Translation and Validation of the Malay Version of the WHO-5 Well-Being Index: Reliability and Validity Evidence from a Sample of Type 2 Diabetes Mellitus Patients
Abstract
1. Introduction
1.1. The WHO-5 Well-Being Index
1.2. The Present Study and Hypotheses
2. Materials and Methods
2.1. Participants
2.2. Study Eligibility
2.3. Ethical and Translation Approval
2.4. Study Procedure
2.4.1. Phase 1: Translation of the WHO-5 Well-Being Index into Malay Language
2.4.2. Phase 2: Validation of the Malay Version of the WHO-5 Well-Being Index
2.5. Measures
2.5.1. The Malay Version of the WHO Well-Being Index
2.5.2. Depression
2.5.3. Emotional Problems
2.5.4. Diabetes Management Self-Efficacy
2.5.5. Diabetes Self-Care Behaviors
2.6. Data Analytic Plan
3. Results
3.1. Internal Consistency and Test–Retest Reliability
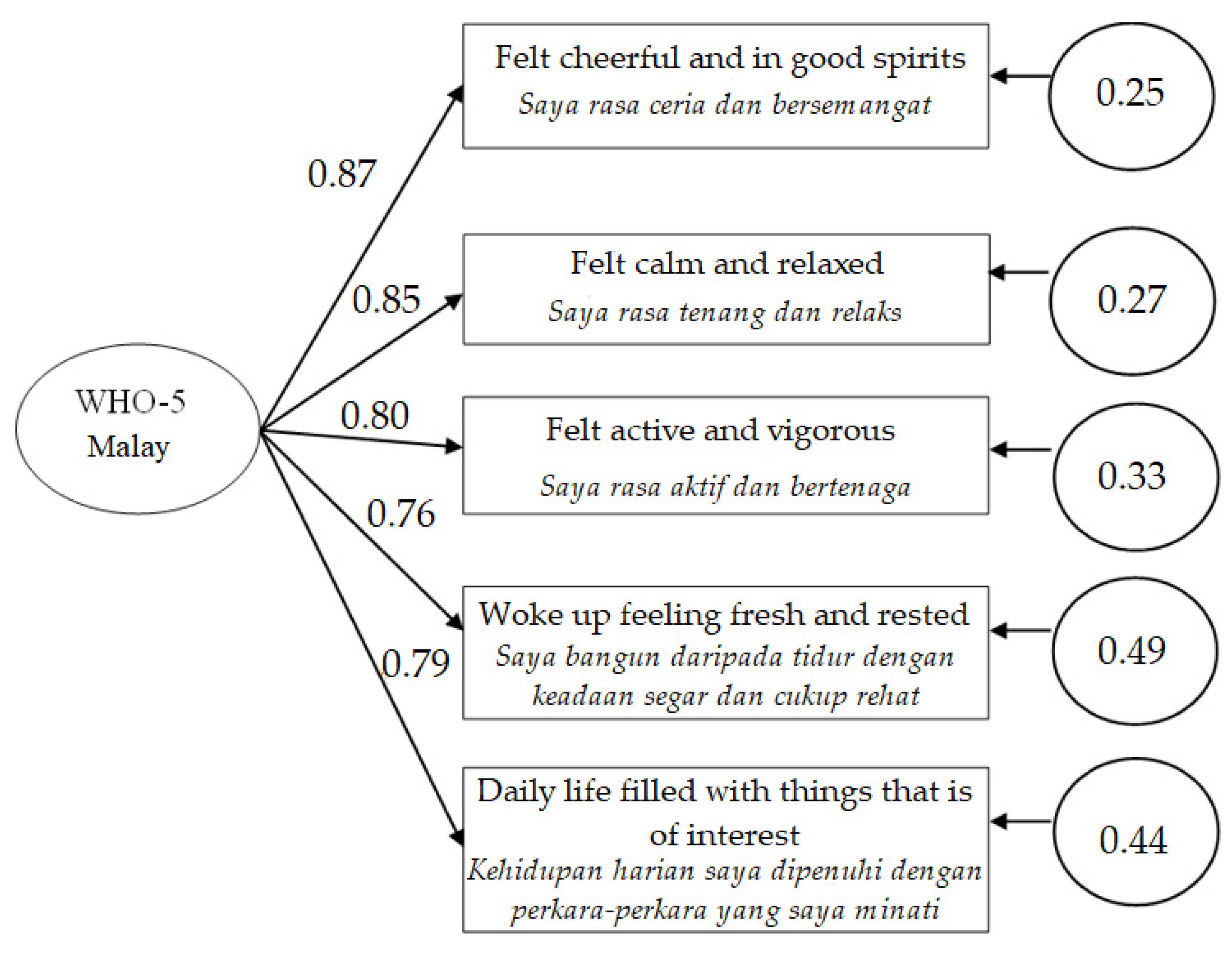
3.2. Factorial Validity
3.3. Concurrent Validity and Convergent Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Sabourin, B.C.; Pursley, S. Psychosocial issues in diabetes self-management: Strategies for healthcare providers. Can. J. Diabetes 2013, 37, 36–40. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peyrot, M.; Rubin, R.R.; Lauritzen, T.; Snoek, F.J.; Matthews, D.R.; Skovlund, S.E. Psychosocial problems and barriers to improved diabetes management: Results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet. Med. 2005, 22, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Chew, B.H.; Vos, R.; Mohd-Sidik, S.; Rutten, G.E.H.M. Diabetes-Related distress, depression and distress-depression among adults with type 2 diabetes mellitus in Malaysia. PLoS ONE 2016, 11, e0152095. [Google Scholar] [CrossRef]
- Kaur, G.; Tee, G.H.; Ariaratnam, S.; Krishnapillai, A.; China, K. Depression, anxiety and stress symptoms among diabetics in Malaysia: A cross sectional study in an urban primary care setting. BMC Fam. Pract. 2013, 14, 69. [Google Scholar] [CrossRef]
- Tan, K.C.; Chan, G.C.; Eric, H.; Maria, A.I.; Norliza, M.J.; Oun, B.H.; Sheerine, M.T.; Wong, S.J.; Liew, S.M. Depression, anxiety and stress among patients with diabetes in primary care: A cross-sectional study. Malays. Fam. Physician 2015, 10, 9–21. [Google Scholar]
- Fiore, V.; Marci, M.; Poggi, A.; Giagulli, V.A.; Licchelli, B.; Iacoviello, M.; Guastamacchia, E.; DE Pergola, G.; Triggiani, V. The association between diabetes and depression: A very disabling condition. Endocrine 2015, 48, 14–24. [Google Scholar] [CrossRef]
- Paduch, A.; Kuske, S.; Schiereck, T.; Droste, S.; Loerbroks, A.; Sørensen, M.; Maggini, M.; Icks, A. Psychosocial barriers to healthcare use among individuals with diabetes mellitus: A systematic review. Prim. Care Diabetes 2017, 11, 495–514. [Google Scholar] [CrossRef]
- Nicolucci, A.; Kovacs Burns, K.; Holt, R.I.G.; Comaschi, M.; Hermanns, N.; Ishii, H.; Kokoszka, A.; Pouwer, F.; Skovlund, S.E.; Stuckey, H.; et al. Diabetes attitudes, wishes and needs second study (DAWN2TM): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet. Med. 2013, 30, 767–777. [Google Scholar] [CrossRef]
- Tan, M.Y.; Magarey, J.M.; Chee, S.S.; Lee, L.F. A brief structured education programme enhances self-care practices and improves glycaemic control in Malaysians with poorly controlled diabetes. Health Educ. Res. 2011, 26, 896–907. [Google Scholar] [CrossRef]
- Hussein, Z.; Taher, S.W.; Kaur, H.; Singh, G.; Chee, W.; Swee, S. Diabetes care in Malaysia: Problems, new models, and solutions. Ann. Glob. Health 2015, 81, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Ooi, C.P.; Loke, S.C.; Zaiton, A.; Tengku-Aizan, H.; Zaitun, Y. Cross-sectional study of older adults with type 2 diabetes mellitus in two rural public primary healthcare facilities in Malaysia. Med. J. Malays. 2011, 66, 108–112. [Google Scholar]
- Winkley, K.; Upsher, R.; Stahl, D.; Pollard, D.; Kasera, A.; Brennan, A.; Heller, S.; Ismail, K. Psychological interventions to improve self-management of type 1 and type 2 diabetes: A systematic review. Health Technol. Assess. 2020, 24, 1–232. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, M.C.; Thompson, D.R.; Castle, D.J.; Jenkins, Z.M.; Ski, C. Psychosocial interventions and wellbeing in individuals with diabetes mellitus: A systematic review and meta-analysis. Front. Psychol. 2017, 8, 2063. [Google Scholar] [CrossRef]
- Stuifbergen, A.K.; Morris, M.; Jung, J.H.; Pierini, D.; Morgan, S. Benefits of wellness interventions for persons with chronic and disabling conditions: A review of the evidence. Disabil. Health J. 2010, 3, 133–145. [Google Scholar] [CrossRef]
- Yap, C.C.; Tam, C.L.; Muniyandy, S.; Kadirvelu, A. Personal attributions, emotion managements, social supports, and diabetes knowledge in diabetes self-care adherence. Int. J. Collab. Res. Intern. Med. Public Health 2015, 7, 104. [Google Scholar]
- Patel, V.; Chatterji, S. Integrating mental health in care for noncommunicable diseases: An imperative for person-centered care. Health Aff. 2015, 34, 1498–1505. [Google Scholar] [CrossRef]
- Young-Hyman, D.; de Groot, M.; Hill-Briggs, F.; Gonzalez, J.S.; Hood, K.; Peyrot, M. Psychosocial care for people with diabetes: A position statement of the American diabetes association. Diabetes Care 2016, 39, 2126–2140. [Google Scholar] [CrossRef]
- Lindert, J.; Bain, P.A.; Kubzansky, L.D.; Stein, C. Well-being measurement and the WHO health policy Health 2010: Systematic review of measurement scales. Eur. J. Public Health 2015, 25, 731–740. [Google Scholar] [CrossRef]
- Cooke, P.J.; Melchert, T.P.; Connor, K. Measuring Well-Being: A review of instruments. Couns. Psychol. 2016, 44, 730–757. [Google Scholar] [CrossRef]
- Bech, P.; Olsen, L.R.; Kjoller, M.; Rasmussen, N.K. Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. Int. J. Methods Psychiatr. Res. 2003, 12, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, G. Importance of screening for wellbeing in diabetes management. Curr. Res. Diabetes Obes. J. 2019, 11, 17. [Google Scholar] [CrossRef][Green Version]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, N.; Caputo, S.; Dzida, G.; Khunti, K.; Meneghini, L.; Snoek, F. Screening, evaluation and management of depression in people with diabetes in primary care. Prim. Care Diabetes 2013, 7, 1–10. [Google Scholar] [CrossRef]
- Bech, P.; Gudex, C.; Staehr Johansen, K. The WHO (Ten) Well-Being index: Validation in diabetes. Psychother Psychosom. 1996, 65, 183–190. [Google Scholar] [CrossRef]
- Hajós, T.R.S.; Pouwer, F.; Skovlund, S.E.; Oudsten, B.L.D.; Geelhoed-Duijvestijn, P.H.L.M.; Tack, C.J.; Snoek, F.J. Psychometric and screening properties of the WHO-5 well-being index in adult outpatients with Type 1 or Type 2 diabetes mellitus. Diabet. Med. 2013, 30, e63–e69. [Google Scholar] [CrossRef]
- Sischka, P.E.; Costa, A.P.; Steffgen, G.; Schmidt, A.F. The WHO-5 well-being index – validation based on item response theory and the analysis of measurement invariance across 35 countries. J. Affect. Disord. Rep. 2020, 1, 100020. [Google Scholar] [CrossRef]
- Halliday, J.A.; Hendrieckx, C.; Busija, L.; Browne, J.L.; Nefs, G.; Pouwer, F.; Speight, J. Validation of the WHO-5 as a first-step screening instrument for depression in adults with diabetes: Results from Diabetes MILES–Australia. Diabetes Res. Clin. Pract. 2017, 132, 27–35. [Google Scholar] [CrossRef]
- Messina, R.; Rucci, P.; Sturt, J.; Mancini, T.; Fantini, M.P. Assessing self-efficacy in type 2 diabetes management: Validation of the italian version of the diabetes management self-efficacy Scale (IT-DMSES). Health Qual. Life Outcomes 2018, 16, 71. [Google Scholar] [CrossRef]
- Hoogendoorn, C.J.; Schechter, C.B.; Llabre, M.M.; Walker, E.A.; Gonzalez, J.S. Distress and Type 2 diabetes self-care: Putting the pieces together. Ann. Behav. Med. 2020, 55, 938–948. [Google Scholar] [CrossRef]
- Suhaimi, A.F.; Ibrahim, N.; Tan, K.-A.; Silim, U.A.; Moore, G.; Ryan, B.; Castle, D.J. Effectiveness of a culturally adapted biopsychosocial intervention (POHON SIHAT) in improving self-efficacy in patients with diabetes attending primary healthcare clinics in Putrajaya, Malaysia: Study protocol of a randomised controlled trial. BMJ Open 2020, 10, e033920. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A practical guide to their development and use. In Health Measurement Scales: A Practical Guide to their Development and Use; Oxford University Press: Oxford, UK, 2008; pp. 1–452. [Google Scholar]
- World Health Organization. WHO|Process of Translation and Adaptation of Instruments. 2010. Available online: http://www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 3 August 2018).
- Sherina, M.S.; Arroll, B.; Goodyear-Smith, F. Criterion validity of the PHQ-9 (Malay version) in a primary care clinic in Malaysia. Med. J. Malays. 2012, 67, 309–315. [Google Scholar]
- Razali, N.; Jannoo, Z.; Yap, B.W.; Gnanasan, S.; Hassali, M.A.; Shafie, A.A.; Karuppannan, M.; Gopalan, Y.; Omar, M.D.; Ramli, N.I. Validation of the Malay Version of the Problem Areas in Diabetes Scale (MY-PAID-20). In Proceedings of the 16th International Conference on Mathematical and Computational Methods in Science and Engineering; WSEAS Press: Zografou, Greece, 2014; pp. 200–207. [Google Scholar]
- Sharoni, S.K.A.; Wu, S.-F.V. Self-efficacy and self-care behavior of Malaysian patients with type 2 diabetes: A cross sectional survey. Nurs. Health Sci. 2012, 14, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.A.; Ismail, M.; Bariyyah, N.; Baharum, N.; Othman, S.; Lazim, S.; Shah, S. Validation of the Summary of Diabetes Self-care Activities (SDSCA) in Malay language for Malaysian adults. Malays. J. Public Health Med. 2016, 16, 227–234. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 3rd ed.; The Guilford Press: New York, NY, USA, 2011; Available online: https://psycnet.apa.org/record/2010-18801-000 (accessed on 12 June 2020).
- George, D.; Mallery, P. SPSS for Windows Step by Step: A Simple Guide and Reference, 4th ed.; Allyn & Bacon: Boston, MA, USA, 2003. [Google Scholar]
- Piedmont, R.L.; Piedmont, R. Factorial Validity. Encycl. Qual. Life Well-Being Res. 2014, 2148–2149. Available online: https://link.springer.com/referenceworkentry/10.1007/978-94-007-0753-5_984 (accessed on 27 February 2022).
- Kyriazos, T.A. Applied Psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in General. Psychology 2018, 9, 2207–2230. [Google Scholar] [CrossRef]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Bellamy, N. Principles of Clinical Outcome Assessment, Rheumatol, 6th ed.; Elsevier Mosby: Philadelphia, PA, USA, 2015; Volumes 1–2, pp. 9–19. [Google Scholar]
- Fink, A. Survey research methods. In International Encyclopedia of Education; Elsevier BV: Amsterdam, The Netherlands, 2010; pp. 152–160. [Google Scholar]
- Massey, C.N.; Feig, E.H.; Duque, L.; Wexler, D.; Moskowitz, J.T.; Huffman, J.C. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res. Clin. Pract. 2019, 147, 118–133. [Google Scholar] [CrossRef]
- Devarajooh, C.; Chinna, K. Depression, distress and self-efficacy: The impact on diabetes self-care practices. PLoS ONE 2017, 12, e0175096. [Google Scholar] [CrossRef]
- Vallis, M.; Burns, K.K.; Hollahan, D.; Ross, S.; Hahn, J. Diabetes attitudes, wishes and needs second study (DAWN2): Understanding diabetes-related psychosocial outcomes for Canadians with diabetes. Can. J. Diabetes 2016, 40, 234–241. [Google Scholar] [CrossRef]
- Saipanish, R.; Lotrakul, M.; Sumrithe, S. Reliability and validity of the Thai version of the WHO-Five Well-Being Index in primary care patients. Psychiatry Clin. Neurosci. 2009, 63, 141–146. [Google Scholar] [CrossRef]
- Eser, E.; Çevik, C.; Baydur, H.; Güneş, S.; Esgin, T.A.; Öztekin Çağlar, S.; Eker, E.; Gümüşsoy, U.; Eser, G.B.; Özyurt, B. Reliability and validity of the Turkish version of the WHO-5, in adults and older adults for its use in primary care settings. Prim. Health Care Res. Dev. 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Awata, S.; Bech, P.E.; Yoshida, S.; Hirai, M.; Suzuki, S.; Yamashita, M.; Ohara, A.; Hinokio, Y.; Matsuoka, H.; Oka, Y. Reliability and validity of the Japanese version of the world health organization-five well-being index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007, 61, 112–119. Available online: http://www.who-5.org (accessed on 20 October 2020). [CrossRef] [PubMed]
- Snoek, F.J.; Kersch, N.Y.A.; Eldrup, E.; Harman-Boehm, I.; Hermanns, N.; Kokoszka, A.; Matthews, D.R.; McGuire, B.E.; Pibernik-Okanović, M.; Singer, J.; et al. Monitoring of individual needs in diabetes (MIND)-2: Follow-up data from the cross-national diabetes attitudes, wishes, and needs (DAWN) MIND study. Diabetes Care 2012, 35, 2128–2132. [Google Scholar] [CrossRef] [PubMed]
- Reisi, M.; Mostafavi, F.; Javadzade, H.; Mahaki, B.; Tavassoli, E.; Sharifirad, G. Impact of Health literacy, self-efficacy, and outcome expectations on adherence to self-care behaviors in Iranians with type 2 diabetes. Oman Med. J. 2016, 31, 52–59. [Google Scholar] [CrossRef]
- Gao, J.; Wang, J.; Zheng, P.; Haardörfer, R.; Kegler, M.C.; Zhu, Y.; Fu, H. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Fam. Pract. 2013, 14, 66. [Google Scholar] [CrossRef]
- Cheng, L.J.; Wang, W.; Lim, S.T.; Wu, V.X. Factors associated with glycaemic control in patients with diabetes mellitus: A systematic literature review. J. Clin. Nurs. 2019, 28, 1433–1450. [Google Scholar] [CrossRef]
- Distefano, C.; Hess, B. Using confirmatory factor analysis for construct validation: An empirical review. J. Psychoeduc. Assess. 2005, 23, 225–241. [Google Scholar] [CrossRef]
| Measures | M | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| WHO-5 Malay | 68.60 | 17.52 | −0.19 | −0.26 |
| PHQ-9 | 4.44 | 4.39 | 2.30 | 7.39 |
| PAID-20 | 26.81 | 16.61 | 0.25 | −0.79 |
| DMSES | 142.40 | 28.61 | 0.00 | −0.58 |
| SDSCA | 3.27 | 1.20 | 0.14 | −0.39 |
| Fit Indices | WHO-5 Malay Well-Being Index | Cutoff Values † |
|---|---|---|
| Ratio of χ2 to df | 2.38 | ≤2 or 3 |
| Goodness of Fit Index | 0.96 | ≥0.95 |
| Normed Fit Index | 0.97 | ≥0.95 |
| Root Mean Square Error of Approximation | 0.03 | <0.06 |
| Tucker–Lewis fit Index | 0.97 | ≥0.95 |
| Comparative fit Index | 0.98 | ≥0.95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suhaimi, A.F.; Makki, S.M.; Tan, K.-A.; Silim, U.A.; Ibrahim, N. Translation and Validation of the Malay Version of the WHO-5 Well-Being Index: Reliability and Validity Evidence from a Sample of Type 2 Diabetes Mellitus Patients. Int. J. Environ. Res. Public Health 2022, 19, 4415. https://doi.org/10.3390/ijerph19074415
Suhaimi AF, Makki SM, Tan K-A, Silim UA, Ibrahim N. Translation and Validation of the Malay Version of the WHO-5 Well-Being Index: Reliability and Validity Evidence from a Sample of Type 2 Diabetes Mellitus Patients. International Journal of Environmental Research and Public Health. 2022; 19(7):4415. https://doi.org/10.3390/ijerph19074415
Chicago/Turabian StyleSuhaimi, Aida Farhana, Shahidah Mohamed Makki, Kit-Aun Tan, Umi Adzlin Silim, and Normala Ibrahim. 2022. "Translation and Validation of the Malay Version of the WHO-5 Well-Being Index: Reliability and Validity Evidence from a Sample of Type 2 Diabetes Mellitus Patients" International Journal of Environmental Research and Public Health 19, no. 7: 4415. https://doi.org/10.3390/ijerph19074415
APA StyleSuhaimi, A. F., Makki, S. M., Tan, K.-A., Silim, U. A., & Ibrahim, N. (2022). Translation and Validation of the Malay Version of the WHO-5 Well-Being Index: Reliability and Validity Evidence from a Sample of Type 2 Diabetes Mellitus Patients. International Journal of Environmental Research and Public Health, 19(7), 4415. https://doi.org/10.3390/ijerph19074415






