Thirty-Year Urbanization Trajectories and Obesity in Modernizing China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Sample Selection
2.3. Urbanization Trajectories
2.4. Dependent Variables
2.5. Covariates
2.6. Statistical Analysis
3. Results
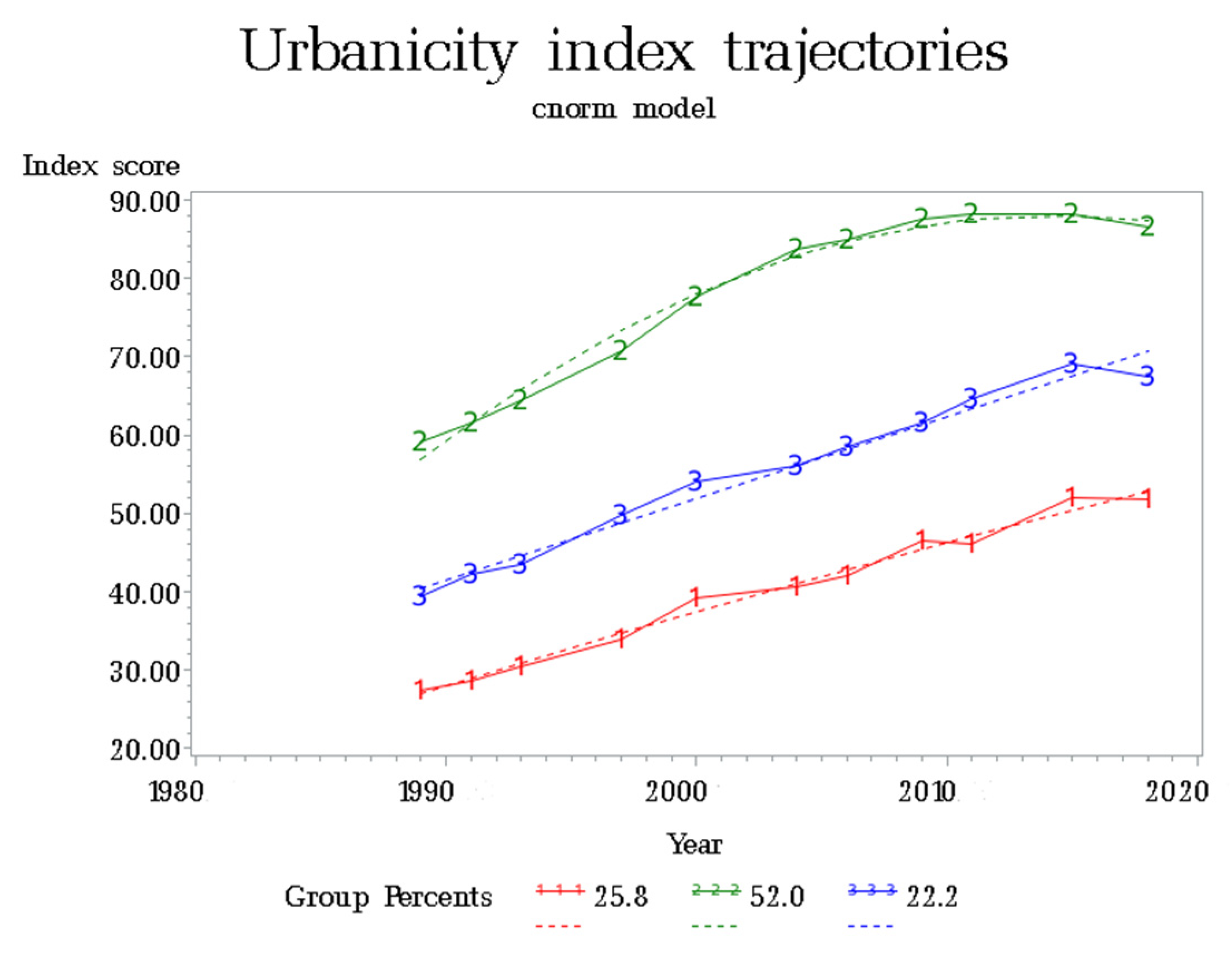
3.1. Urbanization Trajectories
3.2. Characteristics of Entry Participants
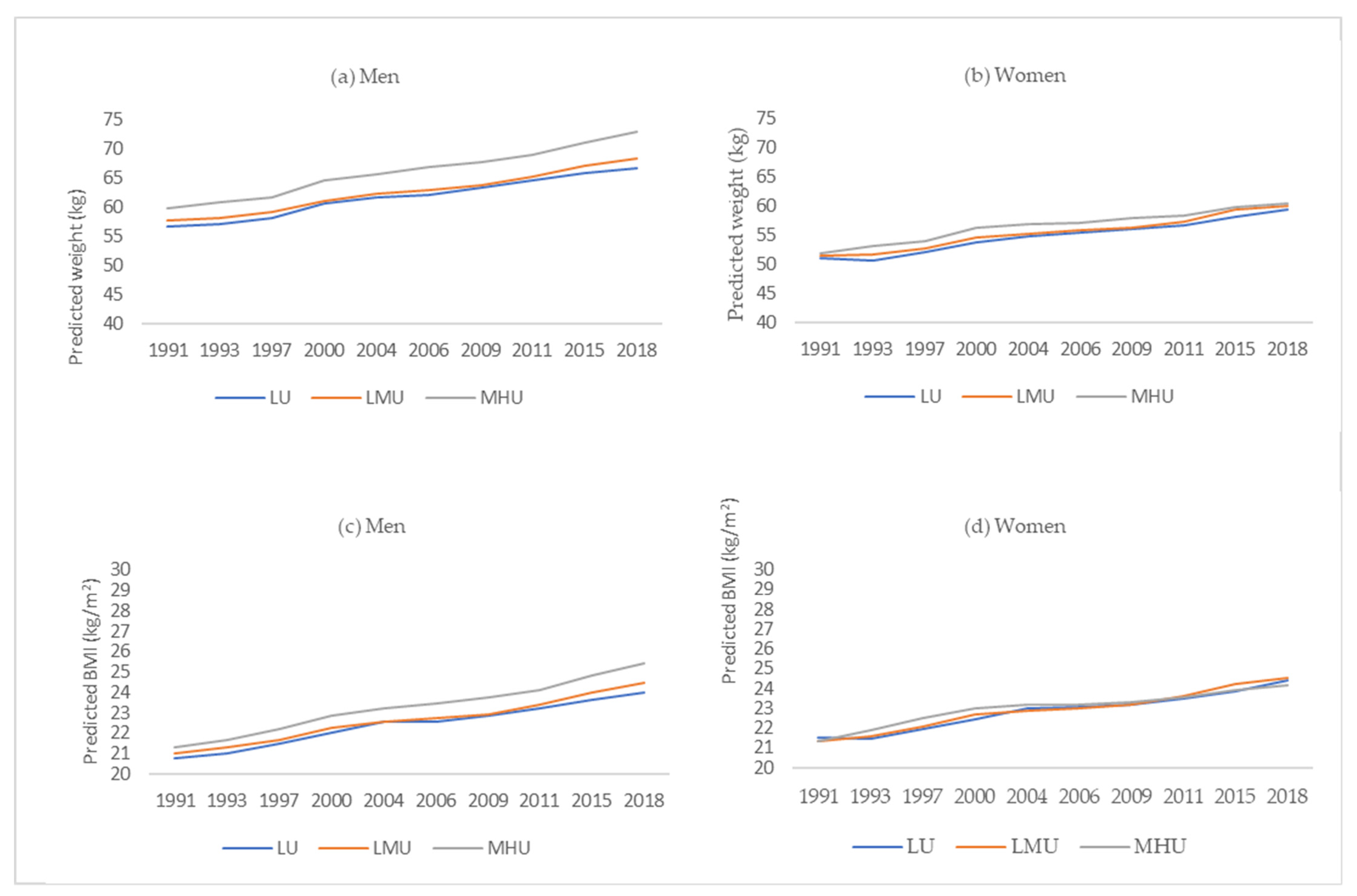
3.3. Association between Urbanization Trajectories and Weight and BMI by Genders
3.4. Association between Urbanization Trajectories and Overweight + Obesity and Obesity by Genders
4. Discussion
4.1. Main Findings
4.2. Comparison with Previous Studies
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Inoue, Y.; Howard, A.G.; Thompson, A.L.; Gordon-Larsen, P. Secular change in the association between urbanisation and abdominal adiposity in China (1993–2011). J. Epidemiol. Community Health 2018, 72, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Chen, J.; Li, Z.; Jiao, B.; Muennig, P. Spatiotemporal Variation of the Association between Urbanicity and Incident Hypertension among Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, Y.; Ma, Y.; Dong, B.; Zou, Z.; Hu, P.; Wang, Z.; Yang, Y.; Song, Y.; Ma, J. Geographical variation and urban-rural disparity of overweight and obesity in Chinese school-aged children between 2010 and 2014: Two successive national cross-sectional surveys. BMJ Open 2019, 9, e025559. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Xu, X.; Dupre, M.E.; Xie, Q.; Qiu, L.; Gu, D. Individual-level factors attributable to urban-rural disparity in mortality among older adults in China. BMC Public Health 2020, 20, 1472. [Google Scholar] [CrossRef] [PubMed]
- Jiamjarasrangsi, W.; Aekplakorn, W.; Vimolkej, T. Validation and comparison study of three urbanicity scales in a Thailand context. BMC Public Health 2016, 16, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novak, N.L.; Allender, S.; Scarborough, P.; West, D. The development and validation of an urbanicity scale in a multi-country study. BMC Public Health 2012, 12, 530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lao, X.Q.; Ma, W.J.; Sobko, T.; Zhang, Y.H.; Xu, Y.J.; Xu, X.J.; Yu, D.M.; Nie, S.P.; Cai, Q.M.; Xia, L.; et al. Overall obesity is leveling-off while abdominal obesity continues to rise in a Chinese population experiencing rapid economic development: Analysis of serial cross-sectional health survey data 2002–2010. Int. J. Obes. 2015, 39, 288–294. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–18. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.J.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The obesity transition: Stages of the global epidemic. Lancet. Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]
- Wang, Y.; Xue, H.; Sun, M.; Zhu, X.; Zhao, L.; Yang, Y. Prevention and control of obesity in China. Lancet. Glob. Health 2019, 7, e1166–e1167. [Google Scholar] [CrossRef]
- Siddiqui, S.T.; Kandala, N.B.; Stranges, S. Urbanisation and geographic variation of overweight and obesity in India: A cross-sectional analysis of the Indian Demographic Health Survey 2005–2006. Int. J. Public Health 2015, 60, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Thapa, R.; Dahl, C.; Aung, W.P.; Bjertness, E. Urban-rural differences in overweight and obesity among 25–64 years old Myanmar residents: A cross-sectional, nationwide survey. BMJ Open 2021, 11, e042561. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.; Zhang, M.; Li, Y.; Li, Z.; Fang, J.; Guo, K. The longitudinal trajectory of body mass index in the Chinese population: A latent growth curve analysis. PLoS ONE 2018, 13, e0207845. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Leung, W.Y.; Chen, Y.S.; Ouyang, Y.F.; Zhao, W.H. Recent Trends in Sedentary Behaviors among Chinese Children According to Demographic and Social Characteristics. Biomed. Environ. Sci. 2021, 34, 593–605. [Google Scholar] [PubMed]
- Sievert, K.; Lawrence, M.; Naika, A.; Baker, P. Processed Foods and Nutrition Transition in the Pacific: Regional Trends, Patterns and Food System Drivers. Nutrients 2019, 11, 1328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trivedi, T.; Liu, J.; Probst, J.; Merchant, A.; Jhones, S.; Martin, A.B. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural Remote Health 2015, 15, 3267. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Tang, Y.; Zhuang, J.; Liu, Y.; Wu, X.; Cai, Y.; Wang, L.; Cao, Z.B.; Chen, P. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: An update from the 2017 physical activity and fitness in China-the youth study. BMC Public Health 2019, 19, 197. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.A.; Greaney, M.L.; Sabik, N.J. Assessment of dietary patterns, physical activity and obesity from a national survey: Rural-urban health disparities in older adults. PLoS ONE 2018, 13, e0208268. [Google Scholar] [CrossRef]
- Jones-Smith, J.C.; Popkin, B.M. Understanding community context and adult health changes in China: Development of an urbanicity scale. Soc. Sci. Med. 2010, 71, 1436–1446. [Google Scholar] [CrossRef] [Green Version]
- Nagin, D.S.; Odgers, C.L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989–2011. Obes. Rev. 2014, 15 (Suppl. S1), 2–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuwahara, K.; Yamamoto, S.; Honda, T.; Nakagawa, T.; Ishikawa, H.; Hayashi, T.; Mizoue, T. Improving and maintaining healthy lifestyles are associated with a lower risk of diabetes: A large cohort study. J. Diabetes Investig. 2021. published online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.; Levy, D.E.; Macy, J.T.; Elam, K.K.; Bidulescu, A.; Seo, D.C. Smoking trajectories from adolescence to early adulthood as a longitudinal predictor of mental health in adulthood: Evidence from 21 years of nationally representative cohort. Addiction 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.F.; Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002, 15, 83–96. [Google Scholar] [PubMed]
- Pierce, J.P.; White, M.M.; Messer, K. Changing age-specific patterns of cigarette consumption in the United States, 1992–2002: Association with smoke-free homes and state-level tobacco control activity. Nicotine Tob. Res. 2009, 11, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Fryar, C.D.; Carroll, M.D.; Freedman, D.S.; Aoki, Y.; Ogden, C.L. Differences in Obesity Prevalence by Demographic Characteristics and Urbanization Level Among Adults in the United States, 2013–2016. JAMA 2018, 319, 2419–2429. [Google Scholar] [CrossRef] [Green Version]
- Feuillet, T.; Valette, J.F.; Charreire, H.; Kesse-Guyot, E.; Julia, C.; Vernez-Moudon, A.; Hercberg, S.; Touvier, M.; Oppert, J.M. Influence of the urban context on the relationship between neighbourhood deprivation and obesity. Soc. Sci. Med. 2020, 265, 113537. [Google Scholar] [CrossRef]
- Hu, Y.; Lin, W.; Tan, X.; Liu, Y.; Wen, Y.; Xing, Y.; Ma, Y.; Liu, H.; Song, Y.; Liang, J.; et al. Trends in urban/rural inequalities in physical growth among Chinese children over three decades of urbanization in Guangzhou: 1985–2015. BMC Public Health 2020, 20, 1190. [Google Scholar] [CrossRef]
- Martinchik, A.N.; Laikam, K.E.; Kozyreva, N.A.; Keshabyants, E.E.; Mikhailov, N.A.; Baturin, A.K.; Smirnova, E.A. The prevalence of obesity in various socio-demographic groups of the population of Russia. Vopr Pitan 2021, 90, 67–76. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 2019, 569, 260–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riha, J.; Karabarinde, A.; Ssenyomo, G.; Allender, S.; Asiki, G.; Kamali, A.; Young, E.H.; Sandhu, M.S.; Seeley, J. Urbanicity and lifestyle risk factors for cardiometabolic diseases in rural Uganda: A cross-sectional study. PLoS Med. 2014, 11, e1001683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ying, X.; Yang, S.; Li, S.; Su, M.; Wang, N.; Chen, Y.; Jiang, Q.; Fu, C. Prevalences of metabolic syndrome and its sex-specific association with socioeconomic status in rural China: A cross-sectional study. BMC Public Health 2021, 21, 2033. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M. Synthesis and implications: China’s nutrition transition in the context of changes across other low- and middle-income countries. Obes. Rev. 2014, 15 (Suppl. S1), 60–67. [Google Scholar] [CrossRef] [Green Version]
- Burant, C.J. Latent Growth Curve Models: Tracking Changes Over Time. Int. J. Aging Hum. Dev. 2016, 82, 336–350. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Xue, H.; Qu, W. A Review of the Growth of the Fast Food Industry in China and Its Potential Impact on Obesity. Int. J. Environ. Res. Public Health 2016, 13, 1112. [Google Scholar] [CrossRef]
- Ren, Y.; Castro Campos, B.; Peng, Y.; Glauben, T. Nutrition Transition with Accelerating Urbanization? Empirical Evidence from Rural China. Nutrients 2021, 13, 921. [Google Scholar] [CrossRef]
- Wu, Y.; Xue, H.; Wang, H.; Su, C.; Du, S.; Wang, Y. The impact of urbanization on the community food environment in China. Asia Pac. J. Clin. Nutr. 2017, 26, 504–513. [Google Scholar]
- Sun, Q.; Li, X.; Rahut, D.B. Gender Differences in Nutritional Intake among Rural-Urban Migrants in China. Int. J. Environ. Res. Public Health 2021, 18, 9821. [Google Scholar] [CrossRef]
- Zhao, J.; Zuo, L.; Sun, J.; Su, C.; Wang, H. Trends and Urban-Rural Disparities of Energy Intake and Macronutrient Composition among Chinese Children: Findings from the China Health and Nutrition Survey (1991 to 2015). Nutrients 2021, 13, 1933. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Zhao, J.; Wu, Y.; Wang, H.; Wang, Z.; Wang, Y.; Zhang, B. Temporal Trends in Dietary Macronutrient Intakes among Adults in Rural China from 1991 to 2011: Findings from the CHNS. Nutrients 2017, 9, 227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, C.; Song, C.; Yuan, F.; Zhang, Y.; Feng, G.; Chen, Z.; Liu, A. The Physical Activity Patterns among Rural Chinese Adults: Data from China National Nutrition and Health Survey in 2010–2012. Int. J. Environ. Res. Public Health 2018, 15, 941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pandey, B.; Reba, M.; Joshi, P.K.; Seto, K.C. Urbanization and food consumption in India. Sci. Rep. 2020, 10, 17241. [Google Scholar] [CrossRef]
- Howard, A.G.; Attard, S.M.; Herring, A.H.; Wang, H.; Du, S.; Gordon-Larsen, P. Socioeconomic gradients in the Westernization of diet in China over 20 years. SSM Popul Health 2021, 16, 100943. [Google Scholar] [CrossRef]
| Men | Women | Overall | |
|---|---|---|---|
| N | 8094 | 8674 | 16,768 |
| Age (years) | 36.79 ± 12.63 | 37.17 ± 12 | 36.99 ± 12.31 |
| Weight (kg) | 62.69 ± 10.85 | 55.03 ± 9.17 | 58.73 ± 10.72 |
| BMI (kg/m2) | 22.33 ± 3.18 | 22.46 ± 3.28 | 22.4 ± 3.23 |
| Entry year (%) | |||
| 1989 | 26.77 | 27.07 | 26.93 |
| 1991 | 18.16 | 16.46 | 17.28 |
| 1993 | 3.98 | 2.7 | 3.32 |
| 1997 | 12.64 | 11.53 | 12.06 |
| 2000 | 7.34 | 7.98 | 7.67 |
| 2004 | 6.6 | 7.02 | 6.82 |
| 2006 | 3.32 | 3.2 | 3.26 |
| 2009 | 5.91 | 6.41 | 6.17 |
| 2011 | 10.75 | 11.72 | 11.25 |
| 2015 | 4.53 | 5.9 | 5.24 |
| Urbanization trajectories (%) | |||
| LU | 28.07 | 26.2 | 27.11 |
| LMU | 25.17 | 24.42 | 24.78 |
| MHU | 46.76 | 49.38 | 48.12 |
| a OO (%) | 25.91 | 27.88 | 26.93 |
| b OB (%) | 5.76 | 5.86 | 5.81 |
| Urbanization Trajectories | Weight | BMI | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 a | Model 1 | Model 2 | Model 3 b | |
| Men | ||||||
| LU (ref) | 0 | 0 | 0 | 0 | 0 | 0 |
| LMU | 1.64 * | 1.11 * | 0.19 | 0.44 * | 0.30 * | 0.10 |
| MHU | 5.52 * | 4.17 * | 0.61 * | 1.17 * | 0.81 * | 0.19 * |
| Women | ||||||
| LU (ref) | 0 | 0 | 0 | 0 | 0 | 0 |
| LMU | 1.27 * | 1.05 * | 0.27 | 0.30 * | 0.29 * | 0.11 |
| MHU | 2.80 * | 2.31 * | 0.21 | 0.45 * | 0.47 * | 0.03 |
| Urbanization Trajectories | OO (BMI ≥ 24 kg/m2) | OB (BMI ≥ 28 kg/m2) | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Men | ||||||
| LU (ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| LMU | 1.35(1.18,1.55) * | 1.22(1.05,1.42) * | 1.14(0.98,1.31) | 1.56(1.29,1.89) * | 1.36(1.11,1.66) * | 1.22(0.99,1.52) |
| MHU | 2.53(2.24,2.85) * | 1.97(1.70,2.27) * | 1.46(1.26,1.69) * | 2.13(1.80,2.52) * | 1.60(1.31,1.96) * | 1.09(0.87,1.35) |
| Women | ||||||
| LU (ref) | 1 | 1 | 1 | 1 | 1 | |
| LMU | 1.15(1.00,1.32) * | 1.17(1.01,1.35) * | 1.07(0.93,1.22) | 1.21(1.01,1.45) * | 1.24(1.02,1.50) * | 1.05(0.85,1.29) |
| MHU | 1.35(1.20,1.52) * | 1.44(1.24,1.66) * | 1.10(0.95,1.27) | 1.35(1.15,1.58) * | 1.49(1.23,1.81) * | 1.03(0.83,1.27) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, W.; Wang, H.; Su, C.; Jia, X.; Zhang, B. Thirty-Year Urbanization Trajectories and Obesity in Modernizing China. Int. J. Environ. Res. Public Health 2022, 19, 1943. https://doi.org/10.3390/ijerph19041943
Du W, Wang H, Su C, Jia X, Zhang B. Thirty-Year Urbanization Trajectories and Obesity in Modernizing China. International Journal of Environmental Research and Public Health. 2022; 19(4):1943. https://doi.org/10.3390/ijerph19041943
Chicago/Turabian StyleDu, Wenwen, Huijun Wang, Chang Su, Xiaofang Jia, and Bing Zhang. 2022. "Thirty-Year Urbanization Trajectories and Obesity in Modernizing China" International Journal of Environmental Research and Public Health 19, no. 4: 1943. https://doi.org/10.3390/ijerph19041943
APA StyleDu, W., Wang, H., Su, C., Jia, X., & Zhang, B. (2022). Thirty-Year Urbanization Trajectories and Obesity in Modernizing China. International Journal of Environmental Research and Public Health, 19(4), 1943. https://doi.org/10.3390/ijerph19041943






