COVID-19-Related Testing, Knowledge and Behaviors among Severe and Chronic Non-Communicable Disease Patients in Neno District, Malawi: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Sociodemographic Characteristics of Patient and Respondents
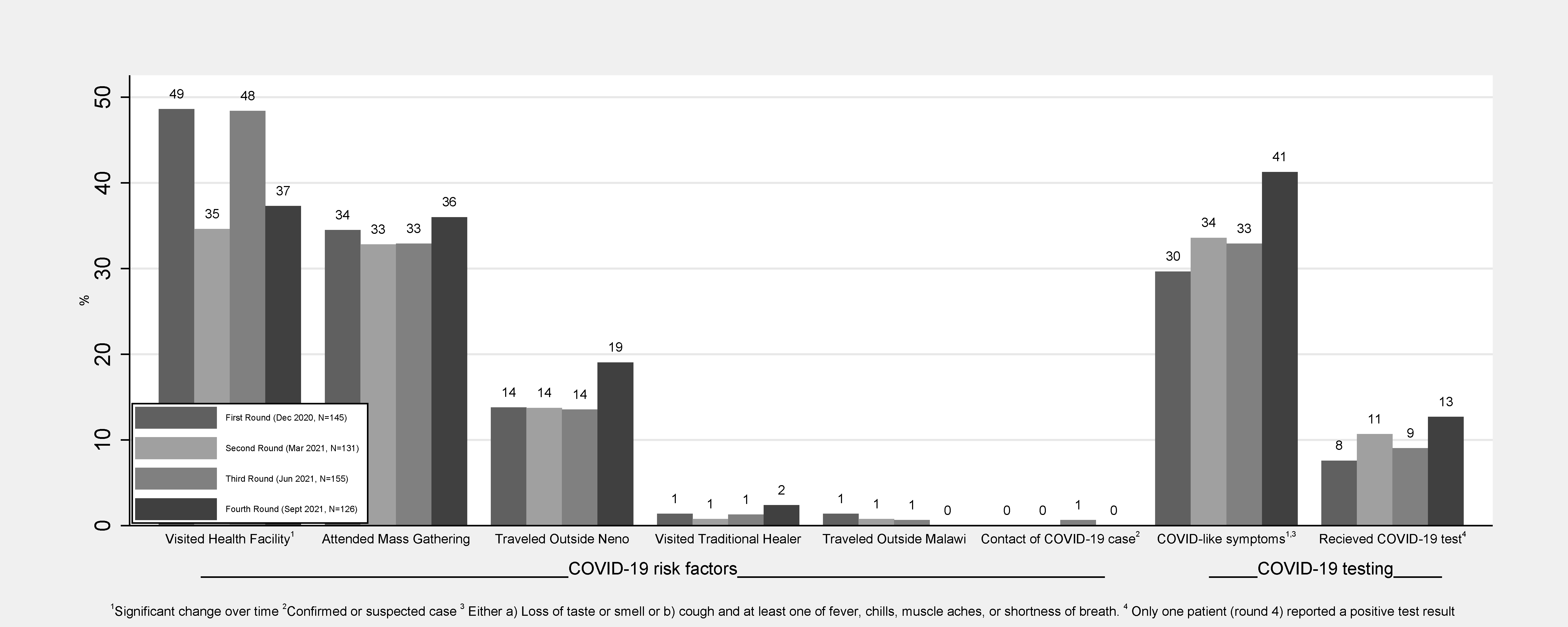
3.2. COVID-19 Risks, Symptoms and Testing among Patients
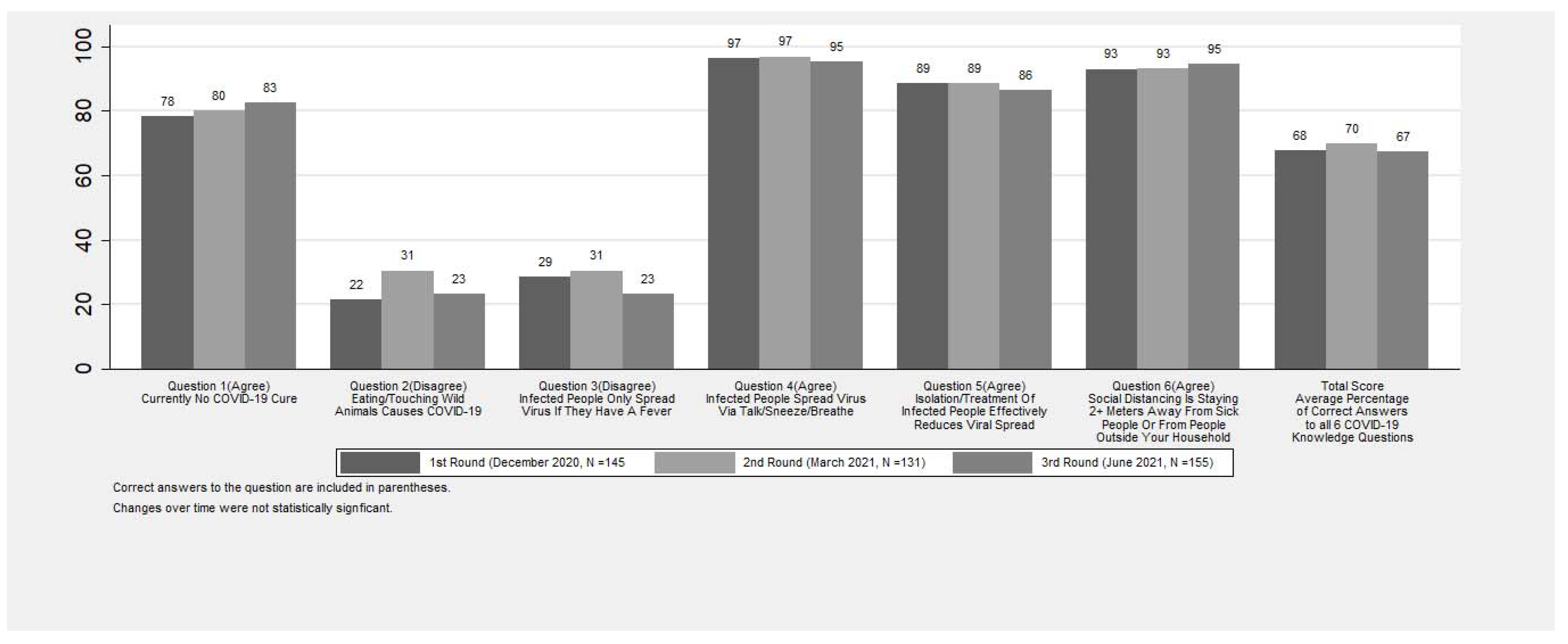
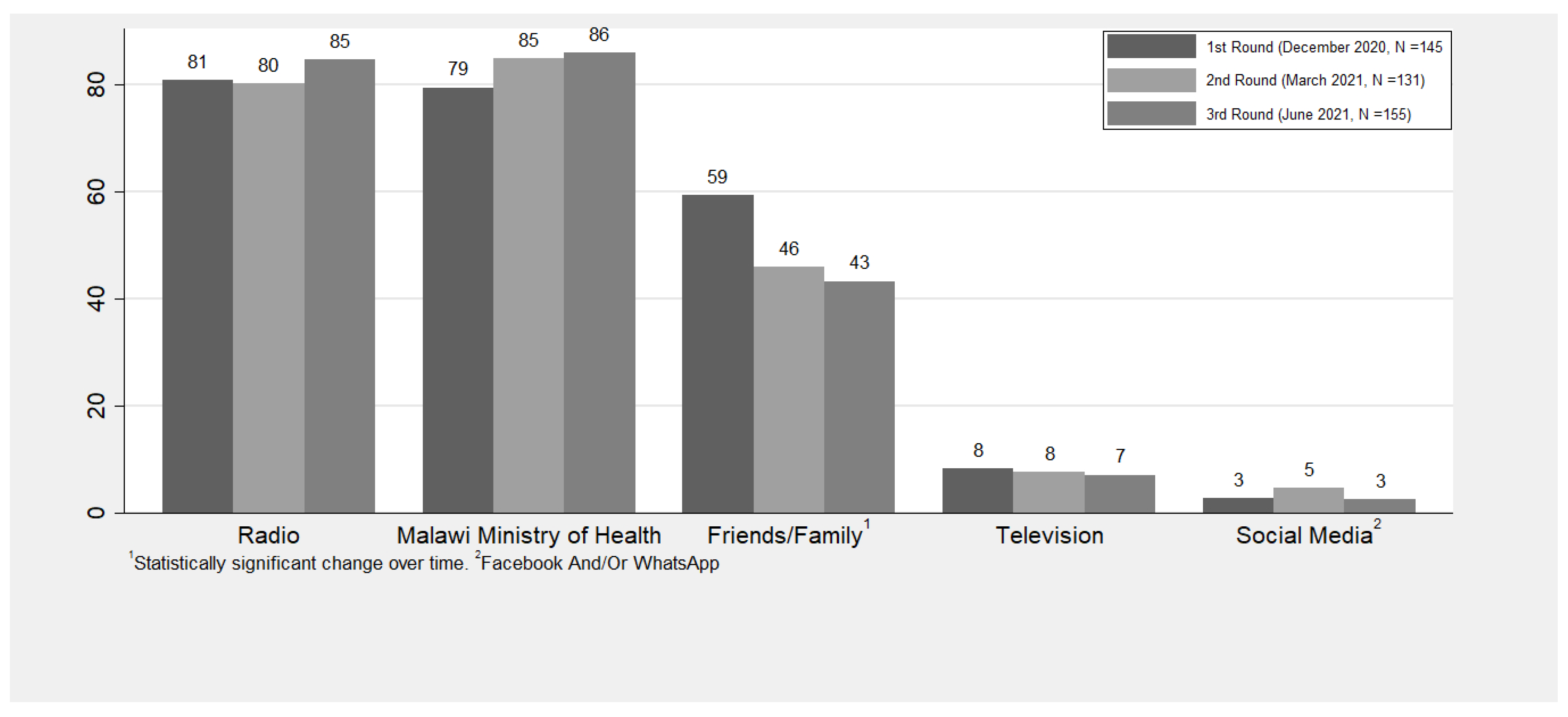
3.3. COVID-19 Knowledge among Respondents
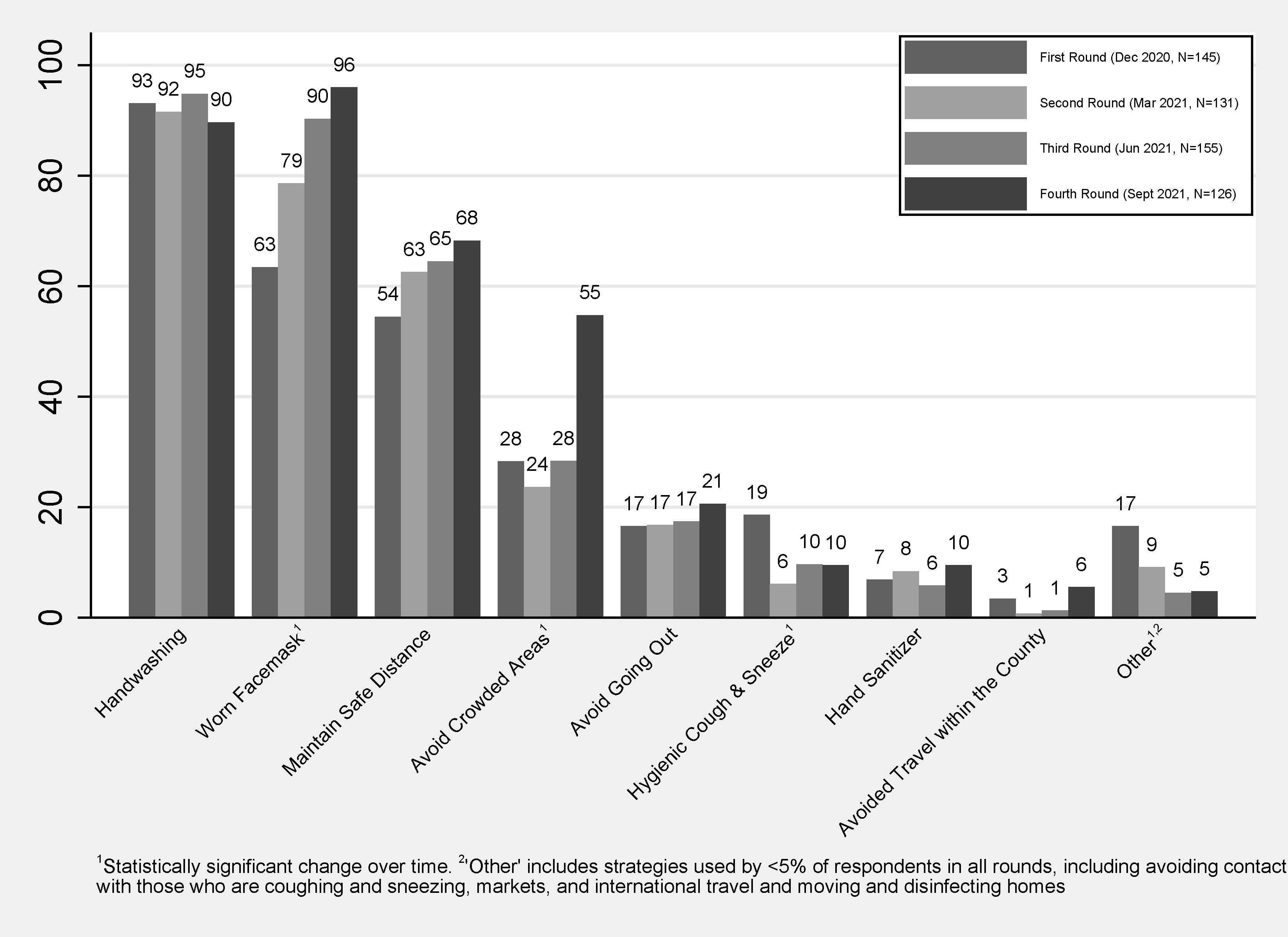
3.4. Infection Prevention Strategy among Households
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Geldsetzer, P. Knowledge and Perceptions of COVID-19 Among the General Public in the United States and the United Kingdom: A Cross-sectional Online Survey. Ann. Intern. Med. 2020, 173, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Bekele, F.; Sheleme, T.; Fekadu, G. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: A systematic review. SAGE Open Med. 2020, 8, 2050312120970721. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, G.; Egolet, R.O.; Yang, R.; Huang, Y.; Zheng, Z. Knowledge, Attitudes, and Practices Related to COVID-19 Among Malawi Adults: A Community-Based Survey. Int. J. Environ. Res. Public Health 2021, 18, 4090. [Google Scholar] [CrossRef] [PubMed]
- Banda, J.; Dube, A.; Brumfield, S.; Amoah, A.; Crampin, A.; Reniers, G.; Helleringer, S. Knowledge, risk perceptions, and behaviors related to the COVID-19 pandemic in Malawi. Demogr. Res. 2021, 44, 459–480. [Google Scholar] [CrossRef]
- Akalu, Y.; Ayelign, B.; Molla, M.D. Knowledge, Attitude and Practice towards COVID-19 among Chronic Disease Patients at Addis Zemen Hospital, Northwest Ethiopia. Infect. Drug Resist. 2020, 13, 1949–1960. [Google Scholar] [CrossRef]
- Melesie Taye, G.; Bose, L.; Beressa, T.B.; Tefera, G.M.; Mosisa, B.; Dinsa, H.; Birhanu, A.; Umeta, G. COVID-19 Knowledge, Attitudes, and Prevention Practices among People with Hypertension and Diabetes Mellitus Attending Public Health Facilities in Ambo, Ethiopia. Infect. Drug Resist. 2020, 13, 4203–4214. [Google Scholar] [CrossRef]
- Huynh, G.; Nguyen, M.Q.; Tran, T.T.; Nguyen, V.T.; Nguyen, T.V.; Do, T.H.T.; Nguyen, P.H.N.; Phan, T.H.Y.; Vu, T.T.; Nguyen, T.N.H. Knowledge, Attitude, and Practices Regarding COVID-19 among Chronic Illness Patients at Outpatient Departments in Ho Chi Minh City, Vietnam. Risk Manag. Healthc. Policy 2020, 13, 1571–1578. [Google Scholar] [CrossRef]
- Brosh-Nissimov, T.; Orenbuch-Harroch, E.; Chowers, M.; Elbaz, M.; Nesher, L.; Stein, M.; Maor, Y.; Cohen, R.; Hussein, K.; Weinberger, M.; et al. BNT162b2 vaccine breakthrough: Clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clin. Microbiol. Infect. 2021, 27, 1652–1657. [Google Scholar] [CrossRef]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef]
- Wang, B.; Li, R.; Lu, Z.; Huang, Y. Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis. Aging (Albany NY) 2020, 12, 6049–6057. [Google Scholar] [CrossRef]
- Saban, M.; Myers, V.; Wilf-Miron, R. Changes in infectivity, severity and vaccine effectiveness against delta COVID-19 variant ten months into the vaccination program: The Israeli case. Prev. Med. 2022, 154, 106890. [Google Scholar] [CrossRef] [PubMed]
- Tregoning, J.S.; Flight, K.E.; Higham, S.L.; Wang, Z.; Pierce, B.F. Progress of the COVID-19 vaccine effort: Viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat. Rev. Immunol. 2021, 21, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Rouw, A.; Wexler, A.; Kates, J.; MIchaud, J.; Global COVID-19 vaccine access: A snapshot of inequality. Kaiser Family Found. 2021. Available online: https://www.kff.org/policy-watch/global-covid-19-vaccine-access-snapshot-of-inequality/ (accessed on 12 June 2022).
- World Health Organization. Malawi Marks One Year of COVID-19 Vaccination, 828, 080 People Receive Full Dose. Available online: https://www.afro.who.int/countries/malawi/news/malawi-marks-one-year-covid-19-vaccination-828-080-people-receive-full-dose (accessed on 1 April 2022).
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors affecting COVID-19 vaccine acceptance: An international survey among low- and middle-income countries. Vaccines 2021, 9, 515. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Id, Y.K.; Yitayih, Y.; Birhanu, Z.; Mekonen, S. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS ONE 2020, 15, e0233744. [Google Scholar] [CrossRef]
- Nwagbara, U.I.; Osual, E.C.; Chireshe, R.; Bolarinwa, O.A.; Saeed, B.Q.; Khuzwayo, N.; Hlongwana, K.W. Knowledge, attitude, perception, and preventative practices towards COVID-19 in sub-Saharan Africa: A scoping review. PLoS ONE 2021, 16, e0249853. [Google Scholar] [CrossRef]
- Saadatjoo, S.; Miri, M.; Hassanipour, S.; Ameri, H.; Arab-Zozani, M. Knowledge, attitudes, and practices of the general population about coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis with policy recommendations. Public Health 2021, 194, 185–195. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Angawi, K.; Alshareef, N.; Qattan, A.M.N.; Helmy, H.Z.; Abudawood, Y.; Alqurashi, M.; Kattan, W.M.; Kadasah, N.A.; Chirwa, G.C.; et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: A cross-sectional study. Front. Public Health 2020, 8, 217. [Google Scholar] [CrossRef]
- Josephson, A.; Kilic, T.; Michler, J.D. Socioeconomic impacts of COVID-19 in low-income countries. Nat. Hum. Behav. 2021, 5, 557–565. [Google Scholar] [CrossRef]
- NSO. Malawi National and District Population Projections 2018–2050; National Statistical Office: Zomba, Malawi, 2020; pp. 1–276. [Google Scholar]
- National Statistical Office. 2018 Malawi Population and Housing Census Main Report; National Statistical Office: Zomba, Malawi, 2019; pp. 1–311. [Google Scholar]
- Bukhman, G.; Mocumbi, A.O.; Atun, R.; Becker, A.E.; Bhutta, Z.; Binagwaho, A.; Clinton, C.; Coates, M.M.; Dain, K.; Ezzati, M.; et al. The Lancet NCDI Poverty Commission: Bridging a gap in universal health coverage for the poorest billion. Lancet 2020, 396, 991–1044. [Google Scholar] [CrossRef]
- World Health Organization. PEN-Plus Meeting in Kigali—The Management and Treatment of Non-Communicable Diseases at Primary Levels Strengthened. Available online: https://www.afro.who.int/news/pen-plus-meeting-kigali-management-and-treatment-non-communicable-diseases-primary-levels (accessed on 1 February 2022).
- Thekkur, P.; Tweya, H.; Phiri, S.; Mpunga, J.; Kalua, T.; Kumar, A.M.V.; Satyanarayana, S.; Shewade, H.D.; Khogali, M.; Zachariah, R.; et al. Assessing the impact of COVID-19 on TB and HIV programme services in selected health facilities in Lilongwe, Malawi: Operational research in real time. Trop. Med. Infect. Dis. 2021, 6, 81. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Banda, J.; Dube, A.N.; Brumfield, S.; Crampin, A.C.; Reniers, G.; Amoah, A.S.; Helleringer, S. Controlling the first wave of the COVID–19 pandemic in Malawi: Results from a panel study. medRxiv 2021. [Google Scholar] [CrossRef]
- COVID Testing. Available online: https://6272f24a8d07c305fab981fc--covid-protocols-web.netlify.app/en/addendum/ward-design-troubleshooting/ (accessed on 12 June 2022).
- Ferree, K.E.; Harris, A.S.; Dulani, B.; Kao, K.; Lust, E.; Metheney, E. Stigma, trust, and procedural integrity: COVID-19 testing in Malawi. World Dev. 2021, 141, 105351. [Google Scholar] [CrossRef] [PubMed]
- Chibwana, M.G.; Jere, K.C.; Kamn’gona, R.; Mandolo, J.; Katunga-Phiri, V.; Tembo, D.; Mitole, N.; Musasa, S.; Sichone, S.; Lakudzala, A.; et al. High SARS-CoV-2 seroprevalence in health care workers but relatively low numbers of deaths in urban Malawi. medRxiv 2020. [Google Scholar] [CrossRef]
- Abdelmoniem, R.; Fouad, R.; Shawky, S.; Amer, K.; Elnagdy, T.; Hassan, W.A.; Ali, A.M.; Ezzelarab, M.; Gaber, Y.; Badary, H.A.; et al. SARS-CoV-2 infection among asymptomatic healthcare workers of the emergency department in a tertiary care facility. J. Clin. Virol. 2021, 134, 104710. [Google Scholar] [CrossRef]
- Mandolo, J.; Msefula, J.; Henrion, M.Y.R.; Brown, C.; Moyo, B.; Samon, A.; Moyo-Gwete, T.; Makhado, Z.; Ayres, F.; Motlou, T.; et al. SARS-CoV-2 exposure in Malawian blood donors: An analysis of seroprevalence and variant dynamics between January 2020 and July 2021. BMC Med. 2021, 19, 303. [Google Scholar] [CrossRef]
| N (%) | |
|---|---|
| Round of Enrollment | |
| First Round (December 2020) | 145 (75.5%) |
| Second Round (March 2021) | 5 (2.6%) |
| Third Round (June 2021) | 42 (21.9%) |
| Fourth Round (September 2021) | 0 (0.0%) |
| Patient Sex | |
| Female | 101 (52.6%) |
| Male | 91 (47.4%) |
| Patient Age | |
| ≤5 years | 9 (4.7%) |
| 6–17 | 16 (8.3%) |
| 18–39 | 39 (20.3%) |
| 40–59 | 57 (29.7%) |
| ≥60 | 71 (37.0%) |
| Patient’s Clinical Program | |
| Type 1 Diabetes | 50 (26.0%) |
| Hypertension | 38 (19.8%) |
| Chronic Heart Failure | 34 (17.7%) |
| Type 2 Diabetes | 20 (10.4%) |
| Chronic liver disease/cirrhosis | 16 (8.3%) |
| Rheumatic/another heart disease | 17 (8.9%) |
| Chronic Kidney Disease | 10 (5.2%) |
| Other | 7 (3.6%) |
| Patient’s number of conditions | |
| 1 | 78 (40.6%) |
| 2 | 70 (36.5%) |
| ≥3 | 44 (22.9%) |
| Respondent type | |
| Patient | 126 (65.6%) |
| Parent | 20 (10.4%) |
| Child | 23 (12.0%) |
| Spouse | 9 (4.7%) |
| Grandparent | 6 (3.1%) |
| Other | 8 (4.2%) |
| Respondent’s Sex | |
| Female | 111 (57.8%) |
| Male | 81 (42.2%) |
| Respondent’s Age | |
| 18–39 | 65 (33.9%) |
| 40–59 | 73 (38.0%) |
| ≥60 | 54 (28.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaniku, H.R.; Aron, M.B.; Vrkljan, K.; Tyagi, K.; Ndambo, M.K.; Banda, G.M.; Nyirongo, R.; Mphande, I.; Mailosi, B.; Talama, G.; et al. COVID-19-Related Testing, Knowledge and Behaviors among Severe and Chronic Non-Communicable Disease Patients in Neno District, Malawi: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2023, 20, 5877. https://doi.org/10.3390/ijerph20105877
Zaniku HR, Aron MB, Vrkljan K, Tyagi K, Ndambo MK, Banda GM, Nyirongo R, Mphande I, Mailosi B, Talama G, et al. COVID-19-Related Testing, Knowledge and Behaviors among Severe and Chronic Non-Communicable Disease Patients in Neno District, Malawi: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2023; 20(10):5877. https://doi.org/10.3390/ijerph20105877
Chicago/Turabian StyleZaniku, Haules Robbins, Moses Banda Aron, Kaylin Vrkljan, Kartik Tyagi, Myness Kasanda Ndambo, Gladys Mtalimanja Banda, Revelation Nyirongo, Isaac Mphande, Bright Mailosi, George Talama, and et al. 2023. "COVID-19-Related Testing, Knowledge and Behaviors among Severe and Chronic Non-Communicable Disease Patients in Neno District, Malawi: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 20, no. 10: 5877. https://doi.org/10.3390/ijerph20105877
APA StyleZaniku, H. R., Aron, M. B., Vrkljan, K., Tyagi, K., Ndambo, M. K., Banda, G. M., Nyirongo, R., Mphande, I., Mailosi, B., Talama, G., Munyaneza, F., Connolly, E., Dullie, L., Barnhart, D. A., & Ruderman, T. (2023). COVID-19-Related Testing, Knowledge and Behaviors among Severe and Chronic Non-Communicable Disease Patients in Neno District, Malawi: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 20(10), 5877. https://doi.org/10.3390/ijerph20105877








