ICU-Associated Costs during the Fourth Wave of the COVID-19 Pandemic in a Tertiary Hospital in a Low-Vaccinated Eastern European Country
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mo, P.; Xing, Y.; Xiao, Y.U.; Deng, L.; Zhao, Q.; Wang, H.; Xiong, Y.; Cheng, Z.; Gao, S.; Liang, K. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis. 2021, 73, e4208–e4213. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Cui, W.; Zhang, F. Who Was the First Doctor to Report the COVID-19 Outbreak in Wuhan, China? J. Nucl. Med. 2020, 61, 782–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- La Maestra, S.; Abbondandolo, A.; De Flora, S. Epidemiological trends of COVID-19 epidemic in Italy over March 2020, From 1000 to 100 000 cases. J. Med. Virol. 2020, 92, 1956–1961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vokó, Z.; Pitter, J.G. The effect of social distance measures on COVID-19 epidemics in Europe: An interrupted time series analysis. GeroScience 2020, 42, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Igan, D.O.; Pierri, N.; Presbitero, A.F.; Soledad, M.; Peria, M. Tracking the Economic Impact of COVID-19 and Mitigation Policies in Europe and the United States. IMF Work. Pap. 2020, 2020, A001. [Google Scholar] [CrossRef]
- Chudasama, Y.V.; Gillies, C.L.; Zaccardi, F.; Coles, B.; Davies, M.J.; Seidu, S.; Khunti, K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. 2020, 14, 965–967. [Google Scholar] [CrossRef]
- Goniewicz, K.; Khorram-Manesh, A.; Hertelendy, A.J.; Goniewicz, M.; Naylor, K.; Burkle, F.M. Current response and management decisions of the European Union to the COVID-19 outbreak: A review. Sustainability 2020, 12, 3838. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Windisch, W.; McAuley, D.F.; Welte, T.; Busse, R. Major differences in ICU admissions during the first and second COVID-19 wave in Germany. Lancet Resp. Med. 2021, 9, e47–e48. [Google Scholar] [CrossRef]
- Janke, A.T.; Mei, H.; Rothenberg, C.; Becher, R.D.; Lin, Z.; Venkatesh, A.K. Analysis of Hospital Resource Availability and COVID-19 Mortality Across the United States. J. Hosp. Med. 2021, 16, 211–214. [Google Scholar] [CrossRef]
- Tyrrell, C.S.B.; Mytton, O.T.; Gentry, S.V.; Thomas-Meyer, M.; Allen, J.L.Y.; Narula, A.A.; McGrath, B.; Lupton, M.; Broadbent, J.; Ahmed, A.; et al. Managing intensive care admissions when there are not enough beds during the COVID-19 pandemic: A systematic review. Thorax 2021, 76, 302–312. [Google Scholar] [CrossRef]
- Jalili, M.; Niroomand, M.; Hadavand, F.; Zeinali, K.; Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: A cross-sectional study. Int. Arch. Occup. Env. Health 2021, 94, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.; Vogt, T.M.; Zhou, F. Patient Characteristics and Costs Associated With COVID-19-Related Medical Care Among Medicare Fee-for-Service Beneficiaries. Ann. Intern. Med. 2021, 174, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Kim, L.; Garg, S.; O’Halloran, A.; Whitaker, M.; Pham, H.; Anderson, E.J.; Armistead, I.; Bennett, N.M.; Billing, L.; Como-Sabetti, K.; et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin. Infect. Dis. 2021, 72, e206–e214. [Google Scholar] [CrossRef] [PubMed]
- Alves, L. Brazilian ICUs short of drugs and beds amid COVID-19 surge. Lancet 2021, 397, 1431–1432. [Google Scholar] [CrossRef]
- Sen-Crowe, B.; Sutherland, M.; McKenney, M.; Elkbuli, A. A Closer Look Into Global Hospital Beds Capacity and Resource Shortages During the COVID-19 Pandemic. J. Surg. Res. 2021, 260, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Vasile, M.C.; Arbune, A.A.; Lupasteanu, G.; Vlase, C.M.; Popovici, G.C.; Arbune, M. Epidemiologic and Clinic Characteristics of the First Wave of the COVID-19 Pandemic in Hospitalized Patients from Galați County. J. Clin. Med. 2021, 10, 4210. [Google Scholar] [CrossRef] [PubMed]
- Plümper, T.; Neumayer, E. Lockdown policies and the dynamics of the first wave of the Sars-CoV-2 pandemic in Europe. J. Eur. Public Policy 2020, 1–21. [Google Scholar] [CrossRef]
- National Institute of Public Health. Available online: https://instnsp.maps.arcgis.com/apps/dashboards/5eced796595b4ee585bcdba03e30c127 (accessed on 10 November 2021).
- Ministry of Internal Affairs. Available online: https://www.mai.gov.ro/category/comunicate-de-presa/ (accessed on 17 January 2022).
- Şoitu, D. Long-Term Healthcare System. Development and Future Policies for Romania. In Decisions and Trends in Social Systems; Soitu, D., Hošková-Mayerová, Š., Maturo, F., Eds.; Lecture Notes in Networks and Systems; Springer: Cham, Switzerland, 2021; Volume 189, pp. 141–155. [Google Scholar]
- López-Valcárcel, B.G.; Vallejo-Torres, L. The costs of COVID-19 and the cost-effectiveness of testing. App. Econ. J. 2021, 29, 77–89. [Google Scholar] [CrossRef]
- McCabe, R.; Kont, M.D.; Schmit, N.; Whittaker, C.; Løchen, A.; Baguelin, M.; Knock, E.; Whittles, L.K.; Lees, J.; Brazeau, N.F.; et al. Modelling intensive care unit capacity under different epidemiological scenarios of the COVID-19 pandemic in three Western European countries. Int. J. Epidemiol. 2021, 50, 753–767. [Google Scholar] [CrossRef]
- Vincent, J.L.; de Mendonça, A.; Cantraine, F.; Moreno, R.; Takala, J.; Suter, P.M.; Sprung, C.L.; Colardyn, F.; Blecher, S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit. Care Med. 1998, 26, 1793–1800. [Google Scholar] [CrossRef]
- Headley, J.; Theriault, R.; Smith, T.L. Independent validation of APACHE II severity of illness score for predicting mortality in patients with breast cancer admitted to the intensive care unit. Cancer 1992, 70, 497–503. [Google Scholar] [CrossRef]
- National Bank of Romania. Available online: https://www.curs-valutar-bnr.ro/curs-valutar-mediu-lunar-2021 (accessed on 15 November 2021).
- Karabatsou, D.; Tsironi, M.; Tsigou, E.; Boutzouka, E.; Katsoulas, T.; Baltopoulos, G. Variable cost of ICU care, a micro-costing analysis. Intensive Crit. Care Nurs. 2016, 35, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Lefrant, J.Y.; Garrigues, B.; Pribil, C.; Bardoulat, I.; Courtial, F.; Maurel, F.; Bazin, J.É. The daily cost of ICU patients: A micro-costing study in 23 French Intensive Care Units. Anaesth Crit. Care Pain Med. 2015, 34, 151–157. [Google Scholar] [CrossRef]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W.; et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pr. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Statistics. Available online: https://insse.ro/cms/sites/default/files/field/publicatii/tendinte_sociale.pdf (accessed on 19 January 2022).
- Onofrei, M.; Cigu, E.; Gavriluta Vatamanu, A.F.; Bostan, I.; Oprea, F. Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania. Int. J. Env. Res. Public Health 2021, 18, 1134. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; AlRuthia, Y.; Balkhi, B.; Alghadeer, S.M.; Temsah, M.H.; Althunayyan, S.M.; Alsofayan, Y.M. Survival and estimation of direct medical costs of hospitalized COVID-19 patients in the Kingdom of Saudi Arabia. Int. J. Res. Public Health 2020, 17, 7458. [Google Scholar] [CrossRef]
- Oksuz, E.; Malhan, S.; Gonen, M.S.; Kutlubay, Z.; Keskindemirci, Y.; Jarrett, J.; Sahin, T.; Ozcagli, G.; Bilgic, A.; Bibilik, M.O.; et al. Cost-Effectiveness Analysis of Remdesivir Treatment in COVID-19 Patients Requiring Low-Flow Oxygen Therapy: Payer Perspective in Turkey. Adv. Ther. 2021, 38, 4935–4948. [Google Scholar] [CrossRef]
- Carrera-Hueso, F.J.; Álvarez-Arroyo, L.; Poquet-Jornet, J.E.; Vázquez-Ferreiro, P.; Martínez-Gonzalbez, R.; El-Qutob, D.; Ramón-Barrios, M.A.; Martínez-Martínez, F.; Poveda-Andrés, J.L.; Crespo-Palomo, C. Hospitalization budget impact during the COVID-19 pandemic in Spain. Health Econ. Rev. 2021, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ohsfeldt, R.L.; Choong, C.K.C.; Mc Collam, P.L.; Abedtash, H.; Kelton, K.A.; Burge, R. Inpatient Hospital Costs for COVID-19 Patients in the United States. Adv. Ther. 2021, 38, 5557–5595. [Google Scholar] [CrossRef] [PubMed]
- Meijs, D.A.M.; van Bussel, B.C.T.; Stessel, B.; Mehagnoul-Schipper, J.; Hana, A.; Scheeren, C.I.E.; Peters, S.A.E.; van Mook, W.N.K.A.; van der Horst, I.C.C.; Marx, G.; et al. Better COVID-19 Intensive Care Unit survival in females, independent of age, disease severity, comorbidities, and treatment. Sci. Rep. 2022, 12, 734. [Google Scholar] [CrossRef] [PubMed]
- Quah, P.; Li, A.; Phua, J. Mortality rates of patients with COVID-19 in the intensive care unit: A systematic review of the emerging literature. Crit. Care 2020, 24, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Wilfong, E.M.; Ovely, C.M.; Gillaspie, E.A.; Huang, L.C.; Shyr, Y.; Casey, J.D.; Rini, B.I.; Semler, M.W. Severity of illness scores at presentation predict ICU admission and mortality in COVID-19. J. Emerg. Crit. Care Med. 2021, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Raschke, R.A.; Agarwal, S.; Rangan, P.; Heise, C.W.; Curry, S.C. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA 2021, 325, 1469–1470. [Google Scholar] [CrossRef] [PubMed]
- Di Fusco, M.; Shea, K.M.; Lin, J.; Nguyen, J.L.; Angulo, F.J.; Benigno, M.; Malhotra, D.; Emir, B.; Sung, A.H.; Hammond, J.L.; et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J. Med. Econ. 2021, 24, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Coca, S.G.; Chan, L.; Melamed, M.L.; Brenner, S.K.; Hayek, S.S.; Sutherland, A.; Puri, S.; Srivastava, A.; Leonberg-Yoo, A.; et al. AKI treated with renal replacement therapy in critically ill patients with COVID-19. J. Am. Soc. Nephrol. 2021, 32, 161–176. [Google Scholar] [CrossRef] [PubMed]
- Hoste, E.A.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; Forni, L.G.; Gomersall, C.D.; Govil, D.; et al. Epidemiology of acute kidney injury in critically ill patients: The multinational AKI-EPI study. Intensive Care Med. 2015, 41, 1411–1423. [Google Scholar] [CrossRef]
- Kahn, J.M.; Rubenfeld, G.D.; Rohrbach, J.; Fuchs, B.D. Cost savings attributable to reductions in intensive care unit length of stay for mechanically ventilated patients. Med. Care 2008, 46, 1226–1233. [Google Scholar] [CrossRef]
- Evans, J.; Kobewka, D.; Thavorn, K.; D’Egidio, G.; Rosenberg, E.; Kyeremanteng, K. The impact of reducing intensive care unit length of stay on hospital costs: Evidence from a tertiary care hospital in Canada. Can. J. Anaesth. 2018, 65, 627–635. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Control. Available online: https://covid19-country-overviews.ecdc.europa.eu/ (accessed on 10 November 2021).
- Romanian Ministry of Health. Available online: https://vaccinare-covid.gov.ro/actualizare-zilnica-01-09-evidenta-persoanelor-vaccinate-impotriva-covid-19/ (accessed on 10 November 2021).
- Cristea, D.; Ilie, D.G.; Constantinescu, C.; Fîrțală, V. Vaccinating against COVID-19, The Correlation between Pro-Vaccination Attitudes and the Belief That Our Peers Want to Get Vaccinated. Vaccines 2021, 9, 1366. [Google Scholar] [CrossRef]
- Buturoiu, R.; Udrea, G.; Oprea, D.-A.; Corbu, N. Who Believes in Conspiracy Theories about the COVID-19 Pandemic in Romania? An Analysis of Conspiracy Theories Believers’ Profiles. Societies 2021, 11, 138. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Self, W.H.; Adams, K.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA 2021, 326, 2043–2054. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, W.; Evans, L.; Alshamsi, F.; Møller, M.H.; Ostermann, M.; Prescott, H.C.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; et al. Surviving Sepsis Campaign Guidelines on the Management of Adults With Coronavirus Disease 2019 (COVID-19) in the ICU: First Update. Crit. Care Med. 2021, 49, 219–234. [Google Scholar] [CrossRef] [PubMed]

| Variable | Year 2021 (n = 36) | Year 2020 (n = 43) | Year 2019 (n = 46) | p Value ^ | p Value 2021 vs. 2020 | p Value 2021 vs. 2019 |
|---|---|---|---|---|---|---|
| Age (years) | 62.0 ± 15.9 | 60.4 ± 18.7 | 62.0 ± 15.9 | 0.73 | 0.91 | 0.92 |
| APACHE II Score | 14.7 ± 7.5 | 24.2 ± 10.0 | 22.6 ± 6.0 | <0.01 * | <0.01 * | <0.01 * |
| SOFA Score | 4.9 ± 2.9 | 9.5 ± 4.1 | 9.1 ± 3.9 | <0.01 * | <0.01 * | <0.01 * |
| ICU LoS (days) | 14.1 ± 8.1 | 11.4 ± 9.5 | 11.0 ± 5.6 | 0.17 | ||
| Hospital LoS (days) | 20.1 ± 14.0 | 22.3 ± 15.9 | 19.7 ± 11.3 | 0.64 | ||
| Survival (%) | 52.7% | 37.2% | 43% | 0.27 | ||
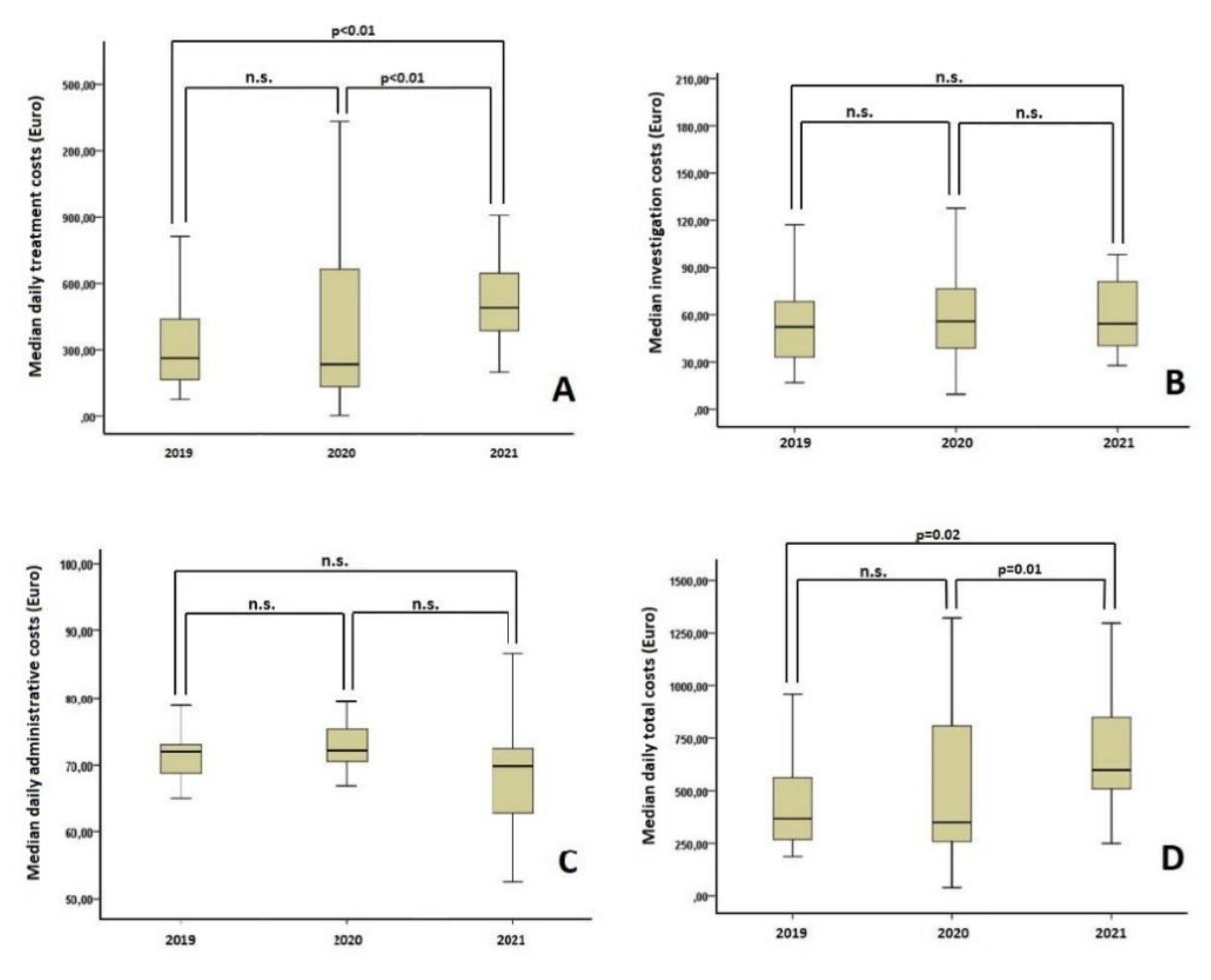
| Median daily treatment cost (euro) | 490.4 [199.3, 1095.0] | 234.5 [12.8, 2045.3] | 263.6 [76.6, 2435.1] | <0.01 * | <0.01 * | <0.01 * |
| Median daily investigation costs (euro) | 54.3 [27.7, 483.0] | 55.9 [9.5, 401.1] | 52.2 [16.9, 765.2] | 0.07 | ||
| Median daily administrative costs (euro) | 69.8 [25.8, 174.4] | 72.2 [6.6, 689.8] | 71.9 [34.9, 720.1] | 0.09 | ||
| Median daily total costs (euro) | 598.4 [249.1, 1296.7] | 350.2 [38.7, 2884.7] | 366.6 [186.2, 2624.3] | <0.01 * | 0.01 * | 0.02 * |
| Variable | Value | p Value |
|---|---|---|
| Age (years) | 62.0 ± 15.9 | 0.88 |
| Vaccinated (%) | 16.7% (n = 6) | |
| Lung involvement (%) | 60 [30, 90] | <0.01 * |
| APACHE II Score | 14.7 ± 7.5 | 0.76 |
| SOFA Score | 4.9 ± 2.9 | 0.49 |
| Days between first symptoms and ICU admission | 7.1 ± 4.2 | 0.27 |
| P/F ratio | 128 ± 50 | <0.01 * |
| Need for invasive mechanical ventilation Days on HFNC | 55.6% (n = 20) 1.5 [0, 8] | 0.38 0.29 |
| Days on NIV | 3.0 [0, 15] | 0.64 |
| Days on IMV | 1 [0, 33] | 0.24 |
| Need for RRT | 22.2% (n = 8) | 0.02 * |
| Need for invasive cardiac output monitoring | 33.3% (n = 12) | 0.22 |
| Antiviral treatment | 88.9% (n = 32) | 0.02 * |
| Immunomodulatory treatment | 36.1% (n = 13) | <0.01 * |
| ICU LoS | 14.1 ± 8.1 | 0.81 |
| Hospital LOS | 20.1 ± 14.0 | 0.01 * |
| Survival (%) | 52.7% (n = 19) | 0.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, M.; Ştefan, O.M.; Ştefan, M.; Văleanu, L.; Tomescu, D. ICU-Associated Costs during the Fourth Wave of the COVID-19 Pandemic in a Tertiary Hospital in a Low-Vaccinated Eastern European Country. Int. J. Environ. Res. Public Health 2022, 19, 1781. https://doi.org/10.3390/ijerph19031781
Popescu M, Ştefan OM, Ştefan M, Văleanu L, Tomescu D. ICU-Associated Costs during the Fourth Wave of the COVID-19 Pandemic in a Tertiary Hospital in a Low-Vaccinated Eastern European Country. International Journal of Environmental Research and Public Health. 2022; 19(3):1781. https://doi.org/10.3390/ijerph19031781
Chicago/Turabian StylePopescu, Mihai, Oana Mara Ştefan, Mihai Ştefan, Liana Văleanu, and Dana Tomescu. 2022. "ICU-Associated Costs during the Fourth Wave of the COVID-19 Pandemic in a Tertiary Hospital in a Low-Vaccinated Eastern European Country" International Journal of Environmental Research and Public Health 19, no. 3: 1781. https://doi.org/10.3390/ijerph19031781
APA StylePopescu, M., Ştefan, O. M., Ştefan, M., Văleanu, L., & Tomescu, D. (2022). ICU-Associated Costs during the Fourth Wave of the COVID-19 Pandemic in a Tertiary Hospital in a Low-Vaccinated Eastern European Country. International Journal of Environmental Research and Public Health, 19(3), 1781. https://doi.org/10.3390/ijerph19031781






