Mobile Applications in Mood Disorders and Mental Health: Systematic Search in Apple App Store and Google Play Store and Review of the Literature
Abstract
:1. Introduction
2. Materials and Methods
2.1. App Search and Filtering
2.2. App Characterization
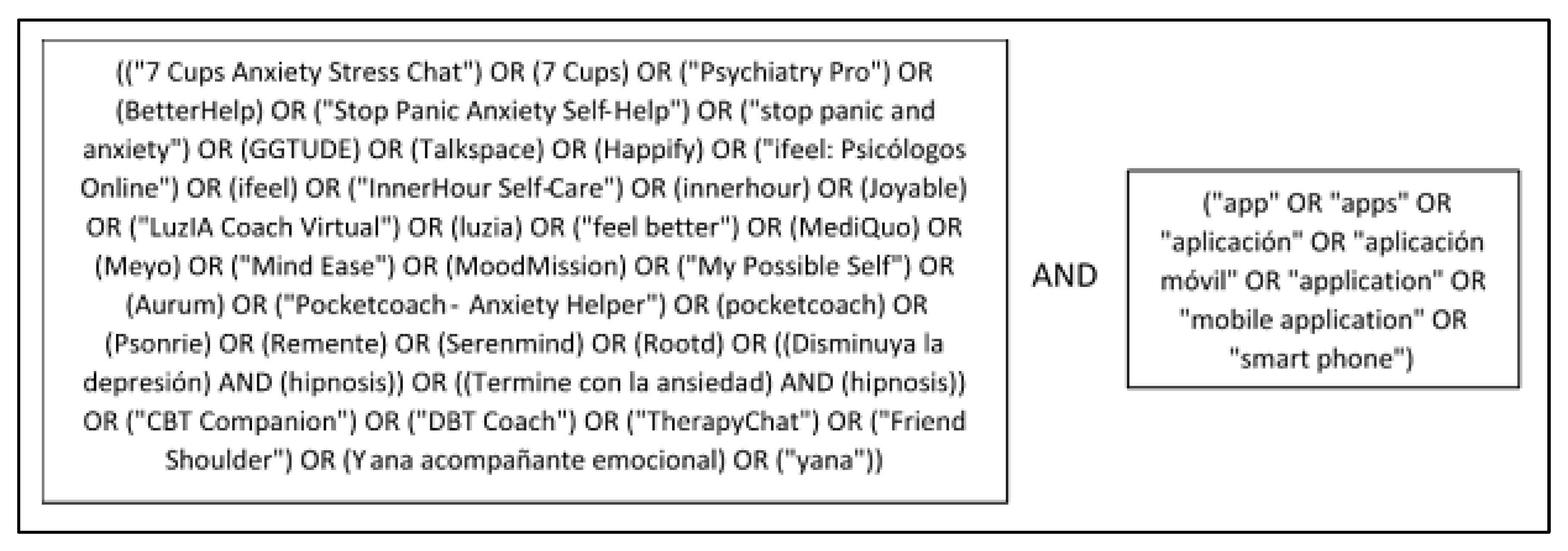
2.3. Publication Search
3. Results
4. Discussion
4.1. Principal Findings
4.2. Safety and Ethical Considerations of MHapps
4.3. Effectiveness and Evidence of MHapps
4.4. Access to and Adoption of Mobile Mental Health Interventions
4.5. Implications for Further Research and Policy
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ditrendia. Informe Mobile En España y En Mundo 2019; Report; Ditendia (Ditrendia Digital Marketing Trends): Madrid, Spain, 2019; Available online: https://mktefa.ditrendia.es/informe-mobile-2019 (accessed on 6 June 2021).
- Spanish National Observatory for Telecommunications and the Information Society (ONTSI). Las TIC En Los Hogares Españoles. Estudio de Demanda y Uso de Servicios de Telecomunicaciones y Sociedad de La Información; ONTSI: Madrid, Spain, 2019.
- Research2guidance. MHealth Economics 2017 Report: Status and Trends in Digital Health; Report; Research2guidance: Berlin, Germany, 2017; Available online: https://research2guidance.com/product/diga-in-germany-entering-the-german-market-with-a-digital-health-solution/ (accessed on 6 June 2021).
- Martinengo, L.; Van Galen, L.; Lum, E.; Kowalski, M.; Subramaniam, M.; Car, J. Suicide prevention and depression apps’ suicide risk assessment and management: A systematic assessment of adherence to clinical guidelines. BMC Med. 2019, 17, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, K.M.; Burrows, V. Ethical and Safety Concerns Regarding the Use of Mental Health–Related Apps in Counseling: Considerations for Counselors. J. Technol. Behav. Sci. 2021, 6, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Mathews, S.C.; McShea, M.J.; Hanley, C.; Ravitz, A.; Labrique, A.B.; Cohen, A.B. Digital health: A path to validation. NPJ Digit. Med. 2019, 2, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ologeanu-Taddei, R. Assessment of mHealth Interventions: Need for New Studies, Methods, and Guidelines for Study Designs. JMIR Med. Informa. 2020, 8, e21874. [Google Scholar] [CrossRef] [PubMed]
- Marcolino, M.S.; Oliveira, J.A.Q.; D’Agostino, M.; Ribeiro, A.L.; Alkmim, M.B.M.; Novillo-Ortiz, D. The Impact of mHealth Interventions: Systematic Review of Systematic Reviews. JMIR mHealth uHealth 2018, 6, e23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Parker, L.; Bero, L.; Gillies, D.; Raven, M.; Mintzes, B.; Jureidini, J.; Grundy, Q. Mental Health Messages in Prominent Mental Health Apps. Ann. Fam. Med. 2018, 16, 338–342. [Google Scholar] [CrossRef] [Green Version]
- Aboujaoude, E.; Salame, W.; Naim, L. Telemental health: A status update. World Psychiatry 2015, 14, 223–230. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Firth, J.; Huckvale, K.; Larsen, M.E.; Cosco, T.D.; Carney, R.; Chan, S.; Pratap, A.; Yellowlees, P.; Wykes, T.; et al. The Emerging Imperative for a Consensus Approach Toward the Rating and Clinical Recommendation of Mental Health Apps. J. Nerv. Ment. Dis. 2018, 206, 662–666. [Google Scholar] [CrossRef]
- Torous, J.; Wisniewski, H.; Bird, B.; Carpenter, E.; David, G.; Elejalde, E.; Fulford, D.; Guimond, S.; Hays, R.; Henson, P.; et al. Creating a Digital Health Smartphone App and Digital Phenotyping Platform for Mental Health and Diverse Healthcare Needs: An Interdisciplinary and Collaborative Approach. J. Technol. Behav. Sci. 2019, 4, 73–85. [Google Scholar] [CrossRef] [Green Version]
- Neary, M.; Schueller, S.M. State of the Field of Mental Health Apps. Cogn. Behav. Pr. 2018, 25, 531–537. [Google Scholar] [CrossRef]
- Lecomte, T.; Potvin, S.; Corbière, M.; Guay, S.; Samson, C.; Cloutier, B.; Francoeur, A.; Pennou, A.; Khazaal, Y. Mobile Apps for Mental Health Issues: Meta-Review of Meta-Analyses. JMIR mHealth uHealth 2020, 8, e17458. [Google Scholar] [CrossRef] [PubMed]
- Knowles, S.E.; Toms, G.; Sanders, C.; Bee, P.; Lovell, K.; Rennick-Egglestone, S.; Coyle, D.; Kennedy, C.; Littlewood, E.; Kessler, D.; et al. Qualitative Meta-Synthesis of User Experience of Computerised Therapy for Depression and Anxiety. PLoS ONE 2014, 9, e84323. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Sijbrandij, M.; Koole, S.L.; Andersson, G.; Beekman, A.T.; Iii, C.F.R. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: A meta-analysis of direct comparisons. World Psychiatry 2013, 12, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Torous, J.; Nicholas, J.; Carney, R.; Rosenbaum, S.; Sarris, J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J. Affect. Disord. 2017, 218, 15–22. [Google Scholar] [CrossRef]
- Firth, J.; Torous, J.; Nicholas, J.; Carney, R.; Pratap, A.; Rosenbaum, S.; Sarris, J. The Efficacy of Smartphone-Based Mental Health Interventions for Depressive Symptoms: A Meta-Analysis of Randomized Controlled Trials. World Psychiatry Off. J. World Psychiatr. Assoc. WPA 2017, 16, 287–298. [Google Scholar] [CrossRef]
- Msc, B.H.; Forchuk, C.; O’Regan, T. The use of technology for mental healthcare delivery among older adults with depressive symptoms: A systematic literature review. Int. J. Ment. Health Nurs. 2019, 28, 657–670. [Google Scholar] [CrossRef]
- Deady, M.; Choi, I.; Calvo, R.A.; Glozier, N.; Christensen, H.; Harvey, S.B. eHealth interventions for the prevention of depression and anxiety in the general population: A systematic review and meta-analysis. BMC Psychiatry 2017, 17, 310. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Staples, P.; Shanahan, M.; Lin, C.; Peck, P.; Keshavan, M.; Onnela, J.-P. Utilizing a Personal Smartphone Custom App to Assess the Patient Health Questionnaire-9 (PHQ-9) Depressive Symptoms in Patients With Major Depressive Disorder. JMIR Ment. Health 2015, 2, e8. [Google Scholar] [CrossRef] [Green Version]
- Khademian, F.; Aslani, A.; Bastani, P. The effects of mobile apps on stress, anxiety, and depression: Overview of systematic reviews. Int. J. Technol. Assess. Health Care 2021, 37, e4. [Google Scholar] [CrossRef]
- Liu, J.-Y.; Xu, K.-K.; Zhu, G.-L.; Zhang, Q.-Q.; Li, X.-M. Effects of smartphone-based interventions and monitoring on bipolar disorder: A systematic review and meta-analysis. World J. Psychiatry 2020, 10, 272–285. [Google Scholar] [CrossRef] [PubMed]
- Melcher, J.; Camacho, E.; Lagan, S.; Torous, J. College student engagement with mental health apps: Analysis of barriers to sustained use. J. Am. Coll. Health 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Liverpool, S.; Mota, C.P.; Sales, C.M.D.; Čuš, A.; Carletto, S.; Hancheva, C.; Sousa, S.; Cerón, S.C.; Moreno-Peral, P.; Pietrabissa, G.; et al. Engaging Children and Young People in Digital Mental Health Interventions: Systematic Review of Modes of Delivery, Facilitators, and Barriers. J. Med. Internet Res. 2020, 22, e16317. [Google Scholar] [CrossRef] [PubMed]
- Borghouts, J.; Eikey, E.; Mark, G.; De Leon, C.; Schueller, S.M.; Schneider, M.; Stadnick, N.; Zheng, K.; Mukamel, D.; Sorkin, D.H. Barriers to and Facilitators of User Engagement With Digital Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2021, 23, e24387. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.G.; Stott, R.; Bromwich, N.; Oblak, S.K.; Espie, C.A.; Rose, J.B. Determinants of and barriers to adoption of digital therapeutics for mental health at scale in the NHS. BMJ Innov. 2020, 6, 92–98. [Google Scholar] [CrossRef]
- Grainger, R.; Devan, H.; Sangelaji, B.; Hay-Smith, J. Issues in reporting of systematic review methods in health app-focused reviews: A scoping review. Health Inform. J. 2020, 26, 2930–2945. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.M.; Dunstan, D.A.; Bartik, W. Apps With Maps—Anxiety and Depression Mobile Apps With Evidence-Based Frameworks: Systematic Search of Major App Stores. JMIR Ment. Health 2020, 7, e16525. [Google Scholar] [CrossRef]
- Wyatt, J.C. How can clinicians, specialty societies and others evaluate and improve the quality of apps for patient use? BMC Med. 2018, 16, 225. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- NIMH. Bipolar Disorder. Available online: https://www.nimh.nih.gov/health/topics/bipolar-disorder (accessed on 31 January 2022).
- Baumel, A.; Correll, C.U.; Birnbaum, M. Adaptation of a peer based online emotional support program as an adjunct to treatment for people with schizophrenia-spectrum disorders. Internet Interv. 2016, 4, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Baumel, A.; Schueller, S.M.; Torous, J. Adjusting an Available Online Peer Support Platform in a Program to Supplement the Treatment of Perinatal Depression and Anxiety. JMIR Ment. Health 2016, 3, e11. [Google Scholar] [CrossRef]
- Baumel, A. Online emotional support delivered by trained volunteers: Users’ satisfaction and their perception of the service compared to psychotherapy. J. Ment. Health 2015, 24, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Baumel, A.; Tinkelman, A.; Mathur, N.; Kane, J.M. Digital Peer-Support Platform (7Cups) as an Adjunct Treatment for Women With Postpartum Depression: Feasibility, Acceptability, and Preliminary Efficacy Study. JMIR mHealth uHealth 2018, 6, e38. [Google Scholar] [CrossRef] [PubMed]
- Marcelle, E.T.; Nolting, L.; Hinshaw, S.P.; Aguilera, A. Effectiveness of a Multimodal Digital Psychotherapy Platform for Adult Depression: A Naturalistic Feasibility Study. JMIR mHealth uHealth 2019, 7, e10948. [Google Scholar] [CrossRef]
- Rizvi, S.L.; Hughes, C.D.; Thomas, M.C. The DBT Coach mobile application as an adjunct to treatment for suicidal and self-injuring individuals with borderline personality disorder: A preliminary evaluation and challenges to client utilization. Psychol. Serv. 2016, 13, 380–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizvi, S.L.; Dimeff, L.A.; Skutch, J.; Carroll, D.; Linehan, M.M. A Pilot Study of the DBT Coach: An Interactive Mobile Phone Application for Individuals With Borderline Personality Disorder and Substance Use Disorder. Behav. Ther. 2011, 42, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Cerea, S.; Ghisi, M.; Bottesi, G.; Carraro, E.; Broggio, D.; Doron, G. Reaching reliable change using short, daily, cognitive training exercises delivered on a mobile application: The case of Relationship Obsessive Compulsive Disorder (ROCD) symptoms and cognitions in a subclinical cohort. J. Affect. Disord. 2020, 276, 775–787. [Google Scholar] [CrossRef]
- Cerea, S.; Ghisi, M.; Bottesi, G.; Manoli, T.; Carraro, E.; Doron, G. Cognitive Behavioral Training Using a Mobile Application Reduces Body Image-Related Symptoms in High-Risk Female University Students: A Randomized Controlled Study. Behav. Ther. 2021, 52, 170–182. [Google Scholar] [CrossRef]
- Roncero, M.; Belloch, A.; Doron, G. Can Brief, Daily Training Using a Mobile App Help Change Maladaptive Beliefs? Crossover Randomized Controlled Trial. JMIR mHealth uHealth 2019, 7, e11443. [Google Scholar] [CrossRef] [Green Version]
- Giraldo-O’Meara, M.; Doron, G. Can self-esteem be improved using short daily training on mobile applications? Examining real world data ofGGSelf-esteem users. Clin. Psychol. 2021, 25, 131–139. [Google Scholar] [CrossRef]
- Pascual-Vera, B.; Roncero, M.; Doron, G.; Belloch, A. Assisting relapse prevention in OCD using a novel mobile app–based intervention: A case report. Bull. Menn. Clin. 2018, 82, 390–406. [Google Scholar] [CrossRef]
- Aboody, D.; Siev, J.; Doron, G. Building resilience to body image triggers using brief cognitive training on a mobile application: A randomized controlled trial. Behav. Res. Ther. 2020, 134, 103723. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.F.; Olah, M.S.; Williams, A.L.; Parks, A.C.; Pressman, S.D. Effect of Brief Biofeedback via a Smartphone App on Stress Recovery: Randomized Experimental Study. JMIR Serious Games 2019, 7, e15974. [Google Scholar] [CrossRef] [PubMed]
- Parks, A.C.; Williams, A.L.; Kackloudis, G.M.; Stafford, J.L.; Boucher, E.M.; Honomichl, R.D. The Effects of a Digital Well-Being Intervention on Patients With Chronic Conditions: Observational Study. J. Med. Internet Res. 2020, 22, e16211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boucher, E.M.; McNaughton, E.C.; Harake, N.; Stafford, J.L.; Parks, A.C. The Impact of a Digital Intervention (Happify) on Loneliness During COVID-19: Qualitative Focus Group. JMIR Ment. Health 2021, 8, e26617. [Google Scholar] [CrossRef]
- Dryman, M.T.; McTeague, L.M.; Olino, T.M.; Heimberg, R.G. Evaluation of an open-access CBT-based Internet program for social anxiety: Patterns of use, retention, and outcomes. J. Consult. Clin. Psychol. 2017, 85, 988–999. [Google Scholar] [CrossRef]
- Bakker, D.; Kazantzis, N.; Rickwood, D.; Rickard, N. Development and Pilot Evaluation of Smartphone-Delivered Cognitive Behavior Therapy Strategies for Mood- and Anxiety-Related Problems: MoodMission. Cogn. Behav. Pr. 2018, 25, 496–514. [Google Scholar] [CrossRef]
- Aizenstros, A.; Bakker, D.; Hofmann, S.G.; Curtiss, J.; Kazantzis, N. Engagement with smartphone-delivered behavioural activation interventions: A study of the MoodMission smartphone application. Behav. Cogn. Psychother. 2021, 49, 569–581. [Google Scholar] [CrossRef]
- Bakker, D.; Kazantzis, N.; Rickwood, D.; Rickard, N. A randomized controlled trial of three smartphone apps for enhancing public mental health. Behav. Res. Ther. 2018, 109, 75–83. [Google Scholar] [CrossRef]
- Marshall, J.M.; Dunstan, D.A.; Bartik, W. Effectiveness of Using Mental Health Mobile Apps as Digital Antidepressants for Reducing Anxiety and Depression: Protocol for a Multiple Baseline Across-Individuals Design. JMIR Res. Protoc. 2020, 9, e17159. [Google Scholar] [CrossRef]
- Bakker, D.; Rickard, N. Engagement with a cognitive behavioural therapy mobile phone app predicts changes in mental health and wellbeing: MoodMission. Aust. Psychol. 2019, 54, 245–260. [Google Scholar] [CrossRef]
- Hull, T.D.; Malgaroli, M.; Connolly, P.S.; Feuerstein, S.; Simon, N.M. Two-way messaging therapy for depression and anxiety: Longitudinal response trajectories. BMC Psychiatry 2020, 20, 297. [Google Scholar] [CrossRef] [PubMed]
- Bantilan, N.; Malgaroli, M.; Ray, B.; Hull, T.D. Just in time crisis response: Suicide alert system for telemedicine psychotherapy settings. Psychother. Res. 2021, 31, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Malgaroli, M.; Hull, T.D.; Stirman, S.W.; Resick, P. Message Delivery for the Treatment of Posttraumatic Stress Disorder: Longitudinal Observational Study of Symptom Trajectories. J. Med. Internet Res. 2020, 22, e15587. [Google Scholar] [CrossRef] [PubMed]
- Hull, T.D.; Mahan, K. A Study of Asynchronous Mobile-Enabled SMS Text Psychotherapy. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2017, 23, 240–247. [Google Scholar] [CrossRef]
- Hull, T.D.; Levine, J.; Bantilan, N.; Desai, A.N.; Majumder, M.S. Analyzing Digital Evidence From a Telemental Health Platform to Assess Complex Psychological Responses to the COVID-19 Pandemic: Content Analysis of Text Messages. JMIR Form. Res. 2021, 5, e26190. [Google Scholar] [CrossRef]
- Bowie-DaBreo, D.; I Sünram-Lea, S.; Sas, C.; Iles-Smith, H. Evaluation of Treatment Descriptions and Alignment With Clinical Guidance of Apps for Depression on App Stores: Systematic Search and Content Analysis. JMIR Form. Res. 2020, 4, e14988. [Google Scholar] [CrossRef]
- Drissi, N.; Ouhbi, S.; Idrissi, M.A.J.; Ghogho, M. An analysis on self-management and treatment-related functionality and characteristics of highly rated anxiety apps. Int. J. Med. Inform. 2020, 141, 104243. [Google Scholar] [CrossRef]
- Lagan, S.; Ramakrishnan, A.; Lamont, E.; Ramakrishnan, A.; Frye, M.; Torous, J. Digital health developments and drawbacks: A review and analysis of top-returned apps for bipolar disorder. Int. J. Bipolar Disord. 2020, 8, 39. [Google Scholar] [CrossRef]
- Marshall, J.M.; Dunstan, D.; Bartik, W. The Digital Psychiatrist: In Search of Evidence-Based Apps for Anxiety and Depression. Front. Psychiatry 2019, 10, 831. [Google Scholar] [CrossRef]
- Yin, H.; Wardenaar, K.J.; Wang, Y.; Wang, N.; Chen, W.; Zhang, Y.; Xu, G.; Schoevers, R.A. Mobile Mental Health Apps in China: Systematic App Store Search. J. Med. Internet Res. 2020, 22, e14915. [Google Scholar] [CrossRef]
- Alhuwail, D.; Albaj, R.; Ahmad, F.; Aldakheel, K. The state of mental digi-therapeutics: A systematic assessment of depression and anxiety apps available for Arabic speakers. Int. J. Med. Inform. 2020, 135, 104056. [Google Scholar] [CrossRef] [PubMed]
- Grau-Corral, I.; Gascon, P.; Iii, F.J.G.; Kostov, B.; Almirall, A.S. Availability of Spanish-Language Medical Apps in Google Play and the App Store: Retrospective Descriptive Analysis Using Google Tools. JMIR mHealth uHealth 2020, 8, e17139. [Google Scholar] [CrossRef] [PubMed]
- Lorca-Cabrera, J.; Martí-Arques, R.; Albacar-Riobóo, N.; Raigal-Aran, L.; Roldan-Merino, J.; Ferré-Grau, C. Mobile Applications for Caregivers of Individuals with Chronic Conditions and/or Diseases: Quantitative Content Analysis. Int. J. Med. Inform. 2021, 145, 104310. [Google Scholar] [CrossRef] [PubMed]
- Feldman, N.; Back, D.; Boland, R.; Torous, J. A systematic review of mHealth application interventions for peripartum mood disorders: Trends and evidence in academia and industry. Arch. Women’s Ment. Health 2021, 24, 881–892. [Google Scholar] [CrossRef]
- Wasil, A.R.; Patel, R.; Cho, J.Y.; Shingleton, R.M.; Weisz, J.R.; DeRubeis, R.J. Smartphone apps for eating disorders: A systematic review of evidence-based content and application of user-adjusted analyses. Int. J. Eat. Disord. 2021, 54, 690–700. [Google Scholar] [CrossRef]
- Portenhauser, A.A.; Terhorst, Y.; Schultchen, D.; Sander, L.B.; Denkinger, M.D.; Stach, M.; Waldherr, N.; Dallmeier, D.; Baumeister, H.; Messner, E.-M. Mobile Apps for Older Adults: Systematic Search and Evaluation Within Online Stores. JMIR Aging 2021, 4, e23313. [Google Scholar] [CrossRef]
- Păsărelu, C.R.; Andersson, G.; Dobrean, A. Attention-deficit/ hyperactivity disorder mobile apps: A systematic review. Int. J. Med. Inform. 2020, 138, 104133. [Google Scholar] [CrossRef]
- Flors-Sidro, J.J.; Househ, M.; Abd-Alrazaq, A.; Vidal-Alaball, J.; Fernandez-Luque, L.; Sanchez-Bocanegra, C.L. Analysis of Diabetes Apps to Assess Privacy-Related Permissions: Systematic Search of Apps. JMIR Diabetes 2021, 6, e16146. [Google Scholar] [CrossRef]
- Abdullah, S.; Choudhury, T. Sensing Technologies for Monitoring Serious Mental Illnesses. IEEE MultiMedia 2018, 25, 61–75. [Google Scholar] [CrossRef]
- Baxter, C.; Carroll, J.-A.; Keogh, B.; Vandelanotte, C. Assessment of Mobile Health Apps Using Built-In Smartphone Sensors for Diagnosis and Treatment: Systematic Survey of Apps Listed in International Curated Health App Libraries. JMIR MHealth UHealth 2020, 8, e16741. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Monteith, S.; Bauer, R.; Whybrow, P.C.; Geddes, J. Ethical Perspectives on Recommending Digital Technology for Patients with Mental Illness. Int. J. Bipolar Disord. 2017, 5, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thornton, L.K.; Kay-Lambkin, F.J. Specific Features of Current and Emerging Mobile Health Apps: User Views among People with and without Mental Health Problems. mHealth 2018, 4, 56. [Google Scholar] [CrossRef] [PubMed]
- Klasnja, P.; Consolvo, S.; Choudhury, T.; Beckwith, R.; Hightower, J. Exploring Privacy Concerns about Personal Sensing. In Pervasive Computing; Tokuda, H., Beigl, M., Friday, A., Brush, A.J.B., Tobe, Y., Eds.; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2009; Volume 5538, pp. 176–183. [Google Scholar] [CrossRef]
- Torous, J.; Wisniewski, H.; Liu, G.; Keshavan, M. Mental Health Mobile Phone App Usage, Concerns, and Benefits Among Psychiatric Outpatients: Comparative Survey Study. JMIR Ment. Health 2018, 5, e11715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Matteo, D.; Fine, A.; Fotinos, K.; Rose, J.; Katzman, M. Patient Willingness to Consent to Mobile Phone Data Collection for Mental Health Apps: Structured Questionnaire. JMIR Ment. Health 2018, 5, e56. [Google Scholar] [CrossRef] [Green Version]
- Hendrikoff, L.; Kambeitz-Ilankovic, L.; Pryss, R.; Senner, F.; Falkai, P.; Pogarell, O.; Hasan, A.; Peters, H. Prospective acceptance of distinct mobile mental health features in psychiatric patients and mental health professionals. J. Psychiatr. Res. 2019, 109, 126–132. [Google Scholar] [CrossRef]
- Dowrick, C.; Frances, A. Medicalising unhappiness: New classification of depression risks more patients being put on drug treatment from which they will not benefit. BMJ 2013, 347, f7140. [Google Scholar] [CrossRef]
- Martinez-Martin, N.; Kreitmair, K. Ethical Issues for Direct-to-Consumer Digital Psychotherapy Apps: Addressing Accountability, Data Protection, and Consent. JMIR Ment. Health 2018, 5, e32. [Google Scholar] [CrossRef]
- Miner, A.S.; Milstein, A.; Schueller, S.; Hegde, R.; Mangurian, C.; Linos, E. Smartphone-Based Conversational Agents and Responses to Questions About Mental Health, Interpersonal Violence, and Physical Health. JAMA Intern. Med. 2016, 176, 619–625. [Google Scholar] [CrossRef]
- Kretzschmar, K.; Tyroll, H.; Pavarini, G.; Manzini, A.; Singh, I. NeurOx Young People’s Advisory Group Can Your Phone Be Your Therapist? Young People’s Ethical Perspectives on the Use of Fully Automated Conversational Agents (Chatbots) in Mental Health Support. Biomed. Inform. Insights 2019, 11, 1178222619829083. [Google Scholar] [CrossRef] [Green Version]
- Clay, R. Using Apps with Your Patients. Available online: https://www.apa.org/monitor/2020/04/career-using-apps (accessed on 6 June 2021).
- Alyami, M.; Giri, B.; Alyami, H.; Sundram, F. Social anxiety apps: A systematic review and assessment of app descriptors across mobile store platforms. Évid. Based Ment. Health 2017, 20, 65–70. [Google Scholar] [CrossRef]
- Wang, K.; Varma, D.S.; Prosperi, M. A systematic review of the effectiveness of mobile apps for monitoring and management of mental health symptoms or disorders. J. Psychiatr. Res. 2018, 107, 73–78. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Geddes, J.; Gitlin, M.; Grof, P.; Kessing, L.V.; Monteith, S.; Faurholt-Jepsen, M.; Severus, E.; Whybrow, P.C. Smartphones in mental health: A critical review of background issues, current status and future concerns. Int. J. Bipolar Disord. 2020, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Foster, K.R.; Callans, D.J. Smartphone Apps Meet Evidence-Based Medicine: The Future of Medicine May (Or May Not) Be in Your Smartphone. IEEE Pulse 2017, 8, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Yuste, R.; Goering, S.; Arcas, B.A.Y.; Bi, G.-Q.; Carmena, J.M.; Carter, A.; Fins, J.J.; Friesen, P.; Gallant, J.; Huggins, J.E.; et al. Four ethical priorities for neurotechnologies and AI. Nature 2017, 551, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baumel, A.; Muench, F.; Edan, S.; Kane, J.M. Objective User Engagement With Mental Health Apps: Systematic Search and Panel-Based Usage Analysis. J. Med. Internet Res. 2019, 21, e14567. [Google Scholar] [CrossRef] [Green Version]
- Huckvale, K.; Nicholas, J.; Torous, J.; Larsen, M.E. Smartphone apps for the treatment of mental health conditions: Status and considerations. Curr. Opin. Psychol. 2020, 36, 65–70. [Google Scholar] [CrossRef]
- About One Mind PsyberGuide. One Mind PsyberGuide. Available online: https://onemindpsyberguide.org/about-psyberguide/ (accessed on 6 June 2021).
- NHS Apps Library—NHS. Available online: https://www.nhs.uk/apps-library/?page=1 (accessed on 6 June 2021).
- FDA/CE Certified Apps Directory. Available online: https://apps.healthskouts.com/ (accessed on 6 June 2021).
- Torous, J.B.; Chan, S.R.; Gipson, S.Y.-M.T.; Kim, J.; Nguyen, T.-Q.; Luo, J.; Wang, P. A Hierarchical Framework for Evaluation and Informed Decision Making Regarding Smartphone Apps for Clinical Care. Psychiatr. Serv. 2018, 69, 498–500. [Google Scholar] [CrossRef]
- Stoyanov, S.R.; Hides, L.; Kavanagh, D.J.; Wilson, H. Development and Validation of the User Version of the Mobile Application Rating Scale (uMARS). JMIR mHealth uHealth 2016, 4, e72. [Google Scholar] [CrossRef] [Green Version]
- mHealth Apps. Available online: https://ticsalutsocial.cat/es/apps/ (accessed on 6 June 2021).
- Segui, F.L.; Bufill, C.P.; Gimenez, N.A.; Roldan, J.M.; Cuyas, F.G. The Prescription of Mobile Apps by Primary Care Teams: A Pilot Project in Catalonia. JMIR mHealth uHealth 2018, 6, e10701. [Google Scholar] [CrossRef]
- Research2guidance. DiGA in Germany: Entering the German Market with a Digital Health Solution; Report; Research2guidance: Berlin, Germany, 2021; Available online: https://research2guidance.com/product/mhealth-economics-2017-current-status-and-future-trends-in-mobile-health/ (accessed on 6 June 2021).
- Digital Therapeutics (DTx). Available online: https://edps.europa.eu/press-publications/publications/techsonar/digital-therapeutics-dtx_en (accessed on 2 February 2022).
- Patel, N.A.; Butte, A.J. Characteristics and challenges of the clinical pipeline of digital therapeutics. npj Digit. Med. 2020, 3, 159. [Google Scholar] [CrossRef]
- Babic, B.; Gerke, S.; Evgeniou, T.; Cohen, I.G. Algorithms on Regulatory Lockdown in Medicine. Science 2019, 366, 1202–1204. [Google Scholar] [CrossRef] [PubMed]

| List of Exclusion Criteria |
|---|
|
| Applications with Published Evidence | ||||
|---|---|---|---|---|
| Name | Type | Publications | Objective | Population |
| 7 Cups: Anxiety & Stress Chat | Chat and e-counselling | 4 published articles [34,35,36,37] | Provide free active listening and paid online therapy | Various patient types, incl. stress, anxiety, depression, etc. |
| BetterHelp: Online Counseling & Therapy | E-counselling | 1 published article [38] | Provide professional counselling, chat, and video messaging with therapist | Various patient types, incl. stress, anxiety, depression, etc. |
| DBT Coach | Cognitive behavioural therapy (CBT) | 2 published articles [39,40] | Dairy, CBT/DBT (dialectical behavior therapy) exercises, peer groups | Various patient types, incl. stress, anxiety, depression, etc. |
| GGtude OCD Anxiety & Depression | CBT | 6 published articles [41,42,43,44,45,46] | Applying CBT methods to break unhelpful thought patterns | OCD, anxiety, depression |
| Happify | Tracker, meditation, exercises | 3 published articles [47,48,49] | Changing negative thought patterns, tracker, and activities/videos | Various patient types, incl. stress, anxiety, depression, etc. |
| Joyable: An AbleTo Program | CBT | 1 published article [50] | 2-month plan to deliver personalized CBT programs and support from coaches | Various patient types, incl. stress, anxiety, depression, etc. |
| MoodMission—Cope with Stress, Moods & Anxiety | Tracker, meditation, exercises | 5 published articles [51,52,53,54,55] | Mood boosting activities, meditation, relaxation, exercise, affirmations, yoga, gratitude | Low mood, depression, stress, anxiety |
| Talkspace Therapy & Counseling | E-counselling | 5 published articles [56,57,58,59,60] | Provide professional counselling, chat, and video messaging with therapist | Various patient types, incl. stress, anxiety, depression, etc. |
| Depression | 8 |
| Postpartum depression | (2) |
| Schizophrenia-spectrum disorders | 1 |
| Anxiety | 7 |
| Social anxiety | (1) |
| Borderline personality disorder | 2 |
| OCD * | 3 |
| Relationship OCD | (1) |
| Body image disorders | 2 |
| Suicide alert system | 1 |
| Self esteem | 1 |
| Loneliness | 1 |
| Response to lab-induced stressor | 1 |
| Mental wellbeing of patients with chronic diseases | 1 |
| Posttraumatic stress disorder | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eis, S.; Solà-Morales, O.; Duarte-Díaz, A.; Vidal-Alaball, J.; Perestelo-Pérez, L.; Robles, N.; Carrion, C. Mobile Applications in Mood Disorders and Mental Health: Systematic Search in Apple App Store and Google Play Store and Review of the Literature. Int. J. Environ. Res. Public Health 2022, 19, 2186. https://doi.org/10.3390/ijerph19042186
Eis S, Solà-Morales O, Duarte-Díaz A, Vidal-Alaball J, Perestelo-Pérez L, Robles N, Carrion C. Mobile Applications in Mood Disorders and Mental Health: Systematic Search in Apple App Store and Google Play Store and Review of the Literature. International Journal of Environmental Research and Public Health. 2022; 19(4):2186. https://doi.org/10.3390/ijerph19042186
Chicago/Turabian StyleEis, Sophie, Oriol Solà-Morales, Andrea Duarte-Díaz, Josep Vidal-Alaball, Lilisbeth Perestelo-Pérez, Noemí Robles, and Carme Carrion. 2022. "Mobile Applications in Mood Disorders and Mental Health: Systematic Search in Apple App Store and Google Play Store and Review of the Literature" International Journal of Environmental Research and Public Health 19, no. 4: 2186. https://doi.org/10.3390/ijerph19042186
APA StyleEis, S., Solà-Morales, O., Duarte-Díaz, A., Vidal-Alaball, J., Perestelo-Pérez, L., Robles, N., & Carrion, C. (2022). Mobile Applications in Mood Disorders and Mental Health: Systematic Search in Apple App Store and Google Play Store and Review of the Literature. International Journal of Environmental Research and Public Health, 19(4), 2186. https://doi.org/10.3390/ijerph19042186








