Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference?
Abstract
1. Introduction
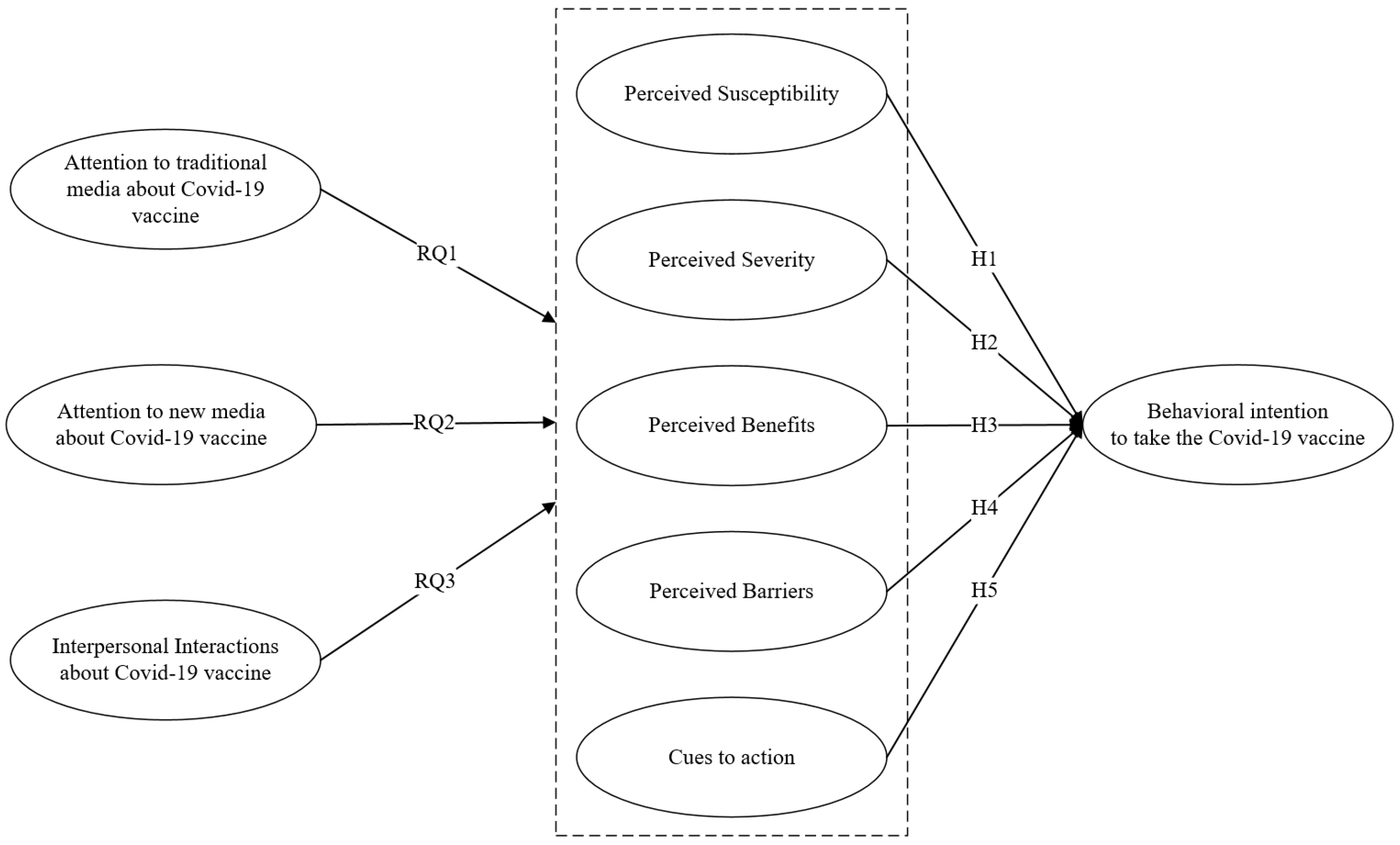
2. Theoretical Model and Development of Hypotheses
2.1. Health Belief Model
2.2. Linking Information Acquisition to the Health Belief Model
3. Methods
3.1. Data Collection
3.2. Measures
3.3. Analytical Approach
4. Results
5. Discussion
6. Implications and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Kong, Y.; Chang, H. Media Use and Health Behavior in H1N1 Flu Crisis: The Mediating Role of Perceived Knowledge and Fear. Atl. J. Commun. 2015, 23, 67–80. [Google Scholar] [CrossRef]
- Pope, J.P.; Pelletier, L.; Guertin, C. Starting Off on the Best Foot: A Review of Message Framing and Message Tailoring, and Recommendations for the Comprehensive Messaging Strategy for Sustained Behavior Change. Health Commun. 2018, 33, 1068–1077. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Watts, J.; Tan, N. From Screen to Screening: Entertainment and News Television Media Effects on Cancer Screening Behaviors. J. Health Commun. 2019, 24, 385–394. [Google Scholar] [CrossRef]
- Acar, D.; Kıcali, Ü.Ö. An Integrated Approach to COVID-19 Preventive Behaviour Intentions: Protection Motivation Theory, Information Acquisition, and Trust. Soc. Work Public Health 2021, 37, 1–16. [Google Scholar] [CrossRef]
- Le, H.T.; Nguyen, D.N.; Beydoun, A.S.; Le, X.T.T.; Nguyen, T.T.; Pham, Q.T.; Ta, N.T.K.; Nguyen, Q.T.; Nguyen, A.N.; Hoang, M.T.; et al. Demand for Health Information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health 2020, 17, 4377. [Google Scholar] [CrossRef]
- Person, B.; Sy, F.; Holton, K.; Govert, B.; Liang, A.; Garza, B.; Gould, D.; Hickson, M.; McDonald, M.; Meijer, C.; et al. Fear and Stigma: The Epidemic within the SARS Outbreak. Emerg. Infect. Dis. 2004, 10, 358–363. [Google Scholar] [CrossRef]
- Sommariva, S.; Vamos, C.; Mantzarlis, A.; Đào, L.U.-L.; Tyson, D.M. Spreading the (Fake) News: Exploring Health Messages on Social Media and the Implications for Health Professionals Using a Case Study. Am. J. Health Educ. 2018, 49, 246–255. [Google Scholar] [CrossRef]
- Gehrau, V.; Fujarski, S.; Lorenz, H.; Schieb, C.; Blöbaum, B. The Impact of Health Information Exposure and Source Credibility on COVID-19 Vaccination Intention in Germany. Int. J. Environ. Res. Public Health 2021, 18, 4678. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Putte, B.V.D.; Yzer, M.; Southwell, B.; De Bruijn, G.-J.; Willemsen, M.C. Interpersonal Communication as an Indirect Pathway for the Effect of Antismoking Media Content on Smoking Cessation. J. Health Commun. 2011, 16, 470–485. [Google Scholar] [CrossRef]
- Ho, S.S.; Peh, X.; Soh, V.W.L. The Cognitive Mediation Model: Factors Influencing Public Knowledge of the H1N1 Pandemic and Intention to Take Precautionary Behaviors. J. Health Commun. 2013, 18, 773–794. [Google Scholar] [CrossRef]
- Chen, L.; Yang, X. Using EPPM to evaluate the effectiveness of fear appeal messages across different media outlets to increase the intention of breast self-examination among Chinese women. Health Commun. 2019, 24, 1369–1376. [Google Scholar] [CrossRef]
- Fleming, K.; Thorson, E.; Zhang, Y. Going Beyond Exposure to Local News Media: An Information-Processing Examination of Public Perceptions of Food Safety. J. Health Commun. 2006, 11, 789–806. [Google Scholar] [CrossRef]
- Audrain-McGovern, J.; Rodriguez, D.; Patel, V.; Faith, M.S.; Rodgers, K.; Cuevas, J. How Do Psychological Factors Influence Adolescent Smoking Progression? The Evidence for Indirect Effects Through Tobacco Advertising Receptivity. Pediatrics 2006, 117, 1216–1225. [Google Scholar] [CrossRef]
- Donadiki, E.; Garcia, R.J.; Hernández-Barrera, V.; Sourtzi, P.; Carrasco-Garrido, P.; Lopez-De-Andres, A.; Jimenez-Trujillo, I.; Velonakis, E. Health Belief Model applied to non-compliance with HPV vaccine among female university students. Public Health 2014, 128, 268–273. [Google Scholar] [CrossRef]
- Coe, A.; Gatewood, S.B.; Moczygemba, L.R.; Goode, J.-V.R.; Beckner, J.O. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innov. Pharm. 2012, 3. [Google Scholar] [CrossRef]
- Rosenstock, I.M. What research in motivation suggests for public health. Am. J. Public Health Nations Health 1960, 50, 295–302. [Google Scholar]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Why people use health services. Milbank Q. 2005, 83, 1–32. [Google Scholar] [CrossRef]
- Champion, V.; Skinner, C.S.; Menon, U. Development of a self-efficacy scale for mammography. Res. Nurs. Health 2005, 28, 329–336. [Google Scholar] [CrossRef]
- Zuo, Y.; Zhang, M.; Si, Y.; Wu, X.; Ren, Z. Prediction of Health Risk Preventative Behavior of Amateur Marathon Runners: A Cross-Sectional Study. Risk Manag. Health Policy 2021, 14, 2929–2944. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; Abubakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S. The health belief model. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Blue, C.L.; Valley, J.M. Predictors of Influenza Vaccine: Acceptance among healthy adult workers. AAOHN J. 2002, 50, 227–233. [Google Scholar] [CrossRef]
- Orji, R.; Vassileva, J.; Mandryk, R. Towards an Effective Health Interventions Design: An Extension of the Health Belief Model. Online J. Public Health Inform. 2012, 4, e9. [Google Scholar] [CrossRef]
- Guidry, J.P.; Carlyle, K.E.; Perrin, P.B.; LaRose, J.G.; Ryan, M.; Messner, M. A path model of psychosocial constructs predicting future Zika vaccine uptake intent. Vaccine 2019, 37, 5233–5241. [Google Scholar] [CrossRef]
- Song, H.R.; Kim, C. Relationship between risk involvement, risk perception, perceived severity and preventive behavior intention of avian influenza. Crisisonomy 2014, 10, 33–49. [Google Scholar]
- Bults, M.; Beaujean, D.J.; de Zwart, O.; Kok, G.; van Empelen, P.; van Steenbergen, J.E.; Richardus, J.H.; Voeten, H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health 2011, 11, 2. [Google Scholar]
- Carpenter, C.J. A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef]
- Shah, G.; Faraz, A.; Khan, H.; Waterfield, K. Perceived Benefits Matter the Most in COVID-19 Preventive Behaviors: Empirical Evidence from Okara District, Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 6772. [Google Scholar] [CrossRef] [PubMed]
- Hyman, R.B.; Baker, S.; Ephraim, R.; Moadel, A.; Philip, J. Health belief model variables as predictors of screening mammography utilization. J. Behav. Med. 1994, 17, 391–406. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.H.; Janz, N.K. The Health Belief Model Applied to Understanding Diabetes Regimen Compliance. Diabetes Educ. 1985, 11, 41–47. [Google Scholar] [CrossRef]
- Austin, L.T.; Ahmad, F.; McNally, M.-J.; Stewart, D.E. Breast and cervical cancer screening in Hispanic women: A literature review using the health belief model. Women’s Health Issues 2002, 12, 122–128. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Harrison, J.A.; Mullen, P.D.; Green, L.W. A meta-analysis of studies of the Health Belief Model with adults. Health Educ. Res. 1992, 7, 107–116. [Google Scholar] [CrossRef]
- Yang, Z.J. Predicting Young Adults’ Intentions to Get the H1N1 Vaccine: An Integrated Model. J. Health Commun. 2015, 20, 69–79. [Google Scholar] [CrossRef]
- Jones, T.; Fowler, M.C.; Hubbard, D. Refining a tool to measure cues to action in encouraging health-promoting behavior—The CHAQ. Am. J. Health Promot. 2000, 14, 170–173. [Google Scholar] [CrossRef]
- Nugrahani, R.R.; Budihastuti, U.R.; Pamungakasari, E.P. Health Belief Model on the Factors Associated with the Use of HPV Vaccine for the Prevention of Cervical Cancer among Women in Kediri, East Java. J. Epidemiol. Public Health 2017, 2, 70–81. [Google Scholar] [CrossRef]
- Chang, C. Behavioral Recommendations in Health Research News as Cues to Action: Self-Relevancy and Self-Efficacy Processes. J. Health Commun. 2016, 21, 954–968. [Google Scholar] [CrossRef]
- Liu, L.; Xie, J.; Li, K.; Ji, S. Exploring How Media Influence Preventive Behavior and Excessive Preventive Intention during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 7990. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, X. Linking Risk Perception to Breast Cancer Examination Intention in China: Examining an Adapted Cognitive Mediation Model. Health Commun. 2021, 36, 1813–1824. [Google Scholar] [CrossRef]
- Karlsson, P. Explaining small effects of information-based drug prevention: The importance of considering preintervention levels in risk perceptions. J. Alcohol Drug Educ. 2008, 52, 9–17. [Google Scholar]
- Ali, S.H.; Foreman, J.; Tozan, Y.; Capasso, A.; Jones, A.M.; DiClemente, R.J. Trends and Predictors of COVID-19 Information Sources and Their Relationship With Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e21071. [Google Scholar] [CrossRef]
- Klein, B.D. User perceptions of data quality: Internet and traditional text sources. J. Comput. Inf. Syst. 2001, 41, 9–15. [Google Scholar] [CrossRef]
- Wang, P.-W.; Lu, W.-H.; Ko, N.-Y.; Chen, Y.-L.; Li, D.-J.; Chang, Y.-P.; Yen, C.-F. COVID-19-Related Information Sources and the Relationship With Confidence in People Coping with COVID-19: Facebook Survey Study in Taiwan. J. Med Internet Res. 2020, 22, e20021. [Google Scholar] [CrossRef]
- Fishman, J.M.; Casarett, D. Mass media and medicine: When the most trusted media mislead. In Mayo Clinic Proceedings; Elsevier Limited: Amsterdam, The Netherlands, 2006; Volume 81, p. 291. [Google Scholar] [CrossRef]
- Gaskell, G.; Allum, N.; Wagner, W.; Kronberger, N.; Torgersen, H.; Hampel, J.; Bardes, J. GM Foods and the Misperception of Risk Perception. Risk Anal. 2004, 24, 185–194. [Google Scholar] [CrossRef]
- Zhang, X.; Wen, D.; Liang, J.; Lei, J. How the public uses social media wechat to obtain health information in china: A survey study. BMC Med Informatics Decis. Mak. 2017, 17, 71–79. [Google Scholar] [CrossRef]
- Guidry, J.P.; Meganck, S.L.; Perrin, P.B.; Messner, M.; Lovari, A.; Carlyle, K.E. #Ebola: Tweeting and Pinning an Epidemic. Atl. J. Commun. 2021, 29, 79–92. [Google Scholar] [CrossRef]
- Chew, C.; Eysenbach, G. Pandemics in the Age of Twitter: Content Analysis of Tweets during the 2009 H1N1 Outbreak. PLoS ONE 2010, 5, e14118. [Google Scholar] [CrossRef]
- Ng, Y.J. Noisy Haze, Quiet Dengue: The Effects of Mass Media, Interpersonal Interactions, and Social Media on Risk Amplification; State University of New York at Buffalo: Buffalo, NY, USA, 2014. [Google Scholar]
- Chaffee, S.H.; Schleuder, J. Measurement and Effects of Attention to Media News. Hum. Commun. Res. 1986, 13, 76–107. [Google Scholar] [CrossRef]
- Liao, Y.; Ho, S.S.; Yang, X. Motivators of Pro-Environmental Behavior: Examining the underlying processes in the influence of presumed media influence model. Sci. Commun. 2016, 38, 51–73. [Google Scholar] [CrossRef]
- Besley, J.C.; Shanahan, J. Media Attention and Exposure in Relation to Support for Agricultural Biotechnology. Sci. Commun. 2005, 26, 347–367. [Google Scholar] [CrossRef]
- Ho, S.S.; Scheufele, D.A.; Corley, E.A. Factors influencing public risk–benefit considerations of nanotechnology: Assessing the effects of mass media, interpersonal communication, and elaborative processing. Public Underst. Sci. 2013, 22, 606–623. [Google Scholar] [CrossRef]
- Yang, X.; Chuah, A.S.F.; Lee, E.W.J.; Ho, S.S. Extending the Cognitive Mediation Model: Examining Factors Associated With Perceived Familiarity and Factual Knowledge of Nanotechnology. Mass Commun. Soc. 2017, 20, 403–426. [Google Scholar] [CrossRef]
- Nan, X.; Kim, J. Predicting H1N1 Vaccine Uptake and H1N1-Related Health Beliefs: The Role of Individual Difference in Consideration of Future Consequences. J. Health Commun. 2014, 19, 376–388. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Chen, M.-F.; Wang, R.-H.; Schneider, J.K.; Tsai, C.-T.; Jiang, D.D.-S.; Hung, M.-N.; Lin, L.-J. Using the Health Belief Model to Understand Caregiver Factors Influencing Childhood Influenza Vaccinations. J. Community Health Nurs. 2011, 28, 29–40. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus Statistical Analysis with Latent Variables: User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411. [Google Scholar]
- Chang, C. News Coverage of Health-Related Issues and Its Impacts on Perceptions: Taiwan as an Example. Health Commun. 2012, 27, 111–123. [Google Scholar] [CrossRef]
- Rowe, G.; Frewer, L.; Sjöberg, L. Newspaper reporting of hazards in the UK and Sweden. Public Underst. Sci. 2000, 9, 59–78. [Google Scholar] [CrossRef] [PubMed]
- Apuke, O.D.; Omar, B. Television News Coverage of COVID-19 Pandemic in Nigeria: Missed Opportunities to Promote Health Due to Ownership and Politics. SAGE Open 2021, 11. [Google Scholar] [CrossRef]
- Trope, Y.; Liberman, N. Construal-level theory of psychological distance. Psychol. Rev. 2010, 117, 440. [Google Scholar] [PubMed]
- Choi, D.-H.; Yoo, W.; Noh, G.Y.; Park, K. The impact of social media on risk perceptions during the MERS outbreak in South Korea. Comput. Hum. Behav. 2017, 72, 422–431. [Google Scholar] [CrossRef]
- Chen, Y. The Roles of Prevention Messages, Risk Perception, and Benefit Perception in Predicting Binge Drinking among College Students. Health Commun. 2018, 33, 877–886. [Google Scholar] [CrossRef]
- Fung, I.C.-H.; Wong, K.K. Efficient use of social media during the avian influenza A(H7N9) emergency response. West. Pac. Surveill. Response J. 2013, 4, 1. [Google Scholar] [CrossRef][Green Version]
- Muniz-Rodriguez, K.; Ofori, S.K.; Bayliss, L.C.; Schwind, J.S.; Diallo, K.; Liu, M.; Yin, J.; Chowell, G.; Fung, I.C.-H. Social Media Use in Emergency Response to Natural Disasters: A Systematic Review With a Public Health Perspective. Disaster Med. Public Health Prep. 2020, 14, 139–149. [Google Scholar] [CrossRef]
- Tran, B.X.; Dang, A.K.; Thai, P.K.; Le, H.T.; Le, X.T.T.; Do, T.T.T.; Nguyen, T.H.; Pham, H.Q.; Phan, H.T.; Vu, G.T.; et al. Coverage of Health Information by Different Sources in Communities: Implication for COVID-19 Epidemic Response. Int. J. Environ. Res. Public Health 2020, 17, 3577. [Google Scholar] [CrossRef]
- Ju, I.; Ohs, J.; Park, T.; Hinsley, A. Interpersonal Communication Influence on Health-Protective Behaviors amid the COVID-19 Crisis. Health Commun. 2021. [Google Scholar] [CrossRef]
- Southwell, B.G.; Torres, A. Connecting Interpersonal and Mass Communication: Science News Exposure, Perceived Ability to Understand Science, and Conversation. Commun. Monogr. 2006, 73, 334–350. [Google Scholar] [CrossRef]
- Teo, L.; Smith, H.; Lwin, M.; Tang, W. Attitudes and perception of influenza vaccines among older people in Singapore: A qualitative study. Vaccine 2019, 37, 6665–6672. [Google Scholar] [CrossRef]
- Li, Y.; Luan, S.; Li, Y.; Hertwig, R. Changing emotions in the COVID-19 pandemic: A four-wave longitudinal study in the United States and China. Soc. Sci. Med. 2021, 285, 114222. [Google Scholar] [CrossRef]
- Burgos, R.M.; Badowski, M.E.; Drwiega, E.; Ghassemi, S.; Griffith, N.; Herald, F.; Johnson, M.; Smith, R.O.; Michienzi, S.M. The race to a COVID-19 vaccine: Opportunities and challenges in development and distribution. Drugs Context 2021, 10, 1–10. [Google Scholar] [CrossRef]
- Zakar, R.; Momina, A.U.; Shahzad, S.; Hayee, M.; Shahzad, R.; Zakar, M.Z. COVID-19 Vaccination Hesitancy or Acceptance and Its Associated Factors: Findings from Post-Vaccination Cross-Sectional Survey from Punjab Pakistan. Int. J. Environ. Res. Public Health 2022, 19, 1305. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef]
- Jones, C.L.; Jensen, J.D.; Scherr, C.L.; Brown, N.R.; Christy, K.; Weaver, J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 2015, 30, 566–576. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, X. Determinants of Beijing Residents’ Intentions to Take Protective Behaviors against Smog: An Application of the Health Belief Model. Health Commun. 2021, 1–13. [Google Scholar] [CrossRef]

| n | Mean | Median | Std. Deviation | Minimum | Maximum | Range | |
|---|---|---|---|---|---|---|---|
| Age | 621 | 28.75 | 27.00 | 9.12 | 18.00 | 75.00 | 18–57 |
| Gender | 621 | 1.56 | 2.00 | 0.50 | 1.00 | 2.00 | 1–2 |
| Education | 621 | 4.97 | 5.00 | 0.65 | 1.00 | 8.00 | 1–8 |
| Income | 621 | 4.99 | 5.00 | 2.89 | 1.00 | 11.00 | 1–11 |
| Traditional Media Attention | 621 | 4.04 | 4.00 | 1.69 | 1.00 | 7.00 | 1–7 |
| New Media Attention | 621 | 5.65 | 6.00 | 1.22 | 1.00 | 7.00 | 1–7 |
| Interpersonal Interactions | 621 | 4.33 | 4.25 | 1.32 | 1.00 | 7.00 | 1–7 |
| Perceived Susceptibility | 621 | 4.68 | 4.67 | 1.58 | 1.00 | 7.00 | 1–7 |
| Perceived Severity | 621 | 5.47 | 5.80 | 1.24 | 1.00 | 7.00 | 1–7 |
| Perceived Benefits | 621 | 5.47 | 5.50 | 1.04 | 1.50 | 7.00 | 1.5–7 |
| Perceived Barriers | 621 | 2.84 | 2.60 | 1.24 | 1.00 | 7.00 | 1–7 |
| Cues to Action | 621 | 5.17 | 5.25 | 1.29 | 1.00 | 7.00 | 1–7 |
| Behavioral Intention | 621 | 5.75 | 6.00 | 1.27 | 1.00 | 7.00 | 1–7 |
| (a) | (b) | (d) | (e) | (f) | (g) | (h) | (i) | (j) | (k) | (l) | (m) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (a) Age | 1 | |||||||||||
| (b) Gender | −0.170 *** | 1 | ||||||||||
| (c) Education | −0.210 *** | 0.031 | 1 | |||||||||
| (d) Income | 0.091 * | −0.184 *** | 0.212 *** | 1 | ||||||||
| (e) Traditional Media Attention | 0.244 *** | −0.058 | −0.127 ** | 0.123 *** | 1 | |||||||
| (f) New Media Attention | 0.075 | 0.030 | −0.002 | 0.097 * | 0.454 *** | 1 | ||||||
| (g) Interpersonal Interactions | 0.240 *** | −0.004 | −0.062 | 0.087 * | 0.526 *** | 0.437 *** | 1 | |||||
| (h) Perceived Susceptibility | 0.189 *** | −0.049 | −0.048 | 0.017 | 0.207 *** | 0.155 *** | 0.242 *** | 1 | ||||
| (i) Perceived Severity | 0.027 | 0.037 | 0.042 | −0.007 | 0.102 * | 0.183 *** | 0.163 *** | 0.241 *** | 1 | |||
| (j) Perceived Benefits | 0.228 *** | −0.054 | −0.103 * | 0.053 | 0.326 *** | 0.326 *** | 0.414 *** | 0.382 *** | 0.255 *** | 1 | ||
| (k) Perceived Barriers | −0.012 | −0.114 ** | 0.016 | 0.027 | −0.063 | −0.220 *** | −0.011 | −0.001 | 0.066 | −0.241 *** | 1 | |
| (l) Cues to Action | 0.067 | −0.005 | −0.046 | −0.019 | 0.297 *** | 0.349 *** | 0.411 *** | 0.264 ** | 0.223 ** | 0.497 *** | −0.290 *** | 1 |
| (m) Behavioral Intention | 0.054 | 0.037 | −0.043 | −0.113 ** | 0.237 *** | 0.282 *** | 0.319 *** | 0.170 *** | 0.172 *** | 0.387 *** | −0.405 *** | 0.653 *** |
| Variable | Loading | M | SD | AVE | CR |
|---|---|---|---|---|---|
| Traditional Media Attention (r = 0.58) | 0.58 | 0.73 | |||
| tma1 | 0.66 | 3.47 | 1.97 | ||
| tma2 | 0.85 | 4.62 | 1.84 | ||
| New Media Attention (r = 0.57) | 0.57 | 0.73 | |||
| nma1 | 0.79 | 5.67 | 1.38 | ||
| nma2 | 0.72 | 5.63 | 1.38 | ||
| Interpersonal Interactions (α = 0.82) | 0.54 | 0.82 | |||
| ii1 | 0.8 | 4.62 | 1.58 | ||
| ii2 | 0.77 | 4.74 | 1.44 | ||
| ii3 | 0.66 | 4.44 | 1.54 | ||
| ii4 | 0.69 | 3.52 | 1.97 | ||
| Perceived Susceptibility (α = 0.85) | 0.64 | 0.84 | |||
| psu1 | 0.96 | 4.55 | 1.90 | ||
| psu2 | 0.80 | 4.33 | 1.86 | ||
| psu3 | 0.60 | 5.16 | 1.64 | ||
| Perceived Severity (α = 0.89) | 0.63 | 0.89 | |||
| pse1 | 0.68 | 4.88 | 1.72 | ||
| pse2 | 0.87 | 5.64 | 1.43 | ||
| pse3 | 0.83 | 5.65 | 1.44 | ||
| pse4 | 0.89 | 5.75 | 1.32 | ||
| pse5 | 0.68 | 5.44 | 1.47 | ||
| Perceived Benefits (α = 0.77) | 0.48 | 0.78 | |||
| pbe1 | 0.81 | 5.61 | 1.17 | ||
| pbe2 | 0.78 | 5.78 | 1.14 | ||
| pbe3 | 0.57 | 5.26 | 1.40 | ||
| pbe4 | 0.56 | 5.21 | 1.63 | ||
| Perceived Barriers (α = 0.85) | 0.52 | 0.84 | |||
| pba1 | 0.76 | 2.12 | 1.48 | ||
| pba2 | 0.77 | 2.94 | 1.47 | ||
| pba3 | 0.84 | 2.57 | 1.49 | ||
| pba4 | 0.63 | 2.94 | 1.67 | ||
| pba5 | 0.58 | 3.61 | 1.74 | ||
| Cues to Action (α = 0.89) | 0.61 | 0.86 | |||
| cta1 | 0.75 | 5.48 | 1.36 | ||
| cta2 | 0.79 | 5.38 | 1.51 | ||
| cta3 | 0.81 | 5.11 | 1.49 | ||
| cta4 | 0.76 | 4.71 | 1.59 | ||
| Behavioral Intention (α = 0.91) | 0.77 | 0.91 | |||
| bi1 | 0.88 | 5.81 | 1.31 | ||
| bi2 | 0.90 | 5.78 | 1.34 | ||
| bi3 | 0.86 | 5.67 | 1.50 |
| Model | χ2 | df | χ2/df | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| Measurement | 1301.78 | 542 | 2.40 | 0.930 | 0.919 | 0.049 |
| HBM | 1200.41 | 515 | 2.33 | 0.935 | 0.922 | 0.047 |
| Path | Estimates | 95% CI | p-Value | |
|---|---|---|---|---|
| LL | UL | |||
| Traditional media attention → vaccine intention | 0.003 | −0.118 | 0.115 | 0.968 |
| New media attention → vaccine intention | 0.284 | 0.159 | 0.412 | 0.000 |
| Interpersonal interactions → vaccine intention | 0.176 | 0.077 | 0.275 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.; Wei, L.; Liu, Z. Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference? Int. J. Environ. Res. Public Health 2022, 19, 3887. https://doi.org/10.3390/ijerph19073887
Yang X, Wei L, Liu Z. Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference? International Journal of Environmental Research and Public Health. 2022; 19(7):3887. https://doi.org/10.3390/ijerph19073887
Chicago/Turabian StyleYang, Xiaodong, Lai Wei, and Zhiyue Liu. 2022. "Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference?" International Journal of Environmental Research and Public Health 19, no. 7: 3887. https://doi.org/10.3390/ijerph19073887
APA StyleYang, X., Wei, L., & Liu, Z. (2022). Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference? International Journal of Environmental Research and Public Health, 19(7), 3887. https://doi.org/10.3390/ijerph19073887






