Added Breathing Resistance during Exercise Impairs Pulmonary Ventilation and Exaggerates Exercise-Induced Hypoxemia Leading to Impaired Aerobic Exercise Performance
Abstract
1. Introduction
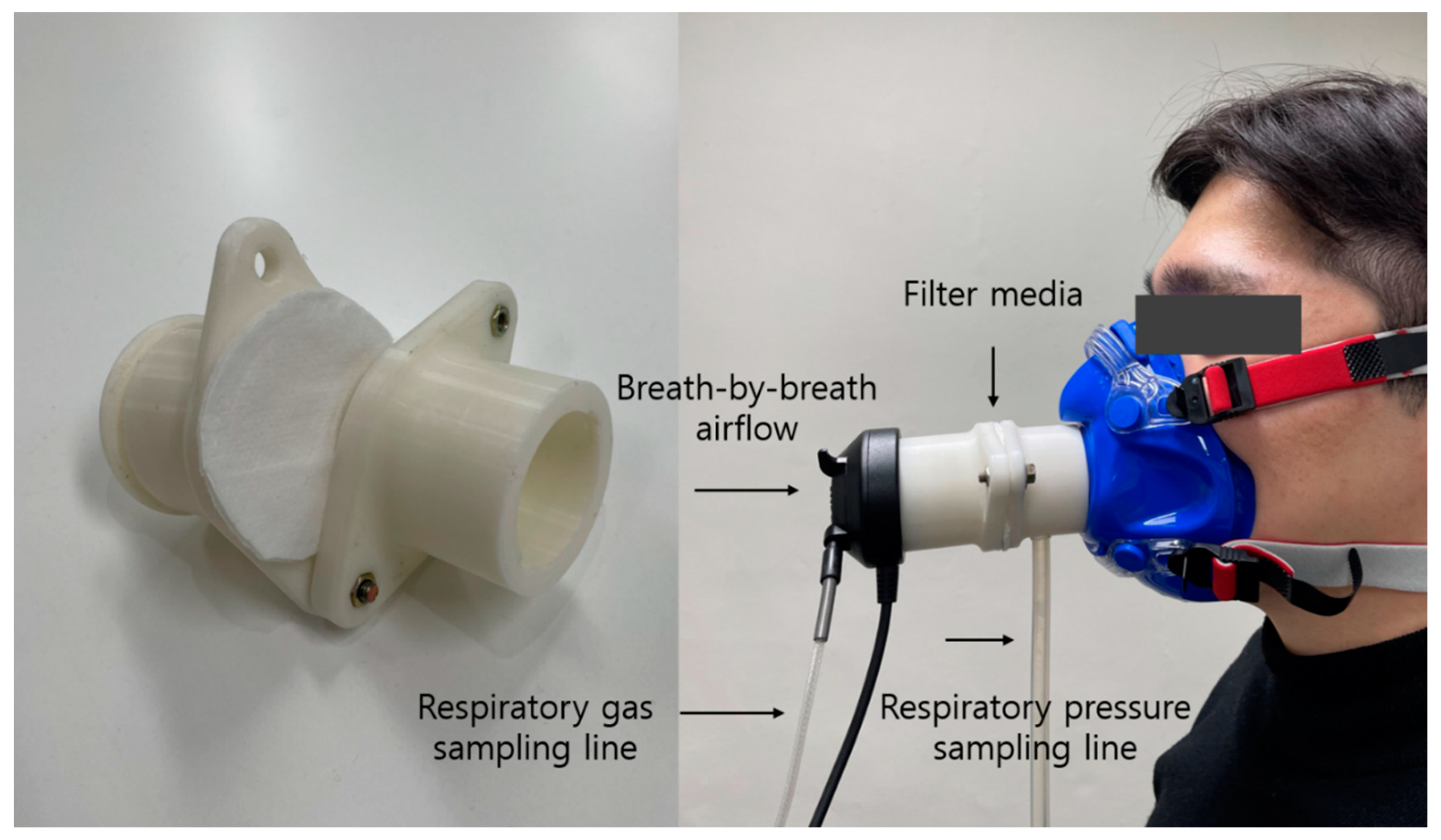
2. Materials and Methods
2.1. Participants
2.2. Experimental Design
2.3. Experimental Procedure
2.4. Statistics
3. Results
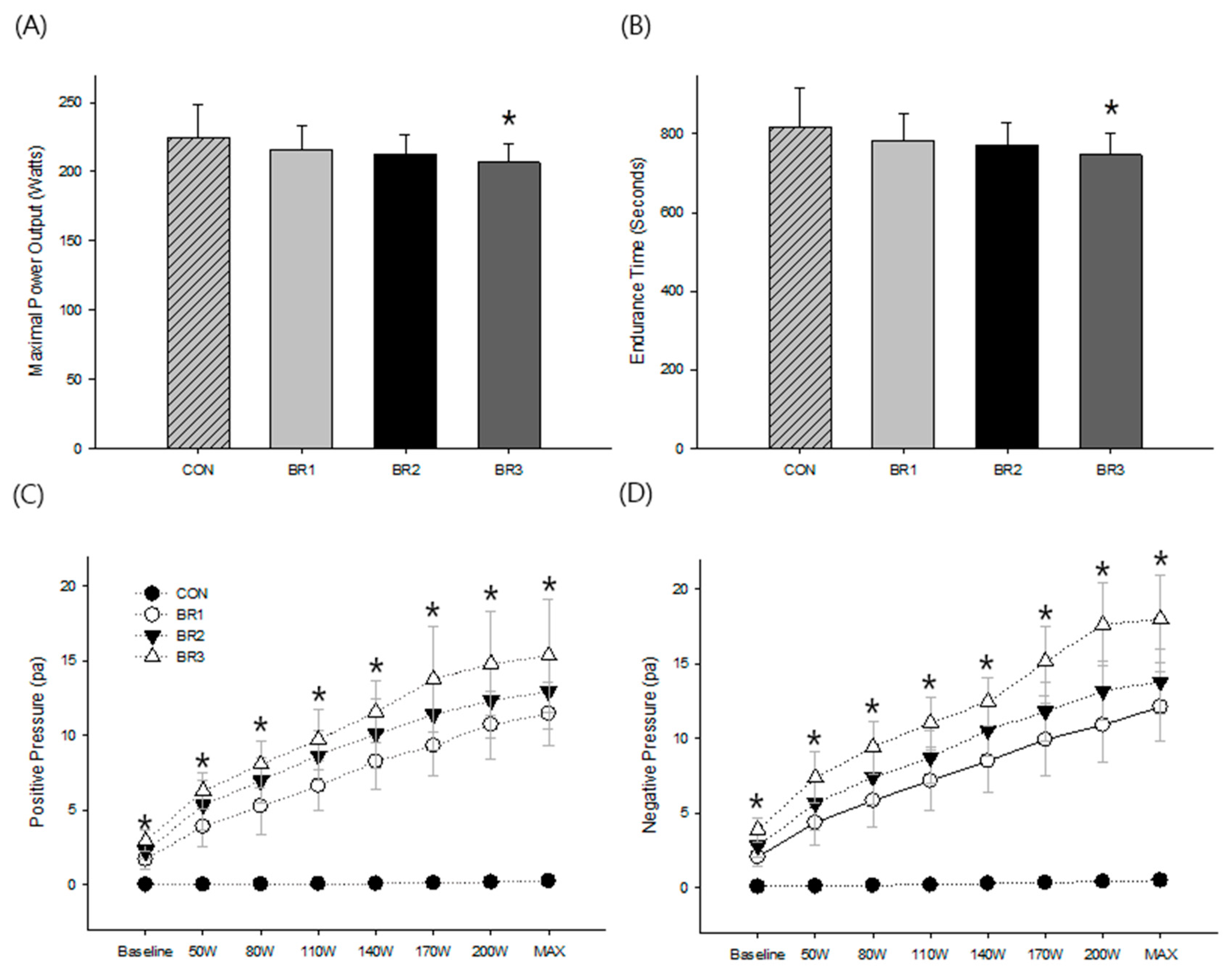
3.1. Exercise Performance
3.2. Respiratory Pressure
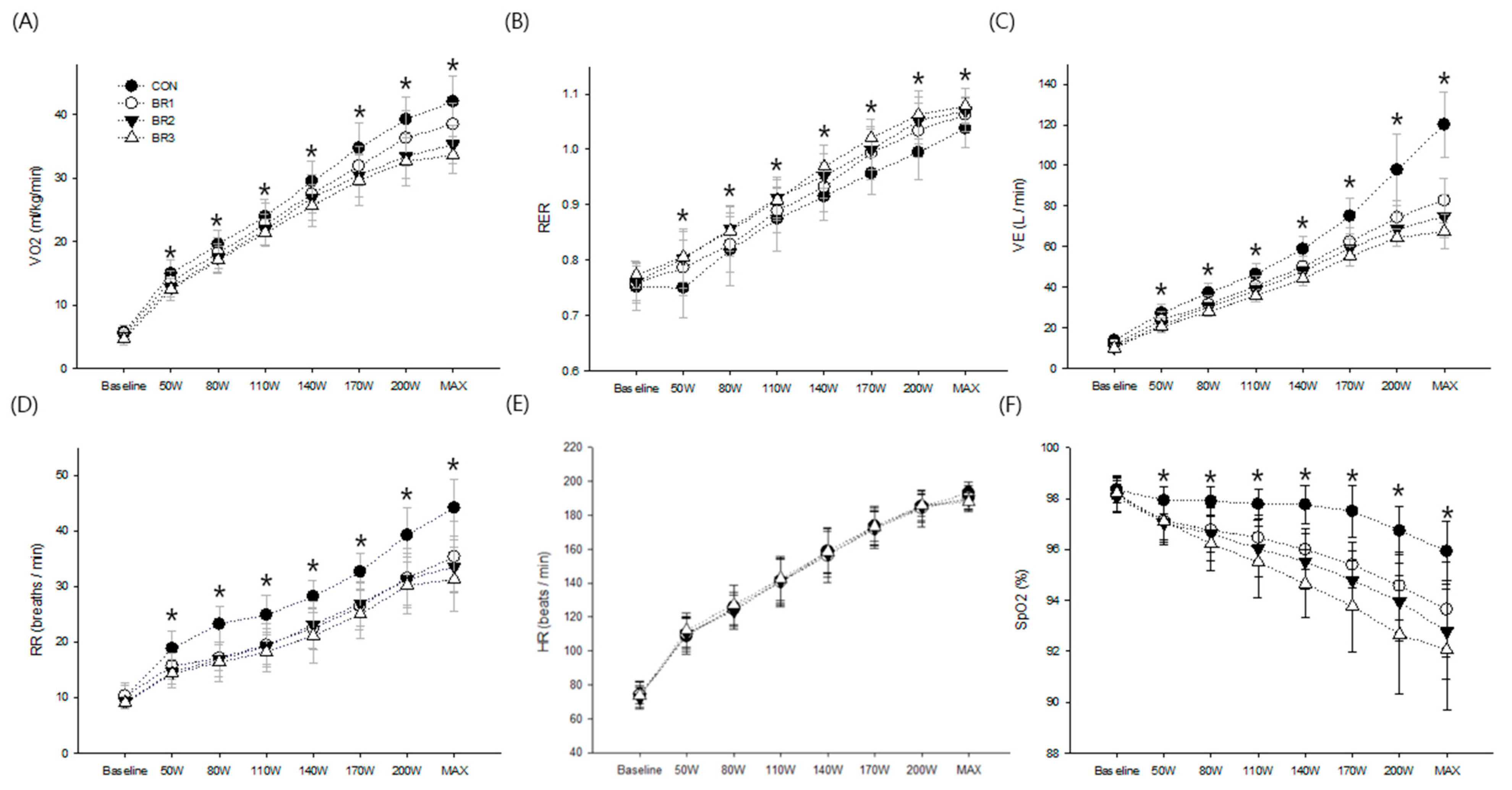
3.3. Cardiopulmonary Response
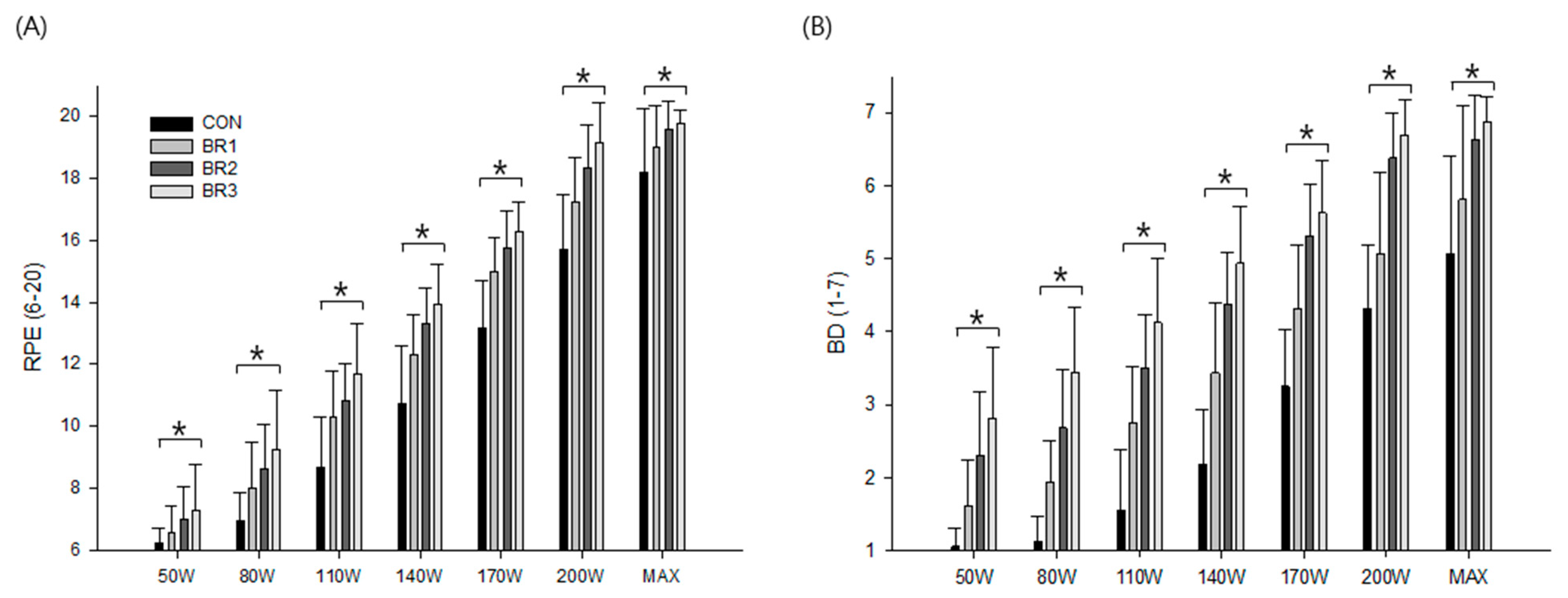
3.4. Subjective Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Considerations for Wearing Cloth Face Coverings. 2020. Available online: https://stacks.cdc.gov/view/cdc/90553 (accessed on 28 June 2020).
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological impact of the N95 filtering facepiece respirator on health-care workers. Respir. Care 2010, 55, 569–577. [Google Scholar] [PubMed]
- Kim, J.-H.; Benson, S.M.; Roberge, R.J. Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am. J. Infect. Control. 2013, 41, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Wu, T.; Powell, J.B.; Roberge, R.J. Physiologic and fit factor profiles of N95 and P100 filtering facepiece respirators for use in hot, humid environments. Am. J. Infect. Control. 2016, 44, 194–198. [Google Scholar] [CrossRef]
- Roberge, R.J.; Kim, J.-H.; Benson, S.M. Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir. Physiol. Neurobiol. 2012, 181, 29–35. [Google Scholar] [CrossRef]
- Shein, S.; Whitticar, S.; Mascho, K.K.; Pace, E.; Speicher, R.; Deakins, K. The effects of wearing facemasks on oxygenation and ventilation at rest and during physical activity. PLoS ONE 2021, 16, e0247414. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Byun, J.; Choi, J.-O.; Shim, D.; Rha, D.-W. The effects of wearing facemasks during vigorous exercise in the aspect of cardiopulmonary response, in-mask environment and subject discomfort. Int. J. Environ. Res. Public Health 2022, 19, 14106. [Google Scholar] [CrossRef] [PubMed]
- Dalakoti, M.; Long, C.; Bains, A.; Djohan, A.; Ahmad, I.; Chan, S.P.; Kua, J.; Chan, P.F.; Yeo, T.J. Effect of surgical mask use on peak physical performance during exercise treadmill testing—A real world, crossover study. Front. Physiol. 2022, 13, 913974. [Google Scholar] [CrossRef]
- Driver, S.; Reynolds, M.; Brown, K.; Vingren, J.L.; Hill, D.W.; Bennett, M.; Gilliland, T.; McShan, E.; Callender, L.; Reynolds, E.; et al. Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test. Br. J. Sports Med. 2022, 56, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020, 109, 1522–1530. [Google Scholar] [CrossRef]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scand. J. Med. Sci. Sports 2021, 31, 70–75. [Google Scholar] [CrossRef]
- Shaw, K.; Zello, G.A.; Butcher, S.J.; Ko, J.B.; Bertrand, L.; Chilibeck, P.D. The impact of face masks on performance and physiological outcomes during exercise: A systematic review and meta-analysis. Appl. Physiol. Nutr. Metab. 2021, 46, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Roberge, R.J.; Powell, J.B.; Shaffer, R.E.; Ylitalo, C.M.; Sebastian, J.M. Pressure drop of filtering facepiece respirators: How low should we go? Int. J. Occup. Med. Environ. Health 2015, 28, 71–80. [Google Scholar] [CrossRef]
- Roberge, R.J.; Kim, J.-H.; Coca, A. Protective facemask impact on human thermoregulation: An overview. Ann. Occup. Hyg. 2012, 56, 102–112. [Google Scholar] [PubMed]
- EN 149:2001; Respiratory Protective Devices—Filtering Half Masks to Protect against Particles—Requirements, Testing, Making. British Standards Institution (BSI): London, UK, 2001.
- Seo, Y.; Vaughan, J.; Quinn, T.D.; Followay, B.; Roberge, R.; Glickman, E.L.; Kim, J.-H. The effect of inspiratory resistance on exercise performance and perception in moderate normobaric hypoxia. High Alt. Med. Biol. 2017, 18, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Roberge, R.J.; Kim, J.-H.; Powell, J.B.; Shaffer, R.E.; Ylitalo, C.M.; Sebastian, J.M. Impact of low filter resistances on subjective and physiological responses to filtering facepiece respirators. PLoS ONE 2013, 8, e84901. [Google Scholar] [CrossRef] [PubMed]
- Caretti, D.; Coyne, K.; Johnson, A.; Scott, W.; Koh, F. Performance when breathing through different respirator inhalation and exhalation resistances during hard work. J. Occup. Environ. Hyg. 2006, 3, 214–224. [Google Scholar] [CrossRef]
- Johnson, A.T.; Scott, W.H.; Lausted, C.G.; Benjamin, M.B.; Coyne, K.M.; Sahota, M.S.; Johnson, M.M. Effect of respirator inspiratory resistance level on constant load treadmill work performance. Am. Ind. Hyg. Assoc. J. 1999, 4, 474–479. [Google Scholar] [CrossRef]
- Melissant, C.F.; Lammers, J.W.; Demedts, M. Relationship between external resistances, lung function changes and maximal exercise capacity. Eur. Respir. J. 1998, 11, 1369–1375. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Wagner, P.D.; Buchan, T.A.; Wright, S.P.; Esfandiari, S.; Fuchs, F.C.; Gray, T.; Currie, K.D.; Sasson, S.; Sasson, Z.; et al. Exercise-induced arterial hypoxemia. J. Appl. Physiol. 1999, 87, 1997–2006. [Google Scholar] [CrossRef]
- Hopkins, S.R. Exercise induced arterial hypoxemia: The role of ventilation-perfusion inequality and pulmonary diffusion limitation. Adv. Exp. Med. Biol. 2006, 588, 17–30. [Google Scholar]
- Guenette, J.A.; Sheel, A.W. Physiological consequences of a high work of breathing during heavy exercise in humans. J. Sci. Med. Sport 2007, 10, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Dominelli, P.B.; Foster, G.E.; Dominelli, G.S.; Henderson, W.R.; Koehle, M.S.; McKenzie, D.C.; Sheel, A.W. Exercise-induced arterial hypoxemia and the mechanics of breathing in healthy young women. J. Appl. Physiol. 2013, 591, 3017–3034. [Google Scholar]
- Mapelli, M.; Salvioni, E.; De Martino, F.; Mattavelli, I.; Gugliandolo, P.; Vignati, C.; Farina, S.; Palermo, P.; Campodonico, J.; Maragna, R.; et al. “You can leave your mask on”: Effects on cardiopulmonary parameters of different airway protective masks at rest and during maximal exercise. Eur. Respir. J. 2021, 58, 2004473. [Google Scholar] [CrossRef]
- Harms, C.A.; Babcock, M.A.; McClaran, S.R.; Pegelow, D.F.; Nickele, G.A.; Nelson, W.B.; Dempsey, J.A. Respiratory muscle work compromises leg blood flow during maximal exercise. J. Appl. Physiol. 1997, 82, 1573–1583. [Google Scholar] [CrossRef] [PubMed]
- Harms, C.A.; Wetter, T.J.; McClaran, S.R.; Pegelow, D.F.; Nickele, G.A.; Nelson, W.B.; Hanson, P.; Dempsey, J.A. Effects of respiratory muscle work on cardiac output and its distribution during maximal exercise. J. Appl. Physiol. 1998, 85, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Code of Federal Register Title 42 Part 84. Respiratory Protective Devices. Final. Rules Not. 1995, 60, 30335–30398.
| Variable | Mean ± SD |
|---|---|
| Age (yrs) | 22.3 ± 3.1 |
| Height (cm) | 176.4 ± 4.8 |
| Weight (kg) | 75.3 ± 8.3 |
| Systolic blood pressure (mm Hg) | 120.1 ± 5.0 |
| Diastolic blood pressure (mm Hg) | 71.5 ± 5.1 |
| Forced vital capacity (FVC; L) | 5.3 ± 0.6 |
| Forced expiratory volume in one second (FEV1; L) | 4.3 ± 0.1 |
| FEV1/FVC (%) | 0.8 ± 0.1 |
| Maximal voluntary ventilation (L) | 175.9 ± 21.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, J.-H.; Jang, M.-H.; Kim, D.-H.; Kim, J.-H. Added Breathing Resistance during Exercise Impairs Pulmonary Ventilation and Exaggerates Exercise-Induced Hypoxemia Leading to Impaired Aerobic Exercise Performance. Int. J. Environ. Res. Public Health 2023, 20, 5757. https://doi.org/10.3390/ijerph20105757
Han J-H, Jang M-H, Kim D-H, Kim J-H. Added Breathing Resistance during Exercise Impairs Pulmonary Ventilation and Exaggerates Exercise-Induced Hypoxemia Leading to Impaired Aerobic Exercise Performance. International Journal of Environmental Research and Public Health. 2023; 20(10):5757. https://doi.org/10.3390/ijerph20105757
Chicago/Turabian StyleHan, Jean-Hee, Min-Hyeok Jang, Dae-Hwan Kim, and Jung-Hyun Kim. 2023. "Added Breathing Resistance during Exercise Impairs Pulmonary Ventilation and Exaggerates Exercise-Induced Hypoxemia Leading to Impaired Aerobic Exercise Performance" International Journal of Environmental Research and Public Health 20, no. 10: 5757. https://doi.org/10.3390/ijerph20105757
APA StyleHan, J.-H., Jang, M.-H., Kim, D.-H., & Kim, J.-H. (2023). Added Breathing Resistance during Exercise Impairs Pulmonary Ventilation and Exaggerates Exercise-Induced Hypoxemia Leading to Impaired Aerobic Exercise Performance. International Journal of Environmental Research and Public Health, 20(10), 5757. https://doi.org/10.3390/ijerph20105757






