Changes in Quantity Measures of Various Forms of Cannabis Consumption among Emerging Adults in Canada in Relation to Policy and Public Health Developments
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Participants and Recruitment
2.3. Measures
2.3.1. Independent Variables
2.3.2. Dependent Variables
2.3.3. Explanatory Variables
2.4. Data Analyses
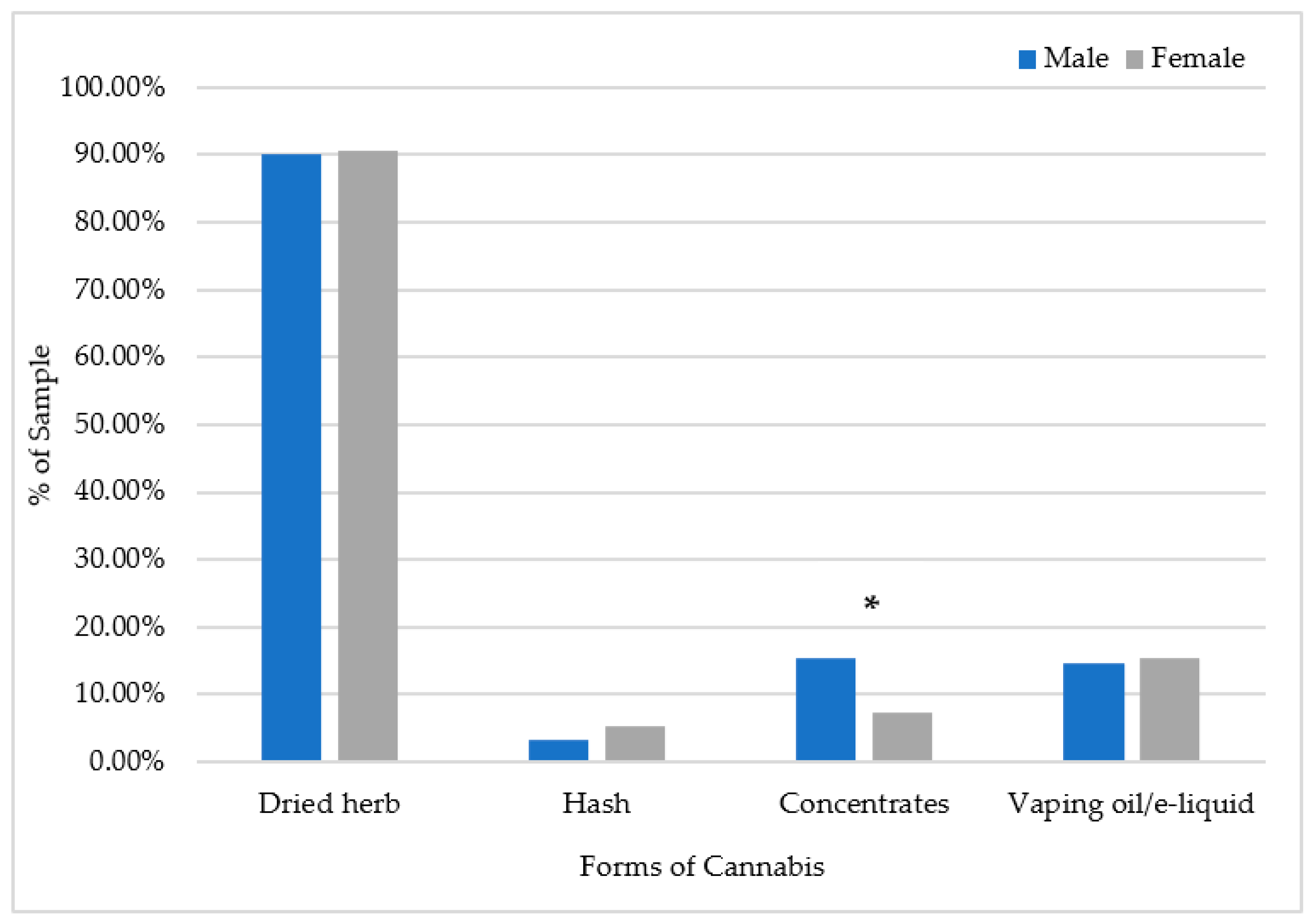
3. Results
Changes in Quantity of Cannabis Consumption Forms
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Leos-Toro, C.; Rynard, V.; Hammond, D. Prevalence of problematic cannabis use in Canada: Cross-sectional findings from the 2013 Canadian Tobacco, Alcohol and Drugs Survey. Can. J. Public Health 2017, 108, e516–e522. [Google Scholar] [CrossRef] [PubMed]
- Rotermann, M.; Macdonald, R. Analysis of trends in the prevalence of cannabis use in Canada, 1985 to 2015. Health Rep. 2018, 29, 10–20. [Google Scholar] [PubMed]
- Rotermann, M. Analysis of trends in the prevalence of cannabis use and related metrics in Canada. Health Rep. 2019, 30, 3–13. [Google Scholar]
- Callaghan, R.C.; Sanches, M.; Benny, C.; Stockwell, T.; Sherk, A.; Kish, S.J. Who consumes most of the cannabis in Canada? Profiles of cannabis consumption by quantity. Drug Alcohol Depend. 2019, 205, 107587. [Google Scholar] [CrossRef]
- Harris-Lane, L.; Winters, E.; Harris, N. Emerging Adult Perceptions of Cannabis Use Based on Age and Sex of User. Emerg. Adulthood 2020, 9, 339–346. [Google Scholar] [CrossRef]
- Mostaghim, A.; Hathaway, A.D. Identity formation, marijuana and “the self”: A study of cannabis normalization among university students. Front. Psychiatry 2013, 4, 160. [Google Scholar] [CrossRef]
- Asbridge, M.; Duff, C.; Marsh, D.C.; Erickson, P.G. Problems with the identification of ‘problematic’ cannabis use: Examining the issues of frequency, quantity, and drug use environment. Eur. Addict. Res. 2014, 20, 254–267. [Google Scholar] [CrossRef]
- Al Iede, M.; Nunn, K.; Milne, B.; Fitzgerald, D.A. The consequences of chronic cannabis smoking in vulnerable adolescents. Paediatr. Respir. Rev. 2017, 24, 44–53. [Google Scholar] [CrossRef]
- Van Der Pol, P.; Liebregts, N.; De Graaf, R.; Korf, D.J.; van den Brink, W.; van Laar, M. Predicting the transition from frequent cannabis use to cannabis dependence: A three-year prospective study. Drug Alcohol Depend. 2013, 133, 352–359. [Google Scholar] [CrossRef]
- Zeisser, C.; Thompson, K.; Stockwell, T.; Duff, C.; Chow, C.; Vallance, K.; Ivsins, A.; Michelow, W.; Marsh, D.; Lucas, P. A ‘standard joint’? The role of quantity in predicting cannabis-related problems. Addict. Res. Theory 2012, 20, 82–92. [Google Scholar] [CrossRef]
- Looby, A.; Earleywine, M. Negative consequences associated with dependence in daily cannabis users. Subst. Abus. Treat. Prev. Policy 2007, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Leos-Toro, C.; Fong, G.T.; Meyer, S.B.; Hammond, D. Cannabis health knowledge and risk perceptions among Canadian youth and young adults. Harm Reduct. J. 2020, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Cooper, Z.D.; Craft, R.M. Sex-dependent effects of cannabis and cannabinoids: A translational perspective. Neuropsychopharmacology 2018, 43, 34–51. [Google Scholar] [CrossRef]
- Greaves, L.; Hemsing, N. Sex and gender interactions on the use and impact of recreational cannabis. Int. J. Environ. Res. Public Health 2020, 17, 509. [Google Scholar] [CrossRef]
- Russell, C.; Rueda, S.; Room, R.; Tyndall, M.; Fischer, B. Routes of administration for cannabis use–basic prevalence and related health outcomes: A scoping review and synthesis. Int. J. Drug Policy 2018, 52, 87–96. [Google Scholar] [CrossRef]
- Melchior, M.; Nakamura, A.; Bolze, C.; Hausfater, F.; El Khoury, F.; Mary-Krause, M.; Da Silva, M.A. Does liberalisation of cannabis policy influence levels of use in adolescents and young adults? A systematic review and meta-analysis. BMJ Open 2019, 9, e025880. [Google Scholar] [CrossRef]
- Government of The Netherlands. Toleration Policy Regarding Soft Drugs and Coffee Shops. Available online: https://www.government.nl/topics/drugs/toleration-policy-regarding-soft-drugs-and-coffee-shops (accessed on 8 June 2023).
- Zhang, M.W.; Ho, R. The cannabis dilemma: A review of its associated risks and clinical efficacy. J. Addict. 2015, 2015, 707596. [Google Scholar] [CrossRef]
- United Nations Office on Drugs and Crime (UNODC). World Drug Report. 2022. Available online: https://www.unodc.org/res/wdr2022/MS/WDR22_Booklet_3.pdf (accessed on 8 June 2023).
- Windle, S.B.; Wade, K.; Filion, K.B.; Kimmelman, J.; Thombs, B.D.; Eisenberg, M.J. Potential harms from legalization of recreational cannabis use in Canada. Can. J. Public Health 2019, 110, 222–226. [Google Scholar] [CrossRef]
- Kerr, D.C.R.; Bae, H.; Phibbs, S.; Kern, A.C. Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon. Addiction 2017, 112, 1992–2001. [Google Scholar] [CrossRef]
- Parnes, J.E.; Smith, J.K.; Conner, B.T. Reefer madness or much ado about nothing? Cannabis legalization outcomes among young adults in the United States. Int. J. Drug Policy 2018, 56, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Rotermann, M. What has changed since cannabis was legalized. Health Rep. 2020, 31, 11–20. [Google Scholar] [PubMed]
- Budney, A.J.; Borodovsky, J.T. The potential impact of cannabis legalization on the development of cannabis use disorders. Prev. Med. 2017, 104, 31–36. [Google Scholar] [CrossRef]
- Fischer, B.; Russell, C.; Sabioni, P.; Van Den Brink, W.; Le Foll, B.; Hall, W.; Rehm, J.; Room, R. Lower-risk cannabis use guidelines: A comprehensive update of evidence and recommendations. Am. J. Public Health 2017, 107, e1–e12. [Google Scholar] [CrossRef] [PubMed]
- Halladay, J.; Petker, T.; Fein, A.; Munn, C.; Mackillop, J. Brief interventions for cannabis use in emerging adults: Protocol for a systematic review, meta-analysis, and evidence map. Syst. Rev. 2018, 7, 106. [Google Scholar] [CrossRef] [PubMed]
- Yousufzai, S.J.; Cole, A.G.; Nonoyama, M.; Barakat, C. Changes in cannabis consumption among emerging adults in relation to policy and public health developments. Subst. Use Misuse 2022, 57, 730–741. [Google Scholar] [CrossRef] [PubMed]
- Borgonhi, E.M.; Volpatto, V.L.; Ornell, F.; Rabelo-da-Ponte, F.D.; Kessler, F.H.P. Multiple clinical risks for cannabis users during the COVID-19 pandemic. Addict. Sci. Clin. Pract. 2021, 16, 5. [Google Scholar] [CrossRef]
- Dubey, M.J.; Ghosh, R.; Chatterjee, S.; Biswas, P.; Chatterjee, S.; Dubey, S. COVID-19 and addiction. Diabetes Metab. Syndr. 2020, 14, 817–823. [Google Scholar] [CrossRef]
- Watson, T.M.; Erickson, P.G. Cannabis legalization in Canada: How might ‘strict’ regulation impact youth? Drugs Educ. Prev. Policy 2018, 26, 1–5. [Google Scholar] [CrossRef]
- Daniulaityte, R.; Zatreh, M.Y.; Lamy, F.R.; Nahhas, R.W.; Martins, S.S.; Sheth, A.; Carlson, R.G. A Twitter-based survey on marijuana concentrate use. Drug Alcohol Depend. 2018, 187, 155–159. [Google Scholar] [CrossRef]
- Hall, W.; Degenhardt, L. High potency cannabis. BMJ 2015, 350, h1205. [Google Scholar] [CrossRef]
- Volkow, N.D.; Baler, R.D.; Compton, W.M.; Weiss, S.R. Adverse health effects of marijuana use. N. Engl. J. Med. 2014, 370, 2219–2227. [Google Scholar] [CrossRef]
- Braymiller, J.L.; Barrington-Trimis, J.L.; Leventhal, A.M.; Islam, T.; Kechter, A.; Krueger, E.A.; Cho, J.; Lanza, I.; Unger, J.B.; McConnell, R. Assessment of Nicotine and Cannabis Vaping and Respiratory Symptoms in Young Adults. JAMA Netw. Open 2020, 3, e2030189. [Google Scholar] [CrossRef] [PubMed]
- King, B.A.; Jones, C.M.; Baldwin, G.T.; Briss, P.A. The EVALI and youth vaping epidemics—Implications for public health. N. Engl. J. Med. 2020, 382, 689–691. [Google Scholar] [CrossRef]
- Gloss, D. An overview of products and bias in research. Neurotherapeutics 2015, 12, 731–734. [Google Scholar] [CrossRef]
- Chand, H.S.; Muthumalage, T.; Maziak, W.; Rahman, I. Pulmonary toxicity and the pathophysiology of electronic cigarette, or vaping product, use associated lung injury. Front. Pharmacol. 2020, 10, 1619. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Crosier, B.S.; Borodovsky, J.T.; Sargent, J.D.; Budney, A.J. Online survey characterizing vaporizer use among cannabis users. Drug Alcohol Depend. 2016, 159, 227–233. [Google Scholar] [CrossRef]
- Jones, C.B.; Hill, M.L.; Pardini, D.A.; Meier, M.H. Prevalence and correlates of vaping cannabis in a sample of young adults. Psychol. Addict. Behav. 2016, 30, 915. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Gotway, M.B.; Crotty Alexander, L.E.; Hariri, L.P. Vaping-related lung injury. Virchows Archiv. 2021, 478, 81–88. [Google Scholar] [CrossRef]
- Ellington, S.; Salvatore, P.P.; Ko, J.; Danielson, M.; Kim, L.; Cyrus, A.; Wallace, M.; Board, A.; Krishnasamy, V.; King, B.A.; et al. Update: Product, substance-use, and demographic characteristics of hospitalized patients in a nationwide outbreak of e-cigarette, or vaping, product use–associated lung injury—United States, August 2019–January 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 44–49. [Google Scholar] [CrossRef]
- Baker, M.M.; Procter, T.D.; Belzak, L.; Ogunnaike-Cooke, S. Vaping-associated lung illness (VALI) in Canada: A descriptive analysis of VALI cases reported from September 2019 to December 2020. La maladie pulmonaire associée au vapotage (MPAV) au Canada: Une analyse descriptive des cas de MPAV signalés entre septembre 2019 et décembre 2020. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2022, 42, 37–44. [Google Scholar] [CrossRef]
- Aberegg, S.K.; Cirulis, M.M.; Maddock, S.D.; Freeman, A.; Keenan, L.M.; Pirozzi, C.S.; Raman, S.M.; Schroeder, J.; Mann, H.; Callahan, S.J. Clinical, Bronchoscopic, and Imaging Findings of e-Cigarette, or Vaping, Product Use—Associated Lung Injury Among Patients Treated at an Academic Medical Center. JAMA Netw. Open 2020, 3, e2019176. [Google Scholar] [CrossRef]
- Blagev, D.P.; Lanspa, M.J. Autopsy insights from the EVALI epidemic. The Lancet. Respir. Med. 2020, 8, 1165–1166. [Google Scholar] [CrossRef]
- Kreslake, J.M.; Diaz, M.C.; Shinaba, M.; Vallone, D.M.; Hair, E.C. Youth and young adult risk perceptions and behaviours in response to an outbreak of e-cigarette/vaping-associated lung injury (EVALI) in the USA. Tob. Control. 2021, 31, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, A.F.; Rodriguez, D.; Mazur, A.; Audrain-McGovern, J. Adolescent perceptions of E-cigarette use and vaping behavior before and after the EVALI outbreak. Prev. Med. 2021, 145, 106419. [Google Scholar] [CrossRef] [PubMed]
- Trivers, K.F.; Watson, C.V.; Neff, L.J.; Jones, C.M.; Hacker, K. Tetrahydrocannabinol (THC)-containing e-cigarette, or vaping, product use behaviors among adults after the onset of the 2019 outbreak of e-cigarette, or vaping, product use-associated lung injury (EVALI). Addict. Behav. 2021, 121, 106990. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020 [Internet]; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/director-general/speeches/detail/who-directorgeneral-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 21 January 2023).
- Cherkasova, M. Addiction in the times of pandemic. Can. J. Addict. 2020, 11, 9. [Google Scholar] [CrossRef]
- Dumas, T.M.; Ellis, W.; Litt, D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J. Adolesc. Health 2020, 67, 354–361. [Google Scholar] [CrossRef]
- Van Laar, M.W.; Oomen, P.E.; Van Miltenburg, C.J.; Vercoulen, E.; Freeman, T.P.; Hall, W.D. Cannabis and COVID-19: Reasons for concern. Front. Psychiatry 2020, 11, 1419. [Google Scholar] [CrossRef]
- Government of Canada. Available online: https://www.canada.ca/en/health-canada/news/2021/12/health-canada-releases-new-data-on-cannabis-use-in-canada.html (accessed on 29 April 2023).
- Sznitman, S.; Rosenberg, D.; Lewis, N. Are COVID-19 health-related and socioeconomic stressors associated with increases in cannabis use in individuals who use cannabis for recreational purposes? Subst. Abus. 2022, 43, 301–308. [Google Scholar] [CrossRef]
- Rosenberg, D.; Sznitman, S. Risk perception, health stressors and reduction in sharing cannabis products during the COVID-19 outbreak: A cross-sectional study. Drugs Alcohol Today 2022, 22, 28–35. [Google Scholar] [CrossRef]
- Hammond, D.; Goodman, S.; Leos-Toro, C.; Wadsworth, E.; Reid, J.L.; Hall, W.; Pacul, R.; Driezen, P.; George, T.; Rehm, J.; et al. International Cannabis Policy Survey; University of Waterloo: Waterloo, ON, Canada, 2018. [Google Scholar]
- Cuttler, C.; Spradlin, A. Measuring cannabis consumption: Psychometric properties of the daily sessions, frequency, age of onset, and quantity of cannabis use inventory (DFAQ-CU). PLoS ONE 2017, 12, e0178194. [Google Scholar] [CrossRef]
- Wong, S.W.; Lin, H.C.; Piper, M.E.; Siddiqui, A.; Buu, A. Measuring characteristics of e-cigarette consumption among college students. J. Am. Coll. Health 2019, 67, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Jeffreys, H. The Theory of Probability; OUP Oxford: Oxford, UK, 1998. [Google Scholar]
- Lee, M.D.; Wagenmakers, E.J. Bayesian Cognitive Modeling: A Practical Course; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Beard, E.; Dienes, Z.; Muirhead, C.; West, R. Using Bayes factors for testing hypotheses about intervention effectiveness in addictions research. Addiction 2016, 111, 2230–2247. [Google Scholar] [CrossRef]
- Patel, T.; Karle, E.; Gubeladze, T.; Pentecost, G.; Krvavac, A. Patient perception of vaping in the midst of the electronic cigarette and vaping product associated lung injury (EVALI) epidemic. Mo. Med. 2020, 117, 265–270. [Google Scholar] [PubMed]
- Perrine, C.G.; Pickens, C.M.; Boehmer, T.K.; King, B.A.; Jones, C.M.; DeSisto, C.L.; Duca, L.M.; Lekiachvili, A.; Kenemer, B.; Shamout, M.; et al. Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping—United States. Morb. Mortal. Wkly. Rep. 2019, 68, 860–864. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.M.; Goniewicz, M.L. The role of policy in the EVALI outbreak: Solution or contributor? Lancet Respir. Med. 2020, 8, 343–344. [Google Scholar] [CrossRef]
- Meier, M.H. Associations between butane hash oil use and cannabis-related problems. Drug Alcohol Depend. 2017, 179, 25–31. [Google Scholar] [CrossRef]
- Loflin, M.; Earleywine, M. A new method of cannabis ingestion: The dangers of dabs? Addict. Behav. 2014, 39, 1430–1433. [Google Scholar] [CrossRef]
- Cassidy, R.N.; Meisel, M.K.; DiGuiseppi, G.; Balestrieri, S.; Barnett, N.P. Initiation of vaporizing cannabis: Individual and social network predictors in a longitudinal study of young adults. Drug Alcohol Depend. 2018, 188, 334–340. [Google Scholar] [CrossRef]
- Frohe, T.; Leeman, R.F.; Patock-Peckham, J.; Ecker, A.; Kraus, S.; Foster, D.W. Correlates of cannabis vape-pen use and knowledge among US college students. Addict. Behav. Rep. 2018, 7, 32–39. [Google Scholar]
- Malouff, J.M.; Rooke, S.E.; Copeland, J. Experiences of marijuana-vaporizer users. Subst. Abus. 2014, 35, 127–128. [Google Scholar] [CrossRef]
- Loflin, M.; Earleywine, M. No smoke, no fire: What the initial literature suggests regarding vapourized cannabis and respiratory risk. Can. J. Respir. Ther. 2015, 51, 7–9. [Google Scholar]
- Harrell, M.B.; Clendennen, S.L.; Sumbe, A.; Case, K.R.; Mantey, D.S.; Swan, S. Cannabis vaping among youth and young adults: A scoping review. Curr. Addict. Rep. 2022, 9, 217–234. [Google Scholar] [CrossRef] [PubMed]
- Vanderbruggen, N.; Matthys, F.; Van Laere, S.; Zeeuws, D.; Santermans, L.; Van den Ameele, S.; Crunelle, C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: Results from a web-based survey. Eur. Addict. Res. 2020, 26, 309–315. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2020: Trends and Developments; Publications Office of the European Union: Luxembourg, 2022. [Google Scholar]
- Caulkins, J.P.; Pardo, B.; Kilmer, B. Intensity of cannabis use: Findings from three online surveys. Int. J. Drug Policy 2020, 79, 102740. [Google Scholar] [CrossRef]
- Walden, N.; Earleywine, M. How high: Quantity as a predictor of cannabis-related problems. Harm Reduct. J. 2008, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Matheson, J.; Sproule, B.; Di Ciano, P.; Fares, A.; Le Foll, B.; Mann, R.E.; Brands, B. Sex differences in the acute effects of smoked cannabis: Evidence from a human laboratory study of young adults. Psychopharmacology 2020, 237, 305–316. [Google Scholar] [CrossRef]
| Legalization | EVALI | COVID-19 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Before October 2018 | Since October 2018 | Before November 2019 | Since November 2019 | Before March 2020 | Since March 2020 | ||
| Forms (units) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Dried Herb (grams) | |||||||
| Total n = 177 | 1.1 (1.8) | 1.3 (1.1) | 1.3 (1.1) | 1.3 (1.1) | 1.4 (2.1) | 1.5 (2.3) | <0.001 ‡ |
| Males n = 76 | 1.6 (0.23) | 1.7 (2.3) | 1.7 (2.3) | 1.7 (2.3) | 1.7 (2.3) | 1.9 (2.6) | 0.41 † |
| Females n = 101 | 0.67 (1.2) a | 1.0 (1.7) a | 1.0 (1.7) | 1.1 (1.7) | 1.1 (1.9) | 1.2 (2.1) | 0.004 † |
| Joint Size (grams) | |||||||
| Total n = 83 | 0.61 (0.43) | 0.74 (0.36) | 0.68 (0.39) | 0.73 (0.36) | 0.69 (0.38) | 0.66 (0.43) | <0.001 ‡ |
| Males n = 26 | 0.72 (0.41) | 0.81 (0.34) | 0.75 (0.35) | 0.82 (0.31) | 0.76 (0.32) | 0.76 (0.39) | 0.17 † |
| Females n = 57 | 0.56 (0.43) | 0.71 (0.37) | 0.64 (0.40) | 0.68 (0.37) | 0.66 (0.40) | 0.62 (0.44) | 0.049 † |
| Number of Joints | |||||||
| Total n = 84 | 0.77 (0.88) | 0.98 (0.97) | 0.88 (0.94) | 0.96 (0.97) | 0.90 (0.91) | 1.1 (1.3) | <0.001 ‡ |
| Males n = 27 | 1.2 (1.1) | 1.5 (1.2) | 1.3 (1.2) | 1.6 (1.2) | 1.3 (1.1) | 1.4 (1.5) | 0.049 † |
| Females n = 57 | 0.58 (0.70) | 0.72 (0.70) | 0.66 (0.70) | 0.68 (0.69) | 0.72 (0.78) | 0.86 (1.1) | 0.006 † |
| Hash (grams) | |||||||
| Total n = 13 | 0.42 (0.52) | 0.52 (0.54) | 0.40 (0.26) | 0.33 (0.19) | 0.25 (0.23) | 0.33 (0.30) | <0.001 ‡ |
| Males n = 4 | 0.38 (0.25) | 0.69 (0.38) | 0.44 (0.13) | 0.44 (0.13) | 0.44 (0.13) | 0.44 (0.13) | 0.15 b |
| Females n = 9 | 0.44 (0.62) | 44 (0.61) | 0.39 (0.31) | 0.28 (0.195) | 0.17 (0.22) | 0.28 (0.341) | 0.39 b |
| Concentrates (grams) | |||||||
| Total n = 28 | 0.32 (0.45) | 0.41 (0.31) | 0.44 (0.43) | 0.43 (0.31) | 0.46 (0.42) | 0.57 (0.51) | <0.001 ‡ |
| Males n = 16 | 0.39 (0.54) | 0.47 (0.35) | 0.53 (0.51) | 0.50 (0.33) | 0.56 (0.49) | 0.63( 0.51) | 0.40 † |
| Females n = 12 | 0.23 (0.29) | 0.33 (0.25) | 0.31 (0.26) | 0.33 (0.27) | 0.33 (0.27) | 0.50 (0.53) | 0.11 † |
| Vapes (number of cartridges) | |||||||
| Total n = 46 | 0.35 (0.80) | 0.71 (1.1) | 0.74 (1.2) | 0.82 (1.1) | 0.82 (1.3) | 1.1 (1.5) | <0.001 ‡ |
| Males n = 17 | 0.50 (1.2) | 0.97 (1.3) | 1.2 (1.5) | 1.0 (1.3) | 1.2 (1.9) | 1.4 (2.0) | 0.29 † |
| Females n = 29 | 0.26 (0.46) | 0.55 (0.99) | 0.47 (0.82) | 0.69 (0.97) | 0.62 (0.66) | 0.87 (1.1) | 0.048 † |
| Legalization | EVALI | COVID-19 | p-Value † | ||||
|---|---|---|---|---|---|---|---|
| Before October 2018 | Since October 2018 | Before November 2019 | Since November 2019 | Before March 2020 | Since March 2020 | ||
| Form (units) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Dried Herb (grams) | |||||||
| Total n = 173 | 15.75 (44.01) | 22.58 (50.70) | 23.39 (55.84) | 26.72 (58.50) | 28.62 (58.50) | 34.44 (67.56) | <0.001 |
| Males n = 73 | 24.15 (56.20) | 30.17 (61.45) | 31.92 (66.41) | 35.42 (70.57) | 36.19 (70.44) | 39.24 (73.94) | 0.097 |
| Females n = 100 | 9.62 (31.39) ab | 17.05 (40.59) | 17.18 (46.02) | 20.36 (47.19) | 23.09 (53.07) a | 30.94 (62.65) b | <0.001 |
| Joints (grams) | |||||||
| Total n = 80 | 11.42 (29.95) | 14.62 (32.97) | 13.83 (33.02) | 14.36 (32.88) | 15.24 (31.85) | 21.25 (43.61) | 0.003 |
| Males n = 26 | 21.98 (43.80) | 27.15 (47.29) | 26.23 (47.73) | 27.18 (47.26) | 23.63 (42.05) | 36.05 (58.94) | 0.083 |
| Females n = 54 | 6.33 (18.73) | 8.59 (21.24) | 7.85 (20.95) | 8.19 (20.93) | 11.20 (25.03) | 14.13 (32.21) | 0.022 |
| Vapes (number of cartridges) | |||||||
| Total n = 44 | 0.83 (2.83) | 1.97 (4.44) | 4.44 (18.29) | 4.81 (18.27) | 2.64 (5.84) | 10.03 (33.47) | 0.179 |
| Males n = 16 | 1.33 (4.30) | 2.55 (5.04) | 3.63 (5.78) | 3.64 (5.78) | 4.49 (8.50) | 17.06 (51.82) | 0.277 |
| Females n = 28 | 0.55 (1.49) | 1.63 (4.11) | 4.90 (22.61) | 5.48 (22.62) | 1.58 (3.31) | 6.00 (15.68) | 0.384 |
| Before Legalization (October 2018) | Between Legalization and EVALI (October 2018 to November 2019) | Between EVALI and COVID-19 (November 2019 to March 2020) | Since COVID-19 (March 2020) | p-Value † | |
|---|---|---|---|---|---|
| Forms (unit) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Dried Herb (grams) | |||||
| Light user (n = 37) | 0.42 (1.15) | 0.61 (1.42) | 0.54 (0.91) | 0.43 (0.77) | 0.617 |
| Heavy user (n = 138) | 1.24 (1.91) abc | 1.50 (2.03) a | 1.59 (2.14) b | 1.79 (2.49) c | <0.001 |
| Joints (grams) | |||||
| Light user (n = 36) | 0.32 (0.33) | 0.34 (0.29) | 0.32 (0.28) | 0.28 (0.39) | 0.507 |
| Heavy user (n = 44) | 0.99 (1.21) abc | 1.22 (1.26) a | 1.25 (1.20) b | 1.61 (1.67) c | <0.001 |
| Vapes (number of vaping cartridges) | |||||
| Light user (n = 26) | 0.23 (0.48) ab | 0.70 (1.03) | 0.76 (0.74) a | 1.11 (1.11) b | 0.005 |
| Heavy user (n = 12) | 0.81 (1.31) | 1.19 (1.28) | 1.39 (1.70) | 1.69 (2.27) | 0.360 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yousufzai, S.J.; Cole, A.G.; Nonoyama, M.; Barakat, C. Changes in Quantity Measures of Various Forms of Cannabis Consumption among Emerging Adults in Canada in Relation to Policy and Public Health Developments. Int. J. Environ. Res. Public Health 2023, 20, 6213. https://doi.org/10.3390/ijerph20136213
Yousufzai SJ, Cole AG, Nonoyama M, Barakat C. Changes in Quantity Measures of Various Forms of Cannabis Consumption among Emerging Adults in Canada in Relation to Policy and Public Health Developments. International Journal of Environmental Research and Public Health. 2023; 20(13):6213. https://doi.org/10.3390/ijerph20136213
Chicago/Turabian StyleYousufzai, Susan J., Adam G. Cole, Mika Nonoyama, and Caroline Barakat. 2023. "Changes in Quantity Measures of Various Forms of Cannabis Consumption among Emerging Adults in Canada in Relation to Policy and Public Health Developments" International Journal of Environmental Research and Public Health 20, no. 13: 6213. https://doi.org/10.3390/ijerph20136213
APA StyleYousufzai, S. J., Cole, A. G., Nonoyama, M., & Barakat, C. (2023). Changes in Quantity Measures of Various Forms of Cannabis Consumption among Emerging Adults in Canada in Relation to Policy and Public Health Developments. International Journal of Environmental Research and Public Health, 20(13), 6213. https://doi.org/10.3390/ijerph20136213








