters explain underreporting. Am. J. Public Health 2002, 92, 1421–1429. [Google Scholar] [CrossRef]
- Quigley, D.D.; Dworsky, M.; Qureshi, N.; Prier, S.; Gidengil, C.A. COVID-19 in the California Workers’ Compensation System: A Study of COVID-19 Claims and Presumptions Under Senate Bill 1159; RAND Corporation: Santa Monica, CA, USA, 2021. [Google Scholar]
- Curtin, S.C.; Heron, M. COVID-19 Death Rates in Urban and Rural Areas: United States, 2020. NCHS Data Brief. 2022, 447, 1–8. [Google Scholar]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020-April 10, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Anzalone, A.J.; Horswell, R.; Hendricks, B.M.; Chu, S.; Hillegass, W.B.; Beasley, W.H.; Harper, J.R.; Kimble, W.; Rosen, C.J.; Miele, L.; et al. Higher hospitalization and mortality rates among SARS-CoV-2-infected persons in rural America. J. Rural. Health 2023, 39, 39–54. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Monnat, S.M. Rural-urban and within-rural differences in COVID-19 vaccination rates. J. Rural. Health 2022, 38, 916–922. [Google Scholar] [CrossRef]
- Thomson, M.D.; Mariani, A.C.; Williams, A.R.; Sutton, A.L.; Sheppard, V.B. Factors Associated With Use of and Satisfaction With Telehealth by Adults in Rural Virginia During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2119530. [Google Scholar] [CrossRef]
- Laskaris, Z.; Hirschtick, J.L.; Xie, Y.; McKane, P.; Fleischer, N.L. COVID-19 in the workplace: Self-reported source of exposure and availability of personal protective equipment by industry and occupation in Michigan. Am. J. Ind. Med. 2022, 65, 994–1005. [Google Scholar] [CrossRef]
- Zabarsky, T.F.; Bhullar, D.; Silva, S.Y.; Mana, T.S.C.; Ertle, M.T.; Navas, M.E.; Donskey, C.J. What are the sources of exposure in healthcare personnel with coronavirus disease 2019 infection? Am. J. Infect. Control 2021, 49, 392–395. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. 12 COVID-19 Vaccination Strategies for Your Community Atlanta, GA2022. Available online: https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/community.html (accessed on 12 January 2023).
- Occupational Safety and Health Administration. Protecting Workers: Guidance on Mitigating and Preventing the Spread of COVID-19 in the Workplace; United States Department of Labor: Washington DC, USA, 2022. Available online: https://www.osha.gov/coronavirus/safework (accessed on 12 January 2023).

| All Workers N (%) | Rural–Urban Commuting Area | Worker Group Assignment | ||||
|---|---|---|---|---|---|---|
| Metropolitan N (%) | Nonmetropolitan N (%) | Public Facing N (%) | Healthcare N (%) | Other N (%) | ||
| N | 2848 | 2548 | 189 | 697 | 1192 | 406 |
| Age, median (IQR) | 42 (32, 51) | 42 (32, 51) | 42 (32, 51.25) | 42 (33, 49) | 40.5 (32, 53) | 44 (35, 54) |
| Sex | ||||||
| Male | 1281 (44.98) | 1103 (43.29) | 125 (66.14) | 507 (72.74) | 335 (28.1) | 177 (43.6) |
| Female | 1453 (51.02) | 1340 (52.59) | 63 (33.33) | 190 (27.26) | 848 (71.14) | 228 (56.16) |
| Unknown | 114 (4) | ꝉ | ꝉ | – | ꝉ | ꝉ |
| Rural–Urban Commuting Area | ||||||
| Metropolitan | 2548 (89.47) | 2548 (100) | – | 566 (81.21) | 1125 (94.38) | 376 (92.61) |
| Nonmetropolitan | 189 (6.64) | – | 189 (100) | 86 (12.34) | 32 (2.68) | 22 (5.42) |
| Unknown | 111 (3.9) | – | – | 45 (6.46) | 35 (2.94) | 8 (1.97) |
| Worker Group Assignment | ||||||
| Public Facing Occupation | 697 (24.47) | 566 (22.21) | 86 (45.5) | 697 (100) | – | – |
| Healthcare Occupation | 1192 (41.85) | 1125 (44.15) | 32 (16.93) | – | 1192 (100) | – |
| Other Occupations | 406 (14.26) | 376 (14.76) | 22 (11.64) | – | – | 406 (100) |
| Unknown | 553 (19.42) | 481 (18.88) | 49 (25.93) | – | – | – |
| Occupation Group * | ||||||
| Architecture and Engineering | 6 (0.21) | 6 (0.24) | – | – | – | 6 (1.48) |
| Building and Grounds Cleaning and Maint. | 55 (1.93) | ꝉ | ꝉ | – | – | 55 (13.55) |
| Business and Financial Operations | 17 (0.6) | ꝉ | ꝉ | ꝉ | – | ꝉ |
| Community and Social Service | 25 (0.88) | ꝉ | ꝉ | 25 (3.59) | – | – |
| Construction and Extraction | 23 (0.81) | ꝉ | ꝉ | – | – | 23 (5.67) |
| Education, Training, and Library | 20 (0.7) | 14 (0.55) | 5 (2.65) | 20 (2.87) | – | – |
| Farming, Fishing, and Forestry | 23 (0.81) | 17 (0.67) | 5 (2.65) | – | – | 23 (5.67) |
| Food Preparation and Serving Related | 31 (1.09) | 23 (0.9) | 6 (3.17) | 18 (2.58) | – | 13 (3.2) |
| Healthcare Practitioners and Technical | 914 (32.09) | 864 (33.91) | 23 (12.17) | – | 914 (76.68) | – |
| Healthcare Support | 242 (8.5) | 226 (8.87) | 8 (4.23) | – | 242 (20.3) | – |
| Installation, Maintenance, and Repair | 30 (1.05) | ꝉ | ꝉ | – | – | 30 (7.39) |
| Management | 56 (1.97) | ꝉ | ꝉ | 5 (0.72) | 36 (3.02) | 15 (3.69) |
| Office and Administrative Support | 189 (6.64) | 175 (6.87) | 10 (5.29) | 17 (2.44) | – | 172 (42.36) |
| Personal Care and Service | 10 (0.35) | 10 (0.39) | – | 10 (1.43) | – | – |
| Production | 28 (0.98) | ꝉ | ꝉ | – | – | 28 (6.9) |
| Protective Service | 591 (20.75) | 482 (18.92) | 69 (36.51) | 588 (84.36) | – | ꝉ |
| Sales and Related | 9 (0.32) | ꝉ | ꝉ | 6 (0.86) | – | ꝉ |
| Transportation and Material Moving | 19 (0.67) | ꝉ | ꝉ | ꝉ | – | 15 (3.69) |
| Unknown | 552 (19.38) | 480 (18.84) | 49 (25.93) | – | – | – |
| Industry Group * | ||||||
| Accommodation and Food Services | 17 (0.6) | ꝉ | ꝉ | ꝉ | – | 8 (1.97) |
| Administrative and Support and Waste Mgmt. | 33 (1.16) | 33 (1.3) | – | ꝉ | ꝉ | 12 (2.96) |
| Agriculture, Forestry, Fishing, and Hunting | 83 (2.91) | 62 (2.43) | 18 (9.52) | 30 (4.3) | – | 28 (6.9) |
| Construction | 8 (0.28) | ꝉ | – | – | – | ꝉ |
| Educational Services | 42 (1.47) | 28 (1.1) | 11 (5.82) | 27 (3.87) | – | 11 (2.71) |
| Healthcare and Social Assistance | 1693 (59.45) | 1606 (63.03) | 43 (22.75) | 55 (7.89) | 1141 (95.72) | 203 (50) |
| Manufacturing | 16 (0.56) | ꝉ | ꝉ | – | – | 5 (1.23) |
| Other Services, Except Public Administration | 7 (0.25) | 7 (0.27) | – | – | – | ꝉ |
| Public Administration | 778 (27.32) | 642 (25.2) | 90 (47.62) | 558 (80.06) | 45 (3.78) | 60 (14.78) |
| Real Estate and Rental and Leasing | 16 (0.56) | 16 (0.63) | – | – | – | ꝉ |
| Retail Trade | 20 (0.7) | ꝉ | ꝉ | 5 (0.72) | – | 9 (2.22) |
| Transportation and Warehousing | 25 (0.88) | ꝉ | ꝉ | ꝉ | – | 15 (3.69) |
| Utilities | 49 (1.72) | ꝉ | ꝉ | – | ꝉ | 37 (9.11) |
| Unknown | 44 (1.54) | 18 (0.71) | 15 (7.94) | 9 (1.29) | ꝉ | ꝉ |
| Rural–Urban Commuting Area | Worker Group Assignment | |||||
|---|---|---|---|---|---|---|
| All Workers N (%) | Metropolitan N (%) | Nonmetropolitan N (%) | Public Facing N (%) | Healthcare N (%) | Other N (%) | |
| N | 2848 | 2548 | 189 | 697 | 1192 | 406 |
| Exposures | ||||||
| Suspected Source | ||||||
| Patient | 540 (18.96) | 516 (20.25) | 11 (5.82) | 36 (5.16) | 427 (35.82) | 51 (12.56) |
| Client/Customer | 240 (8.43) | 208 (8.16) | 10 (5.29) | 152 (21.81) | 63 (5.29) | 14 (3.45) |
| Coworker | 324 (11.38) | 284 (11.15) | 29 (15.34) | 132 (18.94) | 66 (5.54) | 81 (19.95) |
| Personal | 50 (1.76) | 46 (1.81) | ꝉ | 8 (1.15) | 24 (2.01) | 11 (2.71) |
| Not Stated | 1739 (61.06) | 1534 (60.2) | 139 (73.54) | 400 (57.39) | 627 (52.6) | 247 (60.84) |
| Unknown to Patient | 46 (1.62) | 43 (1.69) | ꝉ | 10 (1.43) | 18 (1.51) | 12 (2.96) |
| Exposure Site/Worksite * | ||||||
| Institution | 2249 (78.97) | 2040 (80.06) | 121 (64.02) | 459 (65.85) | 1177 (98.74) | 239 (58.87) |
| Commercial Facility, Non-Mfg. | 90 (3.16) | 83 (3.26) | 5 (2.65) | 13 (1.87) | – | 52 (12.81) |
| Other | 56 (1.97) | 46 (1.81) | 8 (4.23) | 30 (4.3) | 2 (0.17) | 14 (3.45) |
| Agricultural | 23 (0.81) | 17 (0.67) | 5 (2.65) | 2 (0.29) | – | 14 (3.45) |
| Manufacturing | 13 (0.46) | 13 (0.51) | – | 1 (0.14) | – | 6 (1.48) |
| More than One Site | 5 (0.18) | ꝉ | ꝉ | 2 (0.29) | 3 (0.25) | – |
| Unknown | 411 (14.43) | 344 (13.5) | 49 (25.93) | 189 (27.12) | 10 (0.84) | 81 (19.95) |
| Type of Care for DFR | ||||||
| Doctor’s Office | 1036 (36.38) | 858 (33.67) | 118 (62.43) | 333 (47.78) | 326 (27.35) | 135 (33.25) |
| Emergency Department | 530 (18.61) | 513 (20.13) | 12 (6.35) | 34 (4.88) | 286 (23.99) | 90 (22.17) |
| Hospital Admission | 8 (0.28) | 8 (0.31) | – | 4 (0.57) | 3 (0.25) | – |
| No Medical Care Sought | 8 (0.28) | 8 (0.31) | – | 6 (0.86) | – | 2 (0.49) |
| Employee Health Center | 188 (6.6) | 175 (6.87) | 10 (5.29) | 6 (0.86) | 133 (11.16) | 22 (5.42) |
| Telemedicine | 995 (34.94) | 916 (35.95) | 39 (20.63) | 297 (42.61) | 423 (35.49) | 141 (34.73) |
| Unknown | 83 (2.91) | 70 (2.75) | 10 (5.29) | 17 (2.44) | 21 (1.76) | 16 (3.94) |
| Outcomes | ||||||
| Any Symptoms | ||||||
| Yes | 1932 (67.84) | 1727 (67.78) | 118 (62.43) | 516 (74.03) | 802 (67.28) | 281 (69.21) |
| None Reported | 916 (32.16) | 821 (32.22) | 71 (37.57) | 181 (25.97) | 390 (32.72) | 125 (30.79) |
| Hospitalized ** | ||||||
| Yes | 110 (3.86) | 85 (3.34) | 14 (7.41) | 47 (6.74) | 33 (2.77) | 17 (4.19) |
| No | 2738 (96.14) | 2463 (96.66) | 175 (92.59) | 650 (93.26) | 1159 (97.23) | 389 (95.81) |
| Lost Work | ||||||
| Yes | 1525 (53.55) | 1322 (51.88) | 122 (64.55) | 559 (80.2) | 538 (45.13) | 226 (55.67) |
| No | 338 (11.87) | 312 (12.24) | 17 (8.99) | 38 (5.45) | 226 (18.96) | 62 (15.27) |
| Unknown | 985 (34.59) | 914 (35.87) | 50 (26.46) | 100 (14.35) | 428 (35.91) | 118 (29.06) |
| Lost Work Reason | ||||||
| Due to Illness/Symptoms | 1365 (47.93) | 1181 (46.35) | 109 (57.67) | 491 (70.44) | 469 (39.35) | 209 (51.48) |
| Quarantine or Asymptomatic *** | 160 (5.62) | 141 (5.53) | 13 (6.88) | 68 (9.76) | 69 (5.79) | 17 (4.19) |
| No Lost Time | 338 (11.87) | 312 (12.24) | 17 (8.99) | 38 (5.45) | 226 (18.96) | 62 (15.27) |
| Unknown | 985 (34.59) | 914 (35.87) | 50 (26.46) | 100 (14.35) | 428 (35.91) | 118 (29.06) |
| Lost Time Amount **** | ||||||
| <10 days | 472 (16.57) | 418 (16.41) | 29 (15.34) | 219 (31.42) | 139 (11.66) | 56 (13.79) |
| ≥10 days | 592 (20.79) | 507 (19.9) | 47 (24.87) | 214 (30.7) | 215 (18.04) | 92 (22.66) |
| Lost Work but Unknown Amount | 461 (16.19) | 397 (15.58) | 46 (24.34) | 126 (18.08) | 184 (15.44) | 78 (19.21) |
| Unknown | 985 (34.59) | 914 (35.87) | 50 (26.46) | 100 (14.35) | 428 (35.91) | 118 (29.06) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bui, D.P.; Gibb, K.; Fiellin, M.; Rodriguez, A.; Majka, C.; Espineli, C.; Gebreegziabher, E.; Flattery, J.; Vergara, X.P. Occupational COVID-19 Exposures and Illnesses among Workers in California—Analysis of a New Occupational COVID-19 Surveillance System. Int. J. Environ. Res. Public Health 2023, 20, 6307. https://doi.org/10.3390/ijerph20136307
Bui DP, Gibb K, Fiellin M, Rodriguez A, Majka C, Espineli C, Gebreegziabher E, Flattery J, Vergara XP. Occupational COVID-19 Exposures and Illnesses among Workers in California—Analysis of a New Occupational COVID-19 Surveillance System. International Journal of Environmental Research and Public Health. 2023; 20(13):6307. https://doi.org/10.3390/ijerph20136307
Chicago/Turabian StyleBui, David Pham, Kathryn Gibb, Martha Fiellin, Andrea Rodriguez, Claire Majka, Carolina Espineli, Elisabeth Gebreegziabher, Jennifer Flattery, and Ximena P. Vergara. 2023. "Occupational COVID-19 Exposures and Illnesses among Workers in California—Analysis of a New Occupational COVID-19 Surveillance System" International Journal of Environmental Research and Public Health 20, no. 13: 6307. https://doi.org/10.3390/ijerph20136307
APA StyleBui, D. P., Gibb, K., Fiellin, M., Rodriguez, A., Majka, C., Espineli, C., Gebreegziabher, E., Flattery, J., & Vergara, X. P. (2023). Occupational COVID-19 Exposures and Illnesses among Workers in California—Analysis of a New Occupational COVID-19 Surveillance System. International Journal of Environmental Research and Public Health, 20(13), 6307. https://doi.org/10.3390/ijerph20136307






