Abstract
The aim of this systematic review (SR) of SRs was to assess the effectiveness of telerehabilitation based on behavior modification techniques (t-BMT) in patients with chronic musculoskeletal pain. We searched in PubMed, PEDro, Web of Science, CINAHL, PsycINFO, and Google Scholar (January 2022). The outcome measures were pain intensity, disability, psychological distress, pain-related fear of movement, disease impact, depressive symptoms, anxiety symptoms, and physical function. This review was previously registered on the international prospective register of systematic reviews PROSPERO (CRD42021262192). Methodological quality was analyzed using the AMSTAR and ROBIS scales, and the strength of evidence was established according to the Physical Activity Guidelines Advisory Committee grading criteria. Four SRs with and without meta-analyses covering 25 trials and involving 4593 patients were included. Of the three SRs that assessed pain intensity, two reported a significant decrease compared to usual care. Contradictory results were also found in the management of psychological distress, and of depressive and anxiety symptoms. However, two reviews found that t-BMT has significant effects on disability, and one review found that t-BMT seems to be effective for improving pain-related fear of movement and disease impact. Finally, one review found that t-BMT does not seem to be an effective modality to improve physical function. The quality of evidence was limited for all outcomes assessed. The results obtained showed that t-BMT was effective in improving disability, disease impact, and pain-related fear of movement, but it was not effective in improving physical function in patients with chronic pain. Mixed evidence was found for pain intensity, psychological distress, and depressive and anxiety symptoms, with a limited quality of evidence.
1. Introduction
The COVID-19 pandemic has provoked a major shift in the way we treat patients with persistent musculoskeletal pain [1]. The lack of access to clinics and the health emergency undermined face-to-face treatments [2]. An online survey has shown that 80% of chronic pain patients have experienced a worsening of their symptoms during the pandemic and an increase in the interference of pain with daily life, including work and physical activities [3]. It is evident that not treating these patients will lead to severe consequences for them [1]. In this context, telerehabilitation appears as a key solution to counteract the burden of the COVID-19 pandemic on patients with persistent musculoskeletal pain [1,4]. Telerehabilitation is the use of a technology-based virtual platform (e.g., the Internet, mobile applications) to provide various aspects of therapeutic rehabilitation remotely [5]. The use of telecommunication technologies seems promising [6], especially in a society where new technologies are omnipresent. Some pain services have almost quadrupled their use [7]. Suso-Martí et al. [8] showed that there were no statistically significant differences between in-person physical therapy treatment and its delivery via telerehabilitation for various chronic conditions. Physical therapy is essential for patients with severe disabilities, and telerehabilitation should not only allow the physiotherapist to enter the patient’s home, but also allow the individual to get out of lockdown [9]. However, there is no overview of the effects of telerehabilitation on patients with persistent musculoskeletal pain.
As Turk et al. [10] reported, psychosocial and behavioral factors play a significant role in the experience, maintenance, and exacerbation of pain. Part of the problem with chronic pain patients arises from how they react to their pain [11]. Behavioral modification techniques (BMTs), such as cognitive behavioral therapy, do not necessarily require the therapist to be physically present with the patient [12]. There are several systematic review articles with or without meta-analyses that have addressed this topic, but no research article has provided a general overview of the effect of telematic BMT (t-BMT) with respect to clinical endpoints and variables of interest in patients with chronic pain [6,13,14,15].
It is therefore the main aim of this review to synthesize the evidence on the effects of t-BMT in improving pain intensity, disability, psychological distress, depressive symptoms, anxiety symptoms, physical function, pain-related fear of movement, and disease impact, compared with no intervention or in-person treatment, in patients with persistent musculoskeletal pain.
2. Methods
This study was conducted in accordance with the Preferred Reporting Items for Overviews of Systematic Reviews, including a harm checklist (PRIO-harms), which consists of 27 items (56 sub-items), followed by a 5-stage process flow diagram (identification, screening, eligibility, inclusion, and separation of relevant studies) [16]. The review was previously registered on the international prospective register of systematic reviews PROSPERO (CRD42021262192).
2.1. Review Inclusion Criteria
The inclusion criteria employed in this article were based on methodological and clinical factors such as population, intervention, control, outcomes, and study design [17].
2.1.1. Population
The participants selected for the articles were patients older than 18 years diagnosed with any musculoskeletal disorder that was accompanied by chronic pain (e.g., fibromyalgia, chronic lower-back pain, migraine, chronic back pain). Chronic musculoskeletal pain was defined as diseases of the muscles and their associated ligaments and other connective tissue, and of the bones and cartilage, viewed collectively, along with pain that persists over time, under to the medical subject headings (MeSH) “Musculoskeletal diseases”, “Musculoskeletal Pain”, and “Chronic Pain”. Included systematic reviews had to explicitly state that they included patients with chronic pain lasting more than 3 months in their inclusion criteria. However, if they performed a “chronic pain” sub-analysis, we included it as well. Therefore, we excluded patients with acute musculoskeletal pain, traumatic musculoskeletal injuries, or confounding comorbidities such as cancer, as well as articles that did not specify the pain duration of the analyzed patients.
2.1.2. Intervention and Control
The intervention consisted of t-BMT conducted in isolation or combined with other treatment techniques. The following are some examples of known BMTs used in telerehabilitation: cognitive behavioral therapy (CBT), which is aimed at identifying and modifying the client’s maladaptive thoughts and dysfunctional behaviors through behavioral techniques to achieve change; acceptance and commitment therapy (ACT), which is based on the patient’s acceptance of their thoughts and feelings as a necessary part of their life in order to develop new and more flexible ways of thinking; self-management including exercise, which is based on self-monitoring, self-evaluation, and goal setting, among others; exposure behavioral therapy, which is based on the repeated exposure to the feared stimulus or context; and mindfulness, which is based on a moment-to-moment awareness of one’s experience without judgment. Web-based intervention was defined as the use of an online platform, through the Internet or a mobile application, to deliver therapeutic rehabilitation at a distance, according to the MeSH “Telerehabilitation”. We excluded any telerehabilitation not aimed at changing patients’ behavior. The compared groups used the following interventions: usual care; waiting lists; books or guides provided physically or remotely (by mail or e-mail) that are not specifically aimed at changing behavior; equivalent non-telerehabilitation intervention; magazine subscription control intervention; or in-person treatment.
2.1.3. Outcomes
The outcomes employed to assess the effects of t-BMT were pain intensity, disability (lack or limitation of any physical or psychological faculty that makes it impossible or difficult for a person to carry out a normal activity), psychological distress, depressive symptoms, anxiety symptoms, physical function, pain-related fear of movement, and disease impact.
2.1.4. Study Design
We selected systematic reviews (with or without a meta-analysis) of randomized controlled clinical trials (RCCTs) or controlled clinical trials (CCTs), and excluded systematic reviews that included RCCTs or CCTs in combination with non-experimental designs. There were no restrictions for any specific language, as recommended by the international criteria [18].
2.2. Search Strategy
We conducted the search for scientific articles on the following databases from their inception to March 2022: PubMed (Medline), PEDro, Web of Science, CINAHL, PsycINFO, and Google Scholar. The search strategy combined medical subject headings (MeSH) and non-MeSH terms, adding a Boolean operator (OR, NOT, and/or AND) to combine them (Appendix A). The search was conducted by two independent reviewers (C.V.R. and L.S.M.) using the same methodology. Differences that emerged during this phase were resolved by consensus. The reference sections of the original studies were screened manually, and the authors were contacted for further information if necessary.
2.3. Selection Criteria and Data Extraction
Initially, two independent reviewers (J.C.G. and L.S.M.) conducted a screening assessing the relevance of the systematic reviews (with and without meta-analyses) regarding the studies’ questions and objectives. The first screening was based on each study’s title information, abstract, and keywords. The full text was reviewed if there was no consensus or if the abstracts contained insufficient information. In the second phase of the screening, the full text was assessed if the studies met all of the inclusion criteria. Differences between the reviewers were resolved by a discussion and consensus process mediated by a third reviewer (F.C.M.). The data described in the Results section were extracted by means of a structured protocol that ensured that the most relevant information was obtained from each study.
2.4. Methodological Quality Assessment
Two independent reviewers (F.C.M. and L.S.M.) assessed the methodological quality of the systematic reviews (with or without meta-analyses), assessing each of the selected studies based on the Modified Quality Assessment Scale for Systematic Reviews (AMSTAR) developed by Barton et al. [19]—a scale shown to be a valid and reliable tool for assessing the methodological quality of systematic reviews. With a total of 13 items, each worth 2 points (with “yes” scoring 2, “in part” scoring 1, and “no” scoring 0), the maximum possible score is 26. A high-quality cutoff of 20 or more points was provided by the developers. The exclusion and keyword criteria were modified to better evaluate the selected systematic reviews in this study. In addition, we calculated the kappa coefficient (κ) and percentage (%) agreement scores to assess reliability prior to any consensus, and estimated the inter-rater reliability using κ: (1) κ > 0.7 indicates a high level of agreement between the reviewers, (2) κ of 0.5–0.7 indicates a moderate level of agreement, and (3) κ < 0.5 indicates a low level of agreement [20]. Disagreements on the final quality assessment score were resolved by consensus with a third independent reviewer (J.C.G.).
2.4.1. Risk of Bias Assessment
We assessed the risk of bias with the Risk of Bias in Systematic Reviews tool (ROBIS), which consists of 3 phases: (1) relevance assessment (optional); (2) identification of concerns with the review process through 4 domains related to study eligibility criteria, identification and selection of studies, data collection and study appraisal, and synthesis and findings; and (3) judgment on the risk of bias. The ROBIS tool includes signaling questions to evaluate specific domains to help judge the systematic review’s risk of bias, which should be answered as “yes”, “probably yes”, “probably no”, “no”, or “no information”. The risk of bias is therefore judged as “low”, high”, or “unclear” [21]. Two independent reviewers (F.C.M. and L.S.M.) evaluated the risk of bias in the selected studies. Disagreements were resolved through consensus and mediation by a third reviewer (J.C.G.).
2.4.2. Grading of Evidence
The Physical Activity Guidelines Advisory Committee (PAGAC) grading criteria were used to assess the grading of evidence. The criteria used to assess the quality of the evidence were as follows: (1) applicability of the study sample, exposures, and outcomes to the research question; (2) generalizability to the population of interest; (3) risk of bias/study limitations; (4) quantity and consistency of findings across studies; and (5) magnitude and precision of the effect(s). With these data, final evidence grades and conclusion statements for each research question were developed [22].
3. Results
3.1. Study Selection
The initial search revealed 309 records, and an additional 20 were retrieved manually from the references. Through the title and abstract screening and the full-text assessment, only four systematic reviews were eligible according to our criteria [6,13,14,15]. The study screening strategy is shown in the form of a flowchart (Figure 1). In total, 25 randomized controlled trials were included in the different systematic reviews. Only 16% (4/25) were used more than one time.
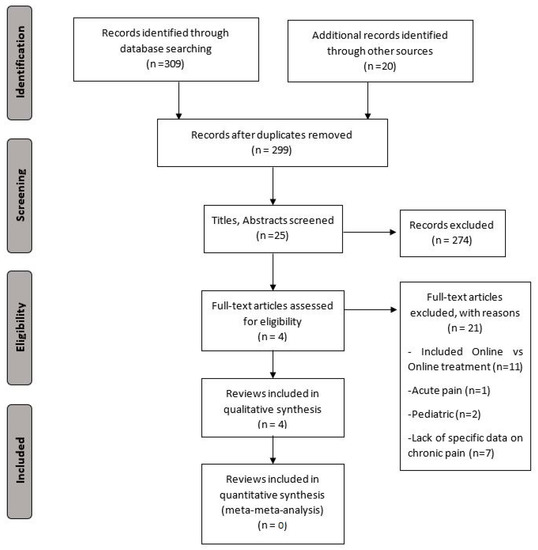
Figure 1.
PRISMA flowchart of study selection.
3.2. Characteristics of the Included Systematic Reviews
This umbrella review included a total of 4593 participants. Table 1 lists the characteristics of the systematic reviews included (i.e., study design, original studies included, demographic characteristics, interventions, variables, and results).

Table 1.
Characteristics of the reviews included in the umbrella review.
Two systematic reviews included chronic lower-back pain [6,13], and two included different types of chronic pain patients, such as fibromyalgia, chronic widespread pain, or headaches and migraine [14,15].
Interventions were mainly Internet-based; only one also included the use of mobile-based interventions [14]. They implemented different BMTs, such as ACT, CBT, education, self-management, exercise, exposure therapy, mindfulness, online feedback, or social support through an e-community. The clinical effects of these interventions were assessed in comparison to the effects of no or minimal intervention, or of an equivalent (or not) in-person intervention. Table 2 lists the details of the different interventions applied.

Table 2.
Intervention analysis.
3.3. Results of the Methodological Quality
The scores ranged from 19 to 23 points out of a possible 26, with a mean score of 20.25 ± 3.12 points. Only one (25%) study scored above 20 points and was considered high-quality (Table 3). The items with the highest scores were those related to the number of databases (the acceptable number was considered to be more than three databases [19]) and the inclusion and exclusion criteria. The lowest-scoring item was the consideration of the level of evidence in the conclusion of the review. The inter-rater reliability of the methodological quality assessment was high (κ = 0.72).

Table 3.
Quality assessment scores.
3.4. Results of Risk of Bias
Table 4 and Figure 2 show the results of the risk of bias assessment using ROBIS. In total, 25% of studies had a low risk of bias. The domains related to the “study eligibility criteria” and the “identification and selection of studies” had the lowest risk of bias (100%). In contrast, the domain related to the “synthesis and findings” had the highest risk of bias (50%). The inter-rater reliability for the risk of bias assessment was high (κ = 0.78).

Table 4.
Risk of bias assessment in systematic reviews through the ROBIS scale.
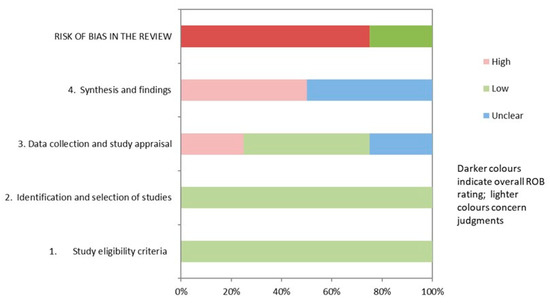
Figure 2.
Graphical representation of the ROBIS results.
3.5. Grading of Evidence Results
Table 5 shows the findings regarding the quality of evidence for each outcome of the research question. The quality of evidence found for all outcome measures was limited.

Table 5.
Summary of findings and quality of evidence (PAGAC).
3.6. Qualitative Synthesis
3.6.1. Pain Intensity
Three reviews with and without meta-analyses assessed the effectiveness of t-BMT on pain intensity in patients with chronic lower-back pain in the short term [6,13,14]. Ariza-Mateos et al. [14] found that t-BMT improved pain intensity in women with chronic pain. Similar results were found by Du et al. [6], who obtained a small effect size in favor of t-BMT on pain intensity (SMD = −0.26; 95% CI −0.42 to −0.09). However, Darío et al. [13] found a non-significant effect in favor of t-BMT in patients with chronic lower-back pain (SMD = −0.05; 95% CI −0.10 to 0.00).
In addition, one review with a meta-analysis showed that t-BMT had no significant effect (SMD = −0.01; 95% CI: −0.74 to 0.72) on pain intensity in chronic lower-back pain in the medium term [13].
3.6.2. Disability
Two reviews with meta-analyses assessed the effectiveness of t-BMT on disability in patients with chronic lower-back pain in the short term [6,13]. Both articles showed statistically significant differences in favor of t-BMT in patients with lower-back pain in the short term. First, Du et al. [6] showed a significant improvement in disability with a small effect size of t-BMT (SMD = −0.34; 95% CI −0.50 to −0.17). Second, Darío et al. [13] found a trivial effect size of t-BMT on disability in the short term (SMD = −0.04; 95% CI −0.07 to −0.02).
However, one review with a meta-analysis showed that t-BMT had no significant effect (SMD = 0.00; 95% CI: −0.06 to 0.07) on disability in chronic lower-back pain in the medium term [13].
3.6.3. Psychological Symptoms
Two reviews with and without meta-analyses found that t-BMT was not superior to in-person treatment (CBT), but had positive effects compared to waiting lists on psychological distress in fibromyalgia (one primary study; n = 40; SMD = 2.647; SE = 0.429) [14,15]; however, both reviews included the same primary study. One review with a meta-analysis found that t-BMT had no positive effects in unspecific chronic pain compared to usual care (one primary study; n = 63; SMD = −0.051; SE = 0.249) [15]. Timepoints of the follow-up results were unclear.
The other meta-analysis, against usual care or waiting lists, showed a small-to-moderate effect size of t-BMT on depressive symptoms in patients with unspecific chronic pain (eight primary studies; n = 1418; SMD = 0.372; SE = 0.128) and fibromyalgia (four primary studies; n = 305; SMD = 0.679; SE = 0.259) but no statistically significant effect on migraine and headache (three primary studies; n = 320; SMD = 0.142; SE = 0.120) [15]. They also showed a small effect size on anxiety in patients with unspecific chronic pain (seven primary studies; n = 1355; SMD = 0.372; SE = 0.128), but no statistically significant effect on migraine and headache (two primary studies; n = 275; SMD = 0.422; SE = 0.301) or fibromyalgia (one primary study; n = 118; SMD = 0.046; SE = 0.183) [15]. Timepoints of the follow-up results were unclear.
One review without a meta-analysis found that t-BMT seems to be effective in improving pain-related fear of movement in patients with fibromyalgia compared to usual care (one primary study; n = 67, p = 0.001) [14]. Timepoints of the follow-up results were unclear.
3.6.4. Disease Impact
One review without a meta-analysis found that t-BMT seems to be effective in improving disease impact in patients with fibromyalgia compared to usual care or waiting lists (five primary studies; n = 403; p = 0.0006 to p < 0.001) [14]. However, it does not seem to be superior to in-person BMT. Timepoints of the follow-up results were unclear.
3.6.5. Physical Function
One review without a meta-analysis found that t-BMT does not seem to be an effective modality to improve the physical function of patients with chronic lower-back pain in the short (one primary study; n = 229) and medium term (one primary study; n = 334), compared to minimal intervention [13].
4. Discussion
4.1. Principal Results
The main aim of this umbrella review was to evaluate the effects of t-BMT on pain intensity, disability, psychological distress, depressive symptoms, anxiety symptoms, physical function, pain-related fear of movement, and disease impact in patients with chronic musculoskeletal pain. Our results showed that t-BMT was not effective in improving physical function in chronic lower-back pain compared with minimal intervention. However, t-BMT seemed to be effective in improving disability, disease impact, and pain-related fear of movement in fibromyalgia when compared with waiting lists or usual care. In addition, it seems that there was mixed evidence in favor of t-BMT regarding pain intensity, psychological distress, and anxiety and depressive symptoms. Regarding the comparison between telematic vs. in-person BMTs, we found no differences in psychological distress and disease impact in fibromyalgia. No other variables reported this comparison. Finally, t-BMT did not seem to be effective in improving anxiety and depressive symptoms in migraine and headache compared with waiting lists or usual care. However, it was effective in improving depressive symptoms and anxiety in an unspecific chronic pain population compared with waiting lists or usual care.
Due to the COVID-19 pandemic, there is growing scientific and societal interest in telerehabilitation. A recent systematic review suggested that telerehabilitation is a strategy comparable to conventional rehabilitation in patients with cardiac or neurological disorders [8]. However, our results do not support this benefit in the totality of variables studied in patients with chronic musculoskeletal pain. It is necessary to highlight the complex nature of rehabilitation for these patients. Chronic musculoskeletal pain depends on a multifactorial interaction of biological, psychological, and social factors [10,23]. It remains challenging to develop conventional treatments that are beneficial for these patients, because many of the current treatments are ineffective. Because telerehabilitation is based on these treatments, it is therefore possible that the results are similar to those of conventional treatments. In addition, previous research has found that telerehabilitation may result in lower patient adherence or confidence, which may decrease the treatment’s effectiveness [24]. Furthermore, difficulties in assessing some outcomes (e.g., physical function) during telerehabilitation might negatively impact the validity and reliability of the results. However, the results of telerehabilitation on psychological symptoms and disease impact reveal the therapeutic potential of these interventions in the management of chronic musculoskeletal pain. In this direction, future trials should evaluate the impact of the time of intervention, as well as the resources used for the procedure, since it seems that longer interventions using face-to-face telerehabilitation systems accompanied by social support may be more effective in this population [25].
4.2. Gap in the Literature
Most of the systematic reviews included were rated as having a high risk of bias. Future reviews should improve on this to increase our confidence in their results. The effect of a technique may be overestimated when we compare it with no intervention [26]. Future systematic reviews should try to avoid pooling studies that compare t-BMT with minimal intervention and studies that compare it with another in-person active intervention in the same statistical analysis, because the effect(s) may be different. We excluded a large proportion of systematic reviews because they did not include only studies evaluating telerehabilitation versus in-person treatment, but compared one type of telerehabilitation versus another. Future reviews should also differentiate studies in different sub-analyses. We found that t-BMT is not effective in patients with chronic lower-back pain; however, there is a necessity to evaluate its effects on other populations to increase its external validity. Future systematic reviews should evaluate the effects of different electronic formats (e.g., synchronous/non-synchronous, on mobile, laptop, tablet, etc.) in different sub-analyses to determine whether all of the different formats are suitable for implementing behavior modification techniques.
4.3. Limitations and Strengths
We found a limited strength of evidence for our results; there is a need to follow to investigate the effects of t-BMT on patients with chronic musculoskeletal pain. The meta-analyses we included considered nonspecifically different types of interventions (CBT, ACT, exposure behavioral therapy, or mindfulness) and different electronic formats (internet-based or mobile-based), so our estimated effect might be different from the true therapeutic effect of t-BMT. In addition, another issue identified is the high risk of bias in some of the studies. With only four included, this is a major limitation. This was found to be due to minor problems in some areas of interest, such as the synthesis of the findings, or the data collection and evaluation of the studies. To improve these aspects for the future, the authors should describe methods of data collection, what data were extracted from studies or collected through other means, how the risk of bias was assessed (e.g., the number of reviewers involved), and the tool used to assess the risk of bias or describe the synthesis methods. In addition, we were not able to assess publication bias through funnel and Doi plots, because only two meta-analyses were compared. This should be taken into consideration as a limitation. Finally, it is important to stress that the Google Scholar database is very limited in terms of Boolean search operators, so it is almost impossible to replicate a search in this database, and this must be made public.
5. Conclusions
The results obtained show that t-BMT was effective in improving disability, pain-related fear of movement, and disease impact compared to minimal intervention, no intervention, or usual care, but not in improving physical function, with a limited quality of evidence. Mixed evidence was found regarding pain intensity, psychological distress, and anxiety and depressive symptoms—also with a limited quality of evidence. Finally, t-BMT was as effective as in-person BMT for the management of psychological distress and disease impact.
Author Contributions
Conceptualization, F.C.-M. and C.V.-R.; methodology, F.C.-M., C.V.-R. and L.S.-M.; validation, J.C. (Joaquín Calatayud), M.B.-D. and J.C. (José Casaña); formal analysis, F.C.-M. and C.V.-R.; investigation, F.C.-M., C.V.-R., L.S.-M., M.B.-D. and J.C. (José Casaña); resources, A.H.-G., J.C. (Joaquín Calatayud) and J.C. (José Casaña); data curation, F.C.-M., L.S.-M., A.H.-G. and C.V.-R.; writing—original draft preparation, all authors; writing—review and editing, all authors; visualization, all authors; supervision, F.C.-M. and J.C. (José Casaña); project administration, J.C. (José Casaña). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. PubMed Systematic Search Strategy
((“Web”) OR (“Cell phone” [MesH]) OR (“eTherapy”) OR (“Internet”) OR (“Online”) OR (“Telerehabilitation”) OR (“Internet-Based Intervention” [MesH]) OR (“Telerehabilitation” [MesH]) OR (Telemedicine [MesH])) AND ((“Chronic Pain”) OR (“Chronic Pain” [Mesh])) AND ((((systematic review [ti] OR systematic literature review [ti] OR systematic scoping review [ti] OR systematic narrative review [ti] OR systematic qualitative review [ti] OR systematic evidence review [ti] OR systematic quantitative review [ti] OR systematic meta-review [ti] OR systematic critical review [ti] OR systematic mixed studies review [ti] OR systematic mapping review [ti] OR systematic cochrane review [ti] OR systematic search and review [ti] OR systematic integrative review [ti]) NOT comment [pt] NOT (protocol [ti] OR protocols [ti])) NOT MEDLINE [subset]) OR (Cochrane Database Syst Rev [ta] AND review [pt]) OR systematic review [pt]).
References
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; de Williams, A.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Lacasse, A.; Pagé, M.G.; Dassieu, L.; Sourial, N.; Janelle-Montcalm, A.; Dorais, M.; Nguena Nguefack, H.L.; Godbout-Parent, M.; Hudspith, M.; Moor, G.; et al. Impact of the COVID-19 pandemic on the pharmacological, physical, and psychological treatments of pain: Findings from the Chronic Pain & COVID-19 Pan-Canadian Study. Pain Rep. 2021, 6, e891. [Google Scholar] [PubMed]
- Nieto, R.; Pardo, R.; Sora, B.; Feliu-Soler, A.; Luciano, J.V. Impact of COVID-19 lockdown measures on Spanish people with chronic pain: An online study survey. J. Clin. Med. 2020, 9, 3558. [Google Scholar] [CrossRef] [PubMed]
- Karos, K.; McParland, J.L.; Bunzli, S.; Devan, H.; Hirsh, A.; Kapos, F.P.; Keogh, E.; Moore, D.; Tracy, L.M.; Ashton-James, C.E. The social threats of COVID-19 for people with chronic pain. Pain 2020, 161, 2229–2235. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, O.J.; Persaud, Y.; Kimball, A.B. Telehealth Systems; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-management program for chronic low back pain: A systematic review and meta-analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Mullins, C.F.; Harmon, D.; O’Connor, T. Quantifying the impact of COVID-19 on chronic pain services in the Republic of Ireland. Ir. J. Med. Sci. 2021, 191, 7–11. [Google Scholar] [CrossRef]
- Suso-Martí, L.; La Touche, R.; Herranz-Gómez, A.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cuenca-Martínez, F. Effectiveness of telerehabilitation in physical therapist practice: An umbrella and mapping review with meta-meta-analysis. Phys. Ther. 2021, 101, pzab075. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Moggio, L.; Ammendolia, A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation. J. Enabling Technol. 2021, 15, 117–121. [Google Scholar] [CrossRef]
- Turk, D.C.; Swanson, K.S.; Tunks, E.R. Psychological approaches in the treatment of chronic pain patients—When pills, scalpels, and needles are not enough. Can. J. Psychiatry 2008, 53, 213–223. [Google Scholar] [CrossRef] [Green Version]
- Sharp, T.J. Chronic pain: A reformulation of the cognitive-behavioural model. Behav. Res. Ther. 2001, 39, 787–800. [Google Scholar] [CrossRef]
- Macea, D.D.; Gajos, K.; Daglia Calil, Y.A.; Fregni, F. The efficacy of web-based cognitive behavioral Interventions for chronic pain: A systematic review and meta-analysis. J. Pain 2010, 11, 917–929. [Google Scholar] [CrossRef] [PubMed]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Mateos, M.J.; Cabrera-Martos, I.; Prados-Román, E.; Granados-Santiago, M.; Rodríguez-Torres, J.; Carmen Valenza, M. A systematic review of internet-based interventions for women with chronic pain. Br. J. Occup. Ther. 2020, 84, 6–14. [Google Scholar] [CrossRef]
- White, V.; Linardon, J.; Stone, J.E.; Holmes-Truscott, E.; Olive, L.; Mikocka-Walus, A.; Hendrieckx, C.; Evans, S.; Speight, J. Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2020, 52, 548–573. [Google Scholar] [CrossRef]
- Bougioukas, K.I.; Liakos, A.; Tsapas, A.; Ntzani, E.; Haidich, A.B. Preferred reporting items for overviews of systematic reviews including harms checklist: A pilot tool to be used for balanced reporting of benefits and harms. J. Clin. Epidemiol. 2018, 93, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.W. Popping the (PICO) question in research and evidence-based practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef]
- Moher, D.; Pham, B.; Jones, A.; Cook, D.J.; Jadad, A.R.; Moher, M.; Tugwell, P.; Klassen, T.P. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998, 352, 609–613. [Google Scholar] [CrossRef]
- Barton, C.J.; Webster, K.E.; Menz, H. Evaluation of the scope and quality of systematic reviews on nonpharmacological conservative treatment for patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2008, 38, 529–541. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Torres, A.; Tennant, B.; Ribeiro-Lucas, I.; Vaux-Bjerke, A.; Piercy, K.; Bloodgood, B. Umbrella and systematic review methodology to support the 2018 physical activity guidelines advisory committee. J. Phys. Act. Health 2018, 15, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Okifuji, A. Psychological factors in chronic pain: Evolution and revolution. J. Consult. Clin. Psychol. 2002, 70, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Hoaas, H.; Andreassen, H.K.; Lien, L.A.; Hjalmarsen, A.; Zanaboni, P. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: A mixed methods study. BMC Med. Inform. Decis. Mak. 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wildevuur, S.E.; Simonse, L.W.L. Information and communication technology—Enabled person-centered care for the “Big Five” chronic conditions: Scoping review. J. Med. Internet Res. 2015, 17, e77. [Google Scholar] [CrossRef] [PubMed]
- Morral, A.; Urrutia, G.; Bonfill, X. Placebo effect and therapeutic context: A challenge in clinical research. Med. Clin. (Barc) 2017, 149, 26–31. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).