The Impact of a Psychoeducational Group Program on the Mental Well-Being of Unit-Based Nurse Leaders: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sample
2.3. Intervention
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
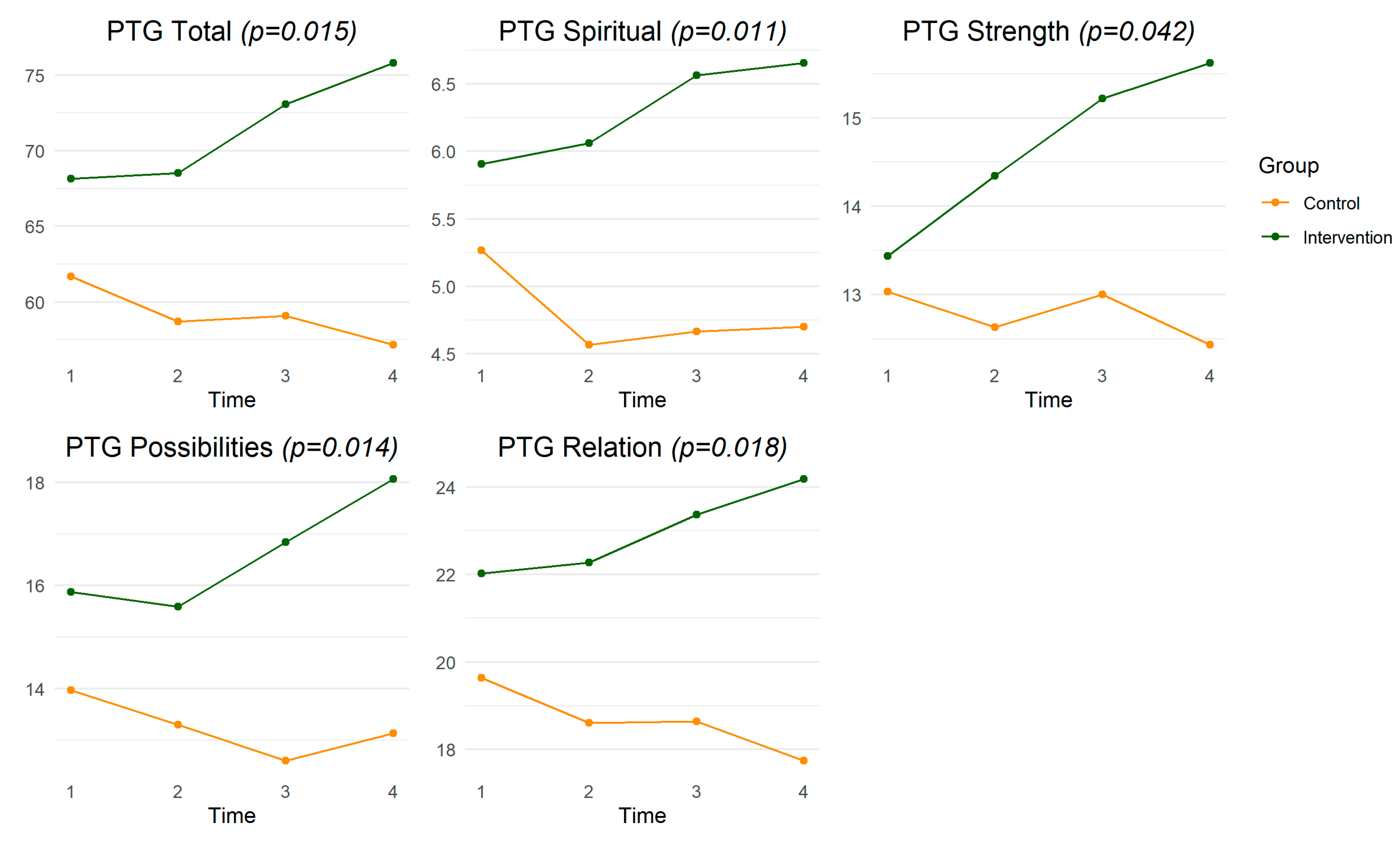
3.1. Post-Traumatic Growth
3.2. Professional Quality of Life
3.3. Program Themes
3.3.1. Resilience
3.3.2. Insight
3.3.3. Self-Compassion
3.3.4. Empowerment
3.4. Perceived Stress, Job Satisfaction, and Self-Efficacy
4. Discussion
4.1. Post-Traumatic Growth
4.2. Professional Quality of Life
4.3. Program Themes
4.3.1. Resilience
4.3.2. Insight
4.3.3. Self-Compassion
4.3.4. Empowerment
4.4. Perceived Stress, Job Satisfaction, and Self-Efficacy
4.5. Limitations
4.6. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hughes, V. Nurse leader impact: A review. Nurs. Manag. 2019, 50, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; McEnroe-Petitte, D.M.; Leocadio, M.C.; Van Bogaert, P.; Cummings, G.G. Stress and ways of coping among nurse managers: An integrative review. J. Clin. Nurs. 2018, 27, 1346–1359. [Google Scholar] [CrossRef]
- Membrive-Jiménez, M.J.; Pradas-Hernández, L.; Suleiman-Martos, N.; Vargas-Román, K.; Cañadas-De la Fuente, G.A.; Gomez-Urquiza, J.L.; De la Fuente-Solana, E.I. Burnout in nursing managers: A systematic review and meta-analysis of related factors, levels and prevalence. Int. J. Environ. Res. Public Health 2020, 17, 3983. [Google Scholar] [CrossRef] [PubMed]
- Steege, L.M.; Pinekenstein, B.J.; Arsenault Knudsen, É.; Rainbow, J.G. Exploring nurse leader fatigue: A mixed methods study. J. Nurs. Manag. 2017, 25, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Stamm, B.H. Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5 (ProQOL). 2009. Available online: http://www.proqol.org (accessed on 2 April 2023).
- Penconek, T.; Tate, K.; Bernardes, A.; Lee, S.; Micaroni, S.P.; Balsanelli, A.P.; de Moura, A.A.; Cummings, G.G. Determinants of nurse manager job satisfaction: A systematic review. Int. J. Nurs. Stud. 2021, 118, 103906. [Google Scholar] [CrossRef] [PubMed]
- Warshawsky, N.E. Building nurse manager well-being by reducing healthcare system demands. J. Nurs. Adm. 2022, 52, 189–191. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Gélinas, C.; Aubé, T.; Tchouaket, E.; Tremblay, D.; Gagnon, M.P.; Côté, J. Influence of caring for COVID-19 patients on nurse’s turnover, work satisfaction and quality of care. J. Nurs. Manag. 2022, 30, 33–43. [Google Scholar] [CrossRef]
- Udod, S.; MacPhee, M.; Baxter, P. Rethinking resilience: Nurses and nurse leaders emerging from the post–COVID-19 environment. J. Nurs. Adm. 2021, 51, 537–540. [Google Scholar] [CrossRef]
- White, J.H. A Phenomenological Study of Nurse Managers’ and Assistant Nurse Managers’ Experiences during the COVID-19 Pandemic in the United States. J. Nurs. Manag. 2021, 29, 1525–1534. [Google Scholar] [CrossRef]
- Bender, A.E.; Berg, K.A.; Miller, E.K.; Evans, K.E.; Holmes, M.R. “Making Sure We Are All Okay”: Healthcare Workers’ Strategies for Emotional Connectedness during the COVID-19 Pandemic. Clin. Soc. Work. J. 2021, 49, 445–455. [Google Scholar] [CrossRef]
- d’Ettorre, G.; Ceccarelli, G.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Alessandri, F.; Koukopoulos, A.E.; Russo, A.; d’Ettorre, G.; Tarsitani, L. Post-Traumatic Stress Symptoms in Healthcare Workers Dealing with the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 601. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. The mental health continuum: From languishing to flourishing in life. J. Health Soc. Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef] [Green Version]
- Keyes, C.L. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 2005, 73, 539–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fowler, K.; Wholeben, M. COVID-19: Outcomes for trauma-impacted nurses and nursing students. Nurse Educ. Today 2020, 93, 104525. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Ripp, J.; Brown, M.; Sinsky, C.A. Caring for Health Care Workers during Crisis: Creating a Resilient Organization; American Medical Association: Chicago, IL, USA, 2020; Available online: https://www.ama-assn.org/system/files/2020-04/caring-forhealth-care-workers-covid-19.pdf (accessed on 3 April 2023).
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef] [Green Version]
- Vanhove, A.J.; Herian, M.N.; Perez, A.L.; Harms, P.D.; Lester, P.B. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. J. Occup. Organ. Psychol. 2016, 89, 278–307. [Google Scholar] [CrossRef] [Green Version]
- Melnyk, B.M.; Kelly, S.A.; Stephens, J.; Dhakal, K.; McGovern, C.; Tucker, S.; Hoying, J.; McRae, K.; Ault, S.; Spurlock, E. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: A systematic review. Am. J. Health Promot. 2020, 34, 929–941. [Google Scholar] [CrossRef]
- Bailey, A.K.; Sawyer, A.T.; Robinson, P.S. A Psychoeducational Group Intervention for Nurses: Rationale, Theoretical Framework, and Development. J. Am. Psychiatr. Nurses Assoc. 2023, 29, 232–240. [Google Scholar] [CrossRef]
- Sawyer, A.T.; McManus, K.; Bailey, A.K. A mixed-methods pilot study of a psychoeducational group programme for nurse managers during the COVID-19 pandemic. J. Nurs. Manag. 2022. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Kolb, A.Y.; Kolb, D.A.; Passarelli, A.; Sharma, G. On becoming an experiential educator: The educator role profile. Simul. Gaming 2014, 45, 204–234. [Google Scholar] [CrossRef]
- Sawyer, A.T.; Bailey, A.K.; Green, J.F.; Sun, J.; Robinson, P.S. Resilience, insight, self-compassion, and empowerment (rise): A randomized controlled trial of a psychoeducational group program for nurses. J. Am. Psychiatr. Nurses Assoc. 2021. Ahead of Print. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy; Guilford press: New York, NY, USA, 1999. [Google Scholar]
- Kent, W.; Hochard, K.D.; Hulbert-Williams, N.J. Perceived stress and professional quality of life in nursing staff: How important is psychological flexibility? J. Context. Behav. Sci. 2019, 14, 11–19. [Google Scholar] [CrossRef]
- Towey-Swift, K.D.; Lauvrud, C.; Whittington, R. Acceptance and commitment therapy (ACT) for professional staff burnout: A systematic review and narrative synthesis of controlled trials. J. Ment. Health 2023, 32, 452–464. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.S. Cognitive Therapy: Basics and Beyond; Guilford Press: New York, NY, USA, 1964. [Google Scholar]
- Kazantzis, N.; Luong, H.K.; Usatoff, A.S.; Impala, T.; Yew, R.Y.; Hofmann, S.G. The processes of cognitive behavioral therapy: A review of meta-analyses. Cognit. Ther. Res. 2018, 42, 349–357. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Lomas, T.; Medina, J.C.; Ivtzan, I.; Rupprecht, S.; Eiroa-Orosa, F.J. A systematic review and meta-analysis of the impact of mindfulness-based interventions on the well-being of healthcare professionals. Mindfulness 2019, 10, 1193–1216. [Google Scholar] [CrossRef] [Green Version]
- Avolio, B.J.; Gardner, W.L. Authentic leadership development: Getting to the root of positive forms of leadership. Leadersh. Q. 2005, 16, 315–338. [Google Scholar] [CrossRef]
- Giordano-Mulligan, M.; Eckardt, S. Authentic Nurse Leadership Conceptual Framework: Nurses’ Perception of Authentic Nurse Leader Attributes. Nurs. Adm. Q. 2019, 43, 164–174. [Google Scholar] [CrossRef]
- Center for Victims of Torture (CVT). ProQOL: Professional Quality of Life. Available online: https://proqol.org/ (accessed on 3 March 2023).
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.M.; Franklin, J.; Langford, P. The self-reflection and insight scale: A new measure of private self-consciousness. Soc. Behav. Pers. 2002, 30, 821–835. [Google Scholar] [CrossRef] [Green Version]
- Raes, F.; Pommier, E.; Neff, K.D.; Van Gucht, D. Construction and factorial validation of a short form of the self-compassion scale. Clin. Psychol. Psychother. 2011, 18, 250–255. [Google Scholar] [CrossRef]
- Spreitzer, G.M. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Acad. Manag. J. 1995, 38, 1442–1465. [Google Scholar] [CrossRef]
- Schwarzer, R.; Jerusalem, M. Generalized self-efficacy scale. J. Weinman S. Wright M. Johnston Meas. Health Psychol. A User’s Portfolio. Causal Control. Beliefs 1995, 35, 37. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Thompson, E.R.; Phua, F.T. A brief index of affective job satisfaction. Group Organ. Manag. 2012, 37, 275–307. [Google Scholar] [CrossRef]
- American Counseling Association (ACA). Code of Ethics. 2014. Available online: https://www.counseling.org/resources/aca-code-of-ethics.pdf (accessed on 2 April 2023).
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Correa, P.B.; Bacon, C.T. The Effect of Leadership Interventions on Staff Nurse Job Enjoyment and Leadership Perception. J. Nurs. Adm. 2019, 49, 215–220. [Google Scholar] [CrossRef]
- Majeed, N.; Jamshed, S. Nursing turnover intentions: The role of leader emotional intelligence and team culture. J. Nurs. Manag. 2021, 29, 229–239. [Google Scholar] [CrossRef]
- Kriakous, S.A.; Elliott, K.A.; Lamers, C.; Owen, R. The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: A Systematic Review. Mindfulness 2021, 12, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Kashdan, T.B.; Kane, J.Q. Post-traumatic distress and the presence of post-traumatic growth and meaning in life: Experiential avoidance as a moderator. Pers. Individ. Differ. 2011, 50, 84–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henson, C.; Truchot, D.; Canevello, A. What promotes post traumatic growth? A systematic review. Eur. J. Trauma Dissociation 2021, 5, 100195. [Google Scholar] [CrossRef]
- Chen, R.; Sun, C.; Chen, J.J.; Jen, H.J.; Kang, X.L.; Kao, C.C.; Chou, K.R. A Large-Scale Survey on Trauma, Burnout, and Posttraumatic Growth among Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs. 2021, 30, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Yim, J.Y.; Kim, J.A. Factors influencing posttraumatic growth among nurses caring for COVID-19 patients: A path analysis. J. Nurs. Manag. 2022, 30, 1940–1948. [Google Scholar] [CrossRef]
- Zhang, X.T.; Shi, S.S.; Qin Ren, Y.; Wang, L. The traumatic experience of clinical nurses during the COVID-19 pandemic: Which factors are related to post-traumatic growth? Risk Manag. Healthc. Policy 2021, 14, 2145–2151. [Google Scholar] [CrossRef] [PubMed]
- Cui, P.P.; Wang, P.P.; Wang, K.; Ping, Z.; Wang, P.; Chen, C. Post-traumatic growth and influencing factors among frontline nurses fighting against COVID-19. Occup. Environ. Med. 2021, 78, 129–135. [Google Scholar] [CrossRef]
- Remegio, W.; Rivera, R.R.; Griffin, M.Q.; Fitzpatrick, J.J. The professional quality of life and work engagement of nurse leaders. Nurse Leader 2021, 19, 95–100. [Google Scholar] [CrossRef]
- Kelly, L.A.; Lefton, C.; Fischer, S.A. Nurse Leader Burnout, Satisfaction, and Work-Life Balance. J. Nurs. Adm. 2019, 49, 404–410. [Google Scholar] [CrossRef]
- Calegari, J.G.; Russo, S.; Luciani, M.; Strepparava, M.G.; Di Mauro, S.; Ausili, D. Association between coping strategies and professional quality of life in nurses and physicians during COVID-19: A cross-sectional study. J. Nurs. Manag. 2022, 30, 4054–4063. [Google Scholar] [CrossRef]
- Hinderer, K.A.; VonRueden, K.T.; Friedmann, E.; McQuillan, K.A.; Gilmore, R.; Kramer, B.; Murray, M. Burnout, compassion fatigue, compassion satisfaction, and secondary traumatic stress in trauma nurses. J. Trauma Nurs. 2014, 21, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.; Cho, H.; Han, K.; Lee, H. Association between nursing work environment and compassion satisfaction among clinical nurses. J. Nurs. Manag. 2020, 28, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Hunsaker, S.; Chen, H.C.; Maughan, D.; Heaston, S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J. Nurs. Scholarsh. 2015, 47, 186–194. [Google Scholar] [CrossRef] [Green Version]
- Shanafelt, T.; Trockel, M.; Ripp, J.; Murphy, M.L.; Sandborg, C.; Bohman, B. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad. Med. 2019, 94, 156–161. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; Gomez-Urquiza, J.L.; Aguayo-Estremera, R.; Cañadas-De La Fuente, G.A.; De La Fuente-Solana, E.I.; Albendín-García, L. The effect of mindfulness training on burnout syndrome in nursing: A systematic review and meta-analysis. J. Adv. Nurs. 2020, 76, 1124–1140. [Google Scholar] [CrossRef] [PubMed]
- Ahola, K.; Toppinen-Tanner, S.; Seppänen, J. Interventions to alleviate burnout symptoms and to support return to work among employees with burnout: Systematic review and meta-analysis. Burnout Res. 2017, 4, 1–11. [Google Scholar] [CrossRef]
- Ceravolo, D.; Raines, D.A. The Impact of a Mindfulness Intervention for Nurse Managers. J. Holist. Nurs. 2019, 37, 47–55. [Google Scholar] [CrossRef]
- Henshall, C.; Davey, Z.; Jackson, D. Nursing resilience interventions-A way forward in challenging healthcare territories. J. Clin. Nurs. 2020, 29, 3597–3599. [Google Scholar] [CrossRef] [Green Version]
- Itchhaporia, D. The Evolution of the Quintuple Aim: Health Equity, Health Outcomes, and the Economy. J. Am. Coll. Cardiol. 2021, 78, 2262–2264. [Google Scholar] [CrossRef]
- Ripp, J.; Shanafelt, T. The health care chief wellness officer: What the role is and is not. Acad. Med. 2020, 95, 1354–1358. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G.; Groleau, J.M. Clinical applications of posttraumatic growth. In Positive Psychology in Practice: Promoting Human Flourishing in Work, Health, Education, and Everyday Life, 2nd ed.; Joseph, S., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2015; pp. 503–518. [Google Scholar]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef] [Green Version]
- Pallesen, K.S.; McCormack, B.; Kjerholt, M.; Borre, L.Z.; Rosted, E.; Hølge-Hazelton, B. An investigation of the level of burnout and resilience among hospital based nurse managers after COVID 19—A cross-sectional questionnaire-based study. J. Nurs. Manag. 2022, 30, 2495–2502. [Google Scholar] [CrossRef]
- Cooper, A.L.; Brown, J.A.; Rees, C.S.; Leslie, G.D. Nurse resilience: A concept analysis. Int. J. Ment. Health Nurs. 2020, 29, 553–575. [Google Scholar] [CrossRef]
- Hart, P.L.; Brannan, J.D.; De Chesnay, M. Resilience in nurses: An integrative review. J. Nurs. Manag. 2014, 22, 720–734. [Google Scholar] [CrossRef] [Green Version]
- Patel, S.S.; Rogers, M.B.; Amlôt, R.; Rubin, G.J. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017, 9. [Google Scholar]
- Harrington, R.; Loffredo, D.A. Insight, rumination, and self-reflection as predictors of well-being. J. Psychol. 2011, 145, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Horton-Deutsch, S.; Sherwood, G. Reflection: An educational strategy to develop emotionally-competent nurse leaders. J. Nurs. Manag. 2008, 16, 946–954. [Google Scholar] [CrossRef] [PubMed]
- Crane, M.F.; Searle, B.J.; Kangas, M.; Nwiran, Y. How resilience is strengthened by exposure to stressors: The systematic self-reflection model of resilience strengthening. Anxiety Stress Coping 2019, 32, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Jayatilleke, N.; Mackie, A. Reflection as part of continuous professional development for public health professionals: A literature review. J. Public Health 2013, 35, 308–312. [Google Scholar] [CrossRef] [Green Version]
- Contreras, J.A.; Edwards-Maddox, S.; Hall, A.; Lee, M.A. Effects of Reflective Practice on Baccalaureate Nursing Students’ Stress, Anxiety and Competency: An Integrative Review. Worldviews Evid. Based Nurs. 2020, 17, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Akerjordet, K.; Severinsson, E. Emotionally intelligent nurse leadership: A literature review study. J. Nurs. Manag. 2008, 16, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Neff, K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Ident. 2003, 2, 85–101. [Google Scholar] [CrossRef] [Green Version]
- Germer, C.K.; Neff, K.D. Self-compassion in clinical practice. J. Clin. Psychol. 2013, 69, 856–867. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D.; Kirkpatrick, K.L.; Rude, S.S. Self-compassion and adaptive psychological functioning. J. Res. Personal. 2007, 41, 139–154. [Google Scholar] [CrossRef]
- MacBeth, A.; Gumley, A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin. Psychol. Rev. 2012, 32, 545–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bluth, K.; Neff, K.D. New frontiers in understanding the benefits of self-compassion. Self Identity 2018, 17, 605–608. [Google Scholar] [CrossRef]
- Heffernan, M.; Quinn Griffin, M.T.; Sister Rita, M.; Fitzpatrick, J.J. Self-compassion and emotional intelligence in nurses. Int. J. Nurs. Pract. 2010, 16, 366–373. [Google Scholar] [CrossRef]
- Biber, D.D.; Ellis, R. The effect of self-compassion on the self-regulation of health behaviors: A systematic review. J. Health Psychol. 2019, 24, 2060–2071. [Google Scholar] [CrossRef]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, Compassion, and Self-Compassion Among Health Care Professionals: What’s New? A Systematic Review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef]
- Neff, K.D.; Knox, M.C.; Long, P.; Gregory, K. Caring for others without losing yourself: An adaptation of the mindful self-compassion program for healthcare communities. J. Clin. Psychol. 2020, 76, 1543–1562. [Google Scholar] [CrossRef]
- Upton, K.V. An investigation into compassion fatigue and self-compassion in acute medical care hospital nurses: A mixed methods study. J. Compassionate Health Care 2018, 5, 7. [Google Scholar] [CrossRef]
- Warren, R.; Smeets, E.; Neff, K. Self-criticism and self-compassion: Risk and resilience: Being compassionate to oneself is associated with emotional resilience and psychological well-being. Curr. Psychiatr. 2016, 15, 18–28. [Google Scholar]
- Raab, K. Mindfulness, self-compassion, and empathy among health care professionals: A review of the literature. J. Health Care Chaplain. 2014, 20, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Seibert, S.E.; Wang, G.; Courtright, S.H. Antecedents and consequences of psychological and team empowerment in organizations: A meta-analytic review. J. Appl. Psychol. 2011, 96, 981. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boudrias, J.S.; Morin, A.J.; Brodeur, M.M. Role of psychological empowerment in the reduction of burnout in Canadian healthcare workers. Nurs. Health Sci. 2012, 14, 8–17. [Google Scholar] [CrossRef]
- Trus, M.; Razbadauskas, A.; Doran, D.; Suominen, T. Work-related empowerment of nurse managers: A systematic review. Nurs. Health Sci. 2012, 14, 412–420. [Google Scholar] [CrossRef]
- Meng, L.; Jin, Y.; Guo, J. Mediating and/or moderating roles of psychological empowerment. Appl. Nurs. Res. 2016, 30, 104–110. [Google Scholar] [CrossRef]
- Li, H.; Shi, Y.; Li, Y.; Xing, Z.; Wang, S.; Ying, J.; Zhang, M.; Sun, J. Relationship between nurse psychological empowerment and job satisfaction: A systematic review and meta-analysis. J. Adv. Nurs. 2018, 74, 1264–1277. [Google Scholar] [CrossRef]
- Van Dyk, J.; Siedlecki, S.L.; Fitzpatrick, J.J. Frontline nurse managers’ confidence and self-efficacy. J. Nurs. Manag. 2016, 24, 533–539. [Google Scholar] [CrossRef]
- Becker, C.B.; Stice, E.; Shaw, H.; Woda, S. Use of empirically supported interventions for psychopathology: Can the participatory approach move us beyond the research-to-practice gap? Behav. Res. Ther. 2009, 47, 265–274. [Google Scholar] [CrossRef] [Green Version]
- Powell, B.J.; McMillen, J.C.; Proctor, E.K.; Carpenter, C.R.; Griffey, R.T.; Bunger, A.C.; Glass, J.E.; York, J.L. A compilation of strategies for implementing clinical innovations in health and mental health. Med. Care Res. Rev. 2012, 69, 123–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carroll, C.; Patterson, M.; Wood, S.; Booth, A.; Rick, J.; Balain, S. A conceptual framework for implementation fidelity. Implement. Sci. 2007, 2, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Intervention (n = 39) | Control (n = 38) | Chi-Square/t | p-Value | ||
|---|---|---|---|---|---|---|
| Count/Mean | %/SD | Count/Mean | %/SD | |||
| Sex | 1.722 | 0.189 | ||||
| Female | 32 | 82.1% | 35 | 92.1% | ||
| Male | 7 | 17.9% | 3 | 7.9% | ||
| Race | 2.857 | 0.582 | ||||
| Asian | 2 | 5.1% | 1 | 2.6% | ||
| Black | 5 | 12.8% | 2 | 5.3% | ||
| Multi | 1 | 2.6% | 1 | 2.6% | ||
| Other | 1 | 2.6% | 0 | 0.0% | ||
| White | 30 | 76.9% | 34 | 89.5% | ||
| Ethnicity | 0.502 | 0.479 | ||||
| Hispanic | 5 | 12.8% | 3 | 7.9% | ||
| Non-Hispanic | 34 | 87.2% | 35 | 92.1% | ||
| Marital Status | 7.429 | 0.115 | ||||
| Single | 10 | 25.6% | 3 | 7.9% | ||
| Married | 24 | 61.5% | 29 | 76.3% | ||
| Separated | 2 | 5.1% | 0 | 0.0% | ||
| Divorced | 2 | 5.1% | 3 | 7.9% | ||
| Partnered Widowed | 1 0 | 2.6% 0.0% | 3 0 | 7.9% 0.0% | ||
| Education | 1.232 | 0.540 | ||||
| Associate’s degree | 5 | 12.8% | 4 | 10.5% | ||
| Bachelor’s degree | 26 | 66.7% | 22 | 57.9% | ||
| Master’s degree | 8 | 20.5% | 12 | 31.6% | ||
| Job Role | 0.312 | 0.577 | ||||
| ANM | 25 | 64.1% | 22 | 57.9% | ||
| NM | 14 | 35.9% | 16 | 42.1% | ||
| Age | 43.97 | 10.60 | 44.76 | 9.24 | 0.348 | 0.729 |
| Years of Experience | 3.92 | 4.93 | 5.00 | 6.19 | 0.846 | 0.400 |
| Variables | Baseline | Endpoint | Effect Size | t | p-Value |
|---|---|---|---|---|---|
| PTGI-Total | 67.91 (22.70) | 69.65 (27.47) | 0.07 | −0.37 | 0.712 |
| PTGI-Relating to Others | 21.76 (8.03) | 22.65 (9.85) | 0.10 | −0.52 | 0.610 |
| PTGI-New Possibilities | 15.79 (6.37) | 15.88 (7.29) | 0.01 | −0.07 | 0.942 |
| PTGI-Personal Strength | 13.50 (4.31) | 14.56 (5.04) | 0.23 | −1.13 | 0.266 |
| PTGI-Spiritual Change | 5.97 (2.88) | 6.21 (3.13) | 0.08 | −0.45 | 0.655 |
| PTGI-Appreciation of Life | 10.88 (3.06) | 10.35 (3.65) | −0.16 | 0.88 | 0.388 |
| BRS | 3.81 (0.61) | 3.79 (0.60) | 0.03 | 0.24 | 0.815 |
| SRIS-Total | 89.88 (14.41) | 93.85 (13.40) | 0.29 | −2.09 | 0.045 |
| SRIS-Insight | 35.82 (7.37) | 37.65 (6.05) | 0.27 | −1.51 | 0.142 |
| SRIS-Self-Reflection | 54.06 (9.86) | 56.21 (9.03) | 0.23 | −1.63 | 0.112 |
| SCS-SF | 3.19 (0.81) | 3.35 (0.81) | 0.18 | −1.72 | 0.095 |
| PEI-Total | 5.41 (0.90) | 5.82 (0.66) | 0.52 | −2.86 | 0.007 |
| PEI-Meaning | 5.82 (0.86) | 6.20 (0.72) | 0.48 | −2.37 | 0.024 |
| PEI-Competence | 5.35 (1.03) | 5.97 (0.76) | 0.68 | −4.90 | <0.001 |
| PEI-Self Determination | 5.26 (1.02) | 5.63 (0.86) | 0.39 | −2.08 | 0.045 |
| PEI-Impact | 5.22 (1.16) | 5.49 (1.17) | 0.23 | −1.11 | 0.275 |
| GSE | 33.29 (3.91) | 33.91 (3.87) | 0.16 | −1.66 | 0.107 |
| PSS | 16.62 (8.13) | 15.38 (7.11) | −0.16 | 1.36 | 0.182 |
| ProQOL-CS | 40.91 (5.57) | 42.82 (6.28) | 0.32 | −3.07 | 0.004 |
| ProQOL-Burnout | 23.06 (6.45) | 21.47 (6.23) | −0.25 | 2.30 | 0.028 |
| ProQOL-STS | 24.76 (6.46) | 23.76 (6.20) | −0.16 | 1.52 | 0.138 |
| BIAJS | 4.13 (0.78) | 4.12 (0.64) | −0.01 | 0.07 | 0.942 |
| Variables | 1-Month | Effect Size | t | p-Value | 3-Month | Effect Size | t | p-Value | 6-Month | Effect Size | t | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PTGI-Total | 72.74 (25.06) | 0.20 | −1.02 | 0.317 | 75.81 (23.16) | 0.34 | −2.72 | 0.011 | 72.09 (25.06) | 0.17 | −0.83 | 0.413 |
| PTGI-Relating to Others | 23.29 (9.02) | 0.18 | −0.89 | 0.379 | 24.19 (8.44) | 0.29 | −1.77 | 0.087 | 23.06 (9.63) | 0.15 | −0.55 | 0.585 |
| PTGI-New Possibilities | 16.88 (6.30) | 0.17 | −0.93 | 0.359 | 18.06 (6.03) | 0.37 | −2.95 | 0.006 | 17.16 (6.28) | 0.22 | −1.14 | 0.265 |
| PTGI-Personal Strength | 15.09 (4.65) | 0.35 | −1.72 | 0.095 | 15.63 (4.23) | 0.50 | −1.36 | 0.182 | 14.72 (4.42) | 0.28 | −1.36 | 0.183 |
| PTGI-Spiritual Change | 6.41 (2.79) | 0.16 | −0.80 | 0.428 | 6.66 (2.73) | 0.25 | −1.73 | 0.093 | 6.25 (3.25) | 0.09 | −0.57 | 0.575 |
| PTGI-Appreciation of Life | 11.06 (3.87) | 0.05 | −0.24 | 0.810 | 11.28 (3.42) | 0.12 | −0.82 | 0.421 | 10.91 (3.60) | 0.01 | 0.00 | 1.00 |
| BRS | 3.99 (0.65) | 0.29 | −1.65 | 0.109 | 3.91 (0.77) | 0.14 | −0.89 | 0.379 | 3.81 (0.79) | 0.00 | −0.04 | 0.969 |
| SRIS-Total | 91.65 (16.69) | 0.11 | −0.82 | 0.420 | 91.28 (16.82) | 0.09 | −1.11 | 0.277 | 88.78 (19.85) | −0.06 | 0.21 | 0.837 |
| SRIS-Insight | 38.09 (5.97) | 0.34 | −2.11 | 0.043 | 37.78 (6.21) | 0.29 | −2.05 | 0.048 | 36.50 (7.44) | 0.09 | −0.81 | 0.422 |
| SRIS-Self-Reflection | 53.56 (11.92) | −0.05 | 0.33 | 0.745 | 53.50 (13.12) | −0.05 | 0.10 | 0.918 | 52.28 (13.88) | −0.15 | 0.73 | 0.468 |
| SCS-SF | 3.42 (0.77) | 0.29 | −2.82 | 0.008 | 3.44 (0.72) | 0.33 | −3.81 | 0.001 | 3.48 (0.86) | 0.35 | −3.06 | 0.005 |
| PEI-Total | 5.85 (0.69) | 0.55 | −3.84 | 0.001 | 5.79 (0.74) | 0.46 | −2.09 | 0.045 | 5.75 (0.97) | 0.36 | −1.57 | 0.126 |
| PEI-Meaning | 6.11 (0.68) | 0.37 | −2.29 | 0.029 | 6.10 (0.69) | 0.36 | −1.43 | 0.161 | 6.23 (0.92) | 0.46 | −2.17 | 0.038 |
| PEI-Competence | 5.88 (0.86) | 0.56 | −4.52 | <0.001 | 5.79 (1.21) | 0.39 | −2.42 | 0.022 | 5.90 (0.90) | 0.57 | −3.11 | 0.004 |
| PEI-Self Determination | 5.69 (0.85) | 0.46 | −2.99 | 0.005 | 5.78 (0.90) | 0.54 | −2.48 | 0.019 | 5.51 (1.39) | 0.21 | −0.75 | 0.457 |
| PEI-Impact | 5.73 (0.92) | 0.49 | −2.91 | 0.006 | 5.47 (1.29) | 0.20 | −0.53 | 0.597 | 5.38 (1.43) | 0.12 | −0.14 | 0.893 |
| GSE | 33.71 (4.13) | 0.10 | −0.96 | 0.344 | 33.69 (3.84) | 0.10 | −1.37 | 0.182 | 33.03 (5.27) | −0.06 | 0.00 | 1.00 |
| PSS | 14.74 (7.61) | 0.24 | 2.06 | 0.048 | 16.16 (8.09) | −0.06 | 0.42 | 0.676 | 16.34 (8.77) | −0.03 | 0.27 | 0.786 |
| ProQOL-CS | 42.38 (5.63) | 0.26 | −2.22 | 0.033 | 41.63 (7.18) | 0.11 | −0.95 | 0.348 | 41.38 (8.21) | 0.07 | −0.59 | 0.562 |
| ProQOL-Burnout | 20.97 (5.02) | −0.36 | 3.10 | 0.004 | 22.41 (7.44) | −0.09 | 0.49 | 0.627 | 21.97 (7.75) | −0.15 | 0.99 | 0.332 |
| ProQOL-STS | 22.91 (6.48) | −0.29 | 2.24 | 0.032 | 23.00 (8.53) | −0.23 | 1.53 | 0.136 | 23.91 (9.03) | −0.11 | 0.57 | 0.573 |
| BIAJS | 4.20 (0.70) | 0.09 | −0.65 | 0.518 | 3.96 (0.71) | −0.23 | 1.58 | 0.125 | 4.07 (1.06) | −0.06 | 0.56 | 0.579 |
| Variables | Group | Baseline | Endpoint | 1-Month | 3-Month | F | p-Value |
|---|---|---|---|---|---|---|---|
| PTGI-Total | Intervention | 67.91 (22.70) | 69.65 (27.47) | 72.74 (25.06) | 75.81 (23.16) | 6.31 | 0.015 |
| Control | 59.76 (25.16) | 56.09 (25.28) | 56.70 (21.66) | 57.17 (23.29) | |||
| PTGI-Relating to Others | Intervention | 21.76 (8.03) | 22.65 (9.85) | 23.29 (9.02) | 24.19 (8.44) | 5.94 | 0.018 |
| Control | 18.61 (9.87) | 17.35 (9.66) | 17.36 (8.62) | 17.73 (8.12) | |||
| PTGI-New Possibilities | Intervention | 15.79 (6.37) | 15.88 (7.29) | 16.88 (6.30) | 18.06 (6.03) | 6.41 | 0.014 |
| Control | 13.89 (6.63) | 13.12 (6.27) | 12.33 (6.22) | 13.13 (6.29) | |||
| PTGI-Personal Strength | Intervention | 13.50 (4.31) | 14.56 (5.04) | 15.09 (4.65) | 15.63 (4.23) | 4.32 | 0.042 |
| Control | 12.32 (5.10) | 11.94 (5.49) | 12.55 (4.37) | 12.43 (4.98) | |||
| PTGI-Spiritual Change | Intervention | 5.97 (2.88) | 6.21 (3.13) | 6.41 (2.79) | 6.66 (2.73) | 6.83 | 0.011 |
| Control | 5.00 (3.01) | 4.35 (2.80) | 4.39 (2.84) | 4.70 (2.78) | |||
| PTGI-Appreciation of Life | Intervention | 10.88 (3.06) | 10.35 (3.65) | 11.06 (3.87) | 11.28 (3.42) | 2.69 | 0.106 |
| Control | 9.95 (3.79) | 9.32 (3.55) | 10.06 (3.38) | 9.17 (3.86) | |||
| BRS | Intervention | 3.81 (0.61) | 3.79 (0.60) | 3.99 (0.65) | 3.91 (0.77) | 0.015 | 0.903 |
| Control | 3.75 (0.63) | 3.78 (0.65) | 3.83 (0.53) | 3.90 (0.46) | |||
| SRIS-Total | Intervention | 89.88 (14.41) | 93.85 (13.40) | 91.65 (16.69) | 91.28 (16.82) | 0.18 | 0.673 |
| Control | 94.10 (15.01) | 92.03 (14.06) | 91.58 (13.70) | 91.37 (15.09) | |||
| SRIS-Insight | Intervention | 35.82 (7.37) | 37.65 (6.05) | 38.09 (5.97) | 37.78 (6.21) | 0.11 | 0.742 |
| Control | 37.71 (6.81) | 35.82 (7.64) | 35.94 (7.36) | 36.10 (7.74) | |||
| SRIS-Self-Reflection | Intervention | 54.06 (9.86) | 56.21 (9.03) | 53.56 (11.92) | 53.50 (13.12) | 0.63 | 0.432 |
| Control | 56.39 (10.74) | 56.21 (10.69) | 55.64 (10.63) | 55.27 (10.74) | |||
| SCS-SF | Intervention | 3.19 (0.81) | 3.35 (0.81) | 3.42 (0.77) | 3.44 (0.72) | 0.08 | 0.778 |
| Control | 3.18 (0.79) | 3.16 (0.72) | 3.26 (0.85) | 3.30 (0.71) | |||
| PEI-Total | Intervention | 5.41 (0.90) | 5.82 (0.66) | 5.85 (0.69) | 5.79 (0.74) | 0.45 | 0.505 |
| Control | 5.55 (0.72) | 5.47 (0.99) | 5.54 (0.89) | 5.64 (0.81) | |||
| PEI-Meaning | Intervention | 5.82 (0.86) | 6.20 (0.72) | 6.11 (0.68) | 6.10 (0.69) | 1.35 | 0.250 |
| Control | 5.85 (0.72) | 5.72 (1.04) | 5.81 (0.90) | 5.91 (0.90) | |||
| PEI-Competence | Intervention | 5.35 (1.03) | 5.97 (0.76) | 5.88 (0.86) | 5.79 (1.21) | 0.01 | 0.910 |
| Control | 5.75 (0.76) | 5.70 (0.99) | 5.81 (0.93) | 5.69 (0.68) | |||
| PEI-Self Determination | Intervention | 5.26 (1.02) | 5.63 (0.86) | 5.69 (0.85) | 5.78 (0.90) | 0.20 | 0.656 |
| Control | 5.34 (1.10) | 5.27 (1.15) | 5.42 (1.11) | 5.59 (0.99) | |||
| PEI-Impact | Intervention | 5.22 (1.16) | 5.49 (1.17) | 5.73 (0.92) | 5.47 (1.29) | 0.36 | 0.551 |
| Control | 5.25 (0.98) | 5.19 (1.36) | 5.10 (1.36) | 5.39 (1.29) | |||
| GSE | Intervention | 33.29 (3.91) | 33.91 (3.87) | 33.71 (4.13) | 33.69 (3.84) | 0.12 | 0.727 |
| Control | 33.16 (3.66) | 32.74 (3.34) | 32.79 (3.72) | 33.83 (3.59) | |||
| PSS | Intervention | 16.62 (8.13) | 15.38 (7.11) | 14.74 (7.61) | 16.16 (8.09) | 0.59 | 0.446 |
| Control | 17.66 (7.47) | 17.91 (6.13) | 17.42 (6.49) | 17.13 (6.90) | |||
| ProQOL-CS | Intervention | 40.91 (5.57) | 42.82 (6.28) | 42.38 (5.63) | 41.63 (7.18) | 0.95 | 0.334 |
| Control | 40.66 (5.45) | 40.41 (5.64) | 40.30 (5.41) | 39.90 (6.51) | |||
| ProQOL-Burnout | Intervention | 23.06 (6.45) | 21.47 (6.23) | 20.97 (5.02) | 22.41 (7.44) | 1.06 | 0.308 |
| Control | 24.11 (5.86) | 23.91 (6.37) | 23.97 (6.69) | 23.87 (6.20) | |||
| ProQOL-STS | Intervention | 24.76 (6.46) | 23.76 (6.20) | 22.91 (6.48) | 23.00 (8.53) | 0.15 | 0.703 |
| Control | 24.05 (6.79) | 23.62 (5.63) | 23.48 (6.20) | 23.33 (6.00) | |||
| BIAJS | Intervention | 4.13 (0.78) | 4.12 (0.64) | 4.20 (0.70) | 3.96 (0.71) | 0.87 | 0.354 |
| Control | 3.90 (0.81) | 3.89 (0.90) | 3.88 (1.02) | 3.92 (0.95) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawyer, A.T.; Tao, H.; Bailey, A.K. The Impact of a Psychoeducational Group Program on the Mental Well-Being of Unit-Based Nurse Leaders: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 6035. https://doi.org/10.3390/ijerph20116035
Sawyer AT, Tao H, Bailey AK. The Impact of a Psychoeducational Group Program on the Mental Well-Being of Unit-Based Nurse Leaders: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2023; 20(11):6035. https://doi.org/10.3390/ijerph20116035
Chicago/Turabian StyleSawyer, Amanda T., Hong Tao, and Amanda K. Bailey. 2023. "The Impact of a Psychoeducational Group Program on the Mental Well-Being of Unit-Based Nurse Leaders: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 20, no. 11: 6035. https://doi.org/10.3390/ijerph20116035
APA StyleSawyer, A. T., Tao, H., & Bailey, A. K. (2023). The Impact of a Psychoeducational Group Program on the Mental Well-Being of Unit-Based Nurse Leaders: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 20(11), 6035. https://doi.org/10.3390/ijerph20116035






