Usability and Engagement Testing of mHealth Apps in Paediatric Obesity: A Narrative Review of Current Literature
Abstract
1. Introduction
1.1. Background to mHealth
1.2. mHealth Interventions in Paediatric Obesity Treatment
1.3. Technical Usability and Engagement Testing
2. Methods
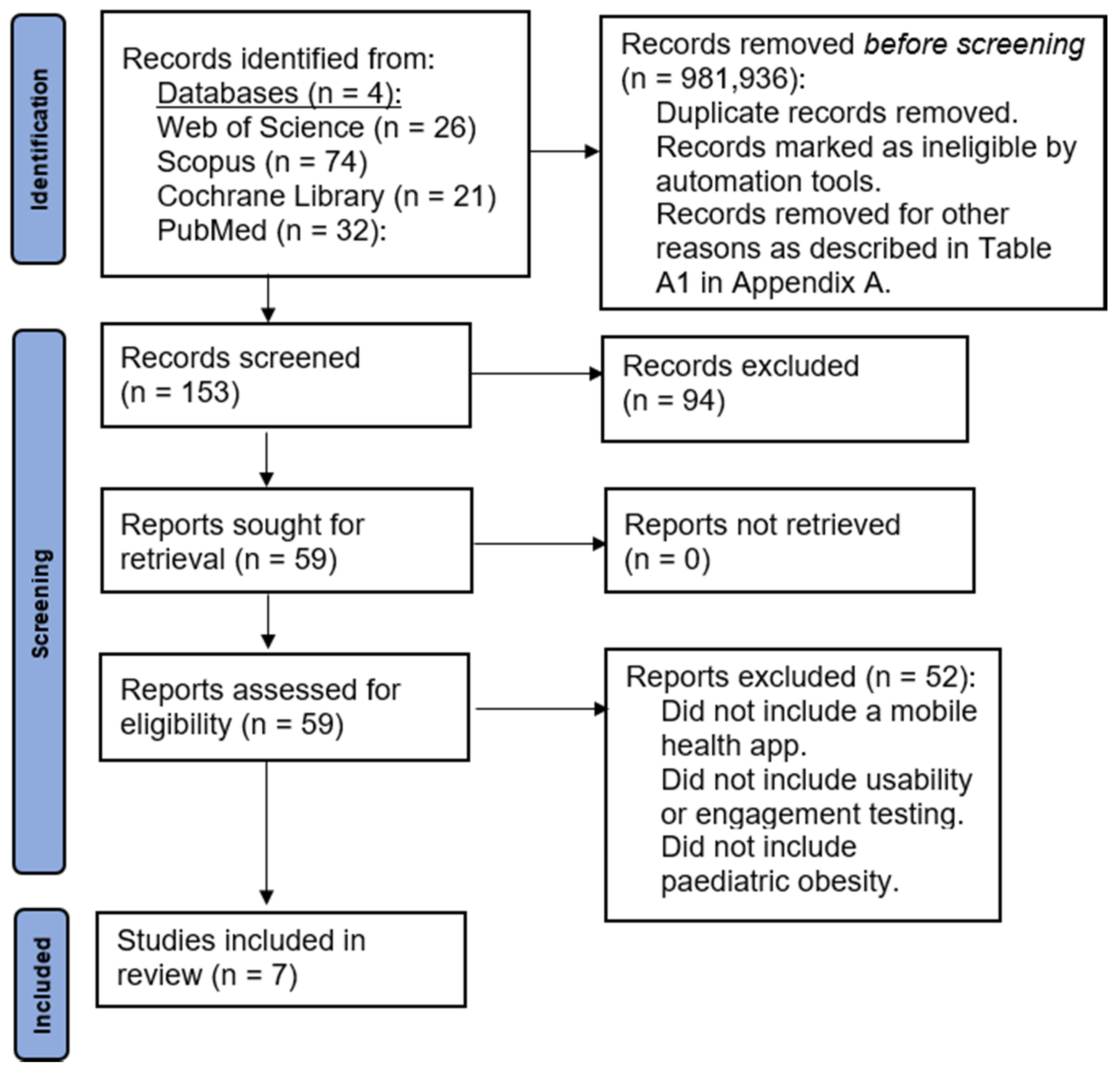
2.1. Information Sources and Search Strategy
2.2. Study Selection
2.2.1. Inclusion Criteria and Searches
- Written in English,
- Involving children and/or adolescents with overweight or obesity (as defined by the study authors),
- Under the age of 18 years,
- Focussed on usability and engagement testing of mHealth applications.
2.2.2. Outcome Measures
3. Results
3.1. Characteristics of Included Studies
3.2. Methods for Evaluating Usability and Engagement in Current Literature
4. Discussion
4.1. Comparison with Usability and Engagement Testing in Other Areas of Paediatrics
4.2. Implications for Practice and Research
4.3. Limitations of Current Usability and Engagement Testing Methods
4.4. Limitations of This Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Search Terms | Database Searched | No. of Hits Screened | Limits Applied |
|---|---|---|---|
| child OR adolescent OR teenager AND obesity AND mobile health application AND usability | Web of Science | 26 | Excluded (n = 981,850): Not peer-reviewed *. Not in English language. Not within time span 2009–2021. Refined by topic “mobile health application”. Refined by topic “AND usability”. |
| childhood AND obesity AND mobile AND health AND Applications * | Scopus | 74 | Excluded (n = 49): Not peer-reviewed. Not in English language (n = 2). Did not include “usability” (n = 47). |
| Childhood OR Adolescence * AND Obesity AND Mobile Phone Application * | Cochrane Library | 0 | N/A |
| obesity in Title Abstract Keyword AND childhood or adolescent or teenager in Title Abstract Keyword AND mobile health application in Title Abstract Keyword—(Word variations were searched) | Cochrane Library | 21 | Excluded (n = 20): Multiple publications (n = 12). Not children/adolescents (n = 4). Not a mobile phone app (n = 4). |
| childhood obesity And Mobile health application And usability And engagement testing | PubMed | 0 | N/A |
| childhood or adolescent or teenagers AND obesity AND Mobile health application * AND usability AND engagement testing | PubMed | 3 | N/A |
| childhood obesity AND Mobile health application | PubMed | 29 | Excluded (n = 18): –Did not involve human participants (n = 14). –Did not involve children/adolescents (n = 4). |
Appendix B
References
- National Institute for Health and Care Excellence (NICE). Obesity: Identification, Assessment and Management: Clinical Guideline [CG189]; National Clinical Guideline Centre: London, UK, 2014; Available online: http://www.nice.org.uk/guidance/cg189 (accessed on 26 October 2021).
- O’Connor, E.A.; Evans, C.V.; Burda, B.U.; Walsh, E.S.; Eder, M.; Lozano, P.J.J. Screening for obesity and intervention for weight management in children and adolescents: Evidence report and systematic review for the US Preventive Services Task Force. Jama 2017, 317, 2427–2444. [Google Scholar] [CrossRef]
- Oude Luttikhuis, H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Cochrane review: Interventions for treating obesity in children. Evid. Based Child Health A Cochrane Rev. J. 2009, 4, 1571–1729. [Google Scholar] [CrossRef]
- Golan, M.; Kaufman, V.; Shahar, D.R. Childhood obesity treatment: Targeting parents exclusively v. parents and children. Br. J. Nutr. 2006, 95, 1008–1015. [Google Scholar] [CrossRef]
- Forsell, C.; Gronowitz, E.; Larsson, Y.; Kjellberg, B.M.; Friberg, P.; Mårild, S.J.A.P. Four-year outcome of randomly assigned lifestyle treatments in primary care of children with obesity. Acta Paediatr. 2019, 108, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Skelton, J.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef]
- Marcin, J.P.; Ellis, J.; Mawis, R.; Nagrampa, E.; Nesbitt, T.S.; Dimand, R.J.J.P. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics 2004, 113, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Mulder, C.; Twisk, J.W.; Van Mechelen, W.; Chinapaw, M.J. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef]
- Lindberg, L.; Danielsson, P.; Persson, M.; Marcus, C.; Hagman, E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: A Swedish prospective cohort study. PLoS Med. 2020, 17, e1003078. [Google Scholar] [CrossRef] [PubMed]
- Hagman, E.; Danielsson, P.; Brandt, L.; Ekbom, A.; Marcus, C. Association between impaired fasting glycaemia in pediatric obesity and type 2 diabetes in young adulthood. Nutr. Diabetes 2016, 6, e227. [Google Scholar] [CrossRef] [PubMed]
- Cummins, N.; Schuller, B.W. Five Crucial Challenges in Digital Health. Front. Digit. Health 2020, 2. [Google Scholar] [CrossRef]
- World Health Organisation. eHealth Online. 2022. Available online: http://www.emro.who.int/health-topics/ehealth/ (accessed on 26 October 2021).
- Dicianno, B.E.; Parmanto, B.; Fairman, A.D.; Crytzer, T.M.; Yu, D.X.; Pramana, G.; Coughenour, D.; Petrazzi, A.A. Perspectives on the evolution of mobile (mHealth) technologies and application to rehabilitation. Phys. Ther. 2015, 95, 397–405. [Google Scholar] [CrossRef]
- Holm, J.C.; Nowicka, P.; Farpour-Lambert, N.J.; O’Malley, G.; Hassapidou, M.; Weiss, R.; Baker, J.L. The Ethics of Childhood Obesity Treatment—from the Childhood Obesity Task Force (COTF) of European Association for the Study of Obesity (EASO). Obes. Facts 2014, 7, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Tully, L.; Case, L.; Arthurs, N.; Sorensen, J.; Marcin, J.P.; O’Malley, G. Barriers and Facilitators for Implementing Paediatric Telemedicine: Rapid Review of User Perspectives. Front. Pediatr. 2021, 9, 630365. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Clinical Excellence (NICE). Weight Management: Lifestyle Services For Overweight or Obese Children and Young People; National Institute for Health and Clinical Excellence (NICE): London, UK, 2013. [Google Scholar]
- Tate, E.B.; Spruijt-Metz, D.; O’Reilly, G.; Jordan-Marsh, M.; Gotsis, M.; Pentz, M.A.; Dunton, G.F. mHealth approaches to child obesity prevention: Successes, unique challenges, and next directions. Transl. Behav. Med. 2013, 3, 406–415. [Google Scholar] [CrossRef]
- Pocketgamer.biz. App Store Metrics. 2021. Available online: https://www.pocketgamer.biz/metrics/app-store/categories/ (accessed on 26 October 2021).
- AppBrain. Android Statistics. 2021. Available online: https://www.appbrain.com/stats/android-market-app-categories (accessed on 26 October 2021).
- Maramba, I.; Chatterjee, A.; Newman, C. Methods of usability testing in the development of eHealth applications: A scoping review. Int. J. Med. Inform. 2019, 126, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Tully, L.; Burls, A.; Sorensen, J.; El-Moslemany, R.; O’Malley, G. Mobile Health for Pediatric Weight Management: Systematic Scoping Review. JMIR Mhealth Uhealth 2020, 8, e16214. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-L.; Guedes, C.M.; Cooper, B.A.; Lung, A.E. Short-Term Efficacy of an Innovative Mobile Phone Technology-Based Intervention for Weight Management for Overweight and Obese Adolescents: Pilot Study. Interact J. Med. Res. 2017, 6, e12. [Google Scholar] [CrossRef]
- Lubans, D.R.; Smith, J.J.; Skinner, G.; Morgan, P.J. Development and implementation of a smartphone application to promote physical activity and reduce screen-time in adolescent boys. Front. Public Health 2014, 2, 42. [Google Scholar] [CrossRef]
- O’Malley, G.; Dowdall, G.; Burls, A.; Perry, I.J.; Curran, N. Exploring the usability of a mobile app for adolescent obesity management. JMIR Mhealth Uhealth 2014, 2, e29. [Google Scholar] [CrossRef]
- O’Malley, G.C. Childhood Obesity Treatment: Integrating Mobile Health Technology into a Paediatric Obesity Service. Ph.D. Thesis, University College Cork, Cork, Ireland, 2015. [Google Scholar]
- LeRouge, C.; Durneva, P.; Sangameswaran, S.; Gloster, A.-M. Design Guidelines for a Technology-Enabled Nutrition Education Program to Support Overweight and Obese Adolescents: Qualitative User-Centered Design Study. J. Med. Internet Res. 2019, 21, e14430. [Google Scholar] [CrossRef]
- Pretlow, R.A.; Stock, C.M.; Allison, S.; Roeger, L. Treatment of child/adolescent obesity using the addiction model: A smartphone app pilot study. Child Obes. 2015, 11, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Johansson, L.; Hagman, E.; Danielsson, P. A novel interactive mobile health support system for pediatric obesity treatment: A randomized controlled feasibility trial. BMC Pediatr. 2020, 20, 447. [Google Scholar] [CrossRef] [PubMed]
- Mameli, C.; Brunetti, D.; Colombo, V.; Bedogni, G.; Schneider, L.; Penagini, F.; Borsani, B.; Zuccotti, G.V. Combined use of a wristband and a smartphone to reduce body weight in obese children: Randomized controlled trial. Pediatr. Obes. 2018, 13, 81–87. [Google Scholar] [CrossRef]
- Jensen, C.D.; Duncombe, K.M.; Lott, M.A.; Hunsaker, S.L.; Duraccio, K.M.; Woolford, S.J. An Evaluation of a Smartphone-Assisted Behavioral Weight Control Intervention for Adolescents: Pilot Study. JMIR Mhealth Uhealth 2016, 4, e102. [Google Scholar] [CrossRef]
- Cueto, V.; Wang, C.J.; Sanders, L.M. Impact of a Mobile App-Based Health Coaching and Behavior Change Program on Participant Engagement and Weight Status of Overweight and Obese Children: Retrospective Cohort Study. JMIR Mhealth Uhealth 2019, 7, e14458. [Google Scholar] [CrossRef]
- Browne, S.; Kechadi, M.T.; O’Donnell, S.; Dow, M.; Tully, L.; Doyle, G.; O’Malley, G. Mobile Health Apps in Pediatric Obesity Treatment: Process Outcomes From a Feasibility Study of a Multicomponent Intervention. JMIR Mhealth Uhealth 2020, 8, e16925. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, Physical Activity and Behavioural Interventions for the Treatment of Overweight or Obese Children from the Age of 6 to 11 Years. Cochrane Database Syst. Rev. 2017, 6, CD012651. Available online: http://europepmc.org/abstract/MED/28639319 (accessed on 26 October 2021). [CrossRef] [PubMed]
- Al-Khudairy, L.; Loveman, E.; Colquitt, J.L.; Mead, E.; Johnson, R.E.; Fraser, H.; Olajide, J.; Murphy, M.; Marian Velho, R.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst. Rev. 2017, 6, CD012691. Available online: http://europepmc.org/abstract/MED/28639320 (accessed on 26 October 2021). [CrossRef] [PubMed]
- Appel, H.B.; Huang, B.; Cole, A.; James, R.; Ai, A.L. Starting the Conversation—A Childhood Obesity Knowledge Project Using an App. Br. J. Med. Med Res. 2014, 4, 1526–1538. [Google Scholar] [CrossRef]
- Smith, J.J.; Morgan, P.J.; Plotnikoff, R.C.; Dally, K.A.; Salmon, J.; Okely, A.D.; Finn, T.L.; Lubans, D.R. Smart-phone obesity prevention trial for adolescent boys in low-income communities: The ATLAS RCT. Pediatrics 2014, 134, e723–e731. [Google Scholar] [CrossRef]
- Nollen, N.L.; Mayo, M.S.; Carlson, S.E.; Rapoff, M.A.; Goggin, K.J.; Ellerbeck, E.F. Mobile technology for obesity prevention: A randomized pilot study in racial—and ethnic-minority girls. Am. J. Prev. Med. 2014, 46, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Turner, T.; Spruijt-Metz, D.; Wen, C.K.; Hingle, M.D. Prevention and treatment of pediatric obesity using mobile and wireless technologies: A systematic review. Pediatr. Obes. 2015, 10, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Quelly, S.B.; Norris, A.E.; DiPietro, J.L. Impact of mobile apps to combat obesity in children and adolescents: A systematic literature review. J. Spec. Pediatr. Nurs. JSPN 2016, 21, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Fedele, D.A.; McConville, A.; Moon, J.; Thomas, J.G. Topical Review: Design Considerations When Creating Pediatric Mobile Health Interventions: Applying the IDEAS Framework. J. Pediatr. Psychol. 2019, 44, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Stoll, R.; Pina, A.; Gary, K.; Amresh, A. Usability of a Smartphone Application to Support the Prevention and Early Intervention of Anxiety in Youth. Cogn. Behav. Pract. 2017, 24, 393–404. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lalmas, M.; O’Brien, H.; Yom-Tov, E. Measuring User Engagement. Synth. Lect. Inf. Concepts Retrieva, Serv. 2014, 6, 1–132. [Google Scholar] [CrossRef]
- Wiebe, E.N.; Lamb, A.; Hardy, M.; Sharek, D. Measuring engagement in video game-based environments: Investigation of the User Engagement Scale. Comput. Hum. Behavior. 2014, 32, 123–132. [Google Scholar] [CrossRef]
- Taki, S.; Lymer, S.; Russell, C.G.; Campbell, K.; Laws, R.; Ong, K.-L.; Elliott, R.; Denney-Wilson, E.; Scott, J.; Baptista, S.; et al. Assessing User Engagement of an mHealth Intervention: Development and Implementation of the Growing Healthy App Engagement Index. JMIR Mhealth Uhealth 2017, 5, e89. [Google Scholar] [CrossRef]
- Newton, A.; March, S.; Gehring, N.; Rowe, A.; Radomski, A. Establishing a Working Definition of User Experience for eHealth Interventions: A Scoping Review of Self-Reported User Experience Measures and Delphi Consultation with eHealth Researchers and Adolescents (Preprint). J. Med. Int. Res. 2020, 23, e25012. [Google Scholar] [CrossRef]
- Albert, B.; Tullis, T. The User Experience: Collecting, Analyzing, And Presenting Usability Metrics (Interactive Technologies), 2nd ed.; Morgan Kaufmann: San Diego, CA, USA, 2013; pp. 99–119. [Google Scholar]
- Wilding, J.; Halford, J.C. Facing the Challenges for Europe—Research into Action: Liverpool European Congress of Obesity, 12–15 May 2013. Obes. Facts 2012, 5, 629–634. [Google Scholar] [CrossRef]
- Yen, P.Y.; Bakken, S. Review of health information technology usability study methodologies. J. Am. Med. Inform. Assoc. JAMIA 2012, 19, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Kergel, D. Digital Learning in Motion: From Book Culture to the Digital Age; Routledge: London, UK, 2020. [Google Scholar]
- Kowatsch, T.; Volland, D.; Shih, I.; Rüegger, D.; Künzler, F.; Barata, F.; Filler, A.; Büchter, D.; Brogle, B.; Heldt, K.; et al. Design and Evaluation of a Mobile Chat App for the Open Source Behavioral Health Intervention Platform MobileCoach. In Proceedings of the International Conference on Design Science Research in Information System and Technology, Karlsruhe, Germany, 30 May–1 June 2017; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Gabrielli, S.; Dianti, M.; Maimone, R.; Betta, M.; Filippi, L.; Ghezzi, M.; Forti, S. Design of a Mobile App for Nutrition Education (TreC-LifeStyle) and Formative Evaluation with Families of Overweight Children. JMIR Mhealth Uhealth 2017, 5, e48. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Jahan, Y.; Fahad, H. Impact of mHealth service: An understanding of TreCLifeStyle mobile app in Trentino province, Italy. Int. J. Healthc. Manag. 2020, 13, 480–487. [Google Scholar] [CrossRef]
- Sandhu, H.; Wilson, K.; Reed, N.; Mihailidis, A. A Mobile Phone App for the Self-Management of Pediatric Concussion: Development and Usability Testing. JMIR Hum. Factors 2019, 6, e12135. [Google Scholar] [CrossRef]
- Dexheimer, J.W.; Kurowski, B.G.; Anders, S.H.; McClanahan, N.; Wade, S.L.; Babcock, L. Usability evaluation of the SMART application for youth with mTBI. Int. J. Med. Inform. 2017, 97, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Bevan, N. Practical Issues in Usability Measurement. Interactions 2006, 13, 42–43. [Google Scholar] [CrossRef]
- Verdaguer, S.; Mateo, K.F.; Wyka, K.; Dennis-Tiwary, T.A.; Leung, M.M. A Web-Based Interactive Tool to Reduce Childhood Obesity Risk in Urban Minority Youth: Usability Testing Study. JMIR Form. Res. 2018, 2, e21. [Google Scholar] [CrossRef] [PubMed]
- Cai, R.A.; Beste, D.; Chaplin, H.; Varakliotis, S.; Suffield, L.; Josephs, F.; Sen, D.; Wedderburn, L.R.; Ioannou, Y.; Hailes, S.; et al. Developing and Evaluating JIApp: Acceptability and Usability of a Smartphone App System to Improve Self-Management in Young People With Juvenile Idiopathic Arthritis. JMIR Mhealth Uhealth 2017, 5, e121. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.B.; Stephenson, J.; Ells, L.; Adu-Ntiamoah, S.; DeSmet, A.; Giles, E.L.; Haste, A.; O’Malley, C.; Jones, D.; Chai, L.K.; et al. The effectiveness of e-health interventions for the treatment of overweight or obesity in children and adolescents: A systematic review and meta-analysis. Obes. Rev. 2021, 23, e13373. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Sadeghi, M.; As’habi, A.; Rahmati, P.; Sheikhtaheri, A. Mobile apps for weight management in children and adolescents; An updated systematic review. Patient Educ. Couns. 2021, 104, 2181–2188. [Google Scholar] [CrossRef]
- Vidmar, A.P.; Salvy, S.J.; Pretlow, R.; Mittelman, S.D.; Wee, C.P.; Fink, C.; Fox, D.S. An addiction-based mobile health weight loss intervention: Protocol of a randomized controlled trial. Contemp. Clin. Trials. 2019, 78, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Reducing Adolescent Obesity with a Mobile Fitness Application: Study Results of Youth Age 15 to 17. In Proceedings of the IEEE 15th International Conference on E-Health Networking, Applications and Services (Healthcom 2013), Lisbon, Portugal, 9–12 October 2013; IEEE: Manhattan, NY, USA, 2013.
- McCullagh, K. The General Data Protection Regulation: A Partial Success for Children on Social Network Sites? In Data Protection, Privacy and European Regulation in the Digital Age; Bräutigam, T., Miettinen, S., Eds.; Unigrafia: Helsinki, Finland, 2016; pp. 110–139. ISBN 978-951-51-2530-9. Available online: https://ssrn.com/abstract=2985724 (accessed on 26 October 2021).
- A Collaboration between the Organisation for the Review of Care and Health Applications (ORCHA) & the British Dietetic Association (BDA). In Mobile Health Approaches to Weight Management: Food for Thought; ORCHA Health: Daresbury, UK, 2021; Available online: https://www.orcha.co.uk/media/1750/orcha_bda-report_jan_2021.pdf (accessed on 26 October 2021).
- Diou, C.; Sarafis, I.; Papapanagiotou, V.; Ioakimidis, I.; Delopoulos AJSJotI. A methodology for obtaining objective measurements of population obesogenic behaviors in relation to the environment. Stat. J. IAOS 2019, 35, 677–690. [Google Scholar] [CrossRef]
| P | Population | Children and adolescents (0–18 years) living with overweight/obesity (as defined by individual studies) |
| C | Concept | Usability (the extent that a product can complete certain tasks in an effective, efficient and satisfactory manner by specific users and in a defined setting) and engagement as defined by the study authors. |
| C | Context | mHealth interventions (the use of smart mobile devices such as phones or tablet PCs) to deliver partial or full weight management programmes |
| Reference and Country (City) | Study Design | Sample Characteristics (Age and Condition) | App Features | Method | Usability and Engagement Outcomes Reported |
|---|---|---|---|---|---|
| (O’ Malley et al., 2014) [24] Ireland (Dublin) | Quantitative and qualitative | 12–17 years living with overweight/obesity (BMI ≥ 98th percentile) (n = 10). Female (n = 3), male (n = 7). | Self-monitoring of PA and food intake, goal setting, social support, tips and rewards. | Time-on-task of novice and expert users. Standardised software usability measurement inventory (SUMI). | Technical usability by end-users. Relative user efficiency score. |
| (Gabrielli et al., 2017) [51] Italy (Trento) | Quantitative and qualitative | 7–12 years who are overweight (BMI 85th–94th percentile) (n = 6). Their parents (n = 6). | PA and diet monitoring. Diet advice. | System Usability Scale (SUS) questionnaire with parents only. Semi-structured interviews with parents and children. | Usability by end-users and suggestions for further improvements. |
| (Kowatsch et al., 2017) [50] Switzerland (St. Gallen) | Qualitative and quantitative | Children undergoing treatment for obesity. Female (n = 8), male (n = 3). Mean age = 12.6 years, SD = 2.4 (n = 11). | Self-monitoring of PA. | Observation. Questionnaire. 7-point Likert scale. | Usability and acceptability by end-users. |
| (Cueto et al., 2019) [31] USA (California) | Quantitative | 5–18 years living with overweight (BMI ≥ 85th percentile)/obesity (BMI ≥ 98th percentile) (n = 1120). | Self-monitoring of eating and PA. Individualised coaching sessions. | The overall collective number of individual coaching sessions, coaching messages, dietary events, and physical-activity events that participants took part in throughout the participation phase. Additionally, the duration of the participation period and programme retention. | High participant engagement. |
| (LeRouge et al., 2019) [26] USA (Washington) | Qualitative and quantitative | 9–18 years with overweight/obesity (BMI 85th–99th percentile range) Phase 1 (n = 48), parents (n = 15), HCPs (n = 6). Phase 2 12–17 years (n = 70), HCPs (n = 10). | Social networking, motivation, “recipe builder”, PA and food management. | Think out loud, semantic differential scale and semi-structured interviews. | Usability by end users. |
| (Browne et al., 2020) [32] Ireland (Dublin) | Qualitative and quantitative | 9–16 years with obesity (BMI ≥ 98th percentile) (n = 20). | PA and diet monitoring. | System usability score surveys, verbal feedback. Engagement was measured from the number of training meals completed and volume of data collected. | Usability was reported for the BigO app but not for the Mandolean app. Low engagement levels and poor acceptability were reported for both apps. Further technical usability testing was advised. |
| (Rahman et al., 2020) [52] Italy (Trentino) | Qualitative and quantitative | 6–12 Years with obesity (n = 6), parents (n = 6), | PA and diet monitoring. Nutrition and portion size information. | System usability scale questionnaire and semi-structured interviews focussed on interface preferences, eating behaviours, and user experience. | Both usability and user satisfaction were reported for both versions of the app but appB received a higher average usability score (score > 92) than appA (score > 85) for its friendly interface and elaborative components. Technological modifications suggested. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arthurs, N.; Tully, L.; O’Malley, G.; Browne, S. Usability and Engagement Testing of mHealth Apps in Paediatric Obesity: A Narrative Review of Current Literature. Int. J. Environ. Res. Public Health 2022, 19, 1453. https://doi.org/10.3390/ijerph19031453
Arthurs N, Tully L, O’Malley G, Browne S. Usability and Engagement Testing of mHealth Apps in Paediatric Obesity: A Narrative Review of Current Literature. International Journal of Environmental Research and Public Health. 2022; 19(3):1453. https://doi.org/10.3390/ijerph19031453
Chicago/Turabian StyleArthurs, Niamh, Louise Tully, Grace O’Malley, and Sarah Browne. 2022. "Usability and Engagement Testing of mHealth Apps in Paediatric Obesity: A Narrative Review of Current Literature" International Journal of Environmental Research and Public Health 19, no. 3: 1453. https://doi.org/10.3390/ijerph19031453
APA StyleArthurs, N., Tully, L., O’Malley, G., & Browne, S. (2022). Usability and Engagement Testing of mHealth Apps in Paediatric Obesity: A Narrative Review of Current Literature. International Journal of Environmental Research and Public Health, 19(3), 1453. https://doi.org/10.3390/ijerph19031453






