Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Setting of the Study—A Retrospective Study
2.1.1. Data Collection
- (A)
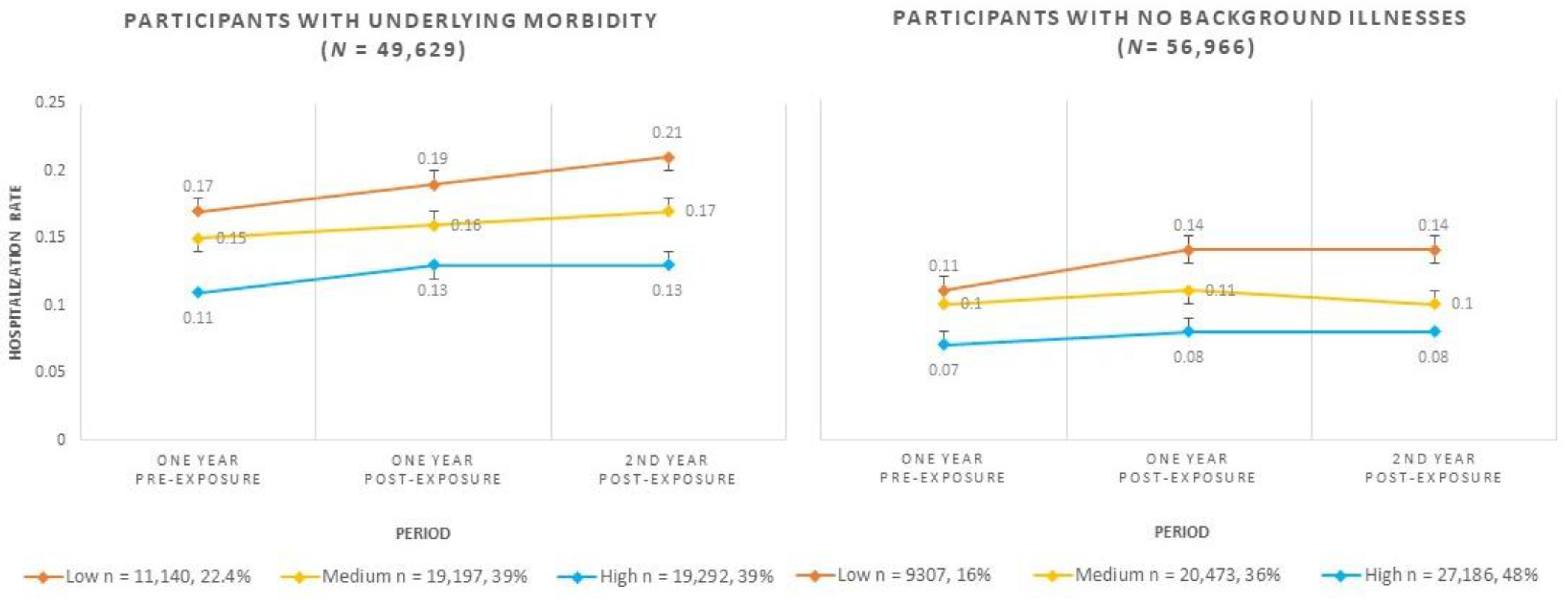
- Morbidity factors based on established MHS registries—We used MHS registries for four chronic morbidities for each patient: cardiovascular, obstructive pulmonary disease, overweight, and diabetes. We chose to focus on these specific morbidities following the well-documented short-term impacts of wildfires on them [4,6,7]. Overweight was chosen due to its increased prevalence in the general population and the association of obesity with other non-communicable diseases. The registries are updated automatically every day, drawing data from many sources: diagnoses, hospital discharge codes, billing information from providers, and prescription information [23]. The study population was divided into two sub-populations: the offset population that did not appear in any of these registries at the time of exposure (n = 56,966, 54%), and those with one or more of the chronic morbidities described above at the time of exposure (n = 49,629, 46%). In this study, we did not measure co-morbidity because our pre-analysis to examine the impact of each chronic condition on the hospitalization rate during the study periods revealed similar findings for each.
- (B)
- Hospitalization over a three-year period—We included the hospitalization days (based on the number of overnight stays) from all types of Israeli hospitals in all wards, except the maternity wards. The hospitalization information spanned from one year pre-exposure (22 November 2015) to two years post-exposure (27 November 2018).
- (C)
- Personal characteristics (age and gender).
- (D)
- Socio-economic status (SES) on a scale of 1–10 (1 = low to 10 = high), based on a poverty index calculated for each residential location. The enumeration area was calculated for each location based on a geographical unit (usually consisting of several thousand individuals) defined by the Israeli Central Bureau of Statistics, based on the homogeneity of the socio-demographic characteristics of the residing population. The poverty index is based on several factors, including: educational level, physical conditions, household income, crowding, and car ownership [24]. The study was approved by MHS’s Institutional Review Board for the Protection of Human Subjects (0028-19-MHS).
2.1.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Socio-Economic Status | Period | Hospitalization Rate | ||
|---|---|---|---|---|
| Mean | 95% Wald Confidence Interval | |||
| Lower | Upper | |||
| Participants with underlying morbidity (n = 49,629) | ||||
| High | One year pre-exposure | 0.11 | 0.11 | 0.11 |
| One year post-exposure | 0.13 | 0.12 | 0.13 | |
| 2nd year post-exposure | 0.13 | 0.13 | 0.14 | |
| Medium | One year pre-exposure | 0.15 | 0.14 | 0.15 |
| One year post-exposure | 0.16 | 0.16 | 0.17 | |
| 2nd year post-exposure | 0.17 | 0.17 | 0.18 | |
| Low | One year pre-exposure | 0.17 | 0.17 | 0.18 |
| One year post-exposure | 0.19 | 0.19 | 0.20 | |
| 2nd year post-exposure | 0.21 | 0.20 | 0.21 | |
| Participants with no background illnesses (n = 56,966) | ||||
| High | One year pre-exposure | 0.07 | 0.07 | 0.08 |
| One year post-exposure | 0.08 | 0.08 | 0.09 | |
| 2nd year post-exposure | 0.08 | 0.08 | 0.08 | |
| Medium | One year pre-exposure | 0.10 | 0.10 | 0.11 |
| One year post-exposure | 0.11 | 0.10 | 0.11 | |
| 2nd year post-exposure | 0.10 | 0.10 | 0.11 | |
| Low | One year pre-exposure | 0.11 | 0.10 | 0.12 |
| One year post-exposure | 0.14 | 0.13 | 0.15 | |
| 2nd year post-exposure | 0.14 | 0.13 | 0.15 | |
References
- Black, C.; Tesfaigzi, Y.; Bassein, J.A.; Miller, L.A. Wildfire smoke exposure and human health: Significant gaps in research for a growing public health issue. Environ. Toxicol. Pharmacol. 2017, 55, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Keim, M.E. Building Human Resilience. The Role of Public Health Preparedness and Response as an Adaptation to Climate Change. Am. J. Prev. Med. 2008, 35, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Health effects of wildfire smoke in children and public health tools: A narrative review. J. Expo. Sci. Environ. Epidemiol. 2020, 31, 1–20. [Google Scholar] [CrossRef]
- Kizer, K.W. Extreme Wildfires—A Growing Population Health and Planetary Problem. JAMA 2020, 324, 1605–1606. [Google Scholar] [CrossRef]
- Cascio, W.E. Wildland fire smoke and human health. Sci. Total Environ. 2017, 624, 586–595. [Google Scholar] [CrossRef]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [Green Version]
- Hänninen, O.O.; Salonen, R.O.; Koistinen, K.; Lanki, T.; Barregard, L.; Jantunen, M. Population exposure to fine particles and esti-mated excess mortality in Finland from an East European wildfire episode. J. Expo. Sci. Environ. Epidemiol. 2009, 9, 414–422. [Google Scholar] [CrossRef] [Green Version]
- Abdo, M.; Ward, I.; O’dell, K.; Ford, B.; Pierce, J.R.; Fischer, E.V.; Crooks, J.L. Impact of Wildfire Smoke on Adverse Pregnancy Outcomes in Colorado, 2007–2015. Int. J. Environ. Res. Public Health 2019, 16, 3720. [Google Scholar] [CrossRef] [Green Version]
- Heft-Neal, S.; Driscoll, A.; Yang, W.; Shaw, G.; Burke, M. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ. Res. 2021, 203, 111872. [Google Scholar] [CrossRef]
- Cleland, H.J.; Proud, D.; Spinks, A.; Wasiak, J. Multidisciplinary team response to a mass burn casualty event: Outcomes and implications. Med. J. Aust. 2011, 194, 589–593. [Google Scholar] [CrossRef]
- Proctor, C.R.; Lee, J.; Yu, D.J.; Shah, A.D.; Whelton, A.J. Wildfire caused widespread drinking water distribution network contamination. AWWA Water Sci. 2020, 2, e1183. [Google Scholar] [CrossRef]
- Ignatavičius, G.; Sakalauskienė, G.; Oškinis, V. Influence of land fires on increase of heavy metal concentrations in river waters of lithuania. J. Environ. Eng. Landsc. Manag. 2006, 14, 46–51. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Cova, T.J.; Dennison, P.E. Setting Wildfire Evacuation Triggers by Coupling Fire and Traffic Simulation Models: A Spatiotemporal GIS Approach. Fire Technol. 2018, 55, 617–642. [Google Scholar] [CrossRef]
- Barnett, J.; Dennis-Rouse, M.; Martinez, V. Wildfire disaster leads to facilities evacuation. Orthop. Nurs. 2009, 28, 17–20. [Google Scholar] [CrossRef]
- Deyoung, S.E.; Chase, J.; Branco, M.P.; Park, B. The Effect of Mass Evacuation on Infant Feeding: The Case of the 2016 Fort McMurray Wildfire. Matern. Child Health J. 2018, 22, 1826–1833. [Google Scholar] [CrossRef]
- Grant, E.; Runkle, J.D. Long-term health effects of wildfire exposure: A scoping review. J. Clim. Chang. Health 2021, 6, 100110. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Ritchie, A.; Brown, M.R.G.; Noble, S.; Mankowsi, M.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; et al. Long-Term Mental Health Effects of a Dev-astating Wildfire Are Amplified by Socio-Demographic and Clinical Antecedents in Elementary and High School Staff. Front. Psychiatry 2016, 11, 448. [Google Scholar] [CrossRef]
- Abatzoglou, J.T.; Williams, A.P. Impact of anthropogenic climate change on wildfire across western US forests. Proc. Natl. Acad. Sci. USA 2016, 113, 11770–11775. [Google Scholar] [CrossRef] [Green Version]
- The State Comptroller and Ombudsman of Israel. Preparadness of Local Authorities for Fires, Their Functioning during the Wave of Fires in November 2016, Compensation for the Casualties and Costs to the Economy. 2018. Available online: https://www.mevaker.gov.il/sites/DigitalLibrary/Pages/Publications/113.aspx?AspxAutoDetectCookieSupport=1 (accessed on 19 April 2022). (In Hebrew)
- Turco, M.; Levin, N.; Tessler, N.; Saaroni, H. Recent changes and relations among drought, vegetation and wildfires in the East-ern Mediterranean: The case of Israel. Glob. Planet. Chang. 2017, 151, 28–35. [Google Scholar] [CrossRef]
- Nguyen, H.; Azzi, M.; White, S.; Salter, D.; Trieu, T.; Morgan, G.; Rahman, M.; Watt, S.; Riley, M.; Chang, L.; et al. The Summer 2019–2020 Wildfires in East Coast Australia and Their Impacts on Air Quality and Health in New South Wales, Australia. Int. J. Environ. Res. Public Health 2021, 18, 3538. [Google Scholar] [CrossRef]
- Clarfield, A.M.; Manor, O.; Bin Nun, G.; Shvarts, S.; Azzam, Z.S.; Afek, A.; Basis, F.; Israeli, A. Health and health care in Israel: An introduction. Lancet 2017, 389, 2503–2513. [Google Scholar] [CrossRef]
- Arbelle, J.E.; Chodick, G.; Goldstein, A.; Porath, A. Multiple chronic disorders—Health care system’s modern challenge in the Maccabi Health Care System. Isr. J. Health Policy Res. 2014, 3, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Israel Central Bureau of Statistics. Characterization and Classification of Geographical Units by the Socio-Economic Level of the Population; Israel Central Bureau of Statistics: Jerusalem, Israel, 2019. [Google Scholar]
- Thomas, K.; Hardy, R.D.; Lazrus, H.; Mendez, M.; Orlove, B.; Rivera-Collazo, I.; Roberts, J.T.; Rockman, M.; Warner, B.P.; Winthrop, R. Explaining differential vulnerability to climate change: A social science review. WIREs Clim. Chang. 2018, 10, e565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, I.P.; Haugo, R.D.; Robertson, J.C.; Levin, P.S. The unequal vulnerability of communities of color to wildfire. PLoS ONE 2018, 13, e0205825. [Google Scholar] [CrossRef] [Green Version]
- Shiba, K.; Kawahara, T.; Aida, J.; Kondo, K.; Kondo, N.; James, P.; Arcaya, M.; Kawachi, I. Causal Inference in Studying the Long-Term Health Effects of Disasters: Challenges and Potential Solutions. Am. J. Epidemiol. 2021, 190, 1867–1881. [Google Scholar] [CrossRef] [PubMed]
- Eitan, O.; Yuval; Barchana, M.; Dubnov, J.; Linn, S.; Carmel, Y.; Broday, D.M. Spatial analysis of air pollution and cancer incidence rates in Haifa Bay, Israel. Sci. Total Environ. 2010, 408, 4429–4439. [Google Scholar] [CrossRef]
- Hrabok, M.; Delorme, A.; Agyapong, V.I. Threats to Mental Health and Well-Being Associated with Climate Change. J. Anxiety Disord. 2020, 76, 102295. [Google Scholar] [CrossRef]
- Amster, E.D.; Fertig, S.S.; Green, M.; Carel, R. 589 Occupational exposures and psycholog-ical symptoms among fire fighters and police during a major wildfire: The carmel cohort study. Occup. Environ. Med. 2018, 75, A590–A591. [Google Scholar]
- Palgi, Y.; Dicker-Oren, S.D.; Greene, T. Evaluating a community fire as human-made vs. natural disaster moderates the relationship between peritraumatic distress and both PTSD symptoms and posttraumatic growth. Anxiety Stress Coping 2020, 33, 569–580. [Google Scholar] [CrossRef]
- Luo, M.S.; Chui, E.W.T.; Li, L.W. The Longitudinal Associations between Physical Health and Mental Health among Older Adults. Aging Ment. Health 2019, 24, 1990–1998. [Google Scholar] [CrossRef]
- Regvat, J.; Žmitek, A.; Vegnuti, M.; Košnik, M.; Šuškovič, S. Anxiety and Depression during Hospital Treatment of Exacerbation of Chronic Obstructive Pulmonary Disease. J. Int. Med Res. 2011, 39, 1028–1038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrier, L.; Ski, C.F.; O’Brien, C.; Jenkins, Z.; Thompson, D.R.; Moore, G.; Ward, G.; Castle, D.J. Bridging the gap between diabetes care and mental health: Perspectives of the Mental health IN DiabeteS Optimal Health Program (MINDS OHP). BMC Endocr. Disord. 2021, 21, 96. [Google Scholar] [CrossRef] [PubMed]
- Headrick, J.P.; Peart, J.N.; Budiono, B.; Shum, D.H.K.; Neumann, D.L.; Stapelberg, N.J. The heartbreak of depression: ‘Psycho-cardiac’ coupling in myocardial infarction. J. Mol. Cell. Cardiol. 2017, 106, 14–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Guidance to Protect Health from Climate Change through Health Adaptation Planning. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/137383/9789241508001_eng.pdf (accessed on 19 April 2022).
| Variable | Study Population (n = 106,595) | ||
|---|---|---|---|
| n | % | ||
| Gender | Female | 55,291 | 51.8 |
| Male | 51,304 | 48.1 | |
| Country of birth | Israel | 76,735 | 72.0 |
| Other | 29,860 | 28.0 | |
| Median age at exposure | 37 (IQR = 17–56) | ||
| Mean SES at exposure | 6.74 (SD = 2.01, rank 2–10) | ||
| Registry | Cardiovascular | 7925 | 7.4 |
| Overweight | 36,850 | 34.6 | |
| Obstructive pulmonary disease | 1253 | 1.2 | |
| Diabetes | 27,425 | 25.7 | |
| Disease | Variable | ||
|---|---|---|---|
| Cardiovascular n = 7925 (7.4%) | Median age | 69 (IQR = 57–78) | |
| SES | 6.47 (SD = 2.18, 2–10) | ||
| Gender | Male | 4706 (59.4%) | |
| Birth country | Israel | 3856 (48.7%) | |
| Obstructive pulmonary disease n = 1253 (1.2%) | Median age | 70 (IQR = 64–77) | |
| SES | 6.19 (SD = 2.21, 2–10) | ||
| Gender | Male | 596 (47.6%) | |
| Birth country | Israel | 556 (44.4%) | |
| Diabetes n = 27,425 (25.7%) | Median age | 61 (IQR = 50–79) | |
| SES | 6.39 (SD = 2.53, 2–10) | ||
| Gender | Male | 12,605 (46%) | |
| Birth country | Israel | 13,623 (49.7%%) | |
| Overweight n = 36,850 (34.6%) | Median age | 50 (IQR = 36–62) | |
| SES | 6.51 (SD = 2.11, 2–10) | ||
| Gender | Male | 18,789 (51%) | |
| Birth country | Israel | 22,801 (61.9) |
| Variables | B | Exp(B) | 95% Confidence Interval for Exp(B) | |||
|---|---|---|---|---|---|---|
| Sig. | Lower | Upper | ||||
| Gender | Male | 0.081 | 1.085 | <0.001 | 1.064 | 1.106 |
| Female | 1 | |||||
| Age at exposure (years) | 0.028 | 1.028 | <0.001 | 1.028 | 1.029 | |
| Study periods | 2nd year post exposure | 0.240 | 1.272 | <0.001 | 1.154 | 1.401 |
| 1st year post-exposure | 0.220 | 1.246 | <0.001 | 1.130 | 1.372 | |
| One year pre-exposure | 1 | |||||
| Registry | With underlying morbidity | 0.465 | 1.593 | <0.001 | 1.466 | 1.730 |
| With no underlying morbidity | 1 | |||||
| SES categories | High | −0.388 | 0.678 | <0.001 | 0.621 | 0.741 |
| Medium | −0.066 | 0.936 | 0.141 | 0.857 | 1.022 | |
| Low | 1 | |||||
| Interactions | ||||||
| With morbidity × High SES × 2nd year post-exposure | −0.138 | 0.871 | 0.121 | 0.732 | 1.037 | |
| With morbidity × High SES × 1st year post-exposure | −0.156 | 0.856 | 0.080 | 0.719 | 1.019 | |
| With morbidity × High SES × 1 year pre-exposure | −0.069 | 0.933 | 0.188 | 0.842 | 1.034 | |
| With morbidity × Medium SES × 2nd year post-exposure | −0.190 | 0.827 | 0.032 | 0.696 | 0.983 | |
| With morbidity × Medium SES × 1st year post-exposure | −0.218 | 0.804 | 0.014 | 0.676 | 0.957 | |
| With morbidity × Medium SES × 1 year pre-exposure | −0.106 | 0.899 | 0.041 | 0.812 | 0.996 | |
| With morbidity × Low SES × 2ndyear post-exposure | −0.074 | 0.928 | 0.186 | 0.831 | 1.037 | |
| With morbidity × Low SES × 1st year post-exposure | −0.119 | 0.888 | 0.036 | 0.795 | 0.992 | |
| With morbidity × Low SES × 1 year pre-exposure | 1 | |||||
| With no morbidity × High SES × 2nd year post-exposure | −0.167 | 0.847 | 0.006 | 0.751 | 0.954 | |
| With no morbidity × High SES × 1st year post-exposure | −0.091 | 0.913 | 0.138 | 0.810 | 1.030 | |
| With no morbidity × High SES × 1 year pre-exposure | 1 | |||||
| With no morbidity × Medium SES × 2nd year post-exposure | −0.220 | 0.802 | <0.001 | 0.711 | 0.905 | |
| With no morbidity × Medium SES × 1st year post-exposure | −0.160 | 0.852 | 0.009 | 0.755 | 0.961 | |
| With no morbidity × Medium SES × 1 year pre-exposure | 1 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen, O.; Shapira, S.; Furman, E. Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel. Int. J. Environ. Res. Public Health 2022, 19, 5012. https://doi.org/10.3390/ijerph19095012
Cohen O, Shapira S, Furman E. Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel. International Journal of Environmental Research and Public Health. 2022; 19(9):5012. https://doi.org/10.3390/ijerph19095012
Chicago/Turabian StyleCohen, Odeya, Stav Shapira, and Eyal Furman. 2022. "Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel" International Journal of Environmental Research and Public Health 19, no. 9: 5012. https://doi.org/10.3390/ijerph19095012
APA StyleCohen, O., Shapira, S., & Furman, E. (2022). Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel. International Journal of Environmental Research and Public Health, 19(9), 5012. https://doi.org/10.3390/ijerph19095012







