Efficacy of a Deep Learning Convolutional Neural Network System for Melanoma Diagnosis in a Hospital Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. QuantusSKIN System
2.3. Statistical Analysis
3. Results
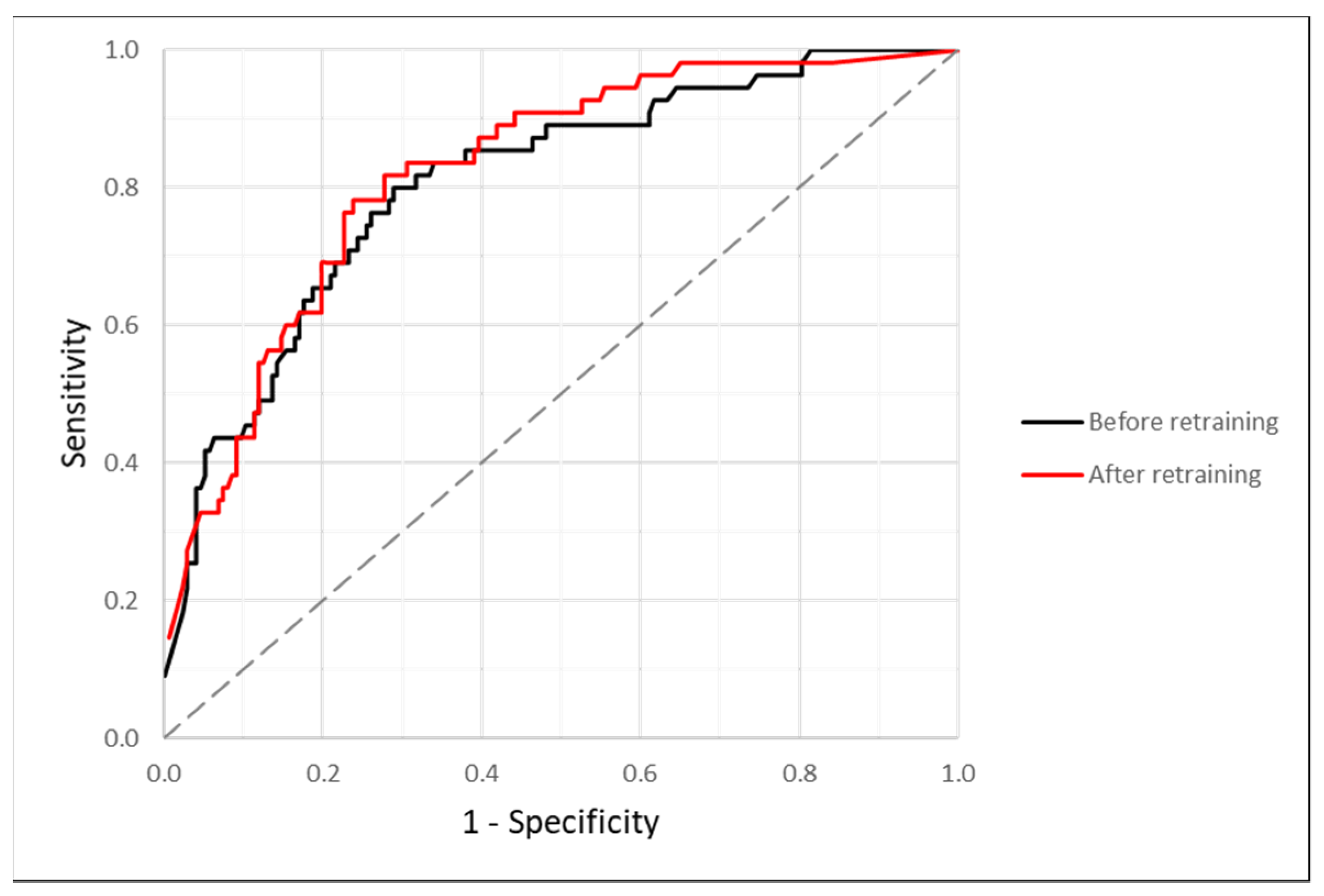
3.1. Efficacy after Re-Training
3.2. Efficacy before Re-Training
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ali, Z.; Yousaf, N.; Larkin, J. Melanoma epidemiology, biology and prognosis. EJC Suppl. 2013, 11, 81–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garbe, C.; Amaral, T.; Peris, K.; Hauschild, A.; Arenberger, P.; Bastholt, L.; Bataille, V.; Del Marmol, V.; Dréno, B.; Fargnoli, M.C.; et al. European consensus-based interdisciplinary guideline for melanoma. Part 1: Diagnostics—Update 2019. Eur. J. Cancer 2020, 126, 141–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Dyba, T.; Randi, G.; Bettio, M.; Gavin, A.; Visser, O.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer 2018, 103, 356–387. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-González, E.; López-Abente, G.; Aragonés, N.; Pollán, M.; Pastor-Barriuso, R.; Sánchez, M.J.; Pérez-Gómez, B. Trends in mortality from cutaneous malignant melanoma in Spain (1982–2016): Sex-specific age-cohort-period effects. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Singh, S.K.; Chakraborty, A.; Das, A.; Bag, R. Melanoma Diagnosis Using Deep Learning and Fuzzy Logic. Diagnostics 2020, 10, 577. [Google Scholar] [CrossRef] [PubMed]
- Tsao, H.; Olazagasti, J.M.; Cordoro, K.M.; Brewer, J.D.; Taylor, S.C.; Bordeaux, J.S.; Chren, M.M.; Sober, A.J.; Tegeler, C.; Bhushan, R.; et al. Early detection of melanoma: Reviewing the ABCDEs. J. Am. Acad. Dermatol. 2015, 72, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, M.E.; Macaskill, P.; Holt, P.E.; Menzies, S.W. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: A meta-analysis of studies performed in a clinical setting. Br. J. Dermatol. 2008, 159, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Kittler, H.; Pehamberger, H.; Wolff, K.; Binder, M. Diagnostic accuracy of dermoscopy. Lancet Oncol. 2002, 3, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Haenssle, H.A.; Fink, C.; Schneiderbauer, R.; Toberer, F.; Buhl, T.; Blum, A.; Kalloo, A.; Hassen, A.B.H.; Thomas, L.; Enk, A.; et al. Man against machine: Diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann. Oncol. 2018, 29, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Hekler, A.; Enk, A.H.; Klode, J.; Hauschild, A.; Berking, C.; Schilling, B.; Haferkamp, S.; Schadendorf, D.; Fröhling, S.; et al. A convolutional neural network trained with dermoscopic images performed on par with 145 dermatologists in a clinical melanoma image classification task. Eur J. Cancer 2019, 111, 148–154. [Google Scholar] [CrossRef] [Green Version]
- Coronado-Gutiérrez, D.; López, C.; Burgos-Artizzu, X.P. Skin cancer high-risk patient screening from dermoscopic images via Artificial Intelligence: An online study. Medrxiv 2021, 1–16. [Google Scholar] [CrossRef]
- Shelhamer, E.; Long, J.; Darrell, T. Fully Convolutional Networks for Semantic Segmentation. IEEE Trans. Pattern Anal. Mach. Intell. 2017, 39, 640–651. [Google Scholar] [CrossRef] [PubMed]
- Szegedy, C.; Liu, W.; Jia, Y.; Sermanet, P.; Reed, S.; Anguelov, D.; Erhan, D.; Vanhoucke, V.; Rabinovich, A. Going deeper with convolutions. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Boston, MA, USA, 7–12 June 2015; pp. 1–9. [Google Scholar]
- Kaur, R.; Gholam Hosseini, H.; Sinha, R. Deep Convolutional Neural Network for Melanoma Detection using Dermoscopy Images. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; Volume 2020, pp. 1524–1527. [Google Scholar] [CrossRef]
- Liu, Y.; Jain, A.; Eng, C.; Way, D.H.; Lee, K.; Bui, P.; Kanada, K.; de Oliveira Marinho, G.; Gallegos, J.; Gabriele, S.; et al. A deep learning system for differential diagnosis of skin diseases. Nat. Med. 2020, 26, 900–908. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Nevus Group | Melanoma Group |
|---|---|---|
| Sample (n) | 177 | 55 |
| Age (years) | 40.91 ± 17.83 | 60.53 ± 18.39 |
| Gender (F/M) | 121/56 | 30/25 |
| Skin lesion location (n, %) | ||
| Scalp | 0 (0.0%) | 1 (1.8%) |
| Face | 5 (2.8%) | 6 (10.9%) |
| Neck | 2 (1.1%) | 2 (3.6%) |
| Trunk | 144 (81.4%) | 26 (47.3%) |
| Upper extremity | 10 (5.7%) | 6 (10.9%) |
| Lower extremity | 10 (5.7%) | 11 (20.0%) |
| Hand | 1 (0.6%) | 0 (0.0%) |
| Foot | 4 (2.3%) | 1 (1.8%) |
| Vulvar skin | 1 (0.6%) | 1 (1.8%) |
| Foreskin | 0 (0.0%) | 1 (1.8%) |
| Error Metric/Study | Diagnostic Threshold (%) | Sensitivity | Specificity | Accuracy | PPV | NPV | F1 Score | F2 Score |
|---|---|---|---|---|---|---|---|---|
| Maximum F1 score | 53.51 | 0.782 | 0.763 | 0.767 | 0.506 | 0.918 | 0.614 | 0.705 |
| Specificity > 0.800 andmaximum sensitivity | 67.33 | 0.691 | 0.802 | 0.776 | 0.521 | 0.893 | 0.594 | 0.648 |
| Haenssle et al. [9] | - | 0.950 | 0.825 | - | - | - | - | - |
| Brinker et al. [10] | - | 0.682 | - | - | - | - | - | - |
| Kaur et al. [14] | - | 0.830 | 0.839 | 0.830 | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-Gonzalez, M.; Azcarraga, C.; Martin-Gil, A.; Carpena-Torres, C.; Jaen, P. Efficacy of a Deep Learning Convolutional Neural Network System for Melanoma Diagnosis in a Hospital Population. Int. J. Environ. Res. Public Health 2022, 19, 3892. https://doi.org/10.3390/ijerph19073892
Martin-Gonzalez M, Azcarraga C, Martin-Gil A, Carpena-Torres C, Jaen P. Efficacy of a Deep Learning Convolutional Neural Network System for Melanoma Diagnosis in a Hospital Population. International Journal of Environmental Research and Public Health. 2022; 19(7):3892. https://doi.org/10.3390/ijerph19073892
Chicago/Turabian StyleMartin-Gonzalez, Manuel, Carlos Azcarraga, Alba Martin-Gil, Carlos Carpena-Torres, and Pedro Jaen. 2022. "Efficacy of a Deep Learning Convolutional Neural Network System for Melanoma Diagnosis in a Hospital Population" International Journal of Environmental Research and Public Health 19, no. 7: 3892. https://doi.org/10.3390/ijerph19073892
APA StyleMartin-Gonzalez, M., Azcarraga, C., Martin-Gil, A., Carpena-Torres, C., & Jaen, P. (2022). Efficacy of a Deep Learning Convolutional Neural Network System for Melanoma Diagnosis in a Hospital Population. International Journal of Environmental Research and Public Health, 19(7), 3892. https://doi.org/10.3390/ijerph19073892







