Defining the Characteristics of an e-Health Tool for Suicide Primary Prevention in the General Population: The StopBlues Case in France
Abstract
1. Introduction
1.1. Background
1.2. Objectives
2. Materials and Methods
2.1. Review of the Literature and of Experience
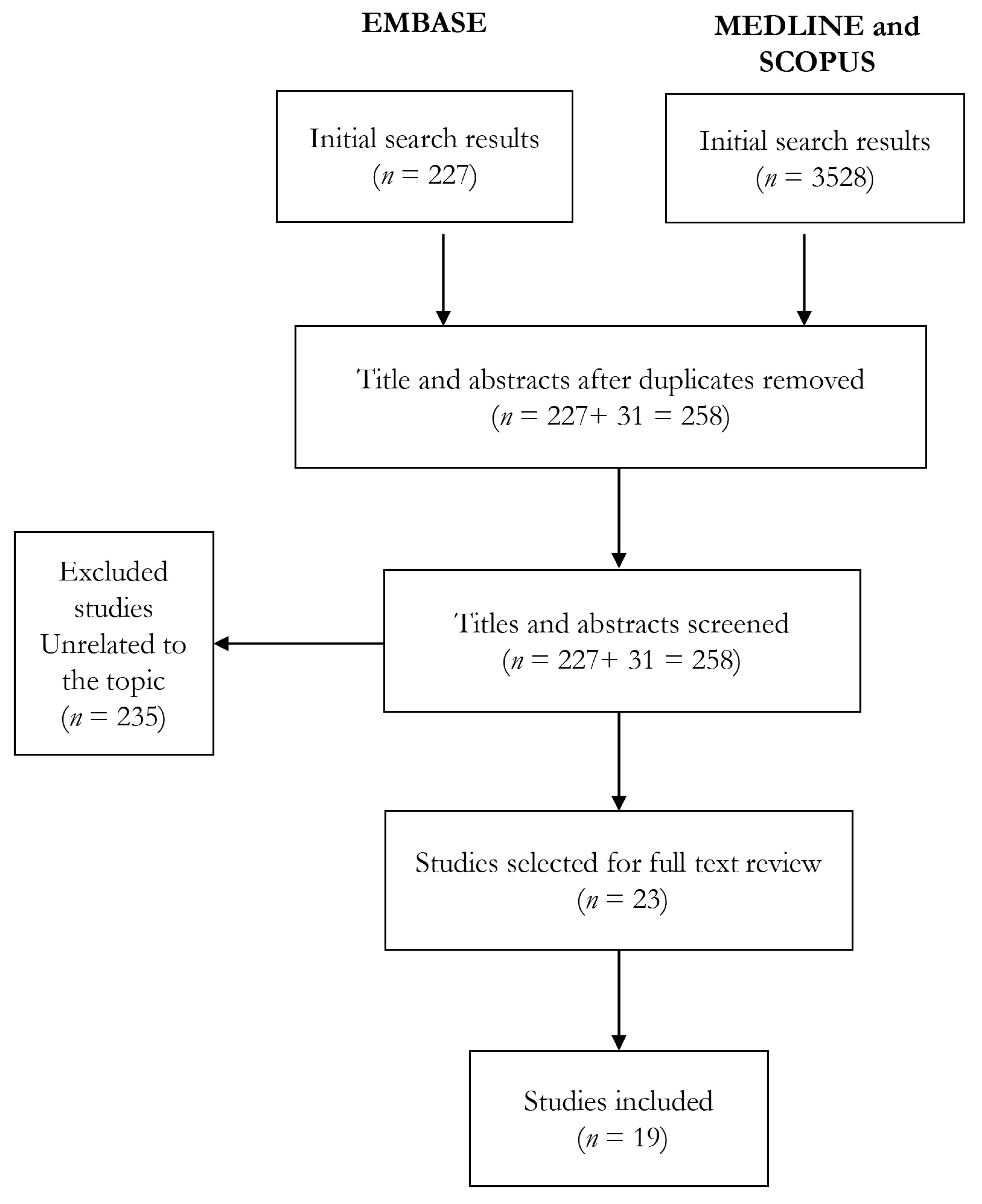
2.1.1. Literature Review
2.1.2. Review of Experience
2.2. Focus Group
2.2.1. Rationale
2.2.2. Participants
2.2.3. Procedure
2.2.4. Analysis
2.3. Experts’ Interview
3. Results
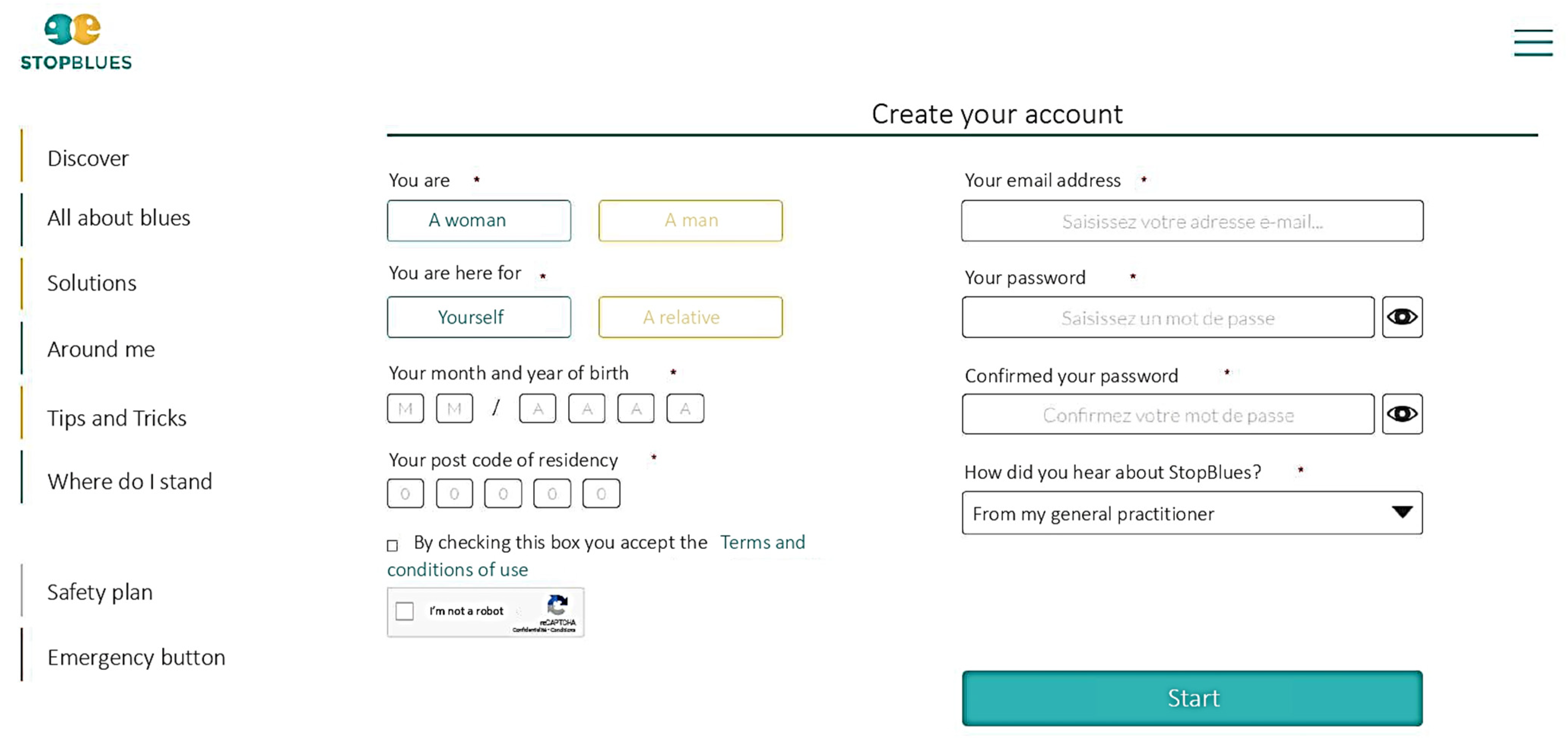
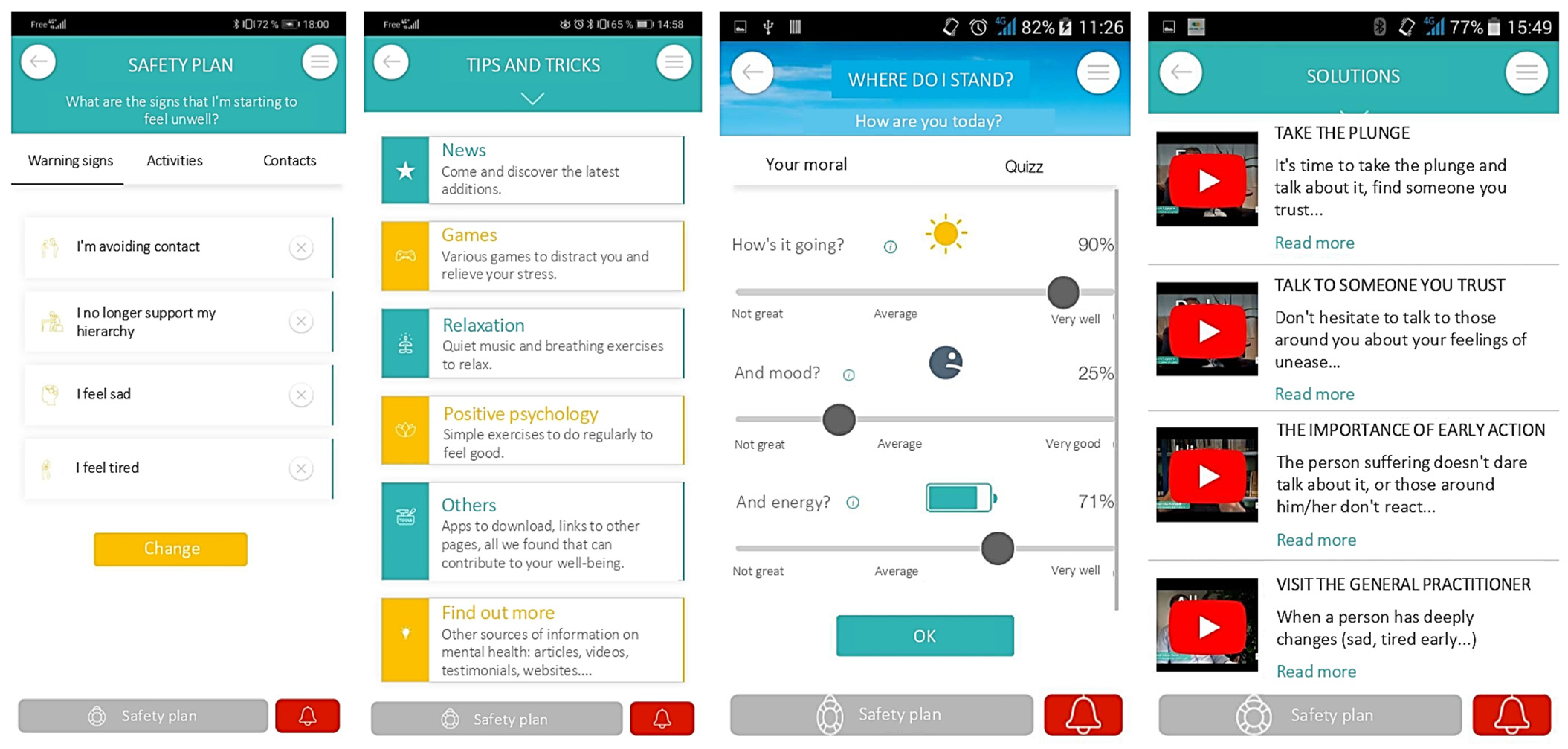
3.1. Characteristics of IT Features
3.2. Content and Structure of the Information
3.2.1. Awareness Strategies to Improve Knowledge in the Target Population
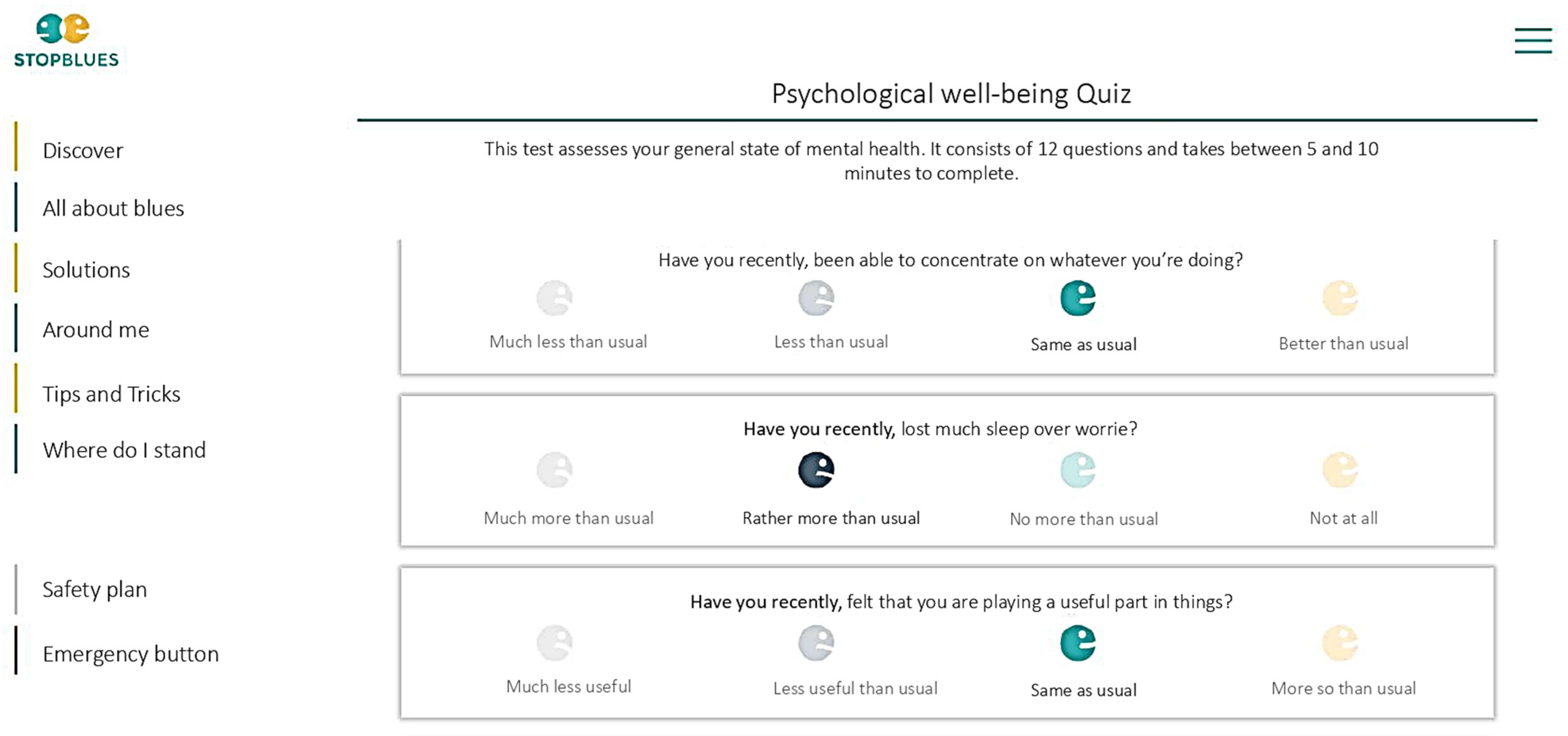
3.2.2. Self-Screening Strategies to Improve Recognition of Suicide Risk and Self-Awareness among the Target Population
3.2.3. Accessing Support Strategies to Improve Access to Help and Treatment for Those Who Need It
3.2.4. Mental Health Strategies to Improve Prevention of Psychological Distress and Suicide
3.3. Structure
3.4. Delivery of Information
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CBHP | community-based health promotion |
| GP | general practitioner |
| INSERM | French National Institute of Health and Medical Research |
| SB | StopBlues |
| WHO | World Health Organization |
| GHQ-12 | Twelve-item General Health Questionnaire |
| PHQ-9 | Nine-item Patient Health Questionnaire |
| GAD-7 | Seven-item Generalized Anxiety Disorder |
| SF-12 | Twelve-item Short-Form Health Survey |
| MINI suicide | Mini International Neuropsychiatric Interview suicidality module |
Appendix A
| # | Keywords | Number of Publications |
|---|---|---|
| 1 | ‘suicide’/exp OR (‘suicide’/exp OR suicide:ab,ti AND (‘gesture’/exp OR gesture:ab,ti OR attempt:ab,ti OR ‘risk’/exp OR risk:ab,ti)) OR ‘suicidal ideation’/exp OR ‘suicidal ideation’:ab,ti OR (‘para suicidal’:ab,ti OR parasuicidal:ab,ti OR suicidal:ab,ti OR ‘suicide related’:ab,ti AND (‘behaviour’/exp OR behaviour:ab,ti OR ‘behavior’/exp OR behavior:ab,ti OR feelings:ab,ti OR thoughts:ab,ti)) OR ‘fatal self-harm’:ab,ti OR ‘fatal self harm’:ab,ti OR ‘fatal self injury’:ab,ti OR ‘fatal self-injury’:ab,ti OR ‘self-destructive:ab,ti and (behavior or behaviour):ab,ti’ OR ‘self destructive behaviour’:ab,ti OR ‘intentional life threatening behaviour’:ab,ti OR ‘intentional life threatening behavior’:ab,ti OR ‘self-cutting’:ab,ti OR ‘self cutting’:ab,ti OR ‘self inflicted wounds’:ab,ti OR ‘self-inflicted wounds’:ab,ti OR (deliberate:ab,ti AND (‘self cutting’:ab,ti OR ‘self poisoning’/exp OR ‘self poisoning’:ab,ti)) OR (‘self poisoning’/exp OR ‘self poisoning’:ab,ti AND (‘overdose’/exp OR overdose:ab,ti)) OR ‘drug overdose’/exp OR ‘drug overdose’:ab,ti OR ‘overdose’/exp OR overdose:ab,ti OR (‘non fatal’:ab,ti OR nonfatal:ab,ti OR fatal:ab,ti OR suicidal:ab,ti AND (‘self harm’/exp OR ‘self harm’:ab,ti OR ‘self injury’/exp OR ‘self injury’:ab,ti OR ‘self mutilation’/exp OR ‘self mutilation’:ab,ti OR ‘auto-mutilation’:ab,ti OR ‘automutilation’/exp OR automutilation:ab,ti)) OR ‘self injurious’:ab,ti OR ‘self-inflicted violence’:ab,ti OR ‘self intoxication’:ab,ti OR ‘self-directed violence’:ab,ti OR dsh:ab,ti OR sh:ab,ti OR si:ab,ti OR ‘sib’/exp OR sib:ab,ti OR ‘siv’/exp OR siv:ab,ti | 528,631 |
| 2 | ‘web based’:ab,ti OR ‘internet based’:ab,ti OR ‘computer based’:ab,ti OR ‘cyber based’:ab,ti OR ‘internet mediated’:ab,ti OR ‘internet supported’:ab,ti OR ‘computer supported’:ab,ti OR ‘computer mediated’:ab,ti OR ‘web mediated’:ab,ti OR ‘web supported’:ab,ti OR ‘mobile health’:ab,ti AND (therapy:ab,ti OR intervention*:ab,ti OR prevention:ab,ti OR ‘prevention program’:ab,ti OR ‘prevention programme’:ab,ti OR ‘preventative tool’:ab,ti) OR ‘cyber intervention’:ab,ti OR ‘internet-supported therapeutic intervention’:ab,ti OR internet:ab,ti OR web:ab,ti OR technolog*:ab,ti OR online:ab,ti OR computer:ab,ti OR cyber*:ab,ti OR net:ab,ti OR virtual:ab,ti OR surf:ab,ti OR ‘electronic mail’:ab,ti OR email:ab,ti OR ‘e mail’:ab,ti OR forum:ab,ti OR ‘social media platform’:ab,ti OR site:ab,ti OR www:ab,ti OR eintervention:ab,ti OR ‘e intervention’:ab,ti OR ‘e therapy’:ab,ti OR etherapy:ab,ti OR ‘e health’:ab,ti OR ehealth:ab,ti OR mhealth:ab,ti OR (mobile:ab,ti AND health:ab,ti AND (app:ab,ti OR application:ab,ti)) | 1,613,911 |
| 3 | #1 AND #2 | 20,700 |
| 4 | Limit 3 to humans | 10,392 |
| 5 | #4 AND (‘camera’/de OR ‘computer’/de OR ‘computer system’/de OR ‘film’/de OR ‘mobile phone’/de OR ‘telephone’/de) AND (‘depression’/de OR ‘drug intoxication’/de OR ‘intoxication’/de OR ‘major depression’/de OR ‘mental disease’/de OR ‘schizophrenia’/de OR ‘suicidal behavior’/de OR ‘suicidal ideation’/de OR ‘suicide’/de OR ‘suicide attempt’/de) AND ‘human’/de | 227 |
References
- WHO. Preventing Suicide: A Global Imperative; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- WHO. Suicide Worldwide in 2019: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-002664-3. [Google Scholar]
- Kendall, T.; Taylor, C.; Bhatti, H.; Chan, M.; Kapur, N. Guideline Development Group of the National Institute for Health and Clinical Excellence Longer Term Management of Self Harm: Summary of NICE Guidance. BMJ 2011, 343, d7073. [Google Scholar] [CrossRef] [PubMed]
- Nakao, M.; Takeuchi, T. The Suicide Epidemic in Japan and Strategies of Depression Screening for Its Prevention. Bull. World Health Organ. 2006, 84, 492–493. [Google Scholar] [CrossRef]
- Matsubayashi, T.; Ueda, M. The Effect of National Suicide Prevention Programs on Suicide Rates in 21 OECD Nations. Soc. Sci. Med. 2011, 73, 1395–1400. [Google Scholar] [CrossRef]
- Office of the Surgeon General (US); National Action Alliance for Suicide Prevention (US). 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention; Publications and Reports of the Surgeon General; US Department of Health & Human Services (US): Washington, DC, USA, 2012. [Google Scholar]
- Bruffaerts, R.; Demyttenaere, K.; Hwang, I.; Chiu, W.-T.; Sampson, N.; Kessler, R.C.; Alonso, J.; Borges, G.; de Girolamo, G.; de Graaf, R.; et al. Treatment of Suicidal People around the World. Br. J. Psychiatry 2011, 199, 64–70. [Google Scholar] [CrossRef]
- Czyz, E.K.; Horwitz, A.G.; Eisenberg, D.; Kramer, A.; King, C.A. Self-Reported Barriers to Professional Help Seeking among College Students at Elevated Risk for Suicide. J. Am. Coll. Health 2013, 61, 398–406. [Google Scholar] [CrossRef]
- Reynders, A.; Kerkhof, A.J.F.M.; Molenberghs, G.; Van Audenhove, C. Attitudes and Stigma in Relation to Help-Seeking Intentions for Psychological Problems in Low and High Suicide Rate Regions. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 231–239. [Google Scholar] [CrossRef]
- Schomerus, G.; Schwahn, C.; Holzinger, A.; Corrigan, P.W.; Grabe, H.J.; Carta, M.G.; Angermeyer, M.C. Evolution of Public Attitudes about Mental Illness: A Systematic Review and Meta-Analysis. Acta Psychiatr. Scand. 2012, 125, 440–452. [Google Scholar] [CrossRef]
- Buchman-Wildbaum, T.; Paksi, B.; Sebestyén, E.; Kun, B.; Felvinczi, K.; Schmelowszky, Á.; Griffiths, M.D.; Demetrovics, Z.; Urbán, R. Social Rejection towards Mentally Ill People in Hungary between 2001 and 2015: Has There Been Any Change? Psychiatry Res. 2018, 267, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Medina, T.R.; Martin, J.K.; Long, J.S. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated with Mental Illness. Am. J. Public Health 2013, 103, 853–860. [Google Scholar] [CrossRef]
- Yin, H.; Wardenaar, K.J.; Xu, G.; Tian, H.; Schoevers, R.A. Mental Health Stigma and Mental Health Knowledge in Chinese Population: A Cross-Sectional Study. BMC Psychiatry 2020, 20, 323. [Google Scholar] [CrossRef] [PubMed]
- Roelandt, J.-L.; Caria, A.; Defromont, L.; Vandeborre, A.; Daumerie, N. Representations of insanity, mental illness and depression in general population in France. Encephale 2010, 36, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.; Marusic, A.; et al. Suicide Prevention Strategies: A Systematic Review. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef] [PubMed]
- Ernst, C.; Lalovic, A.; Lesage, A.; Seguin, M.; Tousignant, M.; Turecki, G. Suicide and No Axis I Psychopathology. BMC Psychiatry 2004, 4, 7. [Google Scholar] [CrossRef]
- Zalsman, G.; Hawton, K.; Wasserman, D.; van Heeringen, K.; Arensman, E.; Sarchiapone, M.; Carli, V.; Höschl, C.; Barzilay, R.; Balazs, J.; et al. Suicide Prevention Strategies Revisited: 10-Year Systematic Review. Lancet Psychiatry 2016, 3, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Robinson-Link, N.; Hoover, S.; Bernstein, L.; Lever, N.; Maton, K.; Wilcox, H. Is Gatekeeper Training Enough for Suicide Prevention? Sch. Ment. Health 2020, 12, 239–249. [Google Scholar] [CrossRef]
- Dueweke, A.R.; Bridges, A.J. Suicide Interventions in Primary Care: A Selective Review of the Evidence. Fam. Syst. Health 2018, 36, 289–302. [Google Scholar] [CrossRef]
- Platt, S.; Niederkrotenthaler, T. Suicide Prevention Programs. Crisis 2020, 41, S99–S124. [Google Scholar] [CrossRef]
- 12e Observatoire S.O.S Amitié Des Souffrances Psychiques 2022 (Chiffres Année 2021). Available online: https://www.sosamitieidf.asso.fr/wp-content/uploads/2022/05/12e-observatoire-des-souffrances-psychiques-2022.pdf (accessed on 25 May 2023).
- World Health Organization. Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Laanani, M.; Imbaud, C.; Tuppin, P.; Poulalhon, C.; Jollant, F.; Coste, J.; Rey, G. Contacts with Health Services During the Year Prior to Suicide Death and Prevalent Conditions a Nationwide Study. J. Affect. Disord. 2020, 274, 174–182. [Google Scholar] [CrossRef]
- Gagné, S.; Vasiliadis, H.-M.; Préville, M. Gender Differences in General and Specialty Outpatient Mental Health Service Use for Depression. BMC Psychiatry 2014, 14, 135. [Google Scholar] [CrossRef]
- WHO. EHealth. Available online: http://www.who.int/ehealth/en/ (accessed on 1 August 2020).
- Harrison, V.; Proudfoot, J.; Wee, P.P.; Parker, G.; Pavlovic, D.H.; Manicavasagar, V. Mobile Mental Health: Review of the Emerging Field and Proof of Concept Study. J. Ment. Health 2011, 20, 509–524. [Google Scholar] [CrossRef]
- Durkee, T.; Hadlaczky, G.; Westerlund, M.; Carli, V. Internet Pathways in Suicidality: A Review of the Evidence. Int. J. Environ. Res. Public Health 2011, 8, 3938–3952. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.H.; Maniam, T.; Chan, L.F.; Ravindran, A.V. Caught in the Web: A Review of Web-Based Suicide Prevention. J. Med. Internet Res. 2014, 16, e30. [Google Scholar] [CrossRef]
- McDaid, D.; Park, A.-L. Online Health: Untangling the Web. In Bupa Health Pulse Survey and Results; BUPA: London, UK, 2011. [Google Scholar]
- Larsen, M.E.; Nicholas, J.; Christensen, H. A Systematic Assessment of Smartphone Tools for Suicide Prevention. PLoS ONE 2016, 11, e0152285. [Google Scholar] [CrossRef] [PubMed]
- Donker, T.; Petrie, K.; Proudfoot, J.; Clarke, J.; Birch, M.-R.; Christensen, H. Smartphones for Smarter Delivery of Mental Health Programs: A Systematic Review. J. Med. Internet Res. 2013, 15, e247. [Google Scholar] [CrossRef] [PubMed]
- Torous, J.; Firth, J.; Huckvale, K.; Larsen, M.E.; Cosco, T.D.; Carney, R.; Chan, S.; Pratap, A.; Yellowlees, P.; Wykes, T.; et al. The Emerging Imperative for a Consensus Approach Toward the Rating and Clinical Recommendation of Mental Health Apps. J. Nerv. Ment. Dis. 2018, 206, 662–666. [Google Scholar] [CrossRef]
- Henderson, C.; Gronholm, P.C. Mental Health Related Stigma as a ‘Wicked Problem’: The Need to Address Stigma and Consider the Consequences. Int. J. Environ. Res. Public Health 2018, 15, 1158. [Google Scholar] [CrossRef] [PubMed]
- Erlandsen, M.A. User Involvement in Mental Health and Substance Abuse: Myth or Reality? Exploring the Role of User Involvement in Clinical Pathway Development. Master’s Thesis, University of Oslo, Oslo, Norway, May 2017. [Google Scholar]
- WHO. Mental Health Gap Action Programme (MhGAP); World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- 2e Rapport de l’Observatoire National Du Suicide—SUICIDE Connaître Pour Prévenir: Dimensions Nationales, Locales et Associatives; Rapport de l’Observatoire National Du Suicide; DREES/InVS; Ministry of Solidarites and Health: Paris, France, 2016.
- Haute Autorité de Santé. La Crise Suicidaire: Reconnaître et Prendre en Charge; H.A.S: Saint-Denis La Plaine, France, 2000. [Google Scholar]
- Fossi Djembi, L.; Vaiva, G.; Debien, C.; Duhem, S.; Demarty, A.-L.; Koudou, Y.-A.; Messiah, A. Changes in the Number of Suicide Re-Attempts in a French Region since the Inception of VigilanS, a Regionwide Program Combining Brief Contact Interventions (BCI). BMC Psychiatry 2020, 20, 26. [Google Scholar] [CrossRef]
- Nunes, A.; Castro, S.L.; Limpo, T. A Review of Mindfulness-Based Apps for Children. Mindfulness 2020, 11, 2089–2101. [Google Scholar] [CrossRef]
- Happli Daypour iPhone sur l’App Store. Available online: https://iphoneaddict.fr/apps/medecine/happli-day.html (accessed on 25 May 2023).
- Seventh Framework Programme of the European Community for Research and Technological Development Including Demonstration Activities (FP7) | Programme | FP7 | CORDIS | European Commission. Available online: https://cordis.europa.eu/programme/id/FP7 (accessed on 31 August 2021).
- Kitzinger, J. Qualitative Research. Introducing Focus Groups. BMJ 1995, 311, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Powell, R.A.; Single, H.M.; Lloyd, K.R. Focus Groups in Mental Health Research: Enhancing the Validity of User and Provider Questionnaires. Int. J. Soc. Psychiatry 1996, 42, 193–206. [Google Scholar] [CrossRef]
- Breen, R.L. A Practical Guide to Focus-Group Research. J. Geogr. High. Educ. 2006, 30, 463–475. [Google Scholar] [CrossRef]
- Morgan, D.L. Focus Groups as Qualitative Research; SAGE: Newcastle Upon Tyne, UK, 1997; ISBN 978-0-7619-0343-7. [Google Scholar]
- Etikan, I.; Musa, S.A.; Alkassim, R.S. Comparison of Convenience Sampling and Purposive Sampling. Am. J. Theor. Appl. Stat. 2015, 5, 1. [Google Scholar] [CrossRef]
- Wong, L.P. Focus Group Discussion: A Tool for Health and Medical Research. Singap. Med. J. 2008, 49, 256–260. [Google Scholar]
- Paillé, P.; Mucchielli, A. Chapitre 11—L’analyse thématique. In L’analyse Qualitative en Sciences Humaines et Sociales, Collection U; Armand Colin: Paris, France, 2012; pp. 231–314. ISBN 978-2-200-24904-5. [Google Scholar]
- Meuser, M.; Nagel, U. The Expert Interview and Changes in Knowledge Production. In Interviewing Experts; Bogner, A., Littig, B., Menz, W., Eds.; Research Methods Series; Palgrave Macmillan: London, UK, 2009; pp. 17–42. ISBN 978-0-230-24427-6. [Google Scholar]
- Gläser, J.; Laudel, G. On Interviewing “Good” and “Bad” Experts. In Interviewing Experts; Research Methods Series; Palgrave Macmillan: London, UK, 2009. [Google Scholar]
- Lambert, S.D.; Loiselle, C.G. Combining Individual Interviews and Focus Groups to Enhance Data Richness. J. Adv. Nurs. 2008, 62, 228–237. [Google Scholar] [CrossRef]
- Arensman, E.; Koburger, N.; Larkin, C.; Karwig, G.; Coffey, C.; Maxwell, M.; Harris, F.; Rummel-Kluge, C.; van Audenhove, C.; Sisask, M.; et al. Depression Awareness and Self-Management Through the Internet: Protocol for an Internationally Standardized Approach. JMIR Res. Protoc. 2015, 4, e99. [Google Scholar] [CrossRef]
- Justicia, A.; Elices, M.; Cebria, A.I.; Palao, D.J.; Gorosabel, J.; Puigdemont, D.; de Diego-Adeliño, J.; Gabilondo, A.; Iruin, A.; Hegerl, U.; et al. Rationale and Methods of the IFightDepression Study: A Double-Blind, Randomized Controlled Trial Evaluating the Efficacy of an Internet-Based Self-Management Tool for Moderate to Mild Depression. BMC Psychiatry 2017, 17, 143. [Google Scholar] [CrossRef] [PubMed]
- De Jaegere, E.; Portzky, G.; van den Berg, M.; Wallyn, S. Ethical Guidelines for Technology-Based Suicide Prevention Programmes WP 5; Euregenas; Ghent University, Flemish Agency for Care and Health: Ghent, Belgium, 2013. [Google Scholar]
- Muñoz-Sánchez, J.-L.; Delgado, C.; Sánchez-Prada, A.; Pérez-López, M.; Franco-Martín, M.A. Use of New Technologies in the Prevention of Suicide in Europe: An Exploratory Study. JMIR Ment. Health 2017, 4, e23. [Google Scholar] [CrossRef]
- Jorm, A.F.; Christensen, H.; Griffiths, K.M. The Impact of Beyondblue: The National Depression Initiative on the Australian Public’s Recognition of Depression and Beliefs about Treatments. Aust. N. Z. J. Psychiatry 2005, 39, 248–254. [Google Scholar] [CrossRef]
- Pirkis, J.; Hickie, I.; Young, L.; Burns, J.; Highet, N.; Davenport, T. An Evaluation of Beyondblue, Australia’s National Depression Initiative. Int. J. Ment. Health Promot. 2005, 7, 35–53. [Google Scholar] [CrossRef]
- Hegerl, U.; Wittenburg, L.; Arensman, E.; Audenhove, C.V.; Coyne, J.C.; McDaid, D.; van der Feltz-Cornelis, C.M.; Gusmão, R.; Kopp, M.; Maxwell, M.; et al. Optimizing Suicide Prevention Programs and Their Implementation in Europe (OSPI Europe): An Evidence-Based Multi-Level Approach. BMC Public Health 2009, 9, 428. [Google Scholar] [CrossRef] [PubMed]
- Hegerl, U.; Maxwell, M.; Harris, F.; Koburger, N.; Mergl, R.; Székely, A.; Arensman, E.; Van Audenhove, C.; Larkin, C.; Toth, M.D.; et al. Prevention of Suicidal Behaviour: Results of a Controlled Community-Based Intervention Study in Four European Countries. PLoS ONE 2019, 14, e0224602. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, K.; Aerts, S.; Muijzers, E.; De Jaegere, E.; van Heeringen, K.; Portzky, G. BackUp: Development and Evaluation of a Smart-Phone Application for Coping with Suicidal Crises. PLoS ONE 2017, 12, e0178144. [Google Scholar] [CrossRef] [PubMed]
- Skovgaard Larsen, J.L.; Frandsen, H.; Erlangsen, A. MYPLAN—A Mobile Phone Application for Supporting People at Risk of Suicide. Crisis 2016, 37, 236–240. [Google Scholar] [CrossRef]
- Suicide Prevention App Awarded $50,000 Prize at White House Conference. Available online: https://news.emory.edu/stories/2013/09/kaslow_relieflink_app/campus.html (accessed on 5 June 2023).
- Andreasson, K.; Krogh, J.; Bech, P.; Frandsen, H.; Buus, N.; Stanley, B.; Kerkhof, A.; Nordentoft, M.; Erlangsen, A. MYPLAN -Mobile Phone Application to Manage Crisis of Persons at Risk of Suicide: Study Protocol for a Randomized Controlled Trial. Trials 2017, 18, 171. [Google Scholar] [CrossRef]
- Buus, N.; Juel, A.; Haskelberg, H.; Frandsen, H.; Larsen, J.L.S.; River, J.; Andreasson, K.; Nordentoft, M.; Davenport, T.; Erlangsen, A. User Involvement in Developing the MYPLAN Mobile Phone Safety Plan App for People in Suicidal Crisis: Case Study. JMIR Ment. Health 2019, 6, e11965. [Google Scholar] [CrossRef]
- Buus, N.; Erlangsen, A.; River, J.; Andreasson, K.; Frandsen, H.; Larsen, J.L.S.; Nordentoft, M.; Juel, A. Stakeholder Perspectives on Using and Developing the MYPLAN Suicide Prevention Mobile Phone Application: A Focus Group Study. Arch. Suicide Res. 2018, 24, 48–63. [Google Scholar] [CrossRef] [PubMed]
- Kaslow, N. ReliefLink: A Preventative Mobile Toolkit for Follow-Up Care of Psychiatric Patients. Available online: https://clinicaltrials.gov/ct2/show/NCT02691221 (accessed on 18 April 2019).
- CREDOC. Baromètre du Numérique 2021—Enquête sur la Diffusion des Technologies de L’information et de la Communication dans la Société Française; ARCEP: Paris, France, 2021; p. 349. [Google Scholar]
- Parts de Marché OS Mobile. Available online: https://www.kantarworldpanel.com/fr/smartphone-os-market-share/ (accessed on 2 August 2018).
- Hébergement des Données de Santé. Available online: https://esante.gouv.fr/labels-certifications/hebergement-des-donnees-de-sante (accessed on 25 November 2021).
- Arango, C.; Díaz-Caneja, C.M.; McGorry, P.D.; Rapoport, J.; Sommer, I.E.; Vorstman, J.A.; McDaid, D.; Marín, O.; Serrano-Drozdowskyj, E.; Freedman, R.; et al. Preventive Strategies for Mental Health. Lancet Psychiatry 2018, 5, 591–604. [Google Scholar] [CrossRef]
- BinDhim, N.F.; Alanazi, E.M.; Aljadhey, H.; Basyouni, M.H.; Kowalski, S.R.; Pont, L.G.; Shaman, A.M.; Trevena, L.; Alhawassi, T.M. Does a Mobile Phone Depression-Screening App Motivate Mobile Phone Users with High Depressive Symptoms to Seek a Health Care Professional’s Help? J. Med. Internet Res. 2016, 18, e156. [Google Scholar] [CrossRef]
- Campion, J.; Bhui, K.; Bhugra, D. European Psychiatric Association (EPA) Guidance on Prevention of Mental Disorders. Eur. Psychiatry 2012, 27, 68–80. [Google Scholar] [CrossRef]
- Bachmann, S. Epidemiology of Suicide and the Psychiatric Perspective. Int. J. Environ. Res. Public Health 2018, 15, 1425. [Google Scholar] [CrossRef]
- Davidson, C.L.; Wingate, L.R.; Grant, D.M.; Judah, M.R.; Mills, A.C. Interpersonal Suicide Risk and Ideation: The Influence of Depression and Social Anxiety. J. Soc. Clin. Psychol. 2011, 30, 842–855. [Google Scholar] [CrossRef]
- Carmody, J.; Baer, R.A. Relationships between Mindfulness Practice and Levels of Mindfulness, Medical and Psychological Symptoms and Well-Being in a Mindfulness-Based Stress Reduction Program. J. Behav. Med. 2008, 31, 23–33. [Google Scholar] [CrossRef]
- Sitbon, A.; Shankland, R.; Krumm, C.-M. Interventions Efficaces En Psychologie Positive: Une Revue Systématique. Can. Psychol. /Psychol. Can. 2019, 60, 35–54. [Google Scholar] [CrossRef]
- Kruzan, K.P.; Meyerhoff, J.; Nguyen, T.; Reddy, M.; Mohr, D.C.; Kornfield, R. “I Wanted to See How Bad It Was”: Online Self-Screening as a Critical Transition Point Among Young Adults with Common Mental Health Conditions. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 29 April 2022; Association for Computing Machinery: New York, NY, USA, 2022; pp. 1–16. [Google Scholar]
- Bakker, D.; Kazantzis, N.; Rickwood, D.; Rickard, N. Mental Health Smartphone Apps: Review and Evidence-Based Recommendations for Future Developments. JMIR Ment. Health 2016, 3, e7. [Google Scholar] [CrossRef]
- Furnham, A.; Cheng, H. GHQ Score Changes from Teenage to Young Adulthood. J. Psychiatr. Res. 2019, 113, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Lundin, A.; Hallgren, M.; Theobald, H.; Hellgren, C.; Torgén, M. Validity of the 12-Item Version of the General Health Questionnaire in Detecting Depression in the General Population. Public Health 2016, 136, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Malpass, A.; Shaw, A.; Kessler, D.; Sharp, D. Concordance between PHQ-9 Scores and Patients’ Experiences of Depression: A Mixed Methods Study. Br. J. Gen. Pract. 2010, 60, e231–e238. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Kroenke, K.; Herzog, W.; Gräfe, K. Measuring Depression Outcome with a Brief Self-Report Instrument: Sensitivity to Change of the Patient Health Questionnaire (PHQ-9). J. Affect. Disord. 2004, 81, 61–66. [Google Scholar] [CrossRef]
- Donker, T.; van Straten, A.; Marks, I.; Cuijpers, P. Quick and Easy Self-Rating of Generalized Anxiety Disorder: Validity of the Dutch Web-Based GAD-7, GAD-2 and GAD-SI. Psychiatry Res. 2011, 188, 58–64. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P. The Mini International Neuropsychiatric Interview (MINI). A Short Diagnostic Structured Interview: Reliability and Validity According to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar]
- Montgomery, S.A.; Asberg, M. A New Depression Scale Designed to Be Sensitive to Change. Br. J. Psychiatry 1979, 134, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Luxton, D.D.; June, J.D.; Kinn, J.T. Technology-Based Suicide Prevention: Current Applications and Future Directions. Telemed. e-Health 2011, 17, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Monteagudo Pena, J.L.; Moreno Gil, O. EHealth for Patient Empowerment in Europe; World Wide Web electronic publication; Ministery of Health: Madrid, Spain, 2007.
- Roca, M.; Vives, M.; López-Navarro, E.; Garcia-Campayo, J.; Gili, M. Cognitive Impairments and Depression: A Critical Review. Actas Españolas Psiquiatr. 2015, 43, 187–193. [Google Scholar]
- Giota, K.G.; Kleftaras, G. Mental Health Apps: Innovations, Risks and Ethical Considerations. E-Health Telecommun. Syst. Netw. 2014, 3, 19–23. [Google Scholar] [CrossRef]
- Bush, N.E.; Smolenski, D.J.; Denneson, L.M.; Williams, H.B.; Thomas, E.K.; Dobscha, S.K. A Virtual Hope Box: Randomized Controlled Trial of a Smartphone App for Emotional Regulation and Coping with Distress. Psychiatr. Serv. 2017, 68, 330–336. [Google Scholar] [CrossRef]
- Little, V.; Neufeld, J.; Cole, A.R. Integrating Safety Plans for Suicidal Patients into Patient Portals: Challenges and Opportunities. Psychiatr. Serv. 2018, 69, 618–619. [Google Scholar] [CrossRef]
- Melvin, G.A.; Gresham, D.; Beaton, S.; Coles, J.; Tonge, B.J.; Gordon, M.S.; Stanley, B. Evaluating the Feasibility and Effectiveness of an Australian Safety Planning Smartphone Application: A Pilot Study within a Tertiary Mental Health Service. Suicide Life-Threat. Behav. 2018, 49, 846–858. [Google Scholar] [CrossRef]
- Stanley, B.; Brown, G.K. Safety Planning Intervention: A Brief Intervention to Mitigate Suicide Risk. Cogn. Behav. Pract. 2012, 19, 256–264. [Google Scholar] [CrossRef]
- Nyer, M.; Gerbarg, P.L.; Silveri, M.M.; Johnston, J.; Scott, T.M.; Nauphal, M.; Owen, L.; Nielsen, G.H.; Mischoulon, D.; Brown, R.P.; et al. A Randomized Controlled Dosing Study of Iyengar Yoga and Coherent Breathing for the Treatment of Major Depressive Disorder: Impact on Suicidal Ideation and Safety Findings. Complement. Ther. Med. 2018, 37, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Sevilla-Llewellyn-Jones, J.; Santesteban-Echarri, O.; Pryor, I.; McGorry, P.; Alvarez-Jimenez, M. Web-Based Mindfulness Interventions for Mental Health Treatment: Systematic Review and Meta-Analysis. JMIR Ment. Health 2018, 5, e10278. [Google Scholar] [CrossRef]
- Lee, H.Y.; Hwang, J.; Ball, J.G.; Lee, J.; Yu, Y.; Albright, D.L. Mental Health Literacy Affects Mental Health Attitude: Is There a Gender Difference? Am. J. Health Behav. 2020, 44, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Meppelink, C.S.; van Weert, J.C.; Haven, C.J.; Smit, E.G. The Effectiveness of Health Animations in Audiences with Different Health Literacy Levels: An Experimental Study. J. Med. Internet Res. 2015, 17, e3979. [Google Scholar] [CrossRef] [PubMed]
- Carrouel, F.; de Vigneulles, B.D.S.; Bourgeois, D.; Kabuth, B.; Baltenneck, N.; Nusbaum, F.; Burge, V.; Roy, S.; Buchheit, S.; Carrion-Martinaud, M.-L.; et al. Mental Health Mobile Apps in the French App Store: Assessment Study of Functionality and Quality. JMIR Mhealth Uhealth 2022, 10, e41282. [Google Scholar] [CrossRef]
- Naslund, J.A.; Aschbrenner, K.A.; Marsch, L.A.; Bartels, S.J. The Future of Mental Health Care: Peer-to-Peer Support and Social Media. Epidemiol. Psychiatr. Sci. 2016, 25, 113–122. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- Kitzinger, J. The Methodology of Focus Groups: The Importance of Interaction between Research Participants. Sociol. Health Illn. 1994, 16, 103–121. [Google Scholar] [CrossRef]
- Haute Autorité de Santé. Assessment of Apps in the Mobile Health (MHealth) Sector—Overview and Quality Criteria of Medical Content for Referencing Digital Services in the Digital Health Space and the Professional Service Package; World Wide Web electronic publication; Haute Autorité de Santé (French National Authority for Health) (HAS): Saint-Denis, France, 2021. [Google Scholar]
- Baumel, A.; Muench, F.; Edan, S.; Kane, J.M. Objective User Engagement with Mental Health Apps: Systematic Search and Panel-Based Usage Analysis. J. Med. Internet Res. 2019, 21, e14567. [Google Scholar] [CrossRef]
- Ashton, J.; Grey, P.; Barnard, K. Healthy Cities—WHO’s New Public Health Initiative. Health Promot. Int. 1986, 1, 319–324. [Google Scholar] [CrossRef]
- Turmaine, K.; Dumas, A.; Chevreul, K. Conditions for the Successful Integration of an EHealth Tool “StopBlues” Into Community-Based Interventions in France: Results from a Multiple Correspondence Analysis. J. Med. Internet Res. 2022, 24, e30218. [Google Scholar] [CrossRef]
- Wahlbeck, K.; Cresswell-Smith, J.; Haaramo, P.; Parkkonen, J. Interventions to Mitigate the Effects of Poverty and Inequality on Mental Health. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Lorant, V.; de Gelder, R.; Kapadia, D.; Borrell, C.; Kalediene, R.; Kovács, K.; Leinsalu, M.; Martikainen, P.; Menvielle, G.; Regidor, E.; et al. Socioeconomic Inequalities in Suicide in Europe: The Widening Gap. Br. J. Psychiatry 2018, 212, 356–361. [Google Scholar] [CrossRef]
- Gandré, C.; Le Jeannic, A.; Vinet, M.-A.; Turmaine, K.; Courtet, P.; Roelandt, J.-L.; Vaiva, G.; Giraudeau, B.; Alberti, C.; Chevreul, K. The PRINTEMPS Study: Protocol of a Cluster-Randomized Controlled Trial of the Local Promotion of a Smartphone Application and Associated Website for the Prevention of Suicidal Behaviors in the Adult General Population in France. Trials 2020, 21, 553. [Google Scholar] [CrossRef] [PubMed]
- Suler, J. The Online Disinhibition Effect. Int. J. Appl. Psychoanal. Stud. 2005, 2, 184–188. [Google Scholar] [CrossRef]
- Powell, J.; Clarke, A. Internet Information-Seeking in Mental Health: Population Survey. Br. J. Psychiatry 2006, 189, 273–277. [Google Scholar] [CrossRef]
- Kuijpers, W.; Groen, W.G.; Aaronson, N.K.; Harten, W.H. van A Systematic Review of Web-Based Interventions for Patient Empowerment and Physical Activity in Chronic Diseases: Relevance for Cancer Survivors. J. Med. Internet Res. 2013, 15, e37. [Google Scholar] [CrossRef]
- Alpay, L.; van der Boog, P.; Dumaij, A. An Empowerment-Based Approach to Developing Innovative e-Health Tools for Self-Management. Health Inform. J. 2011, 17, 247–255. [Google Scholar] [CrossRef]
- Istepanian, R.S.H.; AlAnzi, T. Chapter Twenty Two—Mobile Health (m-Health): Evidence-Based Progress or Scientific Retrogression. In Biomedical Information Technology, 2nd ed.; Feng, D.D., Ed.; Biomedical Engineering; Academic Press: Cambridge, MA, USA, 2020; pp. 717–733. ISBN 978-0-12-816034-3. [Google Scholar]
| Name | Country | Main Objective | Intervention |
|---|---|---|---|
| Optimizing Suicide Prevention Programs and their Implementation in Europe (OSPI Europe) [50,51] | Germany, Hungary, Ireland, and Portugal | To provide an evidence-based and efficient concept for suicide prevention along with the corresponding materials and instruments for the multifaceted intervention and guidelines for the implementation process in any European country. | The European Alliance Against Depression (EAAD) intervention consists of (1) training sessions and practice support for primary care physicians, (2) public relations activities and mass media campaigns, (3) training sessions for community facilitators who serve as gatekeepers for depressed and suicidal persons in the community and treatment, and (4) outreach and support for high risk and self-help groups (e.g., helplines). In OSPI, the EAAD model is enhanced by other evidence-based interventions and implemented simultaneously and in a standardized way in four regions. |
| European Regions Enforcing Actions against Suicide (Euregenas) www.euregenas.eu (accessed on 4 March 2023) [54,55] | Italy, Belgium, Sweden, Romania, Spain, Finland, Germany, Slovenia, United-Kingdom | To contribute to the prevention of suicidality (suicidal ideation, suicide attempts and suicide) in Europe through the development and implementation of technology-based strategies for suicide prevention at regional level. Those strategies can be of use to the European Community as examples of good practice. | WP 5: development of an e-conceptual model to provide all necessary information to be able to create an integrated support and intervention mainframe for e-mental health, directed at the prevention of suicide, which can be adapted to local needs in all European regions and regional health care organizations. WP 6: development of prevention guidelines and toolkits for suicide prevention strategies as well as specific prevention packages for the awareness raising on suicide prevention for the identified target groups. |
| Beyondblue [56,57] | Australia | To evaluate whether a campaign to increase public knowledge about depression (beyondblue: the national depression initiative) has influenced the Australian public’s ability to recognize depression and their beliefs about treatments. | A global campaign with a website: information depending on who you are; a chat; contact number or email; coping strategies for the user or a relative. |
| Preventing Depression and improving Awareness through Networking in the EU (PrediNu) [52,53] | Germany, Ireland, Belgium, Austria, Hungary, Bulgaria, Estonia, Portugal United-Kingdom, Spain and Luxembourg | To improve the care of depression and prevent suicidal behavior using information and communication technologies. | A multilingual information website about depression and suicidal behavior (www.ifightdepression.com) and a multilingual, internet-based self-management program for patients with minor, mild, and moderate forms of depression (the iFightDepression program) were developed. Based on the EAAD and OSPI projects. |
| Name | Country | Main Objective | Tool Structure | Outcomes |
|---|---|---|---|---|
| BackUp [60] | Belgium | To provide a free, easily accessible, independently usable application. It offers evidence-based tools to support a suicidal person coping with a crisis. Equally for people concerned about a suicidal person and want to help. | Tool to reach out; Hope box; Tool to identify coping strategies; Safety plan; Suicidal trigger; Coping strategies; Reach out to family, friends, and professionals; Create a safe environment. | Positive evaluation of the program. Self-help tools can have positive impact on suicidal ideation: (1) reach people not accessible by usual interventions, (2) contribute by being an addition to regular care. |
| MYPLAN [63,64,65] | Denmark | To propose an app-based safety plan to reduce suicidal ideation. | Safety plan; Suicidal trigger; Coping strategies; New strategies; Other strategies for inspiration; Distractions; Map with nearest ED; Prewritten messages to send; Direct phone links; Virtual hope box. | A mobile phone application could be useful for some populations, and the safety plan would help people interrupt an early suicidal process and have a feeling of empowerment. |
| ReliefLink [62,66] | United States | To create a reliable and user-friendly app designed to provide continuity and follow-up linkages for people at risk of committing suicide. | Mood tracking; Reminders for doctor’s appointments and medication; Safety plan (coping strategies); Location of the nearest hospitals and mental health treatment centers; Emergency button that can connect patients to helplines, providers, 911, and friends/family. | Won first prize (USD50,000) in the Suicide Prevention: Continuity of Care and Follow-up App Challenge sponsored by SAMHSA (Substance Abuse and Mental Health Services Administration). |
| Quiz Name | Questionnaire | Goal | Reason for Selection |
|---|---|---|---|
| To test yourself | |||
| Psychological wellbeing Quiz | 12-item General Health Questionnaire (GHQ-12) [79,80] | First screening on global mental health. | Chosen because of its few questions, and its stability and sensitivity to changes over a long period. Often used in general population survey. |
| Depression Quiz | Nine-item Patient Health Questionnaire (PHQ-9) [81,82,83] | To test the level of depression. To lighten the completion, it was only proposed to users with a GHQ-12 score > 2. | Chosen because of its few questions, and reliability and validity to test depression. It is also appreciated by users and does not have a saturation phenomenon. |
| Anxiety Quiz | Seven-item Generalized Anxiety Disorder (GAD-7) [84,85] | To test the level of anxiety. To lighten the completion, it was only proposed to users with a GHQ-12 score > 2. | Chosen because of its few questions, easiness, and reliability in testing anxiety. |
| Suicide risk evaluation | Mini International Neuropsychiatric Interview (MINI) [86,87] | Suicidality module for the level of suicidal risk. This questionnaire was proposed to users only from the moment: PHQ-9 score ≥ 10, or GAD-7 score > 7, or one score of the mood-tracking system was ≤40% or ≤50% with a 20% decrease in comparison to the previous score. | Chosen because of its few questions and reliability as a screening instrument more than to evaluate severity of symptoms. |
| To test a relative | |||
| Depression Quiz | Montgomery and Asberg Depression Rating Scale (MADRS) [88] | To test relatives on depression and anxiety, it had to be hetero-administrated. | Chosen because it has only 10 questions and explores depression and anxiety with very good sensibility and sensitivity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le Jeannic, A.; Turmaine, K.; Gandré, C.; Vinet, M.-A.; Michel, M.; Chevreul, K.; on behalf of the PRINTEMPS Consortium. Defining the Characteristics of an e-Health Tool for Suicide Primary Prevention in the General Population: The StopBlues Case in France. Int. J. Environ. Res. Public Health 2023, 20, 6096. https://doi.org/10.3390/ijerph20126096
Le Jeannic A, Turmaine K, Gandré C, Vinet M-A, Michel M, Chevreul K, on behalf of the PRINTEMPS Consortium. Defining the Characteristics of an e-Health Tool for Suicide Primary Prevention in the General Population: The StopBlues Case in France. International Journal of Environmental Research and Public Health. 2023; 20(12):6096. https://doi.org/10.3390/ijerph20126096
Chicago/Turabian StyleLe Jeannic, Anaïs, Kathleen Turmaine, Coralie Gandré, Marie-Amélie Vinet, Morgane Michel, Karine Chevreul, and on behalf of the PRINTEMPS Consortium. 2023. "Defining the Characteristics of an e-Health Tool for Suicide Primary Prevention in the General Population: The StopBlues Case in France" International Journal of Environmental Research and Public Health 20, no. 12: 6096. https://doi.org/10.3390/ijerph20126096
APA StyleLe Jeannic, A., Turmaine, K., Gandré, C., Vinet, M.-A., Michel, M., Chevreul, K., & on behalf of the PRINTEMPS Consortium. (2023). Defining the Characteristics of an e-Health Tool for Suicide Primary Prevention in the General Population: The StopBlues Case in France. International Journal of Environmental Research and Public Health, 20(12), 6096. https://doi.org/10.3390/ijerph20126096






