Implementation of the Strategy for Breastfeeding and Complementary Feeding in the Federal District in Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Design
2.3. Analyses
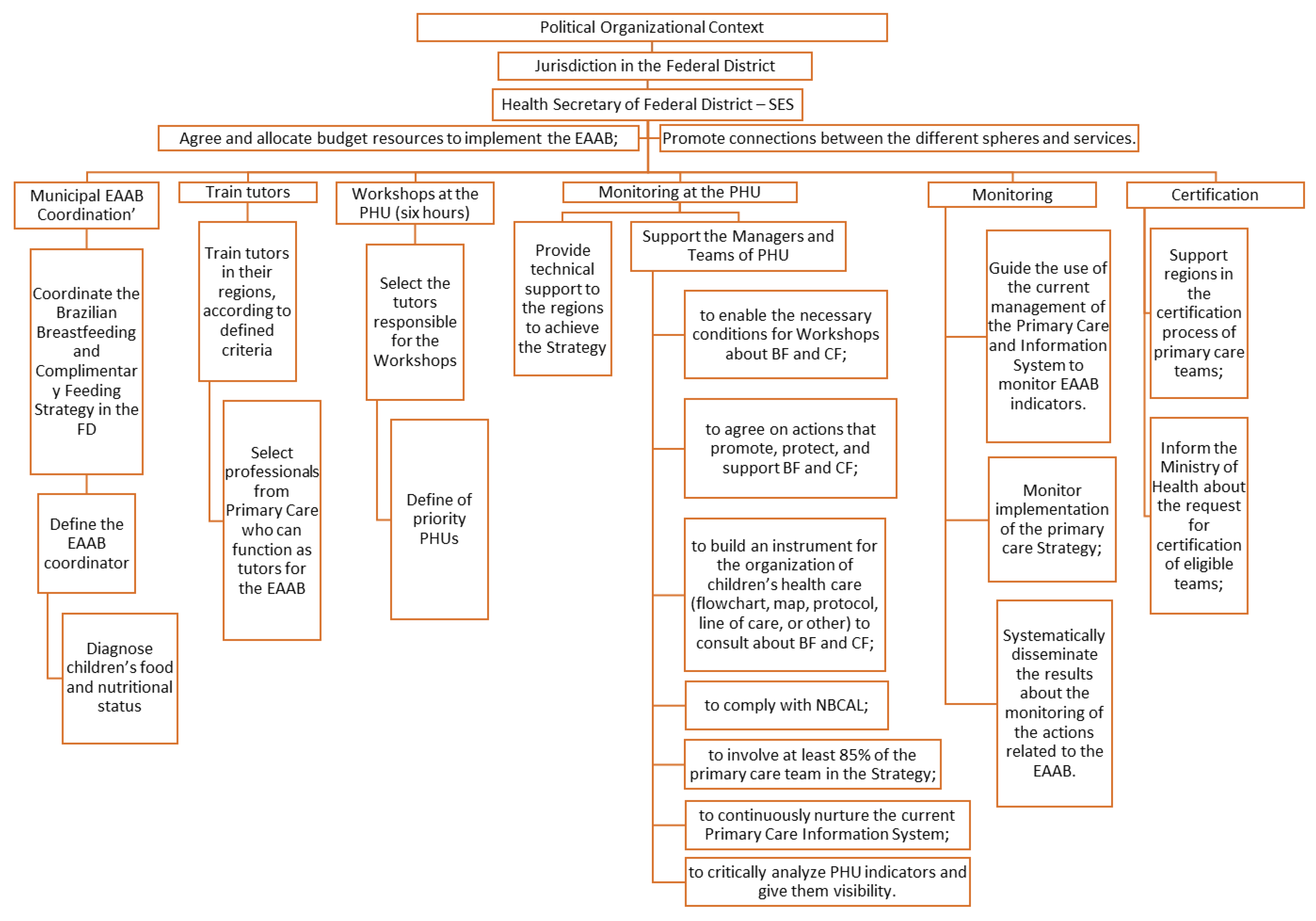
2.3.1. Create the Conceptual Logical Model of the EAAB in the FD
2.3.2. Evaluate the Organizational Context
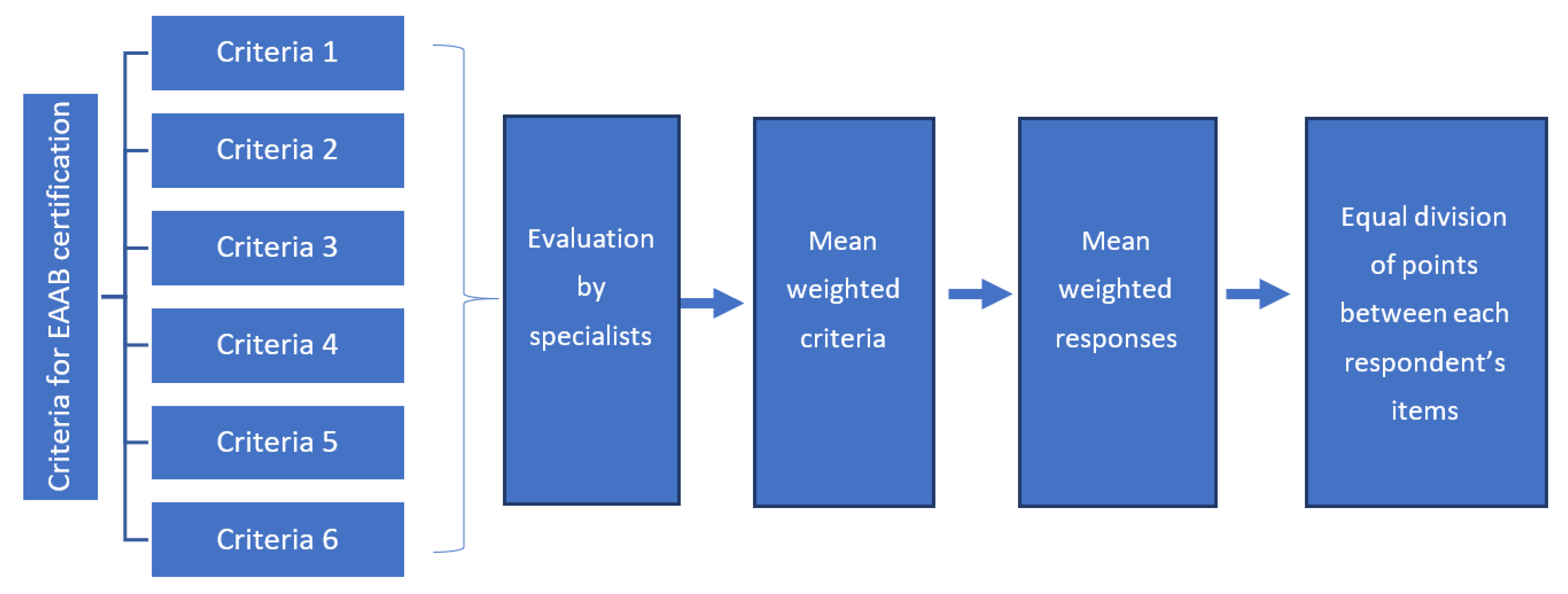
2.3.3. Evaluate the Degree of Implementation of the EAAB in the Health Units
2.3.4. Analyze the Influence of the Organizational Context on the Degree of Implementation
3. Results
3.1. Logical Model of the EAAB Implementation
3.2. Organizational Context of the EAAB in the Federal District
3.3. Degree of the EAAB Implementation in the Federal District
3.4. Influence of Organizational Context on the Degree of Implementation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Infant and Young Child Feeding: A Tool for Assessing National Practices, Policies and Programmes; World Health Organization: Geneva, Switzerland, 2003; ISBN 92-4-156254-4. [Google Scholar]
- Ministry of Health of Brazil. Child Health: Breastfeeding and Complementary Feeding, 2nd ed.; Ministry of Health of Brazil: Brasília, Brazil, 2015; ISBN 978-85-334-2290-2.
- Ministry of Health of Brazil. Dietary Guidelines for Brazilian Children under 2 Years of Age, 1st ed.; Ministry of Health of Brazil: Brasília, Brazil, 2019; ISBN 978-65-5993-020-3.
- Horta, B.L.; Victora, C.G.; World Health Organization. Short-Term Effects of Breastfeeding: A Systematic Review on the Benefits of Breastfeeding on Diarrhoea and Pneumonia Mortality; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-4-150612-0. [Google Scholar]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Long-Term Consequences of Breastfeeding on Cholesterol, Obesity, Systolic Blood Pressure and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Bartick, M.C.; Jegier, B.J.; Green, B.D.; Schwarz, E.B.; Reinhold, A.G.; Stuebe, A.M. Disparities in Breastfeeding: Impact on Maternal and Child Health Outcomes and Costs. J. Pediatr. 2017, 181, 49–55.e6. [Google Scholar] [CrossRef]
- Ministry of Health of Brazil. National Policy for Food and Nutrition, 1st ed.; Ministry of Health of Brazil: Brasília, Brazil, 2013; ISBN 978-85-334-1911-7.
- Ministry of Health of Brazil. National Policy on Integral Attention to the Health of the Child, 1st ed.; Ministry of Health of Brazil: Brasília, Brazil, 2018; ISBN 978-85-334-2596-5.
- Ministry of Health of Brazil. Basis for the Discussion of the National Policy for the Promotion, Protection and Support of Breastfeeding; Ministry of Health of Brazil: Brasília, Brazil, 2017; ISBN 978-85-334-2531-6.
- Federal University of Rio de Janeiro. Breastfeeding: Prevalence and Practices of Breastfeeding in Brazilian Children under 2 Years of Age; Federal University of Rio de Janeiro: Rio de Janeiro, Brazil, 2021. [Google Scholar]
- World Health Organization. Organization Guideline: Counselling of Women to Improve Breastfeeding Practices; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-4-155046-8. [Google Scholar]
- Vitolo, M.R.; Bortolini, G.A.; Campagnolo, P.D.B.; Hoffman, D.J. Maternal Dietary Counseling Reduces Consumption of Energy-Dense Foods among Infants: A Randomized Controlled Trial. J. Nutr. Educ. Behav. 2012, 44, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, L.O.; Vicente, A.S.T.; Damião, J.J.; Rito, R.V.V.F. The Impact of Implementation of the Breastfeeding Friendly Primary Care Initiative on the Prevalence Rates of Breastfeeding and Causes of Consultations at a Basic Healthcare Center. J. Pediatr. (Rio J.) 2008, 84, 147–153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McFadden, A.; Siebelt, L.; Marshall, J.L.; Gavine, A.; Girard, L.-C.; Symon, A.; MacGillivray, S. Counselling Interventions to Enable Women to Initiate and Continue Breastfeeding: A Systematic Review and Meta-Analysis. Int. Breastfeed. J. 2019, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Brazil. Establishes the National Strategy for Promotion of Breastfeeding and Healthy Complementary Feeding in the Brazilian Health System (SUS/Brazil); Ministry of Health of Brazil: Brasília, Brazil, 2013.
- Ministry of Health of Brazil. National Strategy for Promotion of Breastfeeding and Healthy Complementary Feeding in the Brazilian Health System (SUS/Brazil): Implementation Guide; Ministry of Health of Brazil: Brasília, Brazil, 2015; ISBN 978-85-334-2215-5.
- Ministry of Health of Brazil. Information and Management of Primary Care. EAAB System; Ministry of Health of Brazil: Brasília, Brazil, 2012.
- Ministry of Health of Brazil. Brazil Breastfeeding Network: First Steps (2007–2010); Ministry of Health of Brazil: Brasília, Brazil, 2011.
- Venâncio, S.I.; Martins, M.C.N.; Sanches, M.T.C.; de Almeida, H.; Rios, G.S.; de Frias, P.G. Deployment Analysis of the Brazilian Breastfeeding Network: Challenges and Prospects for Promoting Breastfeeding in Primary Care. Cad. Saúde Pública 2013, 29, 2261–2274. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Brazil. Deployment Analysis of the Breastfeeding Network Brazil: Research Report; Ministry of Health of Brazil: Brasília, Brazil, 2013; ISBN 978-85-334-2014-4.
- Bonini, T.d.P.L. Evaluation of the Degree of Implantation and the Effects Observed in the Brazilian Breastfeeding and Feeding Strategy in the Family Health Units of Piracicaba/SP. Ph.D. Thesis. University of State Campinas, Piraciacaba, Brazil, 2019. [Google Scholar]
- Mariot, M.D.M.; do Espirito Santo, L.C.; Riegel, F. Implementation of the Strategy Breastfeeds and Feeds Brazil: Tutors’ Perceptions. Rev. Enferm. 2020, 9, 4. [Google Scholar] [CrossRef]
- Brazilian Institute of Geography and Statistics. IBGE—Brazilian Institute of Geography and Statistics; IBGE: Brasilia, Brazil, 2010. [Google Scholar]
- IBGE—Brazilian Institute of Geography and Statistics. Coordination of Population and Social Indicators. Synthesis of Social Indicators: An Analysis of the Living Conditions of the Brazilian Population; IBGE: Brasilia, Brazil, 2019. [Google Scholar]
- CODEPLAN—Planning Company of the Federal District. District Household Sample Survey; CODEPLAN: Brasilia, Brazil, 2018. [Google Scholar]
- Ministry of Health of Brazil. Live Birth Monitoring Panel; Ministry of Health of Brazil: Brasília, Brazil, 2018.
- Yin, R.K. Case Study Research: Design and Methods, 2nd ed.; Bookman: Porto Alegre, Brazil, 2001; ISBN 85-7307-852-9. [Google Scholar]
- Hartz, Z.M.d.A. Health Evaluation: From Conceptual Models to Practice in the Analysis of Program Implementation; Editora FIOCRUZ: Rio de Janeiro, Brazil, 1997; ISBN 978-85-7541-403-3. [Google Scholar]
- Ministry of Health of Brazil. Instruction for the Implementation Plan of the Brazilian Breastfeeding and Feeding Strategy; Ministry of Health of Brazil: Brasília, Brazil, 2015.
- Matus, C. Triangle of Government. In Politics, Planning and Government; Instituto de Pesquisa Econômica Aplicada—IPEA: Brasília, Brazil, 1993; Volume 2, p. 591. [Google Scholar]
- Melo, D.S. Implementation Process of the Brazilian Breastfeeding and Feeding Strategy: An Analysis of the Program’s Impact Path; University of São Paulo: São Paulo, Brazil, 2020. [Google Scholar]
- Tavares, J.S.; Vieira, D.d.S.; Dias, T.K.C.; Tacla, M.T.G.M.; Collet, N.; Reichert, A.P.d.S. Logframe Model as Analytical Tool for the Brazilian Breastfeeding and Feeding Strategy. Rev. Nutr. 2018, 31, 251–262. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Curry, L.; Minhas, D.; Taylor, L.; Bradley, E. Scaling Up of Breastfeeding Promotion Programs in Low- and Middle-Income Countries: The “Breastfeeding Gear” Model. Adv. Nutr. 2012, 3, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.S.; Cherchiglia, M.L.; César, C.C. The Food and Nutrition Surveillance System as a Tool for Monitoring the National Strategy for Healthy Complementary Nutrition. Rev. Bras. Saúde Materno Infant. 2013, 13, 167–177. [Google Scholar] [CrossRef]
- Rolim, M.D.; Lima, S.M.L.; de Barros, D.C.; de Andrade, C.L.T. Evaluation of the Food and Nutrition Surveillance System (SISVAN) in Food and Nutritional Management Services in the State of Minas Gerais, Brazil. Ciênc. Saúde Coletiva 2015, 20, 2359–2369. [Google Scholar] [CrossRef] [PubMed]
- Passanha, A.; Da Benicio, M.H.; Venancio, S.I.; dos Reis, M.C.G. Implementation of the Brazilian Breastfeeding Network and Prevalence of Exclusive Breastfeeding. Rev. Saúde Pública 2013, 47, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Venancio, S.I.; Giugliani, E.R.J.; Silva, O.L.d.O.; Stefanello, J.; Benicio, M.H.D.; dos Reis, M.C.G.; Issler, R.M.S.; Santo, L.C.d.E.; Cardoso, M.R.A.; Rios, G.S. Association between the Degree of Implementation of the Brazilian Breastfeeding Network and Breastfeeding Indicators. Cad. Saúde Pública 2016, 32. [Google Scholar] [CrossRef]
| Respondent | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mother | Professional | Manager | Coordinator | |||||||
| N° Criterion | Criterion Name | Score on the Criterion | N° of Items | Score on Item | N° of Items | Score on Item | N° of Items | Score on Item | N° of Items | Score on Item |
| 1 | Develop individual or collective systematic actions to promote breastfeeding and complementary feeding | 18 | 3 | 2.3 | 5 | 1.2 | 5 | 1 | ||
| 2 | Monitor breastfeeding and complementary feeding rates | 18 | 1 | 7 | 1 | 6 | 1 | 5 | ||
| 3 | Provide an instrument for child health care organization (flowchart, map, protocol, line of care, or other) to detect problems related to breastfeeding and complementary feeding | 16 | 7 | 0.57 | 8 | 0.75 | 9 | 0.66 | ||
| 4 | Comply with the Brazilian Guidelines for the Marketing of Food for Infants and Young Children, Nipples, Pacifiers, and Bottles (NBCAL) and with Law No. 11,265 of 2006, and do not distribute “substitutes” for breast milk at the PHU | 16 | 5 | 1.2 | 5 | 1.2 | 1 | 4 | ||
| 5 | Count on the participation of at least 85% of the team’s professionals in the developed workshops | 17 | 1 | 9 | 1 | 8 | ||||
| 6 | Fulfill at least one breastfeeding action and one complementary feeding action established in the action plan | 15 | 3 | 2.66 | 3 | 2.3 | ||||
| TOTAL | 100 | |||||||||
| Categories | Indicators | Federal District |
|---|---|---|
| Government Project | Primary Care as a priority—ESF Coverage 1 | less than 50% |
| Breastfeeding and complementary feeding as a priority in policy/legislation or guideline 2 | Law 5374/2014 about the District Policy on BF and the promotion in primary health care of actions to promote, protect, and support breastfeeding and healthy complementary feeding. | |
| Interest in implementing the EAAB 1 | “The PHU manager needs to ‘buy into the idea’, be a partner. He needs to be convinced of the importance of the EAAB for the PHU and the population.” | |
| Receptivity of EAAB in the governmental sphere 2 | “Positive reception. They tried to adapt but maintain the 40 h for the tutor training workshop at EAAB. They left more time for discussion (maintained the training of tutors with a higher workload even though the Ministry of Health had reduced it)” | |
| Competition of EAAB with other priorities 1 | “The health system still works on the logic of disease and not health promotion. The PHU manager is more concerned with spontaneous demand than with health promotion activities for breastfeeding and healthy complementary feeding. The PHU manager needs to understand that the EAAB is important.” | |
| Existence of activities, actions, and/or programs complementary to EAAB 2 | 40-hour breastfeeding counseling course (held in May and August since 2016) in all health regions. A total of 132 professionals were trained in the first semester of 2019. Trains professionals from State Secretary of Health of Federal District (SES), universities, and the supplementary network. Mobilization of Breastmilk Donation Day, District Law for Breastmilk Donation Week, District Law for Golden August. Mobilization of Golden August. Opening of events in partnership with the judicial system, breastfeeding seminars (since 2016). Two seminars for two groups (650 participants in 2018). May: communication mobilization, Amamenta Brasília website, Facebook, application, breast milk donation system, telephone, local events in all HMBs; in August, mobilization in the 7 health regions, where there are HMBs in the region, also participates in the mobilization of World Breastfeeding week (WBW). D-day of breastfeeding. Discussion about NBCAL at an event, film screenings, seminars. 40-hour breastfeeding courses for primary care. | |
| Specific financial resource for EAAB 1 | “There is no specific resource. Funds from lawmakers. SES Funding. Stork Network resource, own resources of SES workers.” | |
| Government Capacity | Existence of an area for Children’s Health 2 | Coordination of Breastfeeding Policies in the FD |
| Existence of EAAB Coordinator or breastfeeding and complementary feeding actions 2 | “Yes, coordinator of breastfeeding policies for the FD” | |
| Stability of the person responsible for breastfeeding actions and healthy complementary feeding (bonded) 2 | Public servant | |
| Professional experience of the person responsible for breastfeeding and healthy complementary feeding actions 2 | 11 years of experience in the position coordinating breastfeeding policies, technical experience in the subject of children’s health, breastfeeding, and complementary feeding. | |
| Institutional functions of EAAB managers compatible with the organizational chart 2 | Pediatrician—coordinator of the breastfeeding policies in the FD | |
| Use of management technologies (periodic meetings about the EAAB, regular contact with tutors and PHU teams, use of the EAAB management system) 1 | “There were monthly meetings that no longer happen with the change in the structure of the SES. Access the EAAB system but reports that few tutors enter information.” | |
| System Governability | Coordination with other areas and/or spheres of government to implement the EAAB 2 | “There is coordination with the Board of the Family Health Strategy and GESNUT (Management of Nutrition Services).” |
| Operationalization of the implementation of the EAAB 2 | Workshop to train tutors trying to cover all health regions, tutors with profiles became workshop facilitators, and others were only trained without acting as tutors. | |
| Support to PHU for the development of actions (monitoring of BF and CF indicators, compliance with NBCAL) 1 | Professional training calendar “Counseling–40 h in May and August (primary care, supplementary, and university) by region. B-course taken in hospitals—24 h (hospital management and counseling) NBCAL—course for professionals (1 course in the last three years) BFHI and CF course in 2018 for breastfeeding professionals. “The monitoring data of breastfeeding and complementary feeding indicators come from surveys (prevalence of 2008), 2014-pilot by telephone. 2016/2017–Project “Early Childhood for Healthy Adults” (PIPAS). e-SUS (entered as an electronic medical record in PHC in 2017/2018, but there is still resistance in filling in part of the PHU servers. The Health Regions must have followed the indicators of compulsorily BF by the SES since 2010. Collection of human milk is also monitored by the SES.” “Local data from recent dietary prevalence surveys? Surveys (2008 prevalence), 2014–telephone pilot. 2016/2017–PIPAS” On the distribution of milk and baby formula in the PHU: “No. Only in the STD/AIDS Reference Units (HIV and HTLV patients)–screening since 2012, an average of 35 women per year diagnosed with HTLV. Children with food allergy (central pharmacy).” | |
| Adherence of the actors involved 1 | “Tutor is not institutional; the manager does not always allow the professional to do the activities of a tutor. Complaint of the tutor “how can the tutor’s workload be made official?” “The PHU manager needs to ‘buy into the idea’(resistant to the EAAB proposal), be a partner. He needs to be convinced of the importance of the EAAB for PHUs and the population.” |
| PHU 1 | PHU 2 | PHU 3 | PHU 4 | PHU 5 | PHU 6 | |
|---|---|---|---|---|---|---|
| Criteria 1 | 61.7 2 | 61.7 2 | 61.7 2 | 74.4 2 | 49.4 3 | 61.7 2 |
| Criteria 2 | 66.7 2 | 61.1 2 | 27.8 3 | 100 1 | 100 1 | 100 1 |
| Criteria 3 | 78.7 2 | 78.7 2 | 61.2 2 | 78.1 2 | 82.5 1 | 78.7 2 |
| Criteria 4 | 85 1 | 100 1 | 100 1 | 85 1 | 85 1 | 70 2 |
| Criteria 5 | 0 4 | 100 1 | 100 1 | 100 1 | 0 4 | 100 1 |
| Criteria 6 | 46.7 3 | 100 1 | 34 3 | 0 4 | 0 4 | 46.7 3 |
| TOTAL | 56.3 2 | 82.7 1 | 63.9 2 | 74.6 2 | 53.8 2 | 76.9 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moura, A.S.; Gubert, M.B.; Venancio, S.I.; Buccini, G. Implementation of the Strategy for Breastfeeding and Complementary Feeding in the Federal District in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 5003. https://doi.org/10.3390/ijerph19095003
Moura AS, Gubert MB, Venancio SI, Buccini G. Implementation of the Strategy for Breastfeeding and Complementary Feeding in the Federal District in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(9):5003. https://doi.org/10.3390/ijerph19095003
Chicago/Turabian StyleMoura, Amanda Souza, Muriel Bauermann Gubert, Sonia Isoyama Venancio, and Gabriela Buccini. 2022. "Implementation of the Strategy for Breastfeeding and Complementary Feeding in the Federal District in Brazil" International Journal of Environmental Research and Public Health 19, no. 9: 5003. https://doi.org/10.3390/ijerph19095003
APA StyleMoura, A. S., Gubert, M. B., Venancio, S. I., & Buccini, G. (2022). Implementation of the Strategy for Breastfeeding and Complementary Feeding in the Federal District in Brazil. International Journal of Environmental Research and Public Health, 19(9), 5003. https://doi.org/10.3390/ijerph19095003







