The Feedback Form and Its Role in Improving the Quality of Trauma Care
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
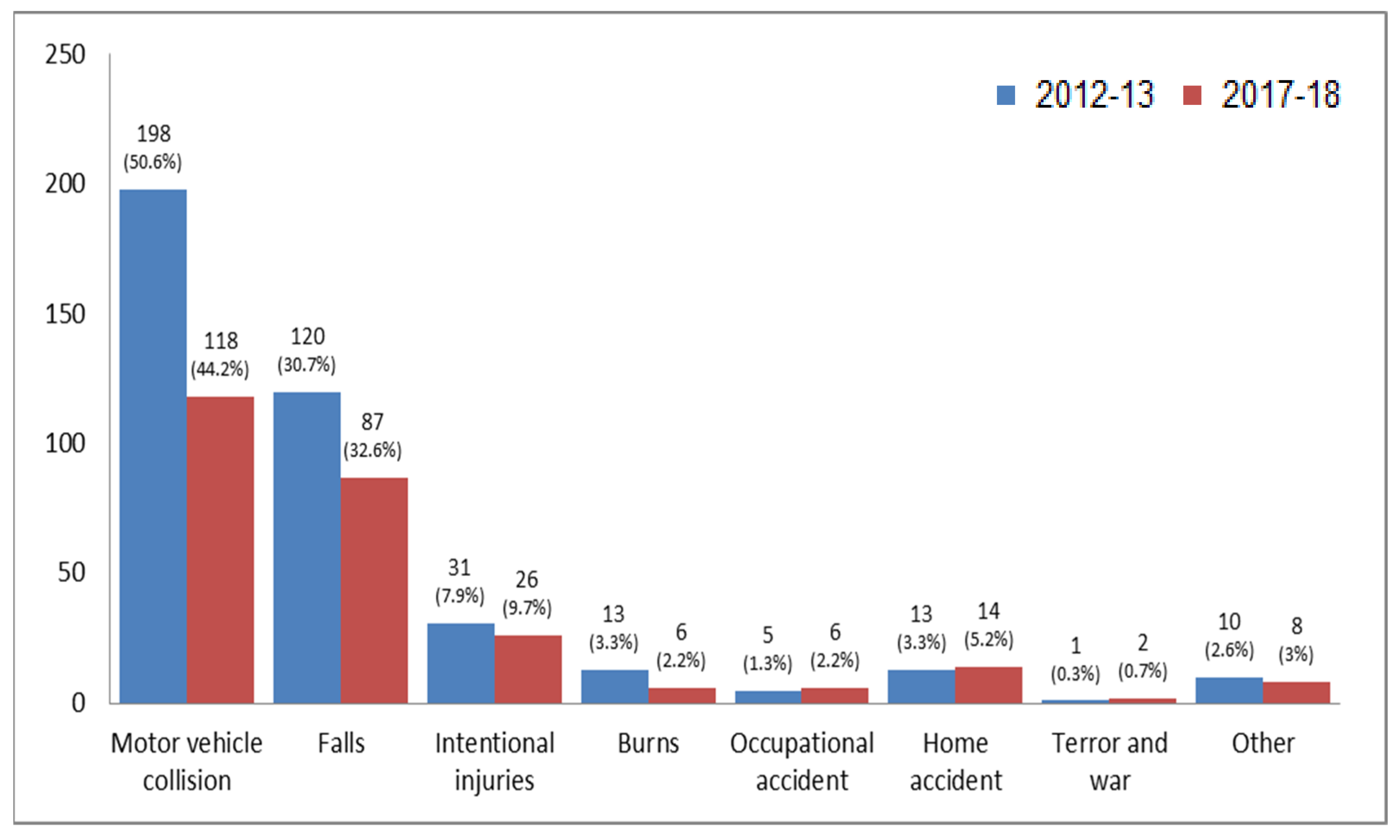
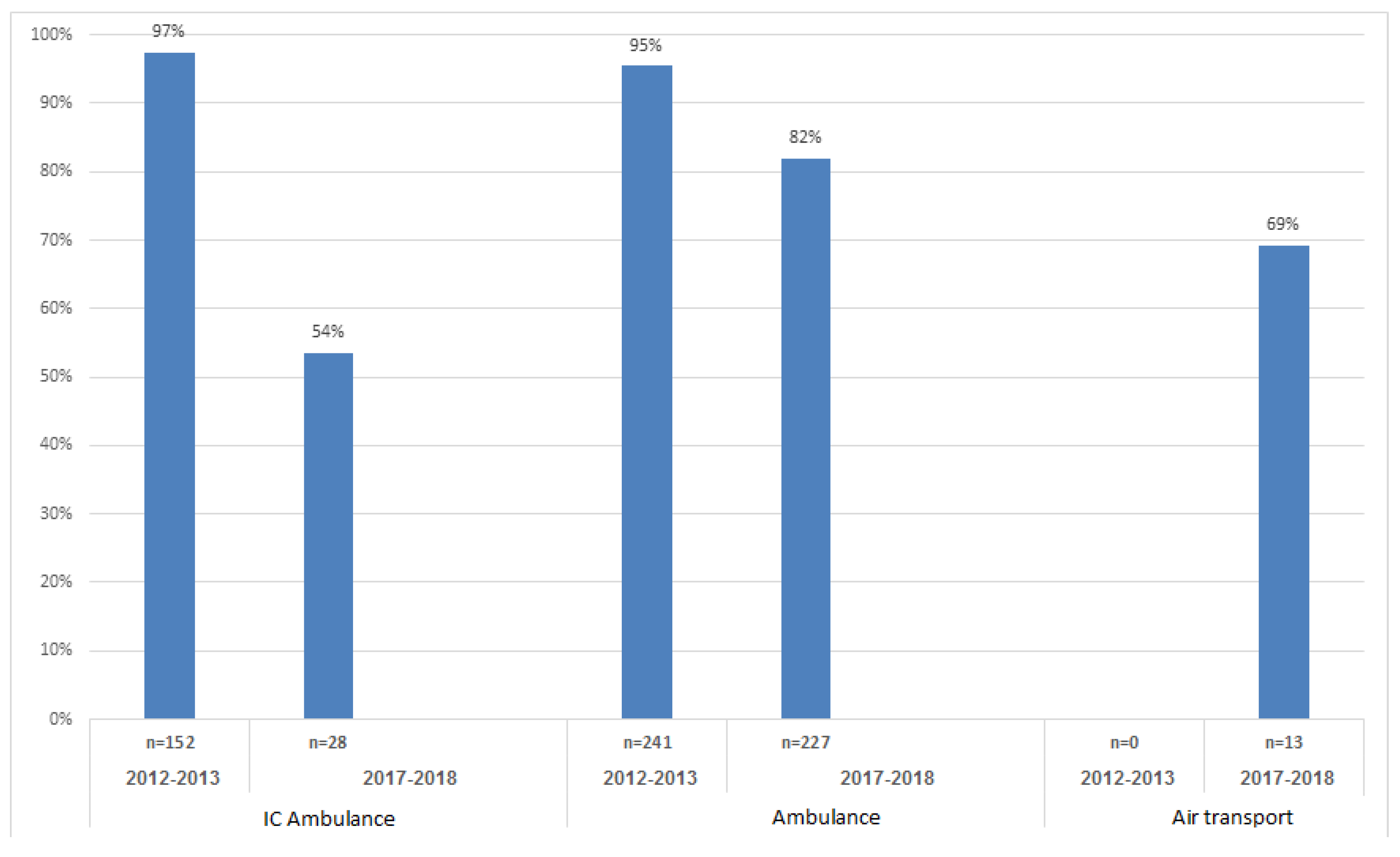
3. Results
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
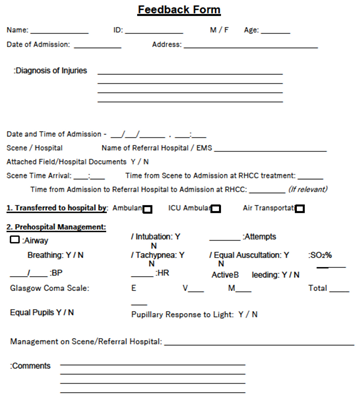
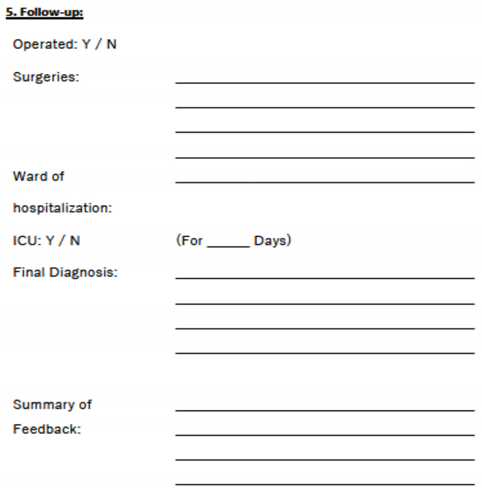
Appendix A
References
- The American Association for the Surgery of Trauma. Trauma Facts. Available online: https://www.aast.org/resources/trauma-facts (accessed on 13 September 2021).
- Adib-Hajbaghery, M.; Maghaminejad, F. Epidemiology of patients with multiple trauma and the quality of their prehospital respiration management in kashan, iran: Six months assessment. Arch. Trauma Res. 2014, 3, e17150. [Google Scholar] [CrossRef]
- World Health Organization. Injuries and violence: The facts 2014. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/149798/9789241508018_eng.pdf?sequence=1&isAllowed=y (accessed on 13 September 2021).
- Celso, B.; Tepas, J.; Langland-Orban, B.; Pracht, E.; Papa, L.; Lottenberg, L.; Flint, L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J. Trauma 2006, 60, 371–378; discussion 378. [Google Scholar] [CrossRef] [PubMed]
- Stürmer, K.M.; Dresing, K.; Bonnaire, F.; Braun, W.; Meenen, N.; Siebert, H.; Suren, E.G. Recommended Guidelines for Diagnostics and Therapy in Trauma Surgery. Recommended Guidelines for Polytrauma. Eur. J. Trauma 2001, 27, 137–150. [Google Scholar] [CrossRef]
- Barie, P.S.; Hydo, L.J.; Fischer, E. A prospective comparison of two multiple organ dysfunction/failure scoring systems for prediction of mortality in critical surgical illness. J. Trauma Acute Care Surg. 1994, 37, 660–666. [Google Scholar] [CrossRef]
- Lockey, D.J. Improved Trauma Outcomes after the Introduction of a Trauma System in England. eClinicalMedicine 2018, 2, 3–4. [Google Scholar] [CrossRef]
- Roh, Y.I.; Kim, H.I.; Cha, Y.S.; Cha, K.-C.; Kim, H.; Lee, K.H.; Hwang, S.O.; Kim, O.H. Mortality Reduction in Major Trauma Patients after Establishment of a Level I Trauma Center in Korea: A Single-Center Experience. J. Trauma Inj. 2017, 30, 131–139. [Google Scholar] [CrossRef]
- Rotondo, M.F.; Cribari, C.; Smith, R.S.; ACS Committee on Trauma (Eds.) Resources for Optimal Care of the Injured Patient; American College of Surgeons: Chicago, IL, USA, 2014; Available online: https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx (accessed on 13 September 2021).
- MacKenzie, E.J.; Rivara, F.P.; Jurkovich, G.J.; Nathens, A.B.; Frey, K.P.; Egleston, B.L.; Salkever, D.S.; Scharfstein, D.O. A national evaluation of the effect of trauma-center care on mortality. N. Engl. J. Med. 2006, 354, 366–378. [Google Scholar] [CrossRef]
- Staudenmayer, K.; Weiser, T.G.; Maggio, P.M.; Spain, D.A.; Hsia, R.Y. Trauma center care is associated with reduced readmissions after injury. J. Trauma Acute Care Surg. 2016, 80, 412–416; discussion 416–418; [Google Scholar] [CrossRef]
- Sasser, S.M.; Hunt, R.C.; Faul, M.; Sugerman, D.; Pearson, W.S.; Dulski, T.; Wald, M.M.; Jurkovich, G.J.; Newgard, C.D.; Lerner, E.B. Guidelines for field triage of injured patients: Recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm. Rep. 2012, 61, 1–20. [Google Scholar]
- Sheahan, G.; Reznick, R.; Klinger, D.; Flynn, L.; Zevin, B. Comparison of faculty versus structured peer-feedback for acquisitions of basic and intermediate-level surgical skills. Am. J. Surg. 2019, 217, 214–221. [Google Scholar] [CrossRef]
- Gude, W.T.; Roos-Blom, M.J.; van der Veer, S.N.; Dongelmans, D.A.; de Jonge, E.; Francis, J.J.; Peek, N.; de Keizer, N.F. Health professionals’ perceptions about their clinical performance and the influence of audit and feedback on their intentions to improve practice: A theory-based study in Dutch intensive care units. Implement. Sci. 2018, 13, 33. [Google Scholar] [CrossRef]
- Wang, C.-J.; Yang, T.-H.; Hung, K.-S.; Wu, C.-H.; Yen, S.-T.; Yen, Y.-T.; Shan, Y.-S. Regular feedback on inter-hospital transfer improved the clinical outcome and survival in patients with multiple trauma: A retrospective cohort study. BMC Emerg. Med. 2021, 21, 150. [Google Scholar] [CrossRef] [PubMed]
- Rae, L.; Bulger, E. Optimizing feedback from a designated level 1 trauma/burn center to referring hospitals. J. Am. Coll. Surg. 2015, 220, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, J. Learning from Errors. Annu. Rev. Psychol. 2017, 68, 465–489. [Google Scholar] [CrossRef] [PubMed]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2012, 6, CD000259. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.C.; Kulhavy, R.W.; Andre, T. Conditions under which feedback facilitates learning from programmed lessons. J. Educ. Psychol. 1972, 63, 186–188. [Google Scholar] [CrossRef]
- Abdel-Rahman, N.; Siman-Tov, M.; Israel Trauma, G.; Peleg, K. Ethnicity and road traffic injuries: Differences between Jewish and Arab children in Israel. Ethn. Health 2013, 18, 391–401. [Google Scholar] [CrossRef]
- Kortbeek, J.B.; Al Turki, S.A.; Ali, J.; Antoine, J.A.; Bouillon, B.; Brasel, K.; Brenneman, F.; Brink, P.R.; Brohi, K.; Burris, D.; et al. Advanced trauma life support, 8th edition, the evidence for change. J. Trauma 2008, 64, 1638–1650. [Google Scholar] [CrossRef]
- Deakin, C.D.; Soreide, E. Pre-hospital trauma care. Curr. Opin. Anaesthesiol. 2001, 14, 191–195. [Google Scholar] [CrossRef][Green Version]
- Lossius, H.M.; Soreide, E.; Hotvedt, R.; Hapnes, S.A.; Eielsen, O.V.; Forde, O.H.; Steen, P.A. Prehospital advanced life support provided by specially trained physicians: Is there a benefit in terms of life years gained? Acta Anaesthesiol. Scand. 2002, 46, 771–778. [Google Scholar] [CrossRef]
- Barnes, J.M.; Underwood, B.J. Fate of first-list associations in transfer theory. J. Exp. Psychol. 1959, 58, 97–105. [Google Scholar] [CrossRef]
- Metcalfe, J.; Kornell, N. Principles of cognitive science in education: The effects of generation, errors, and feedback. Psychon. Bull. Rev. 2007, 14, 225–229. [Google Scholar] [CrossRef]
- Metcalfe, J.; Kornell, N.; Son, L.K. A cognitive-science based programme to enhance study efficacy in a high and low risk setting. Eur. J. Cogn. Psychol. 2007, 19, 743–768. [Google Scholar] [CrossRef] [PubMed]
- Pashler, H.; Cepeda, N.J.; Wixted, J.T.; Rohrer, D. When does feedback facilitate learning of words? J. Exp. Psychol. Learn. Mem. Cogn. 2005, 31, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R. Decreasing Cognitive Load for Novice Students: Effects of Explanatory versus Corrective Feedback in Discovery-Based Multimedia. Instr. Sci. 2004, 32, 99–113. [Google Scholar] [CrossRef]
- Joyce, S.M.; Dutkowski, K.L.; Hynes, T. Efficacy of an EMS quality improvement program in improving documentation and performance. Prehospital Emerg. Care 1997, 1, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Alatis, A.S.; Monahan, B.V.; Raymond, A.D.; Hudson, K.B.; Vieth, J.T. Checklistis Improve EMS Documentation: Quality Improvement in a Collegiate-Based EMS Angency. J. Coll. Emerg. Med. Serv. 2020, 3, 16–21. [Google Scholar] [CrossRef]
- O’Connor, R.E.; Megargel, R.E. The effect of a quality improvement feedback loop on paramedic skills, charting, and behavior. Prehospital Disaster Med 1994, 9, 35–38; discussion 38–39; [Google Scholar] [CrossRef]
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol. 2014, 6, 309–331. [Google Scholar] [CrossRef]
- Hong, R.; Meenan, M.; Prince, E.; Murphy, R.; Tambussi, C.; Rohrbach, R.; Baumann, B.M. Comparison of three prehospital cervical spine protocols for missed injuries. West. J. Emerg. Med. 2014, 15, 471–479. [Google Scholar] [CrossRef]
- The ATLS Subcommittee and the International ATLS Working Group; Trauma, A.C.o.S.C.o. Spine and spinal cord trauma. In Advanced Trauma Life Support: Student Course Manual, 10th ed.; American College of Surgeons: Chicago, IL, USA, 2018; pp. 128–147. [Google Scholar]
- Haut, E.R.; Kalish, B.T.; Efron, D.T.; Haider, A.H.; Stevens, K.A.; Kieninger, A.N.; Cornwell, E.E., 3rd; Chang, D.C. Spine immobilization in penetrating trauma: More harm than good? J. Trauma 2010, 68, 115–120; discussion 120–121. [Google Scholar] [CrossRef] [PubMed]
- Hauswald, M.; Ong, G.; Tandberg, D.; Omar, Z. Out-of-hospital spinal immobilization: Its effect on neurologic injury. Acad. Emerg. Med. 1998, 5, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Purvis, T.A.; Carlin, B.; Driscoll, P. The definite risks and questionable benefits of liberal pre-hospital spinal immobilisation. Am. J. Emerg. Med. 2017, 35, 860–866. [Google Scholar] [CrossRef]
- Ham, W.H.; Schoonhoven, L.; Schuurmans, M.J.; Leenen, L.P. Pressure ulcers, indentation marks and pain from cervical spine immobilization with extrication collars and headblocks: An observational study. Injury 2016, 47, 1924–1931. [Google Scholar] [CrossRef] [PubMed]
- Freauf, M.; Puckeridge, N. To Board or Not to Board: An Evidence Review of Prehospital Spinal Immobilization. JEMS 2015, 40, 43–45. [Google Scholar]
- Stiell, I.G.; Nesbitt, L.P.; Pickett, W.; Munkley, D.; Spaite, D.W.; Banek, J.; Field, B.; Luinstra-Toohey, L.; Maloney, J.; Dreyer, J.; et al. The OPALS Major Trauma Study: Impact of advanced life-support on survival and morbidity. CMAJ 2008, 178, 1141–1152. [Google Scholar] [CrossRef]
- Nemunaitis, G.; Roach, M.J.; Hefzy, M.S.; Mejia, M. Redesign of a spine board: Proof of concept evaluation. Assist. Technol. 2016, 28, 144–151. [Google Scholar] [CrossRef]
- Rao, P.J.; Phan, K.; Mobbs, R.J.; Wilson, D.; Ball, J. Cervical spine immobilization in the elderly population. J. Spine Surg. 2016, 2, 41–46. [Google Scholar] [CrossRef]
- Berben, S.A.; Meijs, T.H.; van Grunsven, P.M.; Schoonhoven, L.; van Achterberg, T. Facilitators and barriers in pain management for trauma patients in the chain of emergency care. Injury 2012, 43, 1397–1402. [Google Scholar] [CrossRef]
- Devriendt, N.; de Rooster, H. Initial Management of Traumatic Wounds. Veter Clin. N. Am. Small Anim. Pract. 2017, 47, 1123–1134. [Google Scholar] [CrossRef]
- Byrnes, M.C.; Irwin, E.; Becker, L.; Thorson, M.; Beilman, G.; Horst, P.; Croston, K. A trauma outreach program provided by a level I trauma center is an effective way to initiate peer review at referring hospitals and foster process improvements. J. Trauma 2010, 68, 778–782. [Google Scholar] [CrossRef] [PubMed]

| Variables | 2012–2013; n = 76 (%) | 2017–2018; n = 68 (%) | p-Value |
|---|---|---|---|
| * Age | 32.7 ± 24.9 | 41.9 ± 25.75 | p < 0.001 |
| # Male Female | 55 (72) 21 (28) | 49 (72) 19 (28) | p = 1.00 |
| ~ Mode of transportation | |||
| Code 1 = Ambulance | 2 (3) | 1 (1.5) | p = 0.51 |
| Code 2 = IC ambulance | 74 (97) | 66 (97) | |
| Code 4 = Air transport | 0 | 1 (1.5) | |
| # Injury | |||
| Code 1 = Motor vehicle collisions | 32 (43) | 23 (34) | |
| Code 2 = Falls | 30 (41) | 22 (33) | |
| Code 3, 4, 8 = Intentional injuries | 5 (7) | 9 (19.5) | |
| Code 5 = Burns | 4 (5) | 0 | |
| Code 6 = Occupational accident | 0 | 2 (3) | |
| Code 7 = home accidents | 1 (1) | 4 (6) | |
| Code 9 = Terror and war | 1 (1) | 1 (1.5) | |
| Code 10 = Other | 1 (1) | 2 (3) | |
| # Primary hospital management (see Appendix A # 4) (1 = yes comment) | 9 (12) | 9 (13) | p = 0.81 |
| # Pain management 1 = yes comment) | 7 (9) | 14 (21) | p = 0.062 |
| # Backboard fixation not performed (1 = yes comment) | 2 (3) | 21 (31) | p < 0.001 |
| # Neck collar fixation not performed (1 = yes comment) | 3 (4) | 27 (37) | p < 0.001 |
| # Pain management | 5 (7) | 14 (21) | p = 0.015 |
| # GCS ≤ 8 GCS > 8 | 52 (69) 23 (31) | 38 (56) 30 (44) | p = 0.12 |
| GCS | 6.5 ± 5.4 | 8.1 ± 5.8 | p = 0.083 |
| # Documentation from hospital (1 = yes comment) | 4 (1) | 52 (26) | p < 0.001 |
| # No field file (1 = yes comment) | 69 (91) | 37 (54) | p < 0.001 |
| # Surgery performed | 51 (67) | 40 (60) | p = 0.39 |
| Variables | 2012–2013; n = 317 (%) | 2017–2018; n = 201 (%) | p-Value |
|---|---|---|---|
| * Age | 33.9 ± 22.7 | 41.9 ± 24.2 | p < 0.001 |
| # Male Female | 253 (80) 63 (20) | 146 (72.5) 55 (27.5) | p = 0.053 |
| ~ Mode of transportation | |||
| Code1 = Ambulance | 150 (47) | 27 (13.5) | p < 0.001 |
| Code 2 = IC ambulance | 167 (53) | 161 (80.5) | |
| Code 4 = Aerial transport | 0 | 12 (6) | |
| # Mechanism of injury | |||
| Code 1 = Motor vehicle collisions | 166 (52) | 95 (48) | |
| Code 2 = Falls | 90 (28) | 64 (32) | |
| Code 3,4,8 = Intentional injuries | 26 (8.5) | 13 (6.5) | |
| Code 5 = Burns | 9 (3) | 6 (3) | |
| Code 6 = Occupational accident | 5 (2) | 4 (2) | |
| Code 7 = Home accident | 12 (4) | 10 (5) | |
| Code 9 = Terror and war | 0 | 1 (0.5) | |
| Code 10 = Others | 9 (3) | 6 (3) | |
| * Time in field (min) | 15.2 ± 8.3 | 13.4 ± 7.9 | p = 0.038 |
| # Pre-hospital management (see Appendix A # 2) (1 = yes comment) | 45 (14.5) | 34 (17) | p = 0.45 |
| # Pain management (1 = yes comment) | 46 (14.4) | 59 (29.3) | p < 0.001 |
| # Backboard fixation not performed (1 = yes comment) | 19 (6) | 67 (33.5) | p < 0.001 |
| # Neck collar fixation not performed (1 = yes comment) | 22 (7) | 73 (36.5) | p < 0.001 |
| # GCS ≤ 8 GCS > 8 | 145 (46) 168 (54) | 74 (37) 124 (63) | p = 0.054 |
| GCS | 9.4 ± 5.8 | 10.2 ± 5.3 | p = 0.10 |
| # No field file (1 = yes comment) | 309 (97.5) | 173(86.5) | p < 0.001 |
| # Surgery performed | 150 (47) | 107 (54) | p = 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bahouth, H.; Abramov, R.; Bodas, M.; Halberthal, M.; Lin, S. The Feedback Form and Its Role in Improving the Quality of Trauma Care. Int. J. Environ. Res. Public Health 2022, 19, 1866. https://doi.org/10.3390/ijerph19031866
Bahouth H, Abramov R, Bodas M, Halberthal M, Lin S. The Feedback Form and Its Role in Improving the Quality of Trauma Care. International Journal of Environmental Research and Public Health. 2022; 19(3):1866. https://doi.org/10.3390/ijerph19031866
Chicago/Turabian StyleBahouth, Hany, Roi Abramov, Moran Bodas, Michael Halberthal, and Shaul Lin. 2022. "The Feedback Form and Its Role in Improving the Quality of Trauma Care" International Journal of Environmental Research and Public Health 19, no. 3: 1866. https://doi.org/10.3390/ijerph19031866
APA StyleBahouth, H., Abramov, R., Bodas, M., Halberthal, M., & Lin, S. (2022). The Feedback Form and Its Role in Improving the Quality of Trauma Care. International Journal of Environmental Research and Public Health, 19(3), 1866. https://doi.org/10.3390/ijerph19031866







