Strategies for the Psychological Support of the Healthcare Workforce during the COVID-19 Pandemic: The ERNST Study
Abstract
:1. Introduction
2. Materials and Methods
Data Analysis
3. Results
4. Discussion
4.1. Strengths and Study Limitations
4.2. Implications for Policy, Practice, and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
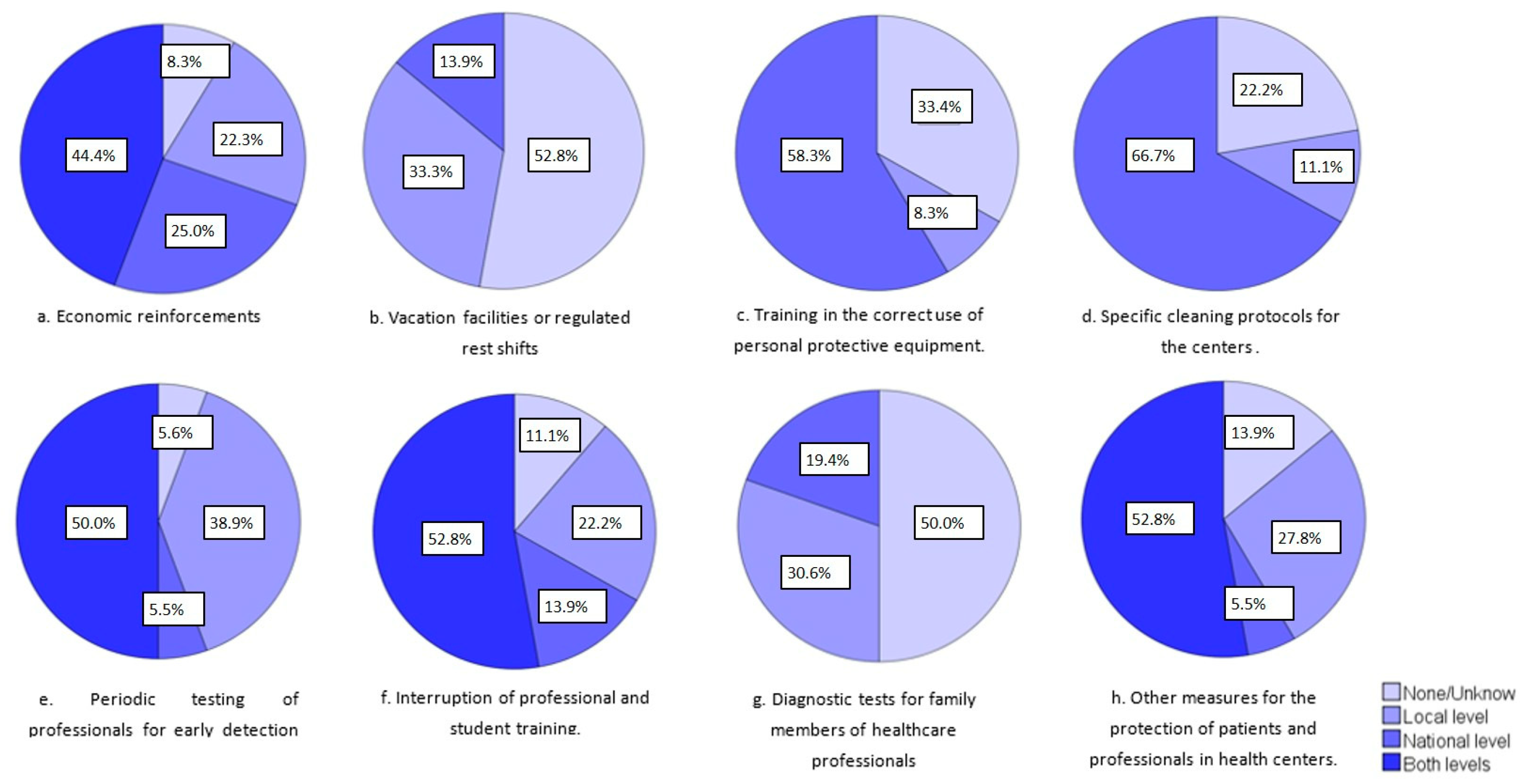
- Initiatives to improve working conditions:
- Economic reinforcements, such as payments and salary increases.
- Vacation facilities or regulated rest shifts.
- Training in the correct use of personal protective equipment.
- Specific cleaning protocols for the centers.
- Periodic testing of professionals for the early detection of infection.
- Interruption of professional and student training.
- Diagnostic tests for the family members of healthcare professionals.
- Other measures for the protection of patients and professionals in health centers (for example, triage and change of mask for everyone who enters the center).
- Hotels for healthcare professionals (or other accommodation options to avoid the risk of contagion to family members and loved ones).
- Modification of leave and vacation dates.
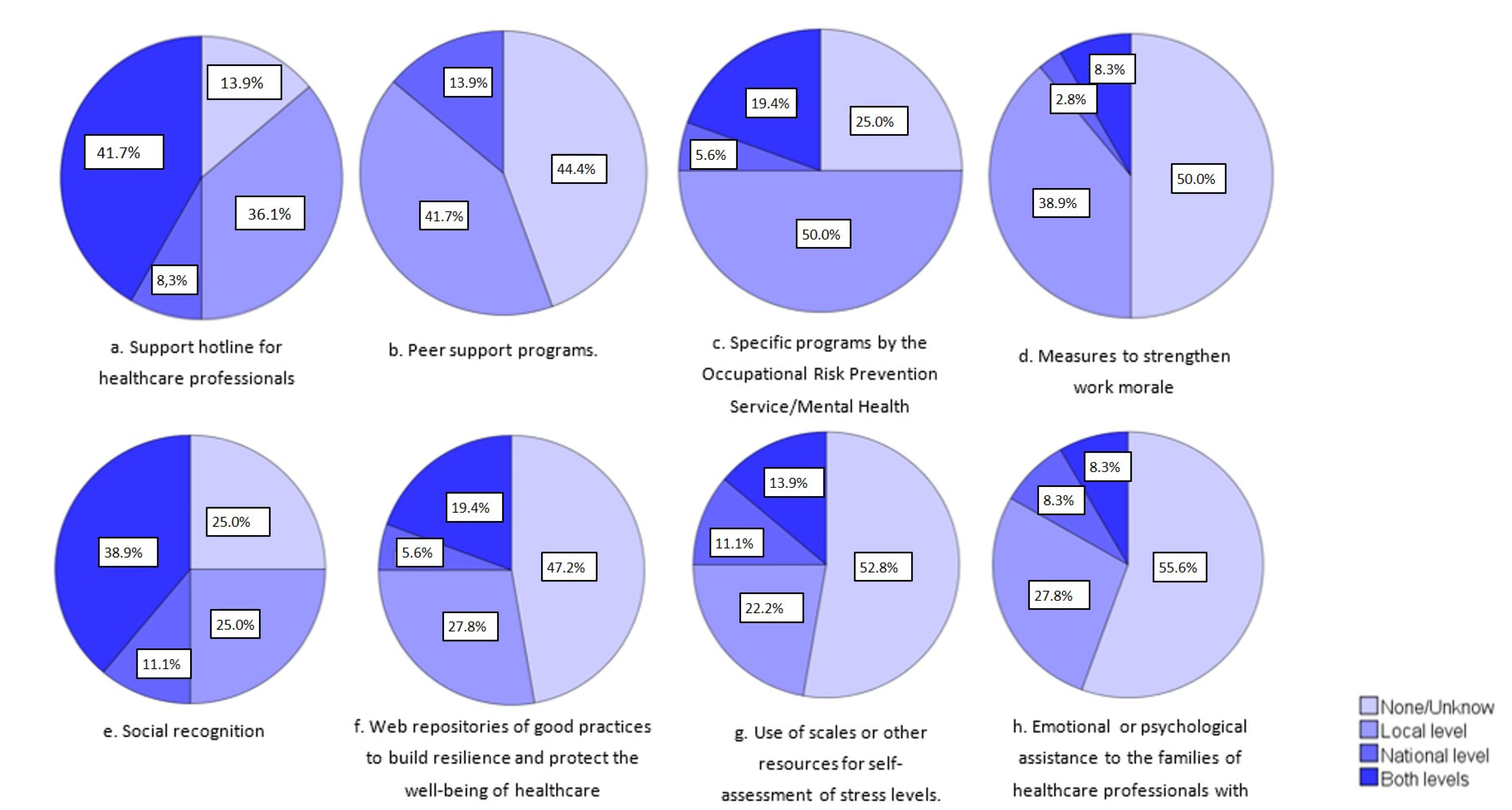
- Initiatives for psycho-emotional reinforcement and support:
- Support hotline for healthcare professionals.
- Peer support programs.
- Specific programs developed by the Occupational Risk Prevention Service/Mental Health Service/Employee Assistance.
- Measures to strengthen work morale.
- Social recognition.
- Web repositories of good practices to build resilience and protect the well-being of healthcare professionals.
- Use of scales or other resources for the self-assessment of stress levels.
- Emotional or psychological assistance to the families of healthcare professionals with COVID-19.
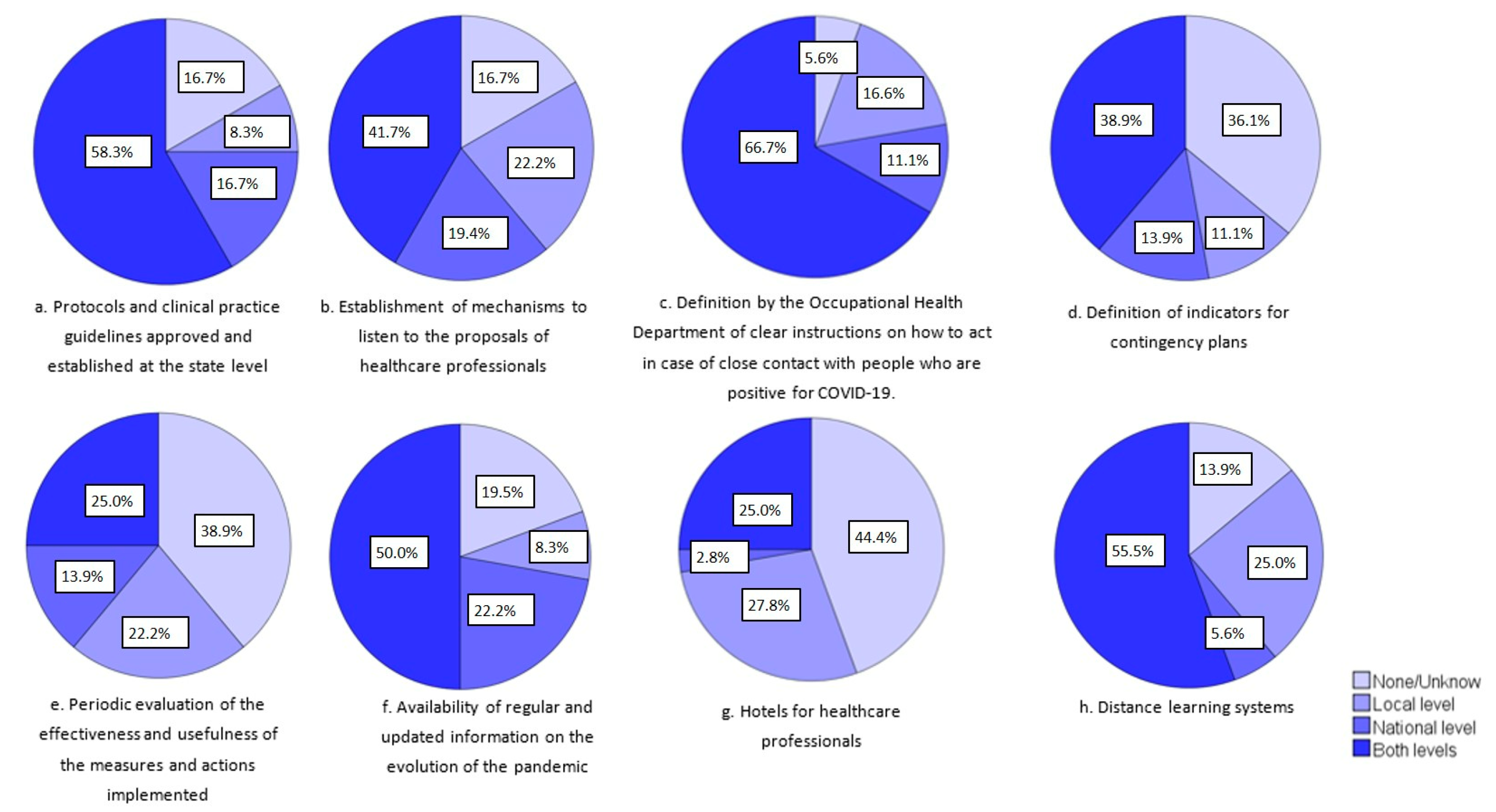
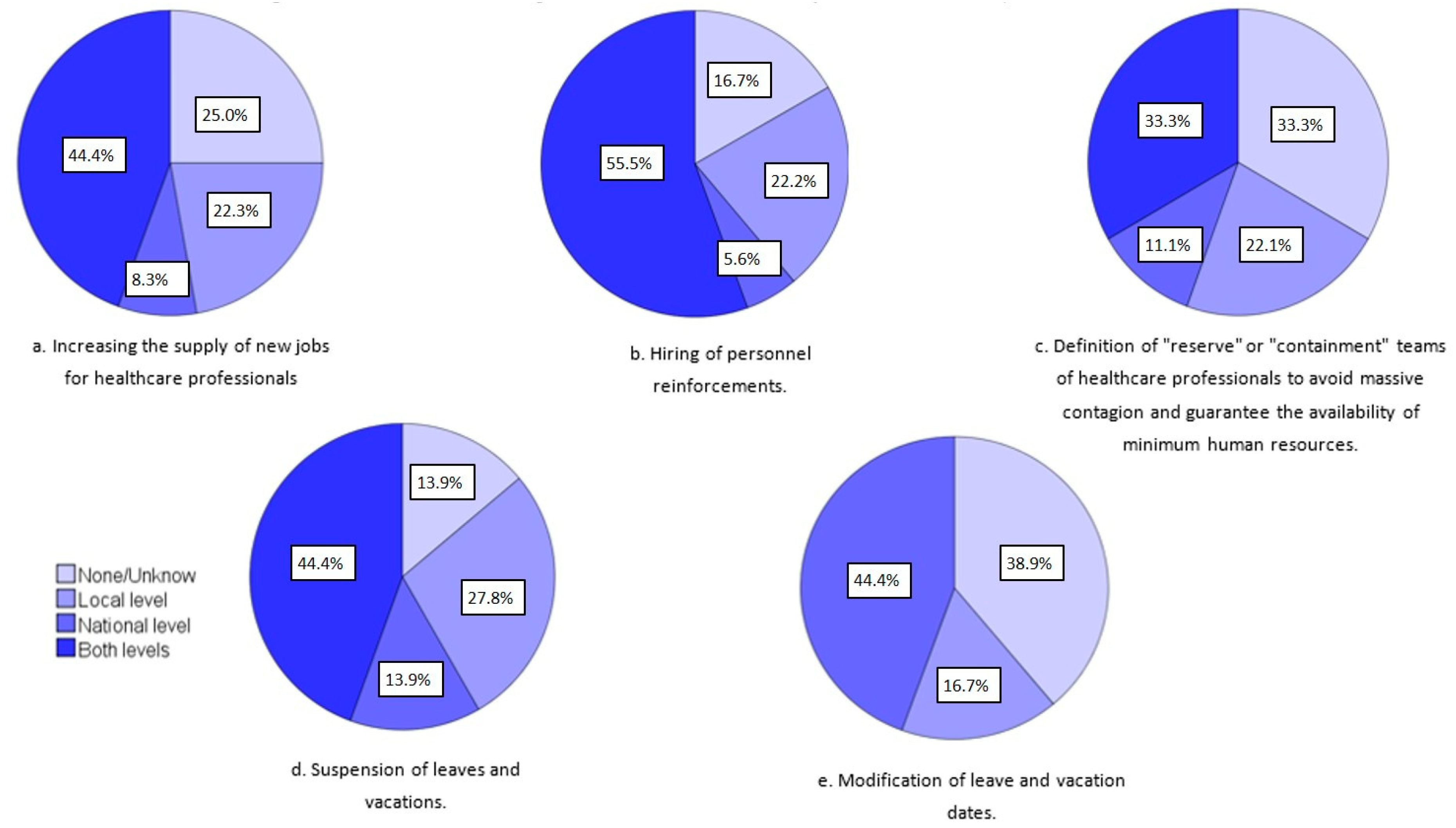
- Initiatives to strengthen staff, teams, and the organization:
- Increasing the supply of new jobs for healthcare professionals.
- Hiring of personnel reinforcements.
- Definition of “reserve” or “containment” teams of healthcare professionals to avoid massive contagion and guarantee the availability of minimum human resources.
- Suspension of leaves and vacations.
- Modification of leave and vacation dates.
- Protocols and clinical practice guidelines approved and established at the state level by the Ministry of Health and other national entities (shared action criteria among regions and health institutions in the country).
- Establishment of mechanisms to listen to the proposals of healthcare professionals (e.g., working groups with professional associations, trade unions, and scientific societies).
- Definition and establishment by the Occupational Health Department of clear instructions on how to act in case of close contact with people who are positive for COVID-19, hospitalization, and discharge of COVID-19 patients.
- Definition of the indicators for the contingency plans.
- Periodic evaluation of the effectiveness and usefulness of the measures and actions implemented.
- Availability of regular and updated information on the evolution of the pandemic at national, regional, and local levels to healthcare professionals (including data on infected and deceased healthcare professionals).
- Distance learning systems (e.g., healthcare professionals in home isolation who advise and train new personnel, training in the use of personal protective equipment, and new protocols and practices)
References
- Johns Hopkins University & Medicine. Coronavirus Resource Center. 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 25 June 2021).
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef] [PubMed]
- Erdem, H.; Lucey, D.R. Healthcare worker infections and deaths due to COVID-19: A survey from 37 nations and a call for WHO to post national data on their website. Int. J. Infect. Dis. 2021, 102, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Danet, A.D. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clin. 2021, 156, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Mira, J.J.; Vicente, M.A.; Lopez-Pineda, A.; Carrillo, I.; Guilabert, M.; Fernández, C.; Pérez-Jover, V.; Delgado, J.M.; Pérez-Pérez, P.; Vargas, A.C.; et al. Preventing and Addressing the Stress Reactions of Health Care Workers Caring for Patients With COVID-19: Development of a Digital Platform (Be + Against COVID). JMIR Mhealth Uhealth 2020, 8, e21692. [Google Scholar] [CrossRef] [PubMed]
- Vanhaecht, K.; Seys, D.; Bruyneel, L.; Cox, B.; Kaesemans, G.; Cloet, M.; Broeck, K.V.D.; Cools, O.; De Witte, A.; Lowet, K.; et al. COVID-19 is having a destructive impact on health-care workers' mental well-being. Int. J. Qual. Health Care 2021, 33, mzaa158. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Sinsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwappach, D.L.; Boluarte, T.A. The emotional impact of medical error involvement on physicians: A call for leadership and organisational accountability. Swiss Med. Wkly. 2009, 139, 9–15. [Google Scholar]
- Wu, A.W.; Connors, C.; Everly, G.S., Jr. COVID-19: Peer Support and Crisis Communication Strategies to Promote Institutional Resilience. Ann. Intern. Med. 2020, 172, 822–823. [Google Scholar] [CrossRef] [Green Version]
- Sagan, A.; Webb, E.; Azzopardi-Muscat, N.; de la Mata, I.; McKee, M.; Figueras, J. (Eds.) Health Systems Resilience during COVID-19: Lessons for Building Back Better; WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2021; Available online: https://tinyurl.com/27na68u2 (accessed on 3 January 2022).
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef]
- The European Researchers’ Network Working on Second Victims (ERNST—COST Action CA19113). Available online: https://cost-ernst.eu/ (accessed on 25 June 2021).
- Producto Interior Bruto. Available online: https://datosmacro.expansion.com/pib (accessed on 5 March 2021).
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Informe Epidemiológico. Características del Personal de Salud Confirmados y Probables de COVID-19. Chile. 12 de January 2020. Available online: https://www.minsal.cl/wp-content/uploads/2021/02/2021-01-21_Informe-PS-COVID-19.pdf (accessed on 25 June 2021).
- Newsletter of the Croatian Medical Chamber Liječničke novine. Croat. Med. Chamb. 2021, 197, 18–19.
- Statens Serum Institut News. 11 April 2020. Available online: https://www.ssi.dk/aktuelt/nyheder/2020/sundhedspersoner-udgor-mere-end-en-femtedel-af-de-coronavirus-smittede (accessed on 25 June 2021).
- Santé Publique France. Études et Enquêtes. 12 May 2021. Available online: https://www.santepubliquefrance.fr/etudes-et-enquetes/recensement-national-des-cas-de-COVID-19-chez-les-professionnels-en-etablissements-de-sante (accessed on 25 June 2021).
- Ministerio de Sanidad; Gobierno de España. Información Coronavirus. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_316_COVID-19.pdf (accessed on 25 June 2021).
- Organización Médica Colegial de España. Consejo General de Colegios Oficiales de Médicos. 18 March 2021. Available online: https://www.cgcom.es/sites/default/files/u183/np_112_victimas_profesion_de_riesgo_18_03_21.pdf (accessed on 5 July 2021).
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Blake, H.; Gupta, A.; Javed, M.; Wood, B.; Knowles, S.; Coyne, E.; Cooper, J. COVID-Well Study: Qualitative Evaluation of Supported Wellbeing Centres and Psychological First Aid for Healthcare Workers during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3626. [Google Scholar] [CrossRef]
- Zaçe, D.; Hoxhaj, I.; Orfino, A.; Viteritti, A.M.; Janiri, L.; Di Pietro, M.L. Interventions to address mental health issues in healthcare workers during infectious disease outbreaks: A systematic review. J. Psychiatr. Res. 2021, 136, 319–333. [Google Scholar] [CrossRef]
- Tartaglia, R.; La Regina, M.; Tanzini, M.; Pomare, C.; Urwin, R.; Ellis, L.A.; Fineschi, V.; Venneri, F.; Seghieri, C.; Lachman, P.; et al. International survey of COVID-19 management strategies. Int. J. Qual. Health Care 2021, 33, mzaa139. [Google Scholar] [CrossRef]
- Busch, I.; Moretti, F.; Campagna, I.; Benoni, R.; Tardivo, S.; Wu, A.W.; Rimondini, M. Promoting the Psychological Well-Being of Healthcare Providers Facing the Burden of Adverse Events: A Systematic Review of Second Victim Support Resources. Int. J. Environ. Res. Public Health 2021, 18, 5080. [Google Scholar] [CrossRef]
- Matisāne, L.; Paegle, L.; Eglīte, M.; Akūlova, L.; Linde, A.A.; Vanadziņš, I.; Mietule, I.; Lonska, J.; Litavniece, L.; Arbidāne, I.; et al. Reasons for Low Protection of Vulnerable Workers from COVID-19—Results from the Quantitative and Qualitative Study on Working Life in Latvia. Int. J. Environ. Res. Public Health 2021, 18, 5188. [Google Scholar] [CrossRef]
- Jarosz, J. The impact of coaching on well-being and performance of managers and their teams during pandemic. Int. J. Evid. Based Coach. Mentor. 2021, 19, 4–27. [Google Scholar]
- Riera, R.; Bagattini, .M.; Pacheco, R.L.; Pachito, D.V.; Roitberg, F.; Ilbawi, A. Delays and Disruptions in Cancer Health Care Due to COVID-19 Pandemic: Systematic Review. JCO Glob. Oncol. 2021, 7, 311–323. [Google Scholar] [CrossRef]
- Abejón, D.; Monzón, E.M.; Deer, T.; Hagedorn, J.M.; Araujo, R.; Abad, C.; Rios, A.; Zamora, A.; Vallejo, R. How to Restart the Interventional Activity in the COVID-19 Era: The Experience of a Private Pain Unit in Spain. Pain Pract. 2020, 20, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Spilg, E.G.; Rushton, C.H.; Phillips, J.L.; Kendzerska, T.; Saad, M.; Gifford, W.; Gautam, M.; Bhatla, R.; Edwards, J.D.; Quilty, L.; et al. The new frontline: Exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2022, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Heath, C.; Sommerfield, A.; Von Ungern-Sternberg, B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; De Gagne, J.C. The impact of resilience on turnover among newly graduated nurses: A 1-year follow-up study. J. Nurs. Manag. 2022. [Google Scholar] [CrossRef]
| Sociodemographic Variables | |
|---|---|
| Sex (n, %) | |
| Female | 36 (64.3%) |
| Male | 20 (35.7%) |
| Age (mean, [min–max]) | 47.0 [24–68] |
| Professional profile (n, %) | |
| Nurse 1 | 5 (8.9%) |
| Physician 1 | 18 (32.1%) |
| Psychologist 1 | 2 (3.6%) |
| Other healthcare professionals | 1 (1.8%) |
| Researchers on public health or related disciplines | 13 (23.2%) |
| Professor in the health area | 15 (26.8%) |
| Other legal, social, or technical profession | 2 (3.6%) |
| Type of work organization (n, %) | |
| Healthcare organization | 21 (37.5%) |
| Higher education and associated organizations | 27 (48.2%) |
| Government/intergovernmental organizations except higher education and healthcare organization | 3 (5.4%) |
| Private non-profit without market revenues, NGO | 2 (3.6%) |
| Country | Number of HCWs Infected with COVID-19 | Number of HCWs who Died from COVID-19 | Date of Data Obtainment | Data Source |
|---|---|---|---|---|
| Argentina 1 | 79,806 | 472 | March 2021 | Ministerio de Sanidad de Argentina |
| Azerbaijan 2 | No data | 45 | July–August 2020 | Erdem and Lucey [3] |
| Belgium 3 | No data | No data | ||
| Bosnia and Herzegovina 3 | 2019 | 8 | April 2021 | Provided by the collaborator |
| Brazil 1 | 48,234 nurses | 556 nurses | February 2021 | Provided by the collaborator |
| Bulgaria 3 | 12670 | No data | April 2021 | Provided by the collaborator |
| Chile 1 | 52,241 | 102 | January 2021 | Epidemiological report from the Ministry of Health [15] |
| Colombia 1 | 3655 | 31 | July–August 2020 | Erdem and Lucey [3] |
| Croatia 3 | 2551 physicians | 2 physicians | February 2021 | Croatian Medical Chamber [16] |
| Czech Republic 3 | 1119 | 2 | July–August 2020 | Erdem and Lucey [3] |
| Denmark 3 | 2380 | 15 | March 2021 | Statens Serum Institut [17] |
| Ecuador 1 | No data | No data | ||
| Estonia 3 | No data | No data | ||
| Finland 3 | 2000 | No data | January 2021 | Provided by the collaborator |
| France 3 | 81,032 | 16 | May 2021 | French public health [18] |
| Germany 3 | 104,387 | 148 | March 2021 | Provided by the collaborator |
| Ireland 3 | 16,381 | 9 | April 2021 | Provided by the collaborator |
| Israel 4 | No data | No data | ||
| Italy 3 | 138,129 | 333 | July 2021 | Ministry of Health from Italy |
| Japan 1 | No data | No data | ||
| Lithuania 3 | No data | No data | ||
| Malta 3 | No data | No data | ||
| Mexico 1 | No data | No data | ||
| Netherlands 3 | No data | No data | ||
| Peru 1 | 13,073 physicians a + 7780 nurses b | 400 physicians a + 90 nurses b | a March 2021 b January 2021 | Provided by the collaborator |
| Poland 3 | 91,949 | 187 | February 2021 | Provided by the collaborator |
| Portugal 3 | 3681 | 1 | July–August 2020 | Erdem and Lucey [3] |
| Romania 3 | 20,504 | 94 | Provided by the collaborator | |
| Serbia 3 | No data | No data | ||
| Slovakia 3 | No data | 40 | September 2021 | Institute of Health Analysis (Ministry of Health) |
| Spain 3 | 128,590 c | 112 d | c February 2021 d March 2021 | c Ministerio de Sanidad de España [19] d Consejo General de Colegios Oficiales de Médicos [20] |
| Sweden 3 | No data | No data | ||
| Switzerland 3 | No data | No data | ||
| Turkey 3 | >120,000 | 383 | January 2021 | Provided by the collaborator |
| United States 1 | 114,529 | 574 | July–August 2020 | Erdem and Lucey [3] |
| Country | Initiatives at National Level | Incidence (per 100,000 Inhabitants) | Lethality (%) | Mortality (per 100,000 Inhabitants) | Per Capita Income (EUR ) |
|---|---|---|---|---|---|
| Argentina | Emotional support with online inquiries and helpline by a net of psychologists (Argentine Society of Intensive Care, only to their partners). | 6589.6 | 2.1 | 140.9 | EUR 7463 |
| Azerbaijan | Support hotline for healthcare workers, peer support programs, measures to strengthen work morale, social recognition, and self-assessment of stress level. | 3143.6 | 1.4 | 44.6 | EUR 4263 |
| Belgium | Website, webinars, and research (example: www.dezorgsamen.be, accessed on 15 September 2021) | 8558.6 | 2.4 | 208.8 | EUR 39,110 |
| Bosnia and Herzegovina | Support hotline for healthcare workers. | 6081.3 | 4.3 | 262.0 | EUR 5266 |
| Brazil | No support interventions, but there is social recognition. | 6895.0 | 2.8 | 190.5 | EUR 6013 |
| Bulgaria | No. | 5875.2 | 4.1 | 239.1 | EUR 8750 |
| Chile | No support interventions, but there is social recognition. | 6302.8 | 2.2 | 138.2 | EUR 11,582 |
| Colombia | Recommendations. | 5644.4 | 2.6 | 145.3 | EUR 4718 |
| Croatia | For the prevention of “burn-out syndrome”: 24 h hotline for psychological help for healthcare workers (Croatian Institute for Public Health). | 8220.2 | 2.2 | 176.8 | EUR 12,170 |
| Czech Republic | Healthcare insurance company partially covers psychotherapy. | 15,241.8 | 1.8 | 273.8 | EUR 19,970 |
| Denmark | No. | 3693.4 | 1.1 | 41.0 | EUR 53,470 |
| Ecuador | No. | 2165.1 | 4.8 | 104.8 | EUR 5592 |
| Estonia | No support interventions, but there is social recognition and the use of scales and other resources for the self-assessment of stress levels. | 5438.5 | 0.9 | 48.0 | EUR 20,440 |
| Finland | Support hotline for healthcare workers. | 1574.2 | 1.0 | 16.5 | EUR 42,940 |
| France | National hotline for psychological support (regional medico-psychological emergency unit). | 8732.6 | 1.8 | 160.5 | EUR 34,040 |
| Germany | No. | 4094.4 | 2.4 | 99.3 | EUR 40,120 |
| Ireland | Psychological support via professional organizations. | 5013.9 | 2.0 | 98.5 | EUR 73,590 |
| Israel | A 24 h hotline for support by psychologists and social workers (Ministry of Health). | 8799.7 | 0.7 | 64.5 | EUR 38,942 |
| Italy | INAIL (National Institute of Workers’ Compensation—Insurance) with the psychologist council activated on a 24 h support telephone line. Taskforce for developing guidelines for the local implementation of psychological support from the HCW webpage. | 6700.2 | 3.0 | 201.2 | EUR 27,780 |
| Japan | Telephone-based consultation initiative for nurses on the frontlines (Japan Nurses’ Association). | 339.1 | 1.9 | 6.4 | EUR 35,059 |
| Lithuania | Psychologist consultation for healthcare workers (Ministry of Health). | 9306.7 | 1.6 | 147.1 | EUR 17,510 |
| Malta | Psychology Department Mater Dei Hospital website in Facebook. | 4535.6 | 1.4 | 62.3 | EUR 25,310 |
| Mexico | (1) Government initiatives: Webpage with some support resources, including mindfulness audio, some videos, a list of emotional support initiatives, and a mental-health-risks questionnaire. (2) University initiatives: Community-exclusive call centers and a telepsychiatry clinic. (3) Civil societies: Telepsychiatry for health professionals, and a list of emotional support networks | 1803.2 | 9.2 | 166.8 | EUR 7379 |
| Netherlands | Websites for information consultation. For example, the Trimbos Institute. Impact Kenniscentrum. | 8987.6 | 1.1 | 101.6 | EUR 45,870 |
| Peru | Phone number by the government for support. Webinars for health workers by psychologists and psychiatrists. Friend call for psychological support. Rapid-response teams. Psychosocial support. | 5428.7 | 3.4 | 186.2 | EUR 5488 |
| Poland | No support interventions, but there is social recognition. | 7423.2 | 2.4 | 180.2 | EUR 13,600 |
| Portugal | Psychological counseling from the national health service to support the psychological concerns and challenges of patients and health professionals (who are providing health care). | 8236.3 | 2.0 | 167.0 | EUR 19,660 |
| Romania | No. | 5533.0 | 2.7 | 148.4 | EUR 11,290 |
| Serbia | No support interventions, but there is social recognition. | 7969.7 | 0.9 | 74.0 | EUR 6710 |
| Slovakia | Psycho-social support teams during the 1st pandemic wave (Ministry of Health). Online application to monitor the stages of depression and anxiety via a questionnaire and to provide recommendations. | 7017.9 | 3.1 | 216.2 | EUR 16,770 |
| Spain | Telephone support from the Ministry of Health. | 7538.9 | 2.2 | 167.3 | EUR 23,690 |
| Sweden | No. | 9582.6 | 1.4 | 138.3 | EUR 45,850 |
| Switzerland | No. | 7618.1 | 1.6 | 122.2 | EUR 75,890 |
| Turkey | RUHSAD (mental health support system) app to offer psychosocial counseling (over the telephone or online systems) and mental health support services. | 5732.9 | 0.8 | 48.0 | EUR 7520 |
| United States | Web repositories of good practices to build resilience and protect the well-being of healthcare professionals, and the use of scales or other resources for the self-assessment of stress levels. | 9739.4 | 1.8 | 173.3 | EUR 55,806 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Pineda, A.; Carrillo, I.; Mula, A.; Guerra-Paiva, S.; Strametz, R.; Tella, S.; Vanhaecht, K.; Panella, M.; Knezevic, B.; Ungureanu, M.-I.; et al. Strategies for the Psychological Support of the Healthcare Workforce during the COVID-19 Pandemic: The ERNST Study. Int. J. Environ. Res. Public Health 2022, 19, 5529. https://doi.org/10.3390/ijerph19095529
López-Pineda A, Carrillo I, Mula A, Guerra-Paiva S, Strametz R, Tella S, Vanhaecht K, Panella M, Knezevic B, Ungureanu M-I, et al. Strategies for the Psychological Support of the Healthcare Workforce during the COVID-19 Pandemic: The ERNST Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5529. https://doi.org/10.3390/ijerph19095529
Chicago/Turabian StyleLópez-Pineda, Adriana, Irene Carrillo, Aurora Mula, Sofia Guerra-Paiva, Reinhard Strametz, Susanna Tella, Kris Vanhaecht, Massimiliano Panella, Bojana Knezevic, Marius-Ionut Ungureanu, and et al. 2022. "Strategies for the Psychological Support of the Healthcare Workforce during the COVID-19 Pandemic: The ERNST Study" International Journal of Environmental Research and Public Health 19, no. 9: 5529. https://doi.org/10.3390/ijerph19095529
APA StyleLópez-Pineda, A., Carrillo, I., Mula, A., Guerra-Paiva, S., Strametz, R., Tella, S., Vanhaecht, K., Panella, M., Knezevic, B., Ungureanu, M.-I., Srulovici, E., Buttigieg, S. C., Skoumalová, I., Sousa, P., Mira, J., & on behalf of the ERNST Consortium Collaborators. (2022). Strategies for the Psychological Support of the Healthcare Workforce during the COVID-19 Pandemic: The ERNST Study. International Journal of Environmental Research and Public Health, 19(9), 5529. https://doi.org/10.3390/ijerph19095529












