The Effects of Horticultural Therapy on Sense of Coherence among Residents of Long-Term Care Facilities: A Quasi Experimental Design
Abstract
1. Introduction
2. Materials and Methods
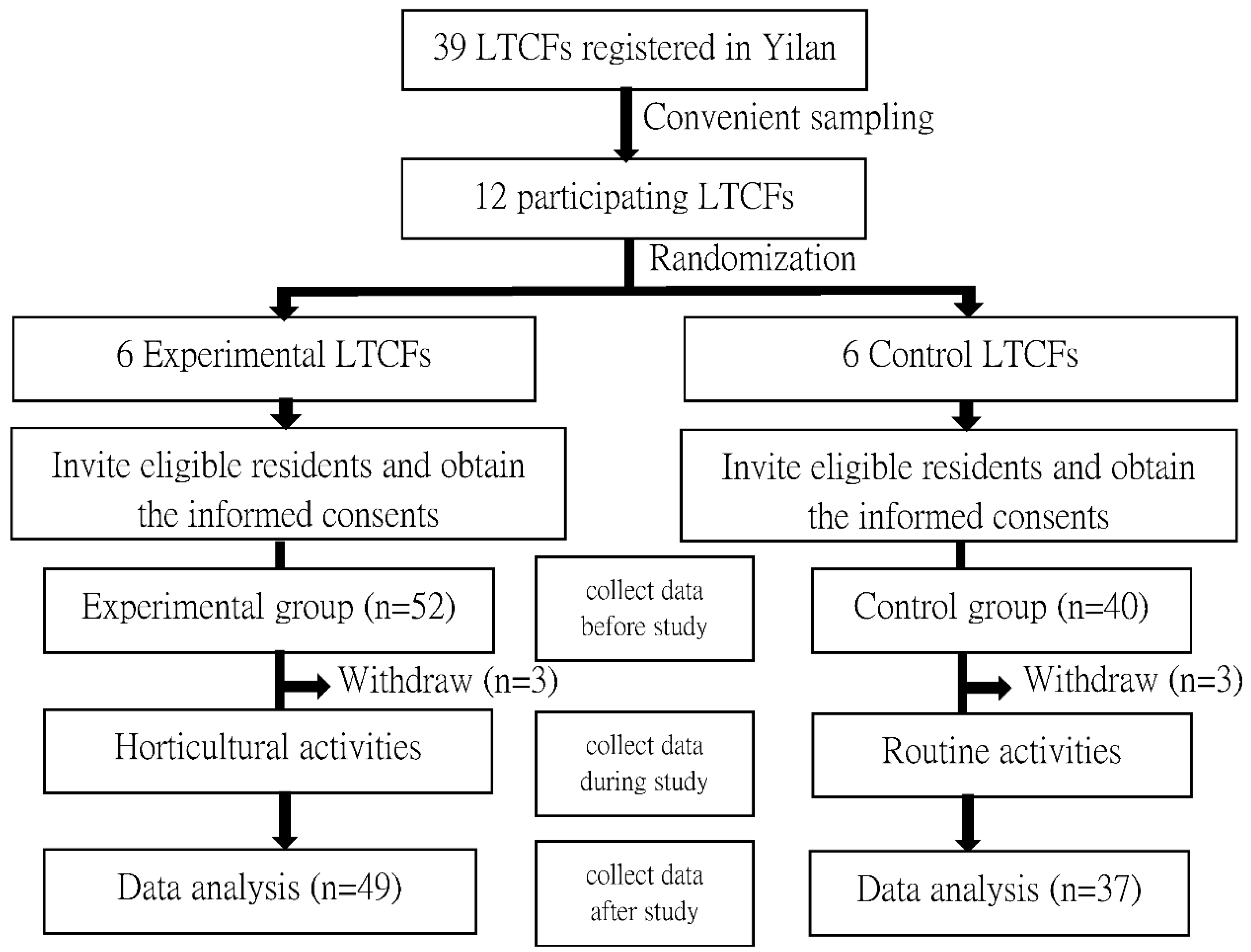
2.1. Study Design and Participants
2.2. Horticultural Activities Design Basis
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Baseline Data
3.2. The Change of SOC Scores before and after Intervention in the Experimental Group
3.3. Comparison of SOC Score between the Experimental and Control Groups
3.4. Difference of SOC Score Improvement between the Experimental and Control Groups at Various Time Points
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloom, D.E.; Chatterji, S.; Kowal, P.; Lloyd-Sherlock, P.; McKee, M.; Rechel, B.; Rosenberg, L.; Smith, J.P. Macroeconomic implications of population ageing and selected policy responses. Lancet 2014, 385, 649–657. [Google Scholar] [CrossRef]
- Freeman, S.; Bishop, K.; Spirgiene, L.; Koopmans, E.; Botelho, F.C.; Fyfe, T.; Xiong, B.; Patchett, S.; MacLeod, M. Factors af-fecting residents transition from long term care facilities to the community: A scoping review. BMC Health Serv. Res. 2017, 17, 689. [Google Scholar] [CrossRef]
- Dept. of Household Registration, Ministry of the Interior. Republic of China (Taiwan). Available online: https://www.ris.gov.tw/app/en/3910 (accessed on 10 April 2022).
- Hirdes, J.P. Addressing the health needs of frail elderly people: Ontario’s experience with an integrated health information system. Age Ageing 2006, 35, 329–331. [Google Scholar] [CrossRef]
- Levin, C.A.; Wei, W.; Akincigil, A.; Lucas, J.A.; Bilder, S.; Crystal, S. Prevalence and Treatment of Diagnosed Depression among Elderly Nursing Home Residents in Ohio. J. Am. Med. Dir. Assoc. 2007, 8, 585–594. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_1 (accessed on 10 April 2022).
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: San Francisco, CA, USA, 1987; Available online: https://psycnet.apa.org/record/1987-97506-000 (accessed on 10 April 2022).
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- Griffiths, C.A. Sense of coherence and mental health rehabilitation. Clin. Rehabil. 2009, 23, 72–78. [Google Scholar] [CrossRef]
- Saevareid, H.I.; Thygesen, E.; Nygaard, H.A.; Lindstrom, T.C. Does sense of coherence affect the relationship between self-rated health and health status in a sample of community-dwelling frail elderly people? Aging Ment. Health 2007, 11, 658–667. [Google Scholar] [CrossRef]
- Antonovsky, A. Health, Stress and Coping: New Perspectives on Mental and Physical Well-Being; Jossey-Bass: San Francisco, CA, USA, 1979. [Google Scholar]
- Jueng, R.-N.; Tsai, D.-C.; Chen, I.-J. Sense of Coherence among Older Adult Residents of Long-Term Care Facilities in Taiwan: A Cross-Sectional Analysis. PLoS ONE 2016, 11, e0146912. [Google Scholar] [CrossRef]
- Drageset, J.; Nygaard, H.A.; Eide, G.E.; Bondevik, M.; Nortvedt, M.W.; Natvig, G.K. Sense of coherence as a resource in rela-tion to health-related quality of life among mentally intact nursing home residents-a questionnaire study. Health Qual. Life Outcomes 2008, 21, 85. [Google Scholar] [CrossRef]
- Drageset, J.; Espehauga, B.; Hallbergc, I.R.; Natvigb, G.K. Sense of coherence among cognitively intact nursing home resi-dents–a five-year longitudinal study. Aging Ment. Health 2014, 18, 889–896. [Google Scholar] [CrossRef]
- Lawton, M.P.; Nahemow, L. Ecology and the aging process. In Psychology of Adult Development and Aging; Eisdorfer, C., Lawton, M.P., Eds.; American Psychological Association: Washington, DC, USA, 1973; pp. 619–674. [Google Scholar]
- Finnegan, S.; Bruce, J.; Lamb, S.; Griffiths, F. Predictors of attendance to group exercise: A cohort study of older adults in long-term care facilities. BMC Geriatr. 2015, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- American Horticultural Therapy Association. About Horticultural Therapy. 2022. Available online: https://www.ahta.org/about-horticultural-therapy (accessed on 10 April 2022).
- Zhao, Y.; Liu, Y.; Wang, Z. Effectiveness of horticultural therapy in people with dementia: A quantitative systematic review. J. Clin. Nurs. 2020. [Google Scholar] [CrossRef] [PubMed]
- Relf, P.D. The therapeutic values of plants. Pediatr. Rehabil. 2005, 8, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.M.; Chiu, P.Y. Meta-analysis of controlled trials testing horticultural therapy for the improvement of cognitive function. Sci. Rep. 2020, 10, 14637. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Lin, R.; Liu, W.; Wu, W. Effectiveness of horticultural therapy on physical functioning and psychological health outcomes for older adults: A systematic review and meta-analysis. J. Clin. Nurs. 2021; epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.Y.; Chan, H.S.; Chen, M.F. Effects of Horticultural Activities on Attitudes toward Aging, Sense of Hope and Hand-Eye Coordination in Older Adults in Residential Care Facilities. Int. J. Environ. Res. Public Health 2021, 18, 6555. [Google Scholar] [CrossRef]
- Super, S.; Wagemakers, A.; Picavet, H.S.J.; Verkooijen, K.T.; Koelen, M.A. Strengthening sense of coherence: Opportunities for theory building in health promotion. Health Promot. Int. 2015, 31, 869–878. [Google Scholar] [CrossRef]
- Mlinac, M.E.; Feng, M.C. Assessment of activities of daily living, self-care, and independence. Arch. Clin. Neuropsychol. 2016, 31, 506–516. [Google Scholar] [CrossRef]
- Hopkins, R.O.; Suchyta, M.R.; Kamdar, B.B.; Darowski, E.; Jackson, J.C.; Needham, D.M. Instrumental activities of daily liv-ing after critical illness: A systematic review. Ann. Am. Thorac. Soc. 2017, 14, 1332–1343. [Google Scholar] [CrossRef]
- Tsiakiri, A.; Vadikolias, K.; Tripsianis, G.; Vlotinou, P.; Serdari, A.; Terzoudi, A.; Heliopoulos, I. Influence of social and de-mographic factors on the montreal cognitive assessment (MoCA) test in rural population of north-eastern Greece. Geriatrics 2021, 6, 43. [Google Scholar] [CrossRef]
- Lach, H.W.; Chang, Y.P.; Edwards, D. Can older adults with dementia accurately report depression using brief forms? Reli-ability and validity of the Geriatric Depression Scale. J. Gerontol. Nurs. 2010, 36, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.T.; Dixon, J. Instrument translation and evaluation of equivalence and psychometric properties: The Chinese Sense of Coherence Scale. J. Nurs. Meas. 2002, 10, 59–76. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.K.; Kwan, R.Y.; Lo, S.K.; Fung, C.Y.; Lau, J.K.; Tse, M.M. Effects of Horticulture on Frail and Prefrail Nursing Home Residents: A Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2018, 19, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.-Y.; Chen, M.-F.; Tsai, C.-C.; Chan, H.-S.; Wu, T.-L. Efficacy of a horticultural activity program for reducing depression and loneliness in older residents of nursing homes in Taiwan. Geriatr. Nurs. 2019, 40, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Masuya, J.; Ota, K.; Mashida, Y. The Effect of a Horticultural Activities Program on the Psychologic, Physical, Cognitive Function and Quality of Life of Elderly People Living in Nursing Homes. Int. J. Nurs. Clin. Pract. 2014, 1, 109. [Google Scholar] [CrossRef]
- Chen, Y.M.; Ji, J.Y. Effects of Horticultural Therapy on Psychosocial Health in Older Nursing Home Residents: A Preliminary Study. J. Nurs. Res. 2015, 23, 167–171. [Google Scholar] [CrossRef]
- Park, S.A.; Lee, A.Y.; Son, K.C.; Lee, W.L.; Kim, D.S. Gardening intervention for physical and psychological health benefits in elder-ly women at community centers. HortTechnology 2016, 26, 474–483. [Google Scholar] [CrossRef]
- Detweiler, M.B.; Self, J.A.; Lane, S.; Spencer, L.; Lutgens, B.; Kim, D.-Y.; Halling, M.H.; Rudder, T.F.; Lehmann, L. Horticultural therapy: A pilot study on modulating cortisol levels and indices of substance craving, posttraumatic stress disorder, depression, and quality of life in veterans. Altern. Ther. Health Med. 2015, 21, 36–41. [Google Scholar]
- Hassan, A.; Chen, Q.; Liu, Y.; Jiang, T.; Guo, L.; Mingyan, J.; Li, N.; Lv, B.Y.; Liu, S. Do plants affect brainwaves? Effect of indoor plants in work environment on mental stress. Eur. J. Hortic. Sci. 2020, 85, 279–283. [Google Scholar] [CrossRef]
- Park, S.A.; Son, S.Y.; Lee, A.Y.; Park, H.G.; Lee, W.L.; Lee, C.H. Metabolite Profiling Revealed That a Gardening Activity Program Im-proves Cognitive Ability Correlated with BDNF Levels and Serotonin Metabolism in the Elderly. Int. J. Environ. Res. Public Health 2020, 17, 541. [Google Scholar]
- Gramaglia, C.; Gattoni, E.; Marangon, D.; Concina, D.; Grossini, E.; Rinaldi, C.; Panella, M.; Zeppegno, P. Non-pharmacological Ap-proaches to Depressed Elderly with No or Mild Cognitive Impairment in Long-Term Care Facilities. A Systematic Review of the Literature. Front. Public Health 2021, 16, 685860. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 86) | Experimental Group (n = 49) | Control Group (n = 37) | p Value |
|---|---|---|---|---|
| Gender, n (%) | 0.501 | |||
| Male | 31 (36.05) | 16 (34.04) | 15 (40.54) | |
| Female | 55 (63.95) | 33 (65.96) | 22 (59.46) | |
| Age, year, mean (SD) | 81.76 (8.47) | 82.22 (7.47) | 81.14 (9.72) | 0.573 |
| Marital Status, n (%) | 0.667 | |||
| Unmarried | 6 (6.97) | 2 (4.08) | 4 (10.81) | |
| Married | 18 (20.93) | 10 (20.08) | 8 (21.62) | |
| Divorced or widowed | 62 (72.10) | 37 (75.50) | 25 (67.57) | |
| Education level, n (%) | 0.297 | |||
| Illiterate | 43 (50.00) | 23 (46.93) | 20 (54.05) | |
| Elementary school | 29 (33.72) | 19 (38.77) | 10 (27.03) | |
| High school and above | 14 (16.28) | 7 (14.30) | 7 (18.92) | |
| Religion, n (%) | 0.143 | |||
| None | 13 (16.21) | 7 (15.11) | 6 (14.28) | |
| Yes | 73 (84.79) | 42 (84.90) | 31 (85.72) | |
| Multi-morbidity, n (%) | 0.101 | |||
| 1 chronic disease | 17 (19.76) | 13 (26.53) | 4 (10.81) | |
| ≥2 chronic diseases | 69 (80.24) | 36 (74.47) | 33 (89.19) | |
| Activities of Daily Living (ADLS), n (%) | 0.940 | |||
| 21–40 | 38 (44.18) | 21 (42.85) | 17 (45.94) | |
| 41–60 | 32 (37.20) | 19 (38.77) | 13 (35.13) | |
| 61–100 | 16 (18.63) | 9 (18.38) | 7 (18.93) | |
| Instrumental Activities of Daily Living (IADLS), n (%) | 0.377 | |||
| 1 item | 34 (39.53) | 16 (32.65) | 18 (48.64) | |
| 2 items | 20 (23.25) | 13 (26.53) | 7 (18.91) | |
| 3 items | 14 (16.27) | 10 (20.40) | 4 (10.81) | |
| ≥4 items | 18 (20.95) | 10 (20.42) | 8 (21.64) | |
| Mini-Mental Status Examination (MMSE), n (%) | 0.379 | |||
| <24 | 13 (5.11) | 9 (18.36) | 4 (10.81) | |
| ≥24 | 73 (84.89) | 40 (81.64) | 33 (89.19) | |
| Geriatric Depression Scale (GDS), n (%) | 0.690 | |||
| <5 | 68 (79.07) | 38 (77.55) | 30 (81.08) | |
| ≥5 | 18 (20.93) | 11 (22.45) | 7 (18.92) | |
| Room type, n (%) | 0.755 | |||
| Single room | 12 (13.95) | 6 (12.24) | 6 (16.21) | |
| 2–6 persons/room | 74 (86.05) | 43 (87.76) | 31 (83.79) | |
| Presence of natural window view, n (%) | 0.172 | |||
| Yes | 34 (39.53) | 22 (44.90) | 12 (32.43) | |
| No | 52 (60.47) | 27 (55.10) | 25 (67.67) | |
| Presence of outdoor public space, n (%) | 0.204 | |||
| Yes | 21 (24.41) | 9 (18.36) | 12 (32.43) | |
| No | 65 (75.59) | 40 (81.64) | 25 (67.57) | |
| Number of leisure activities in LTCF per week, n (%) | 0.547 | |||
| 1–2 per week | 63 (73.26) | 37 (75.51) | 26 (70.27) | |
| 3–4 per week | 23 (26.74) | 12 (24.49) | 11 (29.73) | |
| Number of family visits per week, n (%) | 0.720 | |||
| 1 per week | 44 (89.79) | 25 (51.02) | 19 (51.35) | |
| 2 per week | 13 (15.11) | 6 (12.24) | 7 (18.91) | |
| 3 per week | 18 (20.93) | 12 (24.48) | 6 (16.21) | |
| ≥4 per week | 11 (12.79) | 6 (12.26) | 5 (13.53) | |
| Number of LTCF staff | 15.53 (6.78) | 19.55 (3.51) | 10.22 (6.40) | 0.083 |
| Time | SOC Score | Paired-Variable Difference | t | p Value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Baseline | 50.45 (6.07) | |||
| 4th week | 51.06 (6.28) | −0.61 (0.99) | −4.30 | 0.001 |
| 8th week | 56.22 (7.19) | −5.77 (3.88) | −10.40 | <0.001 |
| 12th week | 56.37 (7.20) | −5.91(3.78) | −10.94 | <0.001 |
| Groups | Baseline Mean ± SD 1 | 4th Week Mean ± SD | 8th Week Mean ± SD | 12th Week Mean ± SD |
|---|---|---|---|---|
| Experimental group | 50.45 ± 6.07 | 51.06 ± 6.28 | 56.22 ± 7.19 | 56.37 ± 7.20 |
| Control group | 52.97 ± 6.00 | 53.03 ± 6.04 | 53.22 ± 5.96 | 53.22 ± 5.96 |
| t | −1.91 | −1.46 | 2.06 | 2.15 |
| p | 0.059 | 0.146 | 0.042 | 0.034 |
| 95% Wald Confidence Interval | Hypothesis Test | ||||||
|---|---|---|---|---|---|---|---|
| Parameter | B | Std. Error | Lower | Upper | Wald Chi-Square | df | p Value |
| intercept | 52.97 | 0.97 | 51.06 | 54.88 | 2961.97 | 1 | 0.000 |
| Experimental group vs. Control group (reference) | 0.24 | 0.13 | −0.05 | 0.044 | 3.71 | 1 | 0.071 |
| Group × 12th week | 5.96 | 6.22 | 4.74 | 7.18 | 91.78 | 1 | <0.001 |
| Group × 8th week | 5.79 | 0.63 | 4.54 | 7.04 | 82.43 | 1 | <0.001 |
| Group × 4th week | 0.53 | 0.15 | 0.23 | 0.84 | 11.93 | 1 | 0.001 |
| scale | 40.43 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jueng, R.-N.; Chen, I.-J. The Effects of Horticultural Therapy on Sense of Coherence among Residents of Long-Term Care Facilities: A Quasi Experimental Design. Int. J. Environ. Res. Public Health 2022, 19, 5412. https://doi.org/10.3390/ijerph19095412
Jueng R-N, Chen I-J. The Effects of Horticultural Therapy on Sense of Coherence among Residents of Long-Term Care Facilities: A Quasi Experimental Design. International Journal of Environmental Research and Public Health. 2022; 19(9):5412. https://doi.org/10.3390/ijerph19095412
Chicago/Turabian StyleJueng, Ruo-Nan, and I-Ju Chen. 2022. "The Effects of Horticultural Therapy on Sense of Coherence among Residents of Long-Term Care Facilities: A Quasi Experimental Design" International Journal of Environmental Research and Public Health 19, no. 9: 5412. https://doi.org/10.3390/ijerph19095412
APA StyleJueng, R.-N., & Chen, I.-J. (2022). The Effects of Horticultural Therapy on Sense of Coherence among Residents of Long-Term Care Facilities: A Quasi Experimental Design. International Journal of Environmental Research and Public Health, 19(9), 5412. https://doi.org/10.3390/ijerph19095412






