The Moderating Effect of Social Support between Loneliness and Depression: Differences between the Young-Old and the Old-Old
Abstract
:1. Introduction
2. Methods
2.1. Data
2.2. Measures
2.2.1. Dependent Variable: Depressive Symptoms
2.2.2. Independent Variable: Loneliness
2.2.3. Moderator Variable: Social Support (Spouse/Partner, Family)
2.2.4. Control Variable
2.3. Data Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Differences of Main Variables between the Young-Old and the Old-Old
3.3. Multivariate Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blazer, D.G. Depression in late life: Review and commentary. J. Gerontology Ser. A Biol. Sci. Med. Sci. 2003, 58, 249–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinman, L.E.; Frederick, J.T.; Prohaska, T.; Satariano, W.A.; Dornberg-Lee, S.; Fisher, R.; Graub, P.B.; Leith, K.; Presby, K.; Sharkey, J.; et al. Recommendations for treating depression in community-based older adults. Am. J. Prev. Med. 2007, 33, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Gonyea, J.G.; Curley, A.; Melekis, K.; Levine, N.; Lee, Y. Loneliness and depression among older adults in urban subsidized housing. J. Aging Health 2018, 30, 458–474. [Google Scholar] [CrossRef] [PubMed]
- Allan, C.E.; Valkanova, V.; Ebmeier, K.P. Depression in older people is underdiagnosed. Practitioner 2014, 258, 19–22. [Google Scholar] [PubMed]
- Conejero, I.; Olié, E.; Courtet, P.; Calati, R. Suicide in older adults: Current perspectives. Clin. Interv. Aging 2018, 13, 691–699. [Google Scholar] [CrossRef] [Green Version]
- Byma, E.A.; Given, C.W.; Given, B.A. Associations among indicators of depression in Medicaid-eligible community-dwelling older adults. Gerontologist 2013, 53, 608–617. [Google Scholar] [CrossRef] [Green Version]
- Luo, Y.; Hawkley, L.C.; Waite, L.J.; Cacioppo, J.T. Loneliness, health, and mortality in old age: A national longitudinal study. Soc. Sci. Med. 2012, 4, 907–914. [Google Scholar] [CrossRef] [Green Version]
- Perissinotto, C.M.; Cenzer, I.S.; Covinsky, K.E. Loneliness in older persons: A predictor of functional decline and death. Arch. Intern. Med. 2012, 172, 1078–1084. [Google Scholar] [CrossRef] [Green Version]
- Green, B.H.; Copeland, J.R.M.; Dewey, M.E.; Sharma, V.; Saunders, P.A.; Davidson, I.A.; Sullivan, C.; McWilliam, C. Risk factors for depression in elderly people: A prospective study. Acta Psychiatr. Scand. 1992, 86, 213–217. [Google Scholar] [CrossRef]
- Singh, A.; Misra, N. Loneliness, depression and sociability in old age. Ind. Psychiatry J. 2009, 18, 51–55. [Google Scholar] [CrossRef]
- Åkerlind, I.; Hörnquist, J.O. Loneliness and alcohol abuse: A review of evidences of an interplay. Soc. Sci. Med. 1992, 34, 405–414. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Crawford, L.E.; Ernst, J.M.; Burleson, M.H.; Kowalewski, R.B.; Malarkey, W.B.; Van Cauter, E.; Berntson, G.G. Loneliness and health: Potential mechanisms. Psychosom. Med. 2002, 64, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.W.; Cutrona, C.E.; de la Mora, A.; Wallace, R.B. Loneliness and nursing home admission among rural older adults. Psychol. Aging 1997, 12, 574–589. [Google Scholar] [CrossRef] [PubMed]
- Coyle, C.E.; Dugan, E. Social isolation, loneliness and health among older adults. J. Aging Health 2012, 24, 1346–1363. [Google Scholar] [CrossRef] [PubMed]
- Jaremka, L.M.; Andridge, R.R.; Fagundes, C.P.; Alfano, C.M.; Povoski, S.P.; Lipari, A.M.; Arnold, M.W.; Farrar, W.B.; Yee, L.D.; Carson, W.E.; et al. Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychol. 2014, 33, 948–957. [Google Scholar] [CrossRef] [PubMed]
- Germani, A.; Delvecchio, E.; Li, J.B.; Lis, A.; Nartova-Bochaver, S.K.; Vazsonyi, A.T.; Mazzeschi, C. The link between individualism–collectivism and life satisfaction among emerging adults from four countries. Appl. Psychol. Health Well-Being 2021, 13, 437–453. [Google Scholar] [CrossRef]
- Nezlek, J.B.; Humphrey, A. Individualism, Collectivism, and Well-being Among a Sample of Emerging Adults in the United States. Emerg. Adulthood 2021, 4, 21676968211054596. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and depression in the elderly: The role of social network. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Liu, L.; Gou, Z.; Zuo, J. Social support mediates loneliness and depression in elderly people. J. Health Psychol. 2016, 21, 750–758. [Google Scholar] [CrossRef]
- Choi, N.G.; Mcdougall, G.J. Comparison of depressive symptoms between homebound older adults and ambulatory older adults. Aging Ment. Health 2007, 11, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Houtjes, W.; Meijel, B.; Ven, P.; Deeg, J.; Van Tilburg, T.; Beekman, T. The impact of an unfavorable depression course on network size and loneliness in older people: A longitudinal study in the community. Int. J. Geriatr. Psychiatry 2014, 29, 1010–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Kong, D.; Sun, B.; Dong, X. Health services utilization among Chinese American older adults: The role of social support. Innov. Aging 2018, 2, 195–196. [Google Scholar] [CrossRef]
- Dupertuis, L.; Aldwin, C.; Bossé, R. Does the source of support matter for different health outcomes? Findings from the normative aging study. J. Aging Health 2001, 13, 494–510. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, K.; Khan, H.T.A. Exploring the relationship between social support and life satisfaction among rural elderly in Japan. Ageing Int. 2016, 41, 414–426. [Google Scholar] [CrossRef]
- Sonnenberg, C.; Deeg, D.; Van Tilburg, T.; Vink, D.; Stek, M.; Beekman, A. Gender differences in the relation between depression and social support in later life. Int. Psychogeriatr. 2013, 25, 61–70. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Chen, L.; Alston, M.; Guo, W. The influence of social support on loneliness and depression among older elderly people in China: Coping styles as mediators. J. Community Psychol. 2019, 47, 1235–1245. [Google Scholar] [CrossRef]
- Maeda, U.; Shen, B.J.; Schwarz, E.R.; Farrell, K.A.; Mallon, S. Self-efficacy mediates the associations of social support and depression with treatment adherence in heart failure patients. Int. J. Behav. Med. 2013, 20, 88–96. [Google Scholar] [CrossRef]
- Tower, R.B.; Kasl, S.V. Gender, marital closeness, and depressive symptoms in elderly couples. J. Gerontol. 1996, 51B, 115–129. [Google Scholar] [CrossRef]
- Choi, N.G.; Ha, J.H. Relationship between spouse/partner support and depressive symptoms in older adults: Gender difference. Aging Ment. Health 2011, 15, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in Older Adults. Annu. Rev. Clin. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef]
- Deng, J.L.; Hu, J.M.; Wu, W.L.; Dong, B.R.; Wu, H.M. Subjective well-being, social support, and age-related functioning among the very old in China. Int. J. Geriatr. Psychiatry 2010, 25, 697–703. [Google Scholar] [CrossRef]
- Kohout, F.J.; Berkman, L.F.; Evans, D.A.; Cornoni-Huntley, J.C.-H. Two Shorter Forms of the CES-D depression symptoms Index. J. Aging Health 1993, 5, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Schuster, T.L.; Kessler, R.C.; Aseltine, R.H. Supportive interactions, negative interactions, and depressed mood. Am. J. Community Psychol. 1990, 18, 423–438. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Guilford Publication: New York, NY, USA, 2017. [Google Scholar]
- Mertler, C.A.; Reinhart, R.V. Advanced and Multivariate Statistical Methods: Practical Application and Interpretation, 6th ed.; Taylor & Francis: New York, NY, USA, 2016. [Google Scholar]
- Adams, K.B.; Sanders, S.; Auth, E.A. Loneliness and depression in independent living retirement communities: Risk and resilience factors. Aging Ment. Health 2004, 8, 475–485. [Google Scholar] [CrossRef]
- Barg, F.K.; Huss-Ashmore, R.; Wittink, M.N.; Murray, G.F.; Bogner, H.R.; Gallo, J.J. A mixed-methods approach to understanding loneliness and depression in older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2006, 61, S329–S339. [Google Scholar] [CrossRef] [Green Version]
- Dean, A.; Kolody, B.; Wood, P. Effects of social support from various sources on depression in elderly persons. J. Health Soc. Behav. 1990, 31, 148–161. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. CDC Promotes Public Health Approach to Address Depression among Older Adults. Available online: www.cdc.gov/aging (accessed on 10 October 2021).
- Ciechanowski, P.; Chaytor, N.; Miller, J.; Fraser, R.; Russo, J.; Unutzer, J.; Gilliam, F. PEARLS depression treatment for individuals with epilepsy: A randomized controlled trial. Epilepsy Behav. 2010, 19, 225–231. [Google Scholar] [CrossRef]
- Harpole, L.H.; Williams, J.W.; Olsen, M.K.; Stechuchak, K.M.; Oddone, E.; Callahan, C.M.; Katon, W.J.; Lin, E.H.; Grypma, L.M.; Unützer, J. Improving depression outcomes in older adults with comorbid medical illness. Gen. Hosp. Psychiatry 2005, 27, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Steinberg, N.S.; Dong, X.; Tiwari, A. A cross-sectional study of coping resources and mental health of Chinese older adults in the United States. Aging Ment. Health 2018, 22, 1448–1455. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zhang, M.; Simon, M.A. The expectation and perceived receipt of filial piety among Chinese older adults in the Greater Chicago area. J. Aging Health 2014, 26, 1225–1247. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chi, I. Correlates of physician visits among older adults in China: The effects of family support. J. Aging Health 2011, 23, 933–953. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Yang, S.; Knapp, M. Sources and directions of social support and life satisfaction among solitary Chinese older adults in Hong Kong: The mediating role of sense of loneliness. Clin. Interv. Aging 2018, 13, 63–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variables | The Young-Old (n = 903) | The Old-Old (n = 629) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Gender | Male | 463 | 51.3 | 376 | 59.8 |
| Female | 440 | 48.7 | 253 | 40.2 | |
| Age | M (SD) | 69.79 (2.58) | 80.21 (4.17) | ||
| Education Attainment | Less than High School | 106 | 11.7 | 96 | 15.3 |
| High School Equivalent | 193 | 21.4 | 157 | 25.0 | |
| Vocational Certificate/Some Degree/Associates | 307 | 34.0 | 196 | 31.2 | |
| Bachelors or More | 297 | 32.9 | 180 | 28.6 | |
| Race | White | 708 | 78.4 | 480 | 76.3 |
| Other | 195 | 21.6 | 149 | 23.7 | |
| Variables | The Young-Old (n = 903) | The Old-Old (n = 629) | t | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Loneliness | 0.86 | 0.73 | 0.87 | 0.67 | −0.126 |
| Spouse Support | 2.29 | 0.50 | 2.26 | 0.51 | 1.448 |
| Family Support | 2.19 | 0.52 | 2.23 | 0.52 | −1.253 |
| Depression | 1.41 | 0.42 | 1.45 | 0.42 | −1.800 |
| Variables | The Young-Old (n = 903) | The Old-Old (n = 629) | |||
|---|---|---|---|---|---|
| B | S.E. | B | S.E. | ||
| Constant | 1.608 | 0.334 | 0.510 | 0.306 | |
| Control Variable | Gender (ref. male) | 0.087 ** | 0.025 | 0.089 ** | 0.032 |
| Age | −0.001 | 0.005 | 0.012 ** | 0.004 | |
| Education Attainment | −0.055 *** | 0.013 | −0.024 | 0.015 | |
| Race (ref. white) | −0.072 * | 0.031 | −0.037 | 0.037 | |
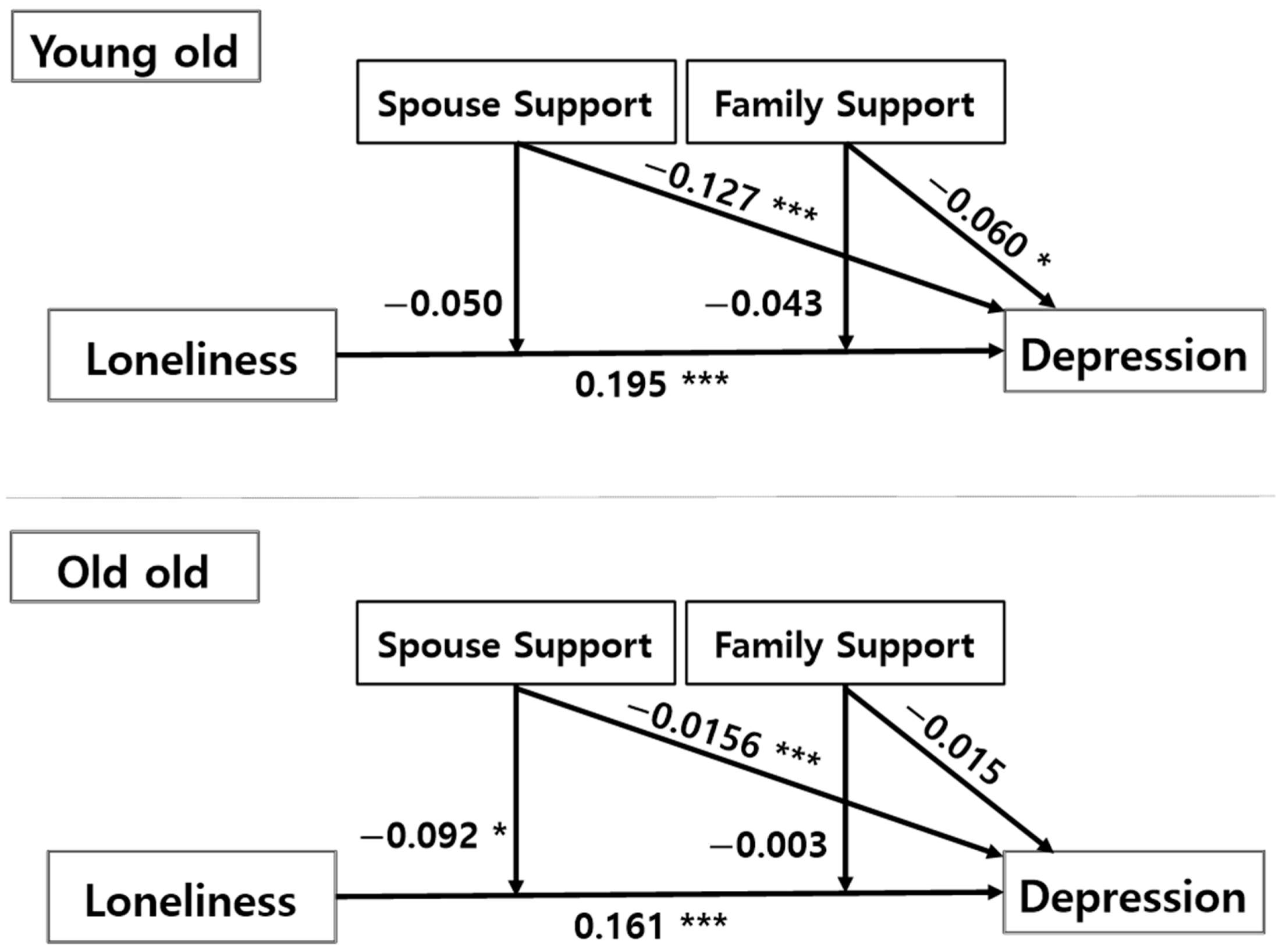
| Independent Variable | Loneliness(A) | 0.195 *** | 0.018 | 0.161 *** | 0.026 |
| Moderator Variable | Spouse Support(B) | −0.127 *** | 0.029 | −0.156 *** | 0.032 |
| Family Support(C) | −0.060 * | 0.027 | 0.015 | 0.033 | |
| Interaction | A × B | −0.050 | 0.036 | −0.092 * | 0.042 |
| A × C | −0.043 | 0.032 | 0.003 | 0.041 | |
| R2 | 0.249 | 0.187 | |||
| F(sig.) | 32.941 *** | 15.816 *** | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, H.; Cho, H.J.; Cho, S.; Ryu, J.; Kim, S. The Moderating Effect of Social Support between Loneliness and Depression: Differences between the Young-Old and the Old-Old. Int. J. Environ. Res. Public Health 2022, 19, 2322. https://doi.org/10.3390/ijerph19042322
Son H, Cho HJ, Cho S, Ryu J, Kim S. The Moderating Effect of Social Support between Loneliness and Depression: Differences between the Young-Old and the Old-Old. International Journal of Environmental Research and Public Health. 2022; 19(4):2322. https://doi.org/10.3390/ijerph19042322
Chicago/Turabian StyleSon, Hyegyeong, Heeran J. Cho, Sunghwan Cho, Juhyun Ryu, and Sunghee Kim. 2022. "The Moderating Effect of Social Support between Loneliness and Depression: Differences between the Young-Old and the Old-Old" International Journal of Environmental Research and Public Health 19, no. 4: 2322. https://doi.org/10.3390/ijerph19042322
APA StyleSon, H., Cho, H. J., Cho, S., Ryu, J., & Kim, S. (2022). The Moderating Effect of Social Support between Loneliness and Depression: Differences between the Young-Old and the Old-Old. International Journal of Environmental Research and Public Health, 19(4), 2322. https://doi.org/10.3390/ijerph19042322






