Best Practices for Notification of Unexpected, Violent, and Traumatic Death: A Scoping Review
Abstract
1. Introduction
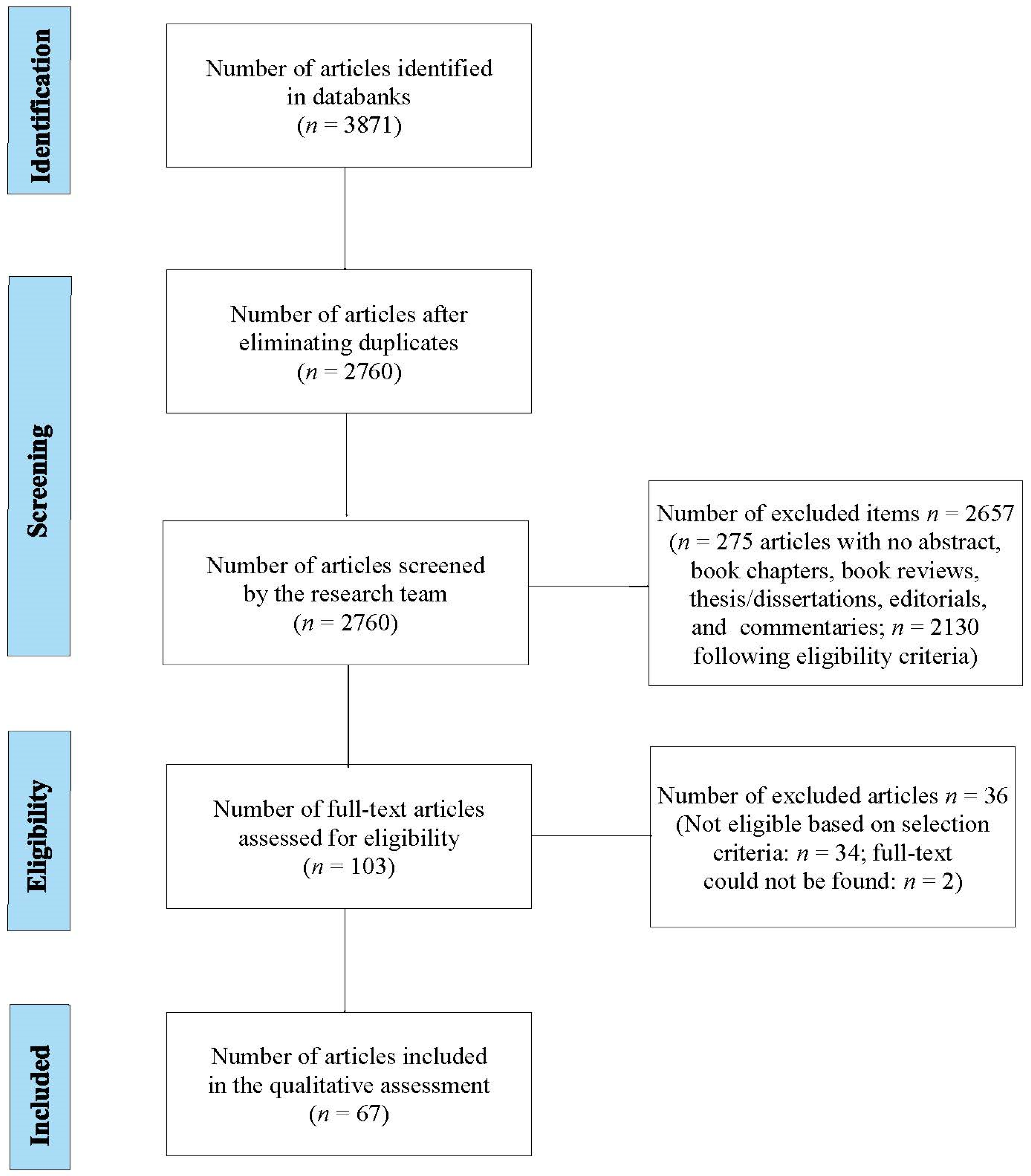
2. Methods
3. Results
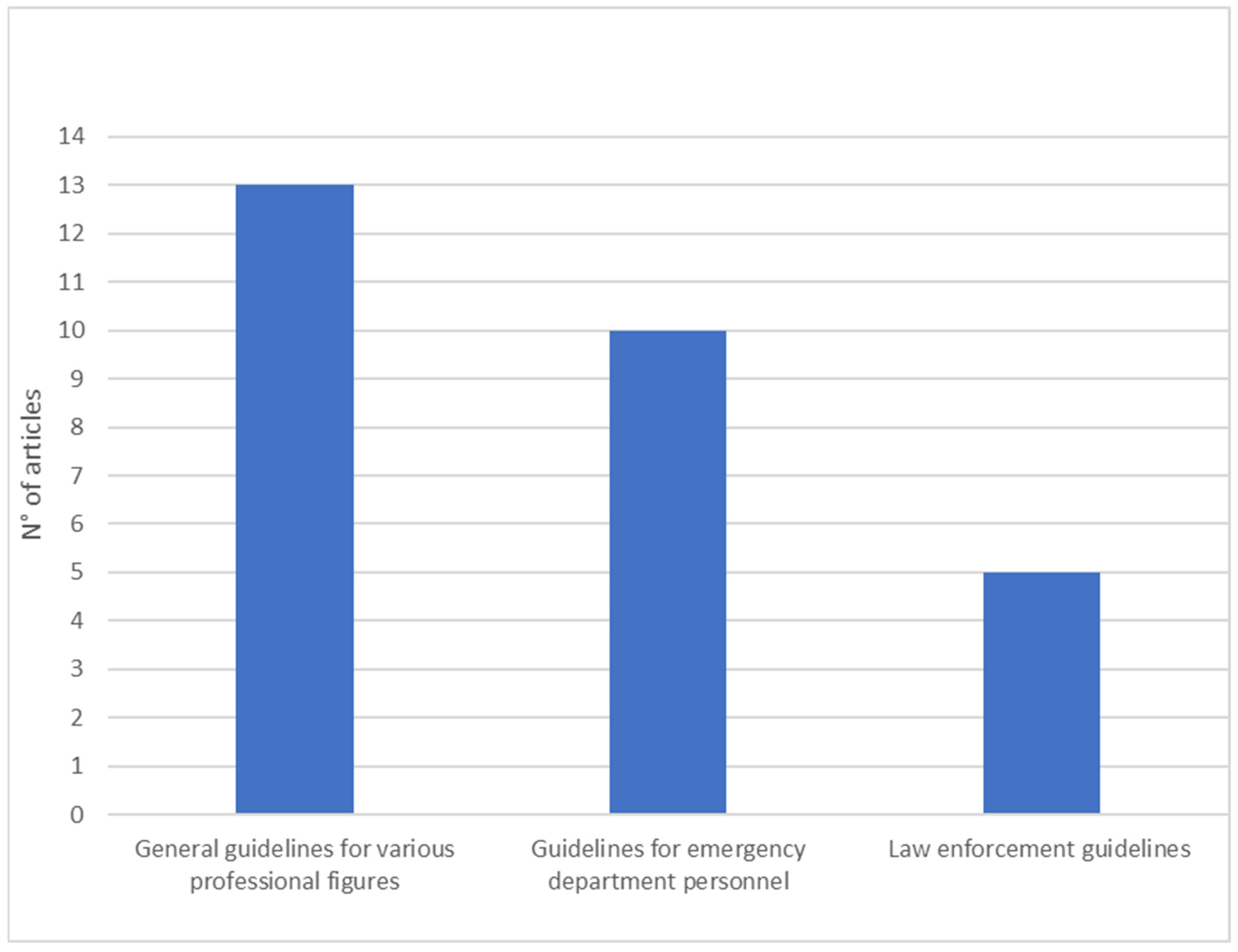
3.1. First Dimension: General Guidelines and in Relation to Various Professional Figures
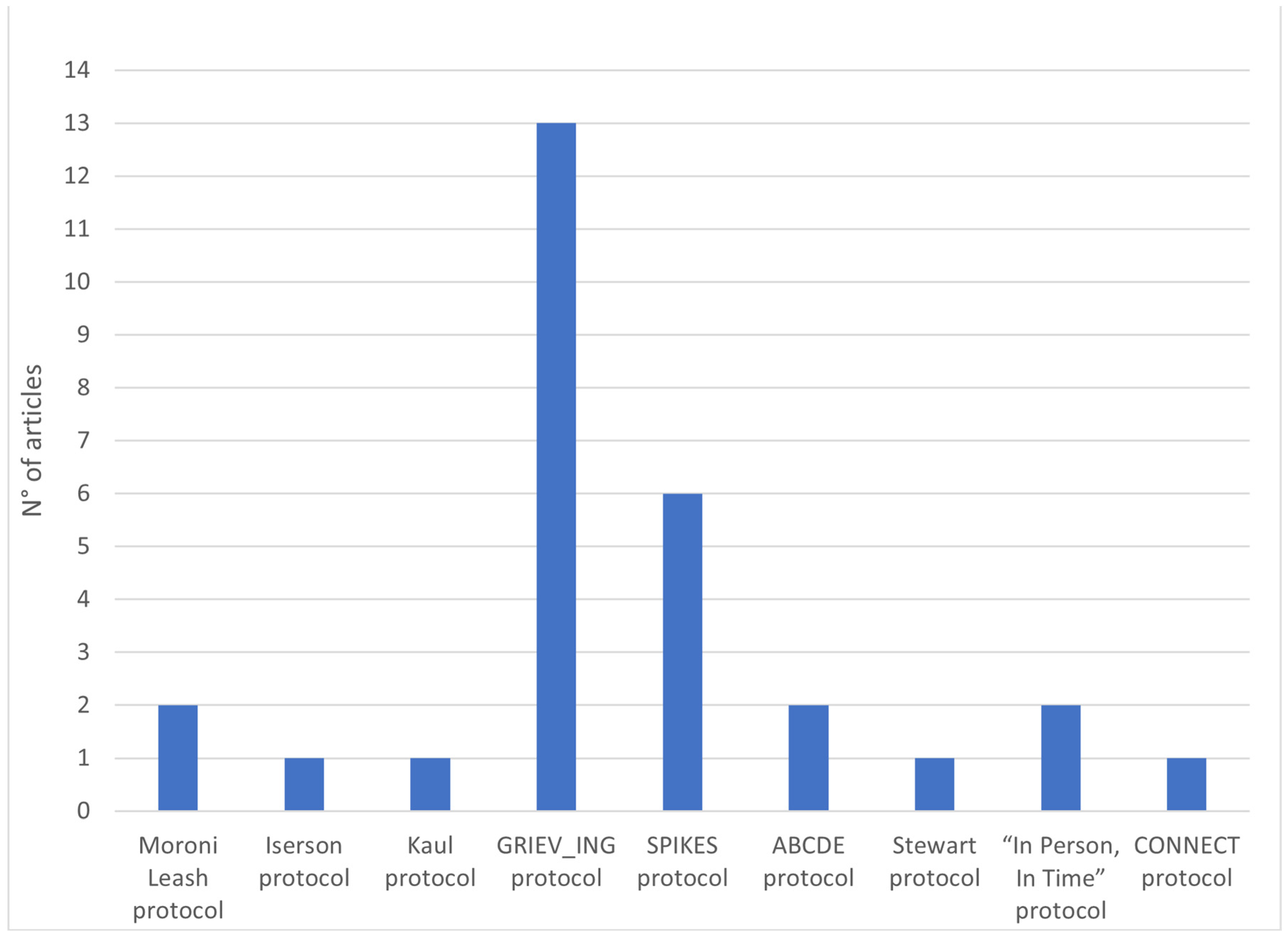
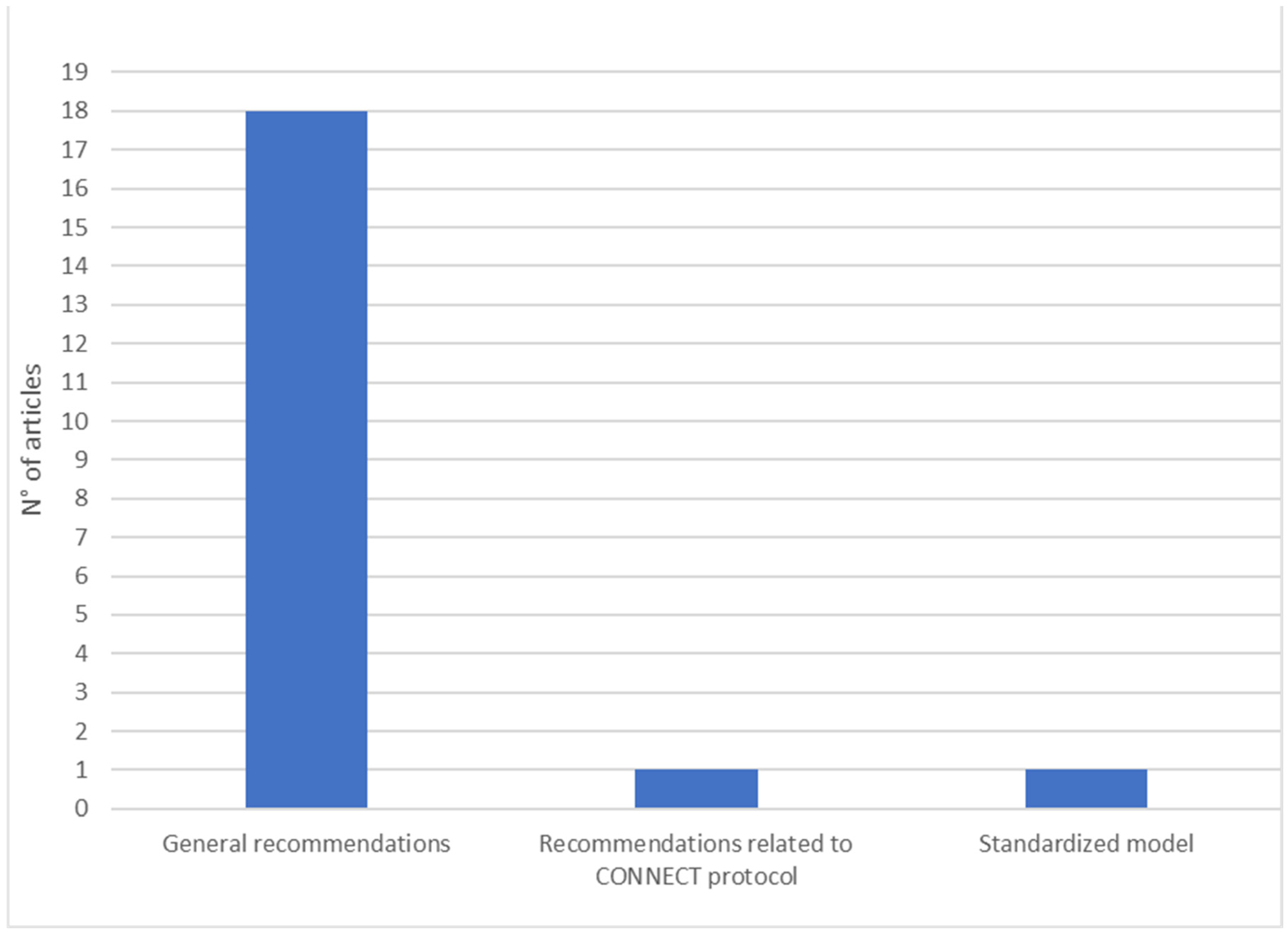
3.2. Second Dimension: Specific Protocols
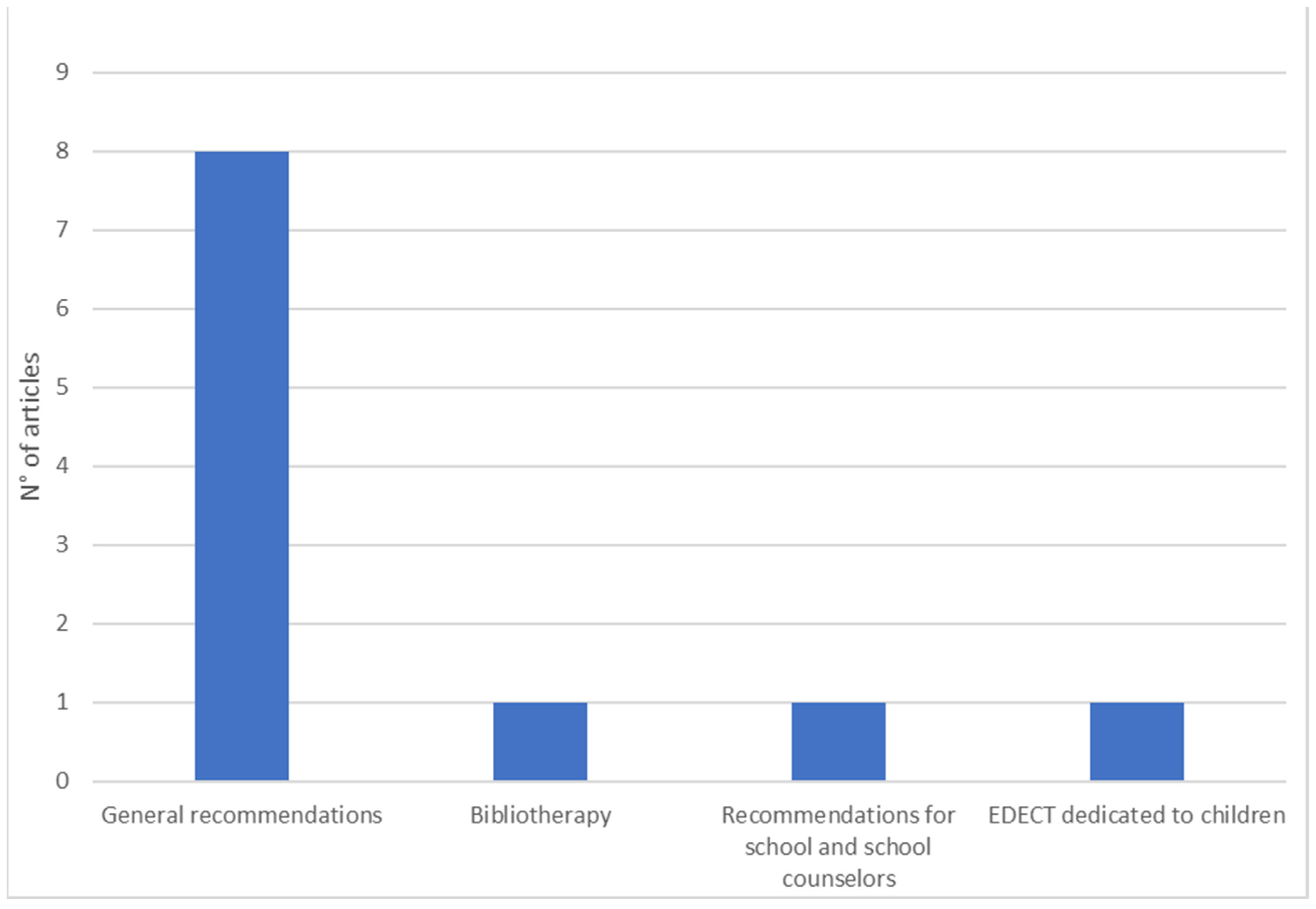
3.3. Third Dimension: Guidelines for Death Notification to Children
3.4. Fourth Dimension: Guidelines for Notification of Death by Telephone
3.5. Fifth Dimension: Best Practices for Death Notification Training Programs
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parris, R.J. Initial management of bereaved relatives following trauma. Trauma 2011, 14, 139–155. [Google Scholar] [CrossRef]
- Hofmann, L.; Glaesmer, H.; Przyrembel, M.; Wagner, B. The Impact of Police Behavior During Death Notifications on Mental Health of the Bereaved: A Cross-Sectional Study. Omega-J. Death Dying 2021, 87, 344–362. [Google Scholar] [CrossRef]
- McGill, G.; Wilson-Menzfeld, G.; Moreland, M.; Kiernan, M.D. “Knock on the Door”—Exploration of Casualty Notification and the Long-Term Impact on Military Families in the UK. J. Loss Trauma 2022, 27, 547–564. [Google Scholar] [CrossRef]
- Nilsson, C.; Blomberg, K.; Bremer, A. Existential loneliness and life suffering in being a suicide survivor: A reflective lifeworld research study. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2122157. [Google Scholar] [CrossRef]
- De Leo, D.; Zammarrelli, J.; Giannotti, A.V.; Donna, S.; Bertini, S.; Santini, A.; Anile, C. Notification of Unexpected, Violent and Traumatic Death: A Systematic Review. Front. Psychol. 2020, 11, 2229. [Google Scholar] [CrossRef] [PubMed]
- Hobgood, C.; Mathew, D.; Woodyard, D.J.; Shofer, F.S.; Brice, J.H. Death in the field: Teaching paramedics to deliver effective death notifications using the educational intervention “GRIEV_ING”. Prehosp. Emerg. Care 2013, 17, 501–510. [Google Scholar] [CrossRef]
- Shomoossi, N.; Rad, M.; Kooshan, M.; Ganjloo, J. Nurses as death notifiers: A report from nurses in Iran. Life Sci. J. 2013, 10, 26–31. [Google Scholar]
- Sobczak, K. The procedure for death notification—“In Person, In Time…”. Anaesthesiol. Intensive Ther. 2013, 45, 241–243. [Google Scholar] [CrossRef]
- Fiorentino, M.; Mosenthal, A.C.; Bryczkowski, S.; Lamba, S. Teaching Residents Communication Skills around Death and Dying in the Trauma Bay. J. Palliat. Med. 2021, 24, 77–82. [Google Scholar] [CrossRef]
- Ahmed, R.; Weaver, L.; Falvo, L.; Bona, A.; Poore, J.; Schroedle, K.; Cooper, D.; Sarmiento, E.; Hughes, M.; Hobgood, C. Rapid-cycle deliberate practice: Death notification. Clin. Teach. 2020, 17, 644–649. [Google Scholar] [CrossRef]
- Brand, M.; Mahlke, K. DNR and the Use of Blended Learning Methodology in German Police Education. In Advances in Web-Based Learning—ICWL 2017; Lecture Notes in Computer Science; Xie, H., Popescu, E., Hancke, G., Fernández Manjón, B., Eds.; Springer: Cham, Switzerland, 2017; Volume 10473. [Google Scholar] [CrossRef]
- Karam, V.Y.; Barakat, H.; Aouad, M.; Harris, I.; Park, Y.S.; Youssef, N.; Boulet, J.J.; Tekian, A. Effect of a simulation-based workshop on breaking bad news for anesthesiology residents: An intervention study. BMC Anesthesiol. 2017, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Campos, A.; Ernest, E.V.; Cash, R.E.; Rivard, M.K.; Panchal, A.R.; Clemency, B.M.; Swor, R.A.; Crowe, R.P. The Association of Death Notification and Related Training with Burnout among Emergency Medical Services Professionals. Prehosp. Emerg. Care 2021, 25, 539–548. [Google Scholar] [CrossRef]
- Dubin, W.R.; Sarnoff, J.R. Sudden unexpected death: Intervention with the survivors. Ann. Emerg. Med. 1986, 15, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Spencer, E.; Baron, D.A.; Pynoos, R.S. Death notification. Bull. Am. Acad. Psychiatry Law 1987, 15, 275–281. [Google Scholar]
- Schmidt, T.A.; Norton, R.L.; Tolle, S.W. Sudden death in the ED: Educating residents to compassionately inform families. J. Emerg. Med. 1992, 10, 643–647. [Google Scholar] [CrossRef] [PubMed]
- Adamowski, K.; Dickinson, G.; Weitzman, B.; Roessler, C.; Carter-Snell, C. Sudden unexpected death in the emergency department: Caring for the survivors. Can. Med. Assoc. J./J. L’association Med. Can. 1993, 149, 1445–1451. [Google Scholar]
- Swisher, L.A.; Nieman, L.Z.; Nilsen, G.J.; Spivey, W.H. Death notification in the emergency department: A survey of residents and attending physicians. Ann. Emerg. Med. 1993, 22, 1319–1323. [Google Scholar] [CrossRef]
- Marrow, J. Telling relatives that a family member has died suddenly. Postgrad. Med. J. 1996, 72, 413–418. [Google Scholar] [CrossRef]
- Leash, R.M. Death notification: Practical guidelines for health care professionals. Crit. Care Nurs. Q. 1996, 19, 21–34. [Google Scholar] [CrossRef]
- Von Bloch, L. Breaking the bad news when sudden death occurs. Soc. Work. Health Care 1996, 23, 91–97. [Google Scholar] [CrossRef]
- Ahrens, W.R.; Hart, R.G. Emergency physicians’ experience with pediatric death. Am. J. Emerg. Med. 1997, 15, 642–643. [Google Scholar] [CrossRef]
- Olsen, J.C.; Buenefe, M.L.; Falco, W.D. Death in the Emergency Department. Ann. Emerg. Med. 1998, 31, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.L.; Walz, B.J.; Smith, R.L. A death education curriculum for emergency physicians, paramedics, and other emergency personnel. Prehosp. Emerg. Care 1999, 3, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.E. Complicated bereavement and posttraumatic stress disorder following fatal car crashes: Recommendations for death notification practice. Death Stud. 1999, 23, 289–321. [Google Scholar] [CrossRef] [PubMed]
- Kaul, R.E. Coordinating the death notification process: The roles of the emergency room social worker and physician following a sudden death. Brief Treat. Crisis Interv. 2001, 1, 101–114. [Google Scholar] [CrossRef]
- Stewart, A.E.; Lord, J.H.; Mercer, D.L. Death Notification Education: A Needs Assessment Study. J. Trauma. Stress 2001, 14, 221–227. [Google Scholar] [CrossRef]
- Benenson, R.S.; Pollack, M.L. Evaluation of emergency medicine resident death notification skills by direct observation. Acad. Emerg. Med. 2003, 10, 219–223. [Google Scholar] [CrossRef]
- Janzen, L.; Cadell, S.; Westhues, A. From Death Notification Through the Funeral: Bereaved Parents’ Experiences and Their Advice to Professionals. Omega-J. Death Dying 2004, 48, 149–164. [Google Scholar] [CrossRef]
- Servaty-Seib, H.L.; Peterson, J.; Spang, D. Notifying individual students of a death loss: Practical recommendations for schools and school counselors. Death Stud. 2003, 27, 167–186. [Google Scholar] [CrossRef]
- Hart, C.W., Jr.; DeBernardo, C.R. Death notification: Considerations for law enforcement personnel. Int. J. Emerg. Ment. Health 2004, 6, 33–37. [Google Scholar]
- Levetown, M. Breaking Bad News in the Emergency Department: When Seconds Count. Adv. Emerg. Nurs. J. 2004, 26, 35–43. [Google Scholar]
- Hobgood, C.; Harward, D.; Newton, K.; Davis, W. The educational intervention “GRIEV_ING” improves the death notification skills of residents. Acad. Emerg. Med. 2005, 12, 296–301. [Google Scholar] [CrossRef]
- Smith-Cumberland, T.L.; Feldman, R.H. Survey of EMTs’ attitudes towards death. Prehosp. Disaster Med. 2005, 20, 184–188. [Google Scholar] [CrossRef]
- Eberwein, K.E. A mental health clinician’s guide to death notification. Int. J. Emerg. Ment. Health 2006, 8, 117–125. [Google Scholar] [PubMed]
- Smith-Cumberland, T.L.; Feldman, R.H. EMTs’ attitudes’ toward death before and after a death education program. Prehosp. Emerg. Care 2006, 10, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Scott, T. Sudden traumatic death: Caring for the bereaved. Trauma 2007, 9, 103–109. [Google Scholar] [CrossRef]
- Miller, L. Death notification for families of homicide victims: Healing dimensions of a complex process. Omega-J. Death Dying 2008, 57, 367–380. [Google Scholar] [CrossRef]
- Mitchell, J.T. A short guide to giving bad news. Int. J. Emerg. Ment. Health 2008, 10, 197–201. [Google Scholar]
- Hobgood, C.D.; Tamayo-Sarver, J.H.; Hollar, D.W., Jr.; Sawning, S. Griev_Ing: Death Notification Skills and Applications for Fourth-Year Medical Students. Teach. Learn. Med. 2009, 21, 207–219. [Google Scholar] [CrossRef]
- Park, I.; Gupta, A.; Mandani, K.; Haubner, L.; Peckler, B. Breaking bad news education for emergency medicine residents: A novel training module using simulation with the SPIKES protocol. J. Emerg. Trauma Shock 2010, 3, 385–388. [Google Scholar] [CrossRef]
- Douglas, L.A.; Cheskes, S.; Feldman, M.; Ratnapalan, S. Paramedics’ experiences with death notification: A qualitative study. J. Paramed. Pract. 2012, 4, 533–539. [Google Scholar] [CrossRef]
- Marco, C.A.; Wetzel, L.R. Communication with survivors of motor vehicle crashes. Emerg. Med. J. 2012, 29, 626–629. [Google Scholar] [CrossRef]
- Roe, E. Practical strategies for death notification in the emergency department. J. Emerg. Nurs. 2012, 38, 130–134. [Google Scholar] [CrossRef]
- Shaw, J.; Dunn, S.; Heinrich, P. Managing the delivery of bad news: An in-depth analysis of doctors’ delivery style. Patient Educ. Couns. 2012, 87, 186–192. [Google Scholar] [CrossRef]
- Scott, P. Sudden death in emergency care: Responding to bereaved relatives. Emerg. Nurse 2013, 21, 36–39. [Google Scholar] [CrossRef]
- Shoenberger, J.M.; Yeghiazarian, S.; Rios, C.; Henderson, S. Death Notification in the Emergency Department: Survivors and Physicians. West. J. Emerg. Med. 2013, 14, 181–185. [Google Scholar] [CrossRef]
- Galbraith, A.; Harder, N.; Macomber, C.A.; Roe, E.; Roethlisberger, K.S. Design andimplementation of an interprofessional death notification simulation. Clin. Simul. Nurs. 2014, 10, e95–e102. [Google Scholar] [CrossRef]
- Rivolta, M.M.; Rivolta, L.; Garrino, L.; Di Giulio, P. Communication of the death of a patient in hospices and nursing homes: A qualitative study. Eur. J. Oncol. Nurs. Off. J. Eur. Oncol. Nurs. Soc. 2014, 18, 29–34. [Google Scholar] [CrossRef]
- Baumann, R.; Stark, S. The role of forensic death investigators interacting with the survivors of death by homicide and suicide. J. Forensic Nurs. 2015, 11, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Reed, S.; Kassis, K.; Nagel, R.; Verbeck, N.; Mahan, J.D.; Shell, R. Breaking bad news is a teachable skill in pediatric residents: A feasibility study of an educational intervention. Patient Educ. Couns. 2015, 98, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Basinger, E.D.; Wehrman, E.; McAninch, K.G. Grief communication and privacy rules: Examining the communication of individuals bereaved by the death of a family member. J. Fam. Commun. 2016, 16, 285–302. [Google Scholar] [CrossRef]
- Carmack, H.J.; DeGroot, J. Development and validation of the communication apprehension about death scale. Omega-J. Death Dying 2016, 74, 239–259. [Google Scholar] [CrossRef]
- Veilleux, J.C.; Bilsky, S.A. After a client death: Suicide postvention recommendations for training programs and clinics. Train. Educ. Prof. Psychol. 2016, 10, 214–222. [Google Scholar] [CrossRef]
- Arruda-Colli, M.N.F.; Weaver, M.S.; Wiener, L. Communication About Dying, Death, and Bereavement: A Systematic Review of Children’s Literature. J. Palliat. Med. 2017, 20, 548–559. [Google Scholar] [CrossRef]
- Ombres, R.; Montemorano, L.; Becker, D. Death Notification: Someone Needs to Call the Family. J. Palliat. Med. 2017, 20, 672–675. [Google Scholar] [CrossRef]
- Shakeri, N.; Fant, A.; Gisondi, M.A.; Salzman, D. Assessment of death notification skills among emergency medicine residents using GRIEV_ING in high-fidelity patient simulation. Med. Sci. Educ. 2017, 27, 881–886. [Google Scholar] [CrossRef]
- Williams-Reade, J.; Lobo, E.; Whittemore, A.A.; Parra, L.; Baerg, J. Enhancing residents’ compassionate communication to family members: A family systems breaking bad news simulation. Fam. Syst. Health 2018, 36, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.D.; Dabney, D.A.; Tapp, S.N.; Ishoy, G.A. Tense Relationships between Homicide Co-Victims and Detectives in the Wake of Murder. Deviant Behav. 2019, 41, 543–561. [Google Scholar] [CrossRef]
- Servotte, J.-C.; Bragard, I.; Szyld, D.; Van Ngoc, P.; Scholtes, B.; Van Cauwenberge, I.; Donneau, A.-F.; Dardenne, N.; Goosse, M.; Pilote, B.; et al. Efficacy of a Short Role-Play Training on Breaking Bad News in the Emergency Department. West. J. Emerg. Med. 2019, 20, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Gerstner, B.; Bona, A.; Falvo, L.; Hobgood, C.; Ahmed, R.A. Death notification: A digital communication platform for simulated patient-based training with medical students. BMJ Simul. Technol. Enhanc. Learn. 2020, 7, 250–252. [Google Scholar] [CrossRef] [PubMed]
- Hughes, P.G.; Hughes, K.E.; Hughes, M.J.; Weaver, L.; Falvo, L.E.; Bona, A.M.; Cooper, D.; Hobgood, C.; Ahmed, R.A. Setup and Execution of the Rapid Cycle Deliberate Practice Death Notification Curriculum. J. Vis. Exp. JoVE 2020, 162, e61646. [Google Scholar] [CrossRef]
- Landa-Ramírez, E.; Domínguez-Vieyra, N.A.; Hernández-Nuñez, M.E.; Díaz-Vásquez, L.P.; Santana-García, I.A. Psychological support during COVID-19 death notifications: Clinical experiences from a hospital in Mexico. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 518–520. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, L.; Glaesmer, H.; Przyrembel, M.; Wagner, B. An Evaluation of a Suicide Prevention E-Learning Program for Police Officers (COPS): Improvement in Knowledge and Competence. Front. Psychiatry 2021, 12, 770277. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Gerstner, B.; Bona, A.; Falvo, L.; Schroedle, K.; Cooper, D.; Sarmiento, E.; Hobgood, C.; Ahmed, R.; Runde, D. Adaptive change in simulation education: Comparison of effectiveness of a communication skill curriculum on death notification using in-person methods versus a digital communication platform. AEM Educ. Train. 2021, 5, e10610. [Google Scholar] [CrossRef] [PubMed]
- De Leo, D.; Congregalli, B.; Guarino, A.; Zammarrelli, J.; Valle, A.; Paoloni, S.; Cipolletta, S. Communicating Unexpected and Violent Death: The Experiences of Police Officers and Health Care Professionals. Int. J. Environ. Res. Public Health 2022, 19, 11030. [Google Scholar] [CrossRef]
- De Leo, D.; Guarino, A.; Congregalli, B.; Zammarrelli, J.; Valle, A.; Paoloni, S.; Cipolletta, S. Receiving Notification of Unexpected and Violent Death: A Qualitative Study of Italian Survivors. Int. J. Environ. Res. Public Health 2022, 19, 10709. [Google Scholar] [CrossRef]
- Sobczak, K. The “CONNECT” Protocol: Delivering Bad News by Phone or Video Call. Int. J. Gen. Med. 2022, 15, 3567–3572. [Google Scholar] [CrossRef]
- Iserson, K.V. Grave Words: Notifying Survivors about Sudden, Unexpected Deaths; Galen Press: Tucson, AZ, USA, 1999. [Google Scholar]
- Stewart, A.E.; Lord, J.H.; Mercer, D.L. A survey of professionals’ training and experiences in delivering death notifications. Death Stud. 2000, 24, 611–631. [Google Scholar]
- Dyer, K.A. Death Pronouncement and Death Notification: What the Resident Needs to Know. Dealing with Death & Dying in Medical Education and Practice. EPERC (End-of-Life Physician Education Resource Center). 2001. Available online: www.eperc.mcw.edu (accessed on 5 November 2022).

| Author (Year) | Country | Target Population | Sample (n) | Study Design | Dimensions | ||||
|---|---|---|---|---|---|---|---|---|---|
| General Guidelines, and in Relation to Various Professional Figures | Specific Protocols | Guidelines for Death Notification to Children | Guidelines for Death Notification by Phone | Good Practice for Death Notification Training Programs | |||||
| Dubin and Sarnoff (1986) [14] | Pennsylvania (USA) | Doctors and health personnel of emergency departments. | NA | Descriptive/ narrative | Recommendations for the emergency department. | NA | Recommendations | Recommendations | NA |
| Spencer et al. (1987) [15] | California (USA) | Homicide detectives of the Los Angeles Police Department. | Fifty subjects filled out a questionnaire. Twenty-one of them also made a telephone interview. | Cross-sectional survey. | NA | NA | NA | NA | Need for training. |
| Schmidt et al. (1992) [16] | Oregon (USA) | Residents of Oregon Health Sciences University. | NA | Descriptive/narrative. | NA | NA | NA | Recommendations | Blended learning course for residents in the emergency department. |
| Adamowski et al. (1993) [17] | Canada | Two groups of survivors in Ottawa General Hospital. | Sixty-six subjects. | Survey. | Recommendations for the emergency department. | NA | NA | Recommendations | NA |
| Swisher et al. (1993) [18] | Pennsylvania (USA) | Forty-five residents and twenty physicians in emergency departments at the Medical College of Pennsylvania. | Sixty-five Subjects. | Survey. | Recommendations for the emergency department. | NA | NA | NA | Need for training. |
| Marrow (1996) [19] | UK | Emergency department personnel. | NA | Descriptive/ narrative. | Recommendations for the emergency department. | NA | Recommendations. | NA | Need for training. |
| Moroni Leash (1996) [20] | California (USA) | Medical professionals, university students in death and dying classes, and family members of newly admitted intensive care unit patients. | Two hundred medical professionals, 100 university students, and 100 family members. | Descriptive/ narrative. | NA | Moroni Leash protocol | Recommendations | Recommendations | NA |
| Von Bloch (1996) [21] | Texas (USA) | Health care professionals. | NA | Descriptive/narrative. | Recommendations for health professionals. | NA | NA | NA | NA |
| Ahrens and Hart (1997) [22] | Illinois (USA) | General emergency physicians. | One hundred and twenty-two subjects. | Survey | NA | NA | NA | NA | Need for training. |
| Olsen et al. (1998) [23] | Chicago (USA) | Emergency department personnel. | NA | Descriptive/narrative. | Recommendations for physicians in the emergency department. | Recommendations. | NA | NA | NA |
| Smith et al. (1999) [24] | Maryland (USA) | Emergency physicians, paramedics, and other emergency personnel. | NA | Descriptive/narrative. | NA | NA | NA | NA | Seminar: EDECT. |
| Stewart (1999) [25] | Florida (USA) | Those involved in notifying a road accident-related death. | NA | Descriptive/narrative. | Recommendations in case of road accidents. | NA | NA | Recommendations. | NA |
| Kaul (2001) [26] | Michigan (USA) | Emergency physicians, paramedics, and other emergency personnel. | NA | Descriptive/ narrative. | NA | Iserson protocol; Moroni Leash protocol; and Kaul protocol. | NA | Recommendations. | NA |
| Stewart et al. (2001) [27] | Florida (USA) | Death notifiers (law enforcement officers, emergency medical technicians, victim advocates, coroners, etc.) in seven cities of the USA. | Two hundred and forty-five subjects. | Survey. | NA | NA | NA | Recommendations. | Need for training; MADD seminar. |
| Benenson and Pollack (2003) [28] | England | Emergency medicine residents. | Seventy subjects. | Prospective observational. | NA | NA | NA | NA | Blended learning course. |
| Janzen et al. (2003–2004) [29] | Canada | Parents who had experienced the sudden death of a child in Ontario. | Twenty subjects. | Qualitative study. | Recommendations for various professionals in cases of pediatric death. | NA | NA | NA | NA |
| Servaty-Seib et al. (2003) [30] | Indiana (USA) | School communities. | NA | Descriptive/ narrative. | NA | NA | Recommendations for school and school counselors. | NA | NA |
| Hart and DeBernardo (2004) [31] | Baltimore (USA) | Law enforcement personnel. | NA | Descriptive/ narrative. | Recommendations for police officers. | NA | NA | Recommendations. | NA |
| Levetown (2004) [32] | Texas (USA) | Emergency care personnel. | NA | Descriptive/ narrative. | Recommendations for staff of the emergency department in the event of the death of a child. | NA | NA | Recommendations. | NA |
| Hobgood et al. (2005) [33] | North Carolina (USA) | Residents in emergency medicine. | Twenty subjects. | Pre-post study. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Smith-Cumberland (2005) [34] | Maryland, Pennsylvania, and Utah (USA) | Emergency medical technicians from 14 states. | One hundred and thirty-six subjects. | Survey. | NA | NA | NA | NA | Need for training. |
| Eberwein (2006) [35] | Maryland (USA) | Mental health professionals. | NA | Descriptive/ narrative. | Recommendations for various professionals. | NA | NA | Recommendations. | NA |
| Smith-Cumberland and Feldman (2006) [36] | Wisconsin (USA) | Emergency medical professionals. | Eighty-three subjects. | Pre-post study. | NA | NA | Part of EDECT dedicated to children. | NA | Blended learning course for emergency department: EDECT, with a focus on CME units. |
| Scott (2007) [37] | England | Emergency medical professionals and police officers. | NA | Descriptive/narrative. | Recommendations for the staff of the emergency department. | NA | NA | NA | NA |
| Miller (2008) [38] | Florida (USA) | Professionals potentially involved in notifying death. | NA | Descriptive/narrative. | Recommendations for various professionals in the case of murder. | NA | Recommendations. | Recommendations. | NA |
| Mitchell (2008) [39] | Maryland (USA) | Professionals potentially involved in notifying death. | NA | Descriptive/ narrative. | Recommendations for various professionals. | NA | Recommendations. | Recommendations. | NA |
| Hobgood et al. (2009) [40] | North Carolina (USA) | Fourth year medical students at the University of North Carolina. | One hundred and forty-eight subjects. | Pre-post study. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Park et al. (2010) [41] | Florida (USA) | Emergency medicine residents. | Fourteen subjects. | Descriptive/narrative. | NA | SPIKE protocol; GRIEV_ING protocol. | NA | NA | Blended learning course for the emergency department. |
| Parris (2011) [1] | UK | Emergency medical professionals. | NA | Descriptive/ narrative. | Recommendations for the emergency department. | NA | NA | Recommendations. | NA |
| Douglas et al. (2012) [42] | Canada | Paramedics in urban and rural areas of Ontario. | Twenty-eight subjects. | Qualitative study. | NA | NA | NA | NA | Need for training. |
| Marco and Wetzel (2012) [43] | Ohio (USA) | Patients who were involved in a fatal motor vehicle crash between 2005 and 2009. | Twenty-one subjects. | Cross-sectional survey study. | Recommendations in the case of a motor vehicle crash. | NA | NA | NA | NA |
| Roe (2012) [44] | Michigan (USA) | Emergency medical professionals. | NA | Descriptive/ narrative. | Recommendations for the staff of the emergency department. | NA | NA | NA | NA |
| Shaw et al. (2012) [45] | Australia | Doctors employed in Sydney metropolitan hospitals. | Thirty-one subjects. | Mixed-method design (quantitative/ qualitative). | NA | NA | NA | NA | Need for training. |
| Hobgood et al. (2013) [6] | North Carolina (USA) | Emergency medical service personnel. | Thirty subjects. | Pre-post design. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Scott (2013) [46] | England | Emergency medical professionals. | NA | Descriptive/ narrative. | Recommendations for the staff of the emergency department. | NA | NA | NA | Exercises for residents. |
| Shoenberger et al. (2013) [47] | South California (USA) | Physicians of emergency departments. | NA | Review. | NA | GRIEV_ING protocol. | NA | NA | Need for training. |
| Shomoossi et al. (2013) [7] | Iran | Nurses working in hospitals in Sabzevar, in Iran. | Ninety-seven subjects. | Development and validation of a scale. | NA | SPIKES protocol; ABCDE protocol; and Stewart protocol. | NA | NA | NA |
| Sobczak (2013) [8] | Poland | Doctors involved in death notification. | NA | Descriptive/ narrative. | NA | SPIKES protocol; “In person, in time” protocol. | . | Recommendations. | NA |
| Galbraith et al. (2014) [48] | Midwestern (USA) | Senior-level nursing and social work students. | Thirty-two subjects. | Development of a valid simulation model. | NA | NA | NA | NA | Simulation for nursing and social work students. |
| Rivolta et al. (2014) [49] | Torino (Italy) | Health care nurses from two nursing homes and two hospices. | Fifty-five subjects. | Qualitative study. | Recommendations for staff of hospices and nursing homes. | NA | NA | NA | NA |
| Baumann and Stark (2015) [50] | New Jersey (USA) | Forensic death investigators and other death notifiers. | NA | Descriptive/narrative. | Recommendations for forensic nurses (FNDIs). | NA | NA | NA | NA |
| Reed et al. (2015) [51] | Ohio (USA) | First year pediatric and internal medicine residents. | Forty-four subjects. | Pre-post design. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Basinger et al. (2016) [52] | Midwestern (USA) | College students who had lost a parent or a sibling. | Twenty-one subjects. | Qualitative study. | Privacy management process. | NA | Recommendations. | NA | NA |
| Carmack and DeGroot (2016) [53] | Virginia (USA) | Lay people recruited via social media and other means. | Three hundred and two subjects in study 1; three hundred and nineteen in study 2. | Development and validation of a new scale. | NA | NA | NA | NA | Need for training. |
| Veilleux and Bilsky (2016) [54] | Arkansas (USA) | Therapists and residents after a patient’s death (e.g., suicide). | NA | Descriptive/narrative. | Recommendations in the case of the suicide of a patient. | NA | NA | Recommendations. | NA |
| Arruda-Colli et al. (2017) [55] | Maryland (USA) | Storybooks about dying, death, and bereavement in English, French, or Spanish, published 1995–2015. | Two hundred and ten subjects. | Review article. | NA | NA | Bibliotherapy. | NA | NA |
| Brand and Mahlke (2017) [11] | Germany | German police officers. | NA | Descriptive/ narrative. | NA | NA | NA | NA | DNR—blended learning course. |
| Karam et al. (2017) [12] | Lebanon | Residents of PGY3 and PGY4 Lebanese anesthesiology. | Sixteen subjects. | Pre-post training. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Ombres et al. (2017) [56] | Maryland (USA) | Internal medicine residents. | Sixty-seven subjects. | Review article. | NA | NA | NA | Standardized model. | NA |
| Shakeri et al. (2017) [57] | Chicago (USA) | American university—4 year emergency medicine training program. | Forty subjects. | Validation study. | NA | GRIEV_ING protocol. | NA | NA | NA |
| Williams-Reade et al. (2018) [58] | California (USA) | Pediatric surgery residents. | 15 | Pre-post study. | NA | SPIKES protocol. | NA | NA | Seminars and simulation. |
| Reed et al. (2019) [59] | Georgia (USA) | Homicide unit members/homicide co-victims. | 52 (26 + 26) | Qualitative study. | Recommendations for police officers. | NA | NA | Recommendations. | Need for training. |
| Servotte et al. (2019) [60] | Belgium | Medical students and residents. | 68 | Pre-post study. | NA | SPIKES protocol. | NA | NA | Blended learning course. |
| Ahmed et al. (2020) [10] | Indiana (USA) | Emergency medicine residents. | 22 | Pre-post study. | NA | GRIEV_ING protocol. | NA | NA | Simulation and Rapid Cycle Deliberate Practice (RCDP). |
| Campos et al. (2020) [13] | Nebraska/Massachusetts/Ohio/New York/Michigan/Texas (USA) | Emergency medical services professionals. | 1514 | Survey | NA | NA | NA | NA | Need for training. |
| De Leo et al. (2020) [5] | Italy | NA | Sixty articles. | Systematic review. | Recommendations for various professionals. | GRIEV_ING protocol; SPIKES protocol; ABCDE protocol; and “In Perso, In Time” protocol. | Recommendations. | Recommendations. | Blended learning course. |
| Hughes et al. (2020a) [61] | Michigan (USA) | Medical school students. | 12 | Validation of a digital communication platform model. | NA | GRIEV_ING protocol. | NA | NA | Blended learning course (digital platform). |
| Hughes et al. (2020b) [62] | Florida/Indiana/Arizona/Michigan (USA) | Emergency medicine physicians. | NA | Descriptive/narrative. | NA | GRIEV_ING protocol | NA | NA | Simulation and Rapid Cycle Deliberate Practice (RCDP). |
| Landa-Ramìrez et al. (2020) [63] | Mexico | Health care professionals. | NA | Descriptive/narrative. | NA | NA | NA | Recommendations. | Online blended learning course. |
| Fiorentino et al. (2021) [9] | New Jersey (USA) | Trauma (general surgery and EM) residents. | 39 | Pre-post study. | NA | NA | NA | NA | Blended learning course. |
| Hofmann et al. (2021a) [64] | Germany | Police officers. | 142 | Pre-post study. | NA | NA | NA | NA | Blended learning course (e-learning program) for police officers. |
| Hofmann et al. (2021b) [2] | Germany | Police officers. | 86 | Qualitative study. | Recommendations for police officers. | NA | NA | NA | Need for training for police officers. |
| Hughes et al. (2021) [65] | Michigan/Indiana (USA) | Emergency medicine residents/ medical school students. | Thirty-four (22 residents + 12 students). | Pre-post study. | NA | GRIEV_ING protocol. | NA | NA | Simulation and Rapid Cycle Deliberate Practice (RCDP). |
| De Leo et al. (2022a) [66] | Italy | Police officers/ health professionals (doctors and nurses). | 155 | Qualitative study. | Recommendations for various professionals. | NA | NA | NA | Need for training. |
| De Leo et al. (2022b) [67] | Italy | Survivors of traumatic death | 52 | Qualitative study. | Recommendations for various professionals. | NA | NA | NA | NA |
| McGill et al. (2022) [3] | United Kingdom | Survivors (spouses, parents, and children) of the deaths of UK Armed Forces members. | 15 | Qualitative study. | Recommendations for veterans. | NA | Recommendations. | NA | NA |
| Sobczak (2022) [68] | Poland | Health care professionals. | NA | Development of a protocol for remote communication of bad news. | NA | CONNECT protocol. | NA | Recommendations related to the CONNECT protocol. | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Leo, D.; Zammarrelli, J.; Marinato, G.; Capelli, M.; Viecelli Giannotti, A. Best Practices for Notification of Unexpected, Violent, and Traumatic Death: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 6222. https://doi.org/10.3390/ijerph20136222
De Leo D, Zammarrelli J, Marinato G, Capelli M, Viecelli Giannotti A. Best Practices for Notification of Unexpected, Violent, and Traumatic Death: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(13):6222. https://doi.org/10.3390/ijerph20136222
Chicago/Turabian StyleDe Leo, Diego, Josephine Zammarrelli, Giulia Marinato, Marta Capelli, and Andrea Viecelli Giannotti. 2023. "Best Practices for Notification of Unexpected, Violent, and Traumatic Death: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 13: 6222. https://doi.org/10.3390/ijerph20136222
APA StyleDe Leo, D., Zammarrelli, J., Marinato, G., Capelli, M., & Viecelli Giannotti, A. (2023). Best Practices for Notification of Unexpected, Violent, and Traumatic Death: A Scoping Review. International Journal of Environmental Research and Public Health, 20(13), 6222. https://doi.org/10.3390/ijerph20136222







