Feasibility of a Virtual Educational Programme for Behaviour Change in Cardiac Patients from a Low-Resource Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedures
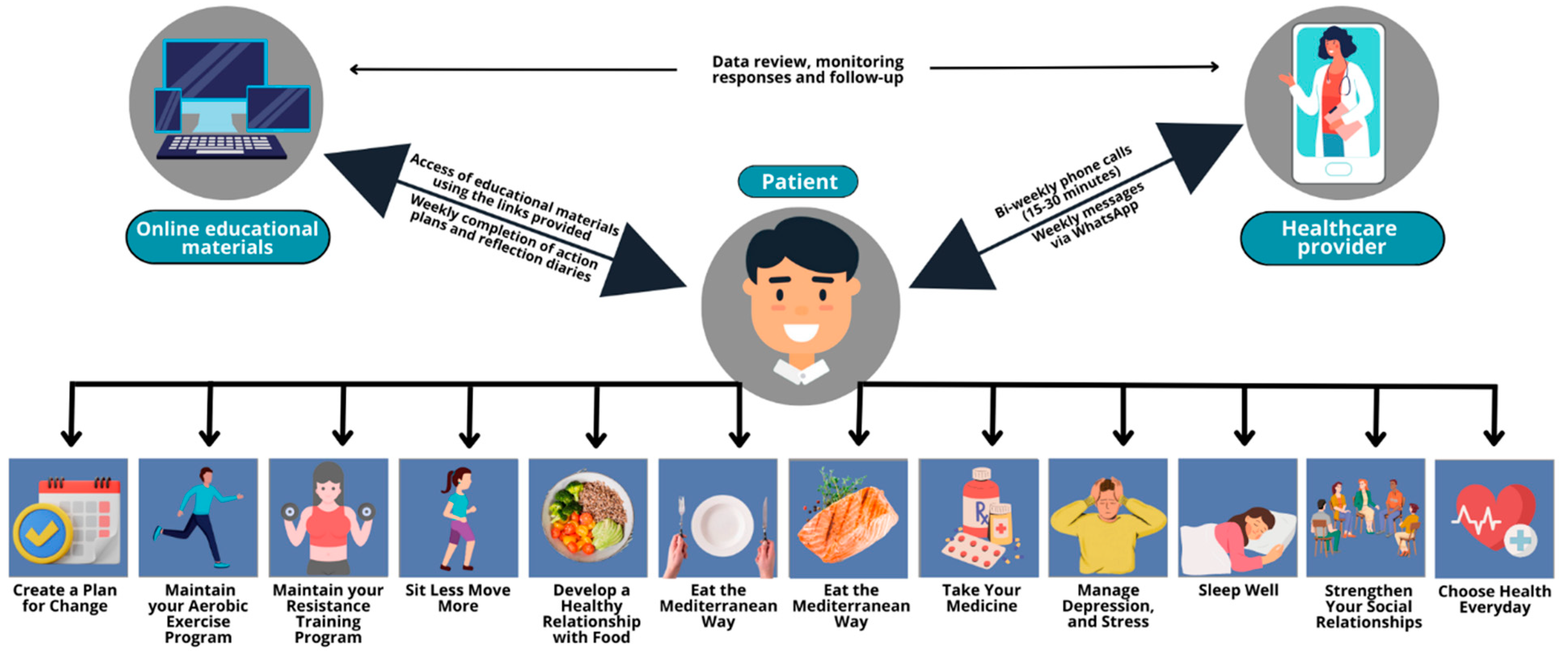
2.4. Intervention
2.5. Feasibility Measures
2.6. Data Analysis
3. Results
3.1. Patient Participants
3.2. Acceptability
3.3. Demand
3.4. Implementation
3.5. Practicality
3.6. Limited Efficacy Testing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- Bowry, A.D.K.; Lewey, J.; Dugani, S.B.; Choudhry, N.K. The Burden of Cardiovascular Disease in Low- and Middle-Income Countries: Epidemiology and Management. Can. J. Cardiol. 2015, 31, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Stevens, B.; Pezzullo, L.; Verdian, L.; Tomlinson, J.; George, A.; Bacal, F. The Economic Burden of Heart Conditions in Brazil. Braz. Arch. Cardiol. 2018, 111, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Landmann-Szwarcwald, C.; Macinko, J. A Panorama of Health Inequalities in Brazil. Int. J. Equity Health 2016, 15, 174. [Google Scholar] [CrossRef]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The Role of Cardiac Rehabilitation in Improving Cardiovascular Outcomes. Nat. Rev. Cardiol. 2022, 19, 180–194. [Google Scholar] [CrossRef]
- Buckley, B.J.R.; De Koning, I.A.; Harrison, S.L.; Fazio-Eynullayeva, E.; Underhill, P.; Kemps, H.M.C.; Lip, G.Y.H.; Thijssen, D.H.J. Exercise-Based Cardiac Rehabilitation vs. Percutaneous Coronary Intervention for Chronic Coronary Syndrome: Impact on Morbidity and Mortality. Eur. J. Prev. Cardiol. 2022, 29, 1074–1080. [Google Scholar] [CrossRef]
- Grace, S.L.; Turk-Adawi, K.I.; Contractor, A.; Atrey, A.; Campbell, N.; Derman, W.; Ghisi, G.L.M.; Oldridge, N.; Sarkar, B.K.; Yeo, T.J.; et al. Cardiac Rehabilitation Delivery Model for Low-Resource Settings. Heart 2016, 102, 1449–1455. [Google Scholar] [CrossRef]
- Shields, G.E.; Wells, A.; Doherty, P.; Heagerty, A.; Buck, D.; Davies, L.M. Cost-Effectiveness of Cardiac Rehabilitation: A Systematic Review. Heart 2018, 104, 1403–1410. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Supervia, M.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.; et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine 2019, 13, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Britto, R.R.; Supervia, M.; Turk-Adawi, K.; Chaves, G.S.D.S.; Pesah, E.; Lopez-Jimenez, F.; Pereira, D.A.G.; Herdy, A.H.; Grace, S.L. Cardiac Rehabilitation Availability and Delivery in Brazil: A Comparison to Other Upper Middle-Income Countries. Braz. J. Phys. Ther. 2020, 24, 167–176. [Google Scholar] [CrossRef]
- Ghisi, G.L.D.M.; Xu, Z.; Liu, X.; Mola, A.; Gallagher, R.; Babu, A.S.; Yeung, C.; Marzolini, S.; Buckley, J.; Oh, P.; et al. Impacts of the COVID-19 Pandemic on Cardiac Rehabilitation Delivery around the World. Glob. Heart 2021, 16, 43. [Google Scholar] [CrossRef] [PubMed]
- Jardim, I.D.S.C.; Milani, M.; Castro, I.; Hansen, D.; Karsten, M.; Cahalin, L.P.; Cipriano, G.F.B.; Cipriano, G. Impacto Da COVID-19 Nos Programas de Reabilitação Cardiovascular No Brasil: Um Estudo Transversal Baseado Em Uma Pesquisa Online. Braz. Arch. Cardiol. 2023, 120, e20220135. [Google Scholar] [CrossRef] [PubMed]
- Ghisi, G.L.M.; Santos, R.Z.; Korbes, A.S.; Souza, C.A.D.; Karsten, M.; Oh, P.; Benetti, M. Percepções Dos Participantes de Reabilitação Cardíaca Sobre Seus Comportamentos Em Saúde e Necessidades de Informação Durante a Pandemia COVID-19 No Brasil. Braz. Arch. Cardiol. 2022, 118, 949–960. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.L.; Gifford, A.L.; Miller, C.J.; Bauer, M.S.; Lehmann, L.S.; Charness, M.E. Provider Perceptions of Virtual Care During the Coronavirus Disease 2019 Pandemic: A Multispecialty Survey Study. Med. Care 2021, 59, 646. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Donald, G. A Brief Summary of Pilot and Feasibility Studies: Exploring Terminology, Aims, and Methods. Eur. J. Integr. Med. 2018, 24, 65–70. [Google Scholar] [CrossRef]
- Ghisi, G.L.D.M.; Aultman, C.; Konidis, R.; Sandison, N.; Oh, P. Developing a Group-Based Virtual Education Curriculum for Cardiac Rehabilitation and the Associated Toolkit to Support Implementation in Canada and across the Globe. Heart Lung 2023, 57, 80–94. [Google Scholar] [CrossRef]
- Ghisi, G.L.D.M.; Chaves, G.S.S.; Loures, J.B.; Bonfim, G.M.; Britto, R. Validation of the Brazilian-Portuguese Version of a Short Questionnaire to Assess Knowledge in Cardiovascular Disease Patients (CADE-Q SV). Braz. Arch. Cardiol. 2018, 111, 841–849. [Google Scholar] [CrossRef]
- Machado, C.C.D.S.; Malaguti, C.; Trevizan, P.F.; Ezequiel, D.G.A.; Seixas, M.B.; Da Silva, L.P. Psychometric Validation of the Brazilian Portuguese Version of Bandura’s Exercise Self-Efficacy Scale in Diabetes Patients. J. Diabetes Metab. Disord. 2020, 19, 925–932. [Google Scholar] [CrossRef]
- Araujo, P.A.B.D.; Sties, S.W.; Wittkopf, P.G.; Netto, A.S.; Gonzáles, A.I.; Lima, D.P.; Guimarães, S.N.; Aranha, E.E.; Andrade, A.; Carvalho, T.D. Índice da qualidade do sono de Pittsburgh para uso na reabilitação cardiopulmonar e metabólica. Rev. Bras. Med. Esporte 2015, 21, 472–475. [Google Scholar] [CrossRef]
- De Lima Osório, F.; Mendes, A.V.; Crippa, J.A.; Loureiro, S.R. Study of the Discriminative Validity of the PHQ-9 and PHQ-2 in a Sample of Brazilian Women in the Context of Primary Health Care. Perspect. Psychiatr. Care 2009, 45, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and Analysis of Pilot Studies: Recommendations for Good Practice: Design and Analysis of Pilot Studies. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Villagomez, P.; Zurlini, C.; Wimmer, M.; Roberts, L.; Trieu, B.; McGrath, B.; Wiesel, R.; Ologhobo, T.; Goldsmith, S.; Robbins, L. Shift to Virtual Self-Management Programs During COVID-19: Ensuring Access and Efficacy for Older Adults. Front. Public Health 2021, 9, 663875. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Ghisi, G.L.M.; Zhang, L.; Hyun, K.; Pakosh, M.; Gallagher, R. Systematic Review, Meta-Analysis and Meta-Regression to Determine the Effects of Patient Education on Health Behaviour Change in Adults Diagnosed with Coronary Heart Disease. J. Clin. Nurs. 2022. [Google Scholar] [CrossRef]
- Pavy, B.; Barbet, R.; Carré, F.; Champion, C.; Iliou, M.-C.; Jourdain, P.; Juillière, Y.; Monpère, C.; Brion, R. Therapeutic Education in Coronary Heart Disease: Position Paper from the Working Group of Exercise Rehabilitation and Sport (GERS) and the Therapeutic Education Commission of the French Society of Cardiology. Arch. Cardiov. Dis. 2013, 106, 680–689. [Google Scholar] [CrossRef]
- Shi, W.; Ghisi, G.L.M.; Zhang, L.; Hyun, K.; Pakosh, M.; Gallagher, R. A Systematic Review, Meta-Analysis, and Meta-Regression of Patient Education for Secondary Prevention in Patients with Coronary Heart Disease: Impact on Psychological Outcomes. Eur. J. Cardiov. Nurs. 2022, 21, 643–654. [Google Scholar] [CrossRef]
- Pool, M.D.O.; Hooglugt, J.-L.Q.; Schijven, M.P.; Mulder, B.J.M.; Bouma, B.J.; De Winter, R.J.; Pinto, Y.; Winter, M.M. Review of Digitalized Patient Education in Cardiology: A Future Ahead? Cardiology 2021, 146, 263–271. [Google Scholar] [CrossRef]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. Glob. Heart 2017, 12, 323. [Google Scholar] [CrossRef]
- de Melo Ghisi, G.L.; Dos Santos, R.Z.; Aranha, E.E.; Nunes, A.D.; Oh, P.; Benetti, M.; Grace, S.L. Perceptions of Barriers to Cardiac Rehabilitation Use in Brazil. Vasc. Health Risk Manag. 2013, 9, 485–491. [Google Scholar] [CrossRef]
- Whitehead, D. Health Promotion and Health Education: Advancing the Concepts. J. Adv. Nurs. 2004, 47, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Zamani-Alavijeh, F.; Araban, M.; Harandy, T.F.; Bastami, F.; Almasian, M. Sources of Health Care Providers’ Self-Efficacy to Deliver Health Education: A Qualitative Study. BMC Med. Educ. 2019, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Mardani Hamuleh, M.; Shahraki Vahed, A.; Roozitalab, M. A comparison of the importance of patient educational programs in the viewpoint of nurses and patients. Pars J. Med. Sci. 2010, 8, 49–55. [Google Scholar] [CrossRef]
- Abdi, A.; Izadi, A.; Vafaeei, K.; Lorestani, E. Assessment of patient education barriers in viewpoint of nurses and general physicians. Res. J. Appl. Basic Sci. 2014, 8, 2252–2256. [Google Scholar]
- Farahani, M.A.; Mohammadi, E.; Ahmadi, F.; Mohammadi, N. Factors influencing the patient education: A qualitative research. Iran. J. Nurs. Midwifery Res. 2013, 18, 133. [Google Scholar] [PubMed]
- Vanzella, L.M.; Oh, P.; Pakosh, M.; Ghisi, G.L.D.M. Barriers and Facilitators to Virtual Education in Cardiac Rehabilitation: A Systematic Review of Qualitative Studies. Eur. J. Cardiov. Nurs. 2022, 21, 414–429. [Google Scholar] [CrossRef]
- Hwang, R.; Mandrusiak, A.; Morris, N.R.; Peters, R.; Korczyk, D.; Bruning, J.; Russell, T. Exploring Patient Experiences and Perspectives of a Heart Failure Telerehabilitation Program: A Mixed Methods Approach. Heart Lung 2017, 46, 320–327. [Google Scholar] [CrossRef]
| Feasibility Measure | Definition | Outcomes | Data Source | Data Analysis |
|---|---|---|---|---|
| Acceptability | To what extent the intervention is suitable and satisfying for target individuals | Patients’ satisfaction with the intervention | Satisfaction questionnaire designed for patient participants (6 questions) | Descriptive statistics (Likert-type scale) and qualitative analysis (open-ended questions) |
| Healthcare providers’ satisfaction with delivering education virtually to patients | Satisfaction questionnaire designed for healthcare providers delivering the intervention (3 questions) | |||
| Demand | To what extent the programme is likely to be used | Patients: internet access, device to access Internet, use of Internet to search for health information, reasons to participate in the virtual educational programme | Questionnaire about Internet use (4 questions) | Descriptive statistics (frequency) |
| Perceived demand reported by patients (usefulness of information and effectiveness of bi-weekly) | ||||
| Implementation | To what extent can the intervention be fully implemented as planned | Access and use of virtual education tools (weekly educational materials, completion of weekly action plans and reflection diaries) | Data recorded from the links provided and self-reported by patients | Descriptive statistics (frequency) and qualitative analysis (open-ended questions) |
| Healthcare providers’ perceptions about success and failure of the intervention | Semi-structured 1:1 interview with healthcare providers delivering the intervention | |||
| Practicality | To what extent can the intervention be performed by participants using the intended means and resources | Ability of patient participants to carry out intervention activities and maintain healthy habits after end of intervention | Semi-structured 1:1 interview with patient participants | Qualitative analysis (open-ended questions) |
| Healthcare providers’ perceptions about factors affecting implementation ease or difficulty | Semi-structured 1:1 interview with healthcare providers delivering the intervention | |||
| Limited efficacy testing | What are the preliminary impacts of the intervention on study variables | Preliminary effects of the intervention on disease-related knowledge, exercise self-efficacy, sleep quality, depressive symptoms, and physical activity level | Psychometric validated questionnaires completed by patient participants pre- and post-intervention | Descriptive statistics (Δ post-pre) |
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 22 (64.7) |
| Female | 12 (35.3) |
| Marital Status | |
| Married | 21 (61.8) |
| Divorced | 5 (14.6) |
| Widow | 4 (11.8) |
| Single | 4 (11.8) |
| Highest Educational Level | |
| High school or lower | 20 (58.8) |
| More than high school | 13 (38.3) |
| No information | 1 (2.9) |
| Monthly Family Income a | |
| 5 minimum wages or under | 20 (58.8) |
| More than 5 minimum wages | 8 (23.5) |
| No information | 6 (17.6) |
| Cardiac Diagnosis/Procedures b | |
| Heart failure | 22 (64.7) |
| Acute myocardial infarction | 21 (61.8) |
| Percutaneous coronary intervention | 18 (52.9) |
| Coronary artery disease | 18 (52.9) |
| Coronary artery bypass graft | 10 (29.4) |
| Cardiovascular Risk Factors b | |
| Hypertension | 25 (73.5) |
| Dyslipidaemia | 15 (44.1) |
| Smoking (current or past) | 15 (44.1) |
| Diabetes Type II | 12 (35.3) |
| Duration of CR Participation | |
| Between 6 and 12 months | 5 (14.7) |
| 12 months | 3 (8.8) |
| Between 13 and 18 months | 20 (58.8) |
| More than 18 months | 6 (17.6) |
| Feasibility Measure | Outcome | Description | Results a |
|---|---|---|---|
| Acceptability | Satisfaction (patients) | Overall satisfaction with the programme | 9.0 (7.4–10.0)/10 |
| Satisfaction with the educational content | 9.0 (8.6–9.5)/10 | ||
| Satisfaction with the delivery of education (i.e., via WhatsApp) | 9.0 (8.1–10.0)/10 | ||
| Satisfaction with the action plans and diaries | 9.1 (8.9–10.0)/10 | ||
| Satisfaction (healthcare providers) | Overall satisfaction with the programme | 9.8 (9.6–10.0)/10 | |
| Satisfaction with the educational content | 8.5 (7.3–9.0)/10 | ||
| Satisfaction with the delivery of education (i.e., via WhatsApp) | 8.1 (7.7–9.0)/10 | ||
| Demand | Internet use (patients) | Have internet access | 18 (90.0) |
| Device mostly used to access internet: cell phone | 16 (80.0) | ||
| Use of Internet to search for health information | 14 (70.0) | ||
| Reasons to participate in the virtual educational programme (patients) | Opportunity to learn about exercise | 8 (40.0) | |
| Maintain or improve health through education | 8 (40.0) | ||
| Learn about their overall health condition | 5 (25.0) | ||
| Stay in touch with programme during the pandemic | 3 (15.0) | ||
| Perceived demand (patients) | Usefulness of information, yes | 20 (100.0) | |
| Effectiveness of bi-weekly calls, yes | 18 (90.0) | ||
| Implementation b | Access and use of virtual education tools | Use of weekly educational materials (video and booklet) | 34 (100.0) |
| Creation of weekly learning plans | 18 (53.0) | ||
| Creation of reflection diaries | 16 (47.0) | ||
| Practicality | Ability of patient participants to carry out intervention activities and maintain healthy habits after end of intervention | Heart health behaviours changed after intervention, yes | 19 (95.0) |
| Maximum Score | Pre-Intervention Scores | Post-Intervention Scores | Δ Post-Pre * | |
|---|---|---|---|---|
| Disease-related knowledge | 20 | 8.9 ± 3.2 | 6.9 ± 4.2 | −2.0 |
| Exercise self-efficacy | 100 | 53.9 ± 15.9 | 56.7 ± 13.7 | +2.8 |
| Sleep quality | 21 | 6.4 ± 4.3 | 5.3 ± 4.4 | −1.1 |
| Depressive symptoms | 6 | 1.6 ± 1.9 | 1.1 ± 1.4 | −0.5 |
| High-intensity physical activity level | 34 (100%) | 6 (40%) | 14 (70%) | +30% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, R.Z.d.; Almeida, S.; Scheafer, A.K.; Karsten, M.; Oh, P.; Benetti, M.; Ghisi, G.L.d.M. Feasibility of a Virtual Educational Programme for Behaviour Change in Cardiac Patients from a Low-Resource Setting. Int. J. Environ. Res. Public Health 2023, 20, 5934. https://doi.org/10.3390/ijerph20115934
Santos RZd, Almeida S, Scheafer AK, Karsten M, Oh P, Benetti M, Ghisi GLdM. Feasibility of a Virtual Educational Programme for Behaviour Change in Cardiac Patients from a Low-Resource Setting. International Journal of Environmental Research and Public Health. 2023; 20(11):5934. https://doi.org/10.3390/ijerph20115934
Chicago/Turabian StyleSantos, Rafaella Zulianello dos, Sidnei Almeida, Andrea Korbes Scheafer, Marlus Karsten, Paul Oh, Magnus Benetti, and Gabriela Lima de Melo Ghisi. 2023. "Feasibility of a Virtual Educational Programme for Behaviour Change in Cardiac Patients from a Low-Resource Setting" International Journal of Environmental Research and Public Health 20, no. 11: 5934. https://doi.org/10.3390/ijerph20115934
APA StyleSantos, R. Z. d., Almeida, S., Scheafer, A. K., Karsten, M., Oh, P., Benetti, M., & Ghisi, G. L. d. M. (2023). Feasibility of a Virtual Educational Programme for Behaviour Change in Cardiac Patients from a Low-Resource Setting. International Journal of Environmental Research and Public Health, 20(11), 5934. https://doi.org/10.3390/ijerph20115934








