Risk of Hypertension and Type 2 Diabetes in Relation to Changes in Alcohol Consumption: A Nationwide Cohort Study
Abstract
1. Introduction
2. Methods
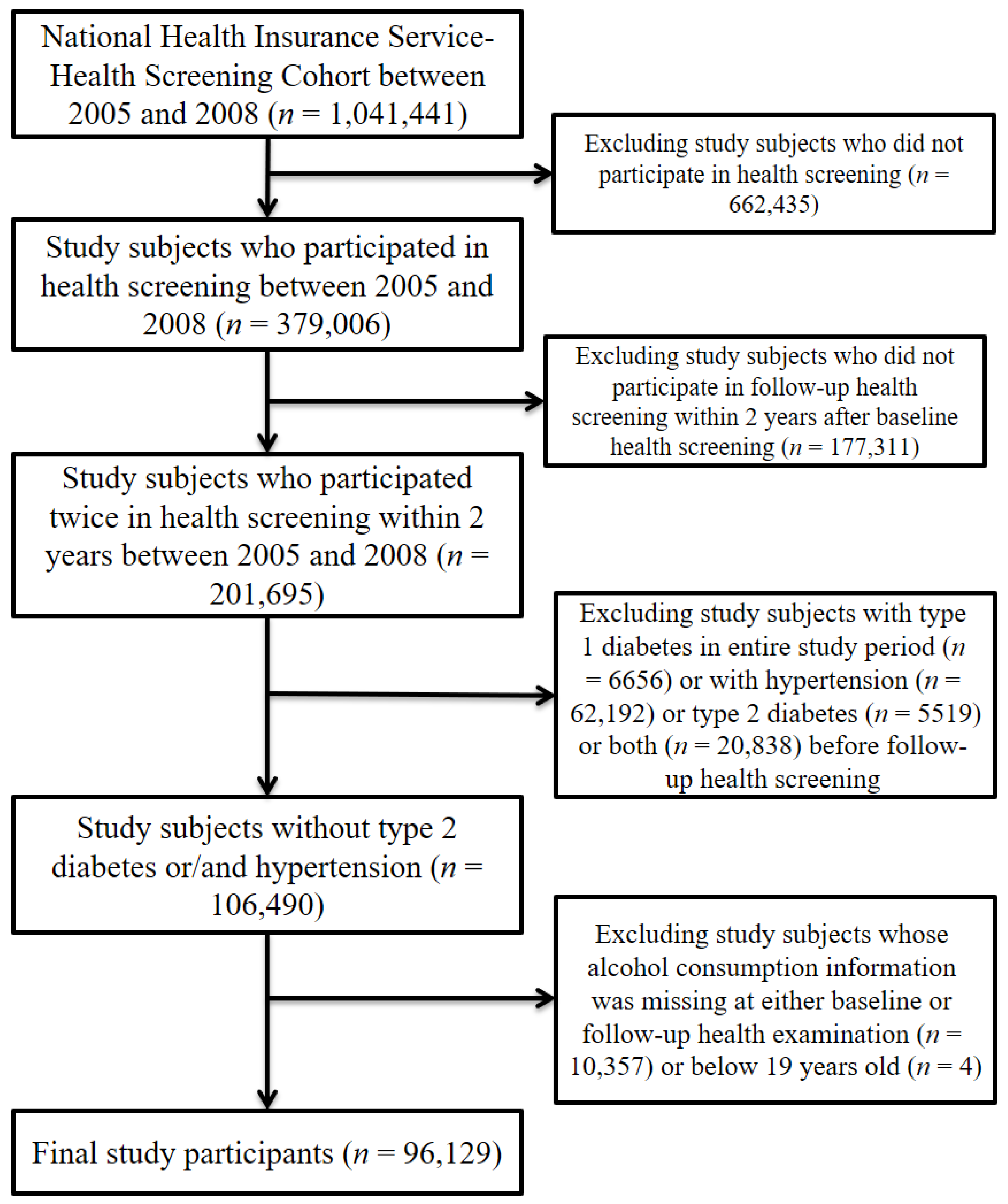
2.1. Data and Study Sample
2.2. Measurements for Hypertension and Type 2 Diabetes
2.3. Measurements for Alcohol Consumption
2.4. Measurement for Potential Confounding Factors
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shin, S.; Bai, L.; Oiamo, T.H.; Burnett, R.T.; Weichenthal, S.; Jerrett, M.; Kwong, J.C.; Goldberg, M.S.; Copes, R.; Kopp, A.; et al. Association Between Road Traffic Noise and Incidence of Diabetes Mellitus and Hypertension in Toronto, Canada: A Population-Based Cohort Study. J. Am. Heart Assoc. 2020, 9, e013021. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies from 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Pigeyre, M.; Sjaarda, J.; Chong, M.; Hess, S.; Bosch, J.; Yusuf, S.; Gerstein, H.; Pare, G. ACE and Type 2 Diabetes Risk: A Mendelian Randomization Study. Diabetes Care 2020, 43, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.B.D.R.F.; Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar]
- Noubiap, J.J.; Nansseu, J.R.; Nyaga, U.F.; Sime, P.S.; Francis, I.; Bigna, J.J. Global prevalence of resistant hypertension: A meta-analysis of data from 3.2 million patients. Heart 2019, 105, 98–105. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 28 March 2022).
- Ciarambino, T.; Ciaburri, F.; Paoli, V.D.; Caruso, G.; Giordano, M.; D’Avino, M. Arterial Hypertension and Diabetes Mellitus in COVID-19 Patients: What Is Known by Gender Differences? J. Clin. Med. 2021, 10, 3740. [Google Scholar] [CrossRef]
- Room, R.; Babor, T.; Rehm, J. Alcohol and public health. Lancet 2005, 365, 519–530. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, H.J. Trends in Alcohol Consumption for Korean Adults from 1998 to 2018: Korea National Health and Nutritional Examination Survey. Nutrients 2021, 13, 609. [Google Scholar] [CrossRef]
- Ricci, C.; Schutte, A.E.; Schutte, R.; Smuts, C.M.; Pieters, M. Trends in alcohol consumption in relation to cause-specific and all-cause mortality in the United States: A report from the NHANES linked to the US mortality registry. Am. J. Clin. Nutr. 2020, 111, 580–589. [Google Scholar] [CrossRef]
- Okubo, Y.; Sairenchi, T.; Irie, F.; Yamagishi, K.; Iso, H.; Watanabe, H.; Muto, T.; Tanaka, K.; Ota, H. Association of alcohol consumption with incident hypertension among middle-aged and older Japanese population: The Ibarakai Prefectural Health Study (IPHS). Hypertension 2014, 63, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Yoo, M.G.; Park, K.J.; Kim, H.J.; Jang, H.B.; Lee, H.J.; Park, S.I. Association between alcohol intake and incident hypertension in the Korean population. Alcohol 2019, 77, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.J.; Hu, H.Y.; Lee, Y.L.; Ko, M.C.; Ku, P.W.; Yen, Y.F.; Chu, D. Frequency of alcohol consumption and risk of type 2 diabetes mellitus: A nationwide cohort study. Clin. Nutr. 2019, 38, 1368–1372. [Google Scholar] [CrossRef] [PubMed]
- Peng, M.; Zhang, J.; Zeng, T.; Hu, X.; Min, J.; Tian, S.; Wang, Y.; Liu, G.; Wan, L.; Huang, Q.; et al. Alcohol consumption and diabetes risk in a Chinese population: A Mendelian randomization analysis. Addiction 2019, 114, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Knott, C.; Bell, S.; Britton, A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015, 38, 1804–1812. [Google Scholar] [CrossRef]
- Briasoulis, A.; Agarwal, V.; Messerli, F.H. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J. Clin. Hypertens. 2012, 14, 792–798. [Google Scholar] [CrossRef]
- Tsubono, Y.; Yamada, S.; Nishino, Y.; Tsuji, I.; Hisamichi, S. Choice of comparison group in assessing the health effects of moderate alcohol consumption. JAMA 2001, 286, 1177–1178. [Google Scholar] [CrossRef]
- Chikritzhs, T.; Fillmore, K.; Stockwell, T. A healthy dose of scepticism: Four good reasons to think again about protective effects of alcohol on coronary heart disease. Drug. Alcohol. Rev. 2009, 28, 441–444. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch. Intern. Med. 2006, 166, 2437–2445. [Google Scholar] [CrossRef]
- Jung, S.; Kim, M.K.; Shin, J.; Lee, N.; Woo, H.W.; Choi, B.Y.; Shin, M.H.; Shin, D.H.; Lee, Y.H. Positive association of alcohol consumption with incidence of hypertension in adults aged 40 years and over: Use of repeated alcohol consumption measurements. Clin. Nutr. 2020, 39, 3125–3131. [Google Scholar] [CrossRef]
- Lui, C.K.; Kerr, W.C.; Li, L.; Mulia, N.; Ye, Y.; Williams, E.; Greenfield, T.K.; Lown, E.A. Lifecourse Drinking Patterns, Hypertension, and Heart Problems Among U.S. Adults. Am. J. Prev. Med. 2020, 58, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Joosten, M.M.; Chiuve, S.E.; Mukamal, K.J.; Hu, F.B.; Hendriks, H.F.; Rimm, E.B. Changes in alcohol consumption and subsequent risk of type 2 diabetes in men. Diabetes 2011, 60, 74–79. [Google Scholar] [CrossRef][Green Version]
- He, X.; Rebholz, C.M.; Daya, N.; Lazo, M.; Selvin, E. Alcohol consumption and incident diabetes: The Atherosclerosis Risk in Communities (ARIC) study. Diabetologia 2019, 62, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Zhang, S.; Duan, W.; Ren, X.; Wei, C.; Sun, C.; Li, Y. Eighteen-year alcohol consumption trajectories and their association with risk of type 2 diabetes and its related factors: The China Health and Nutrition Survey. Diabetologia 2019, 62, 970–980. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, T.H.; Han, E. Smoking Cessation, Weight Change, Diabetes, and Hypertension in Korean Adults. Am. J. Prev. Med. 2021, 60, 205–212. [Google Scholar] [CrossRef]
- Lee, C.H.; Han, K.D.; Yoo, J.; Kwak, M.S. Synergistic harmful interaction between sustained physical inactivity and hypertension/diabetes mellitus on the risk of all-cause mortality: A retrospective observational cohort study. J. Hypertens. 2021, 39, 2058–2066. [Google Scholar] [CrossRef]
- Seong, S.C.; Kim, Y.Y.; Park, S.K.; Khang, Y.H.; Kim, H.C.; Park, J.H.; Kang, H.J.; Do, C.H.; Song, J.S.; Lee, E.J.; et al. Cohort profile: The National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 2017, 7, e016640. [Google Scholar] [CrossRef]
- US Department of Health Human Services. NIAAA council approves definition of binge drinking. NIAAA Newsl. 2004, 3, 3. [Google Scholar]
- Joo, Y.S.; Koh, H.; Nam, K.H.; Lee, S.; Kim, J.; Lee, C.; Yun, H.R.; Park, J.T.; Kang, E.W.; Chang, T.I.; et al. Alcohol Consumption and Progression of Chronic Kidney Disease: Results From the Korean Cohort Study for Outcome in Patients with Chronic Kidney Disease. Mayo Clin. Proc. 2020, 95, 293–305. [Google Scholar] [CrossRef]
- WHO Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Marchi, K.C.; Muniz, J.J.; Tirapelli, C.R. Hypertension and chronic ethanol consumption: What do we know after a century of study? World J. Cardiol. 2014, 6, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Baer, D.J.; Judd, J.T.; Brown, E.D.; Campbell, W.S.; Taylor, P.R. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women: A randomized controlled trial. JAMA 2002, 287, 2559–2562. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, F.; Disse, E.; Laville, M.; Mari, A.; Hojlund, K.; Anderwald, C.H.; Piatti, P.; Balkau, B.; Group, R.S. Moderate alcohol consumption is associated with improved insulin sensitivity, reduced basal insulin secretion rate and lower fasting glucagon concentration in healthy women. Diabetologia 2012, 55, 3228–3237. [Google Scholar] [CrossRef]
- Fan, A.Z.; Russell, M.; Dorn, J.; Freudenheim, J.L.; Nochajski, T.; Hovey, K.; Trevisan, M. Lifetime alcohol drinking pattern is related to the prevalence of metabolic syndrome. The Western New York Health Study (WNYHS). Eur. J. Epidemiol. 2006, 21, 129–138. [Google Scholar] [CrossRef]
- Korea Institute for Health and Social Affairs. The Fifth Korea National Health and Nutrition Examination Survey (KNHANES V), 2011—Health Behaviors of Adults; Korea Institute for Health and Social Affairs: Yeongi-gun, Korea, 2012. [Google Scholar]


| Variables | Baseline Health Screening (2005–2007) | Follow-Up Health Screening (2006–2008) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Total | 96,129 | 100.0 | 96,129 | 100.0 | |
| Status of alcohol consumption | |||||
| Nondrinking | 48,506 | 50.5 | 47,758 | 49.7 | |
| Occasional moderate drinking | 15,486 | 16.1 | 15,453 | 16.1 | |
| Frequent moderate drinking | 429 | 0.4 | 470 | 0.5 | |
| Occasional binge drinking | 30,532 | 31.8 | 31,199 | 32.5 | |
| Frequent binge drinking | 1176 | 1.2 | 1249 | 1.3 | |
| Men | 50,298 | 52.3 | 50,298 | 52.3 | |
| Age (years), mean ± SD | 41.3 | 12.8 | 42.8 | 13.0 | |
| BMI (kg/m2) | |||||
| ≤18.5 | 5162 | 5.4 | 4917 | 5.1 | |
| 18.5–23 | 44,824 | 46.6 | 43,841 | 45.6 | |
| 23–25 | 22,741 | 23.7 | 22,860 | 23.8 | |
| 25–30 | 21,592 | 22.5 | 22,454 | 23.4 | |
| ≥30 | 1796 | 1.9 | 2046 | 2.1 | |
| SBP (mm Hg), mean ± SD | 117.1 | 12.9 | 117.4 | 12.8 | |
| DBP (mm Hg), mean ± SD | 73.3 | 8.8 | 73.3 | 8.7 | |
| Fasting glucose (mg/dL), mean ± SD | 89.9 | 13.4 | 91.0 | 13.7 | |
| Total cholesterol (mg/dL), mean ± SD | 188.7 | 35.2 | 190.1 | 36.4 | |
| Smoking status | |||||
| Nonsmoking | 63,408 | 66.0 | 63,750 | 66.3 | |
| Ex-smoking | 7925 | 8.2 | 8038 | 8.4 | |
| Current smoking | 23,904 | 24.9 | 23,681 | 24.6 | |
| Exercise | 44,262 | 46.0 | 46,154 | 48.0 | |
| Nutrition intake behaviors | |||||
| Meat as staple food | 6337 | 6.6 | 6269 | 6.5 | |
| Vegetables as staple food | 16,584 | 17.3 | 16,124 | 16.8 | |
| Mixed intake | 72,577 | 75.5 | 73,380 | 76.3 | |
| Household income | |||||
| Low | 32,951 | 34.3 | 28,726 | 29.9 | |
| Middle | 41,655 | 43.3 | 43,826 | 45.6 | |
| High | 21,523 | 22.4 | 23,577 | 24.5 | |
| Residential area | |||||
| Metropolitan | 18,153 | 18.9 | 18,057 | 18.8 | |
| Urban | 26,177 | 27.2 | 25,887 | 26.9 | |
| Rural | 51,799 | 53.9 | 52,185 | 54.3 | |
| Family history of diabetes | 6732 | 7.0 | 7434 | 7.7 | |
| Family history of hypertension | 7063 | 7.3 | 8148 | 8.5 | |
| Comorbidities | |||||
| Dyslipidemia | 10,979 | 11.4 | 15,305 | 15.9 | |
| Stroke | 1060 | 1.1 | 1544 | 1.6 | |
| Ischemic heart disease | 4133 | 4.3 | 5575 | 5.8 | |
| Cancer | 3086 | 3.2 | 4122 | 4.3 | |
| Variable | No. of Study Participants | Person-Years | Cases | HR | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Hypertension † | ||||||||
| Nondrinking | 48,506 | 367,181 | 16,142 | 1.00 | ||||
| Occasional moderate drinking | 15,486 | 122,348 | 4031 | 0.99 | 0.96 | 1.03 | 0.677 | |
| Frequent moderate drinking | 429 | 2695 | 242 | 1.01 | 0.88 | 1.16 | 0.917 | |
| Occasional binge drinking | 30,532 | 238,312 | 8016 | 1.11 | 1.07 | 1.15 | <0.001 | |
| Frequent binge drinking | 1176 | 7682 | 612 | 1.24 | 1.13 | 1.36 | <0.001 | |
| Type 2 diabetes ‡ | ||||||||
| Nondrinking | 48,506 | 406,556 | 10,514 | 1.00 | ||||
| Occasional moderate drinking | 15,486 | 131,642 | 2546 | 0.98 | 0.93 | 1.02 | 0.290 | |
| Frequent moderate drinking | 429 | 3236 | 185 | 0.98 | 0.83 | 1.15 | 0.798 | |
| Occasional binge drinking | 30,532 | 254,385 | 5086 | 1.10 | 1.06 | 1.15 | <0.001 | |
| Frequent binge drinking | 1176 | 8966 | 453 | 1.21 | 1.09 | 1.35 | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.W.; Han, E.; Kim, T.H. Risk of Hypertension and Type 2 Diabetes in Relation to Changes in Alcohol Consumption: A Nationwide Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 4941. https://doi.org/10.3390/ijerph19094941
Choi JW, Han E, Kim TH. Risk of Hypertension and Type 2 Diabetes in Relation to Changes in Alcohol Consumption: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(9):4941. https://doi.org/10.3390/ijerph19094941
Chicago/Turabian StyleChoi, Jae Woo, Euna Han, and Tae Hyun Kim. 2022. "Risk of Hypertension and Type 2 Diabetes in Relation to Changes in Alcohol Consumption: A Nationwide Cohort Study" International Journal of Environmental Research and Public Health 19, no. 9: 4941. https://doi.org/10.3390/ijerph19094941
APA StyleChoi, J. W., Han, E., & Kim, T. H. (2022). Risk of Hypertension and Type 2 Diabetes in Relation to Changes in Alcohol Consumption: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health, 19(9), 4941. https://doi.org/10.3390/ijerph19094941







