Mental Health during COVID-19 Pandemic: The Role of Optimism and Emotional Regulation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Approach and Procedure
2.2. Participants and Sampling Strategy
2.3. Measures
2.4. Statistical Analyses
3. Results
3.1. Descriptive Statistics, Internal Consistency and Pearson Correlation Coefficients
3.2. Competing Measurement Models
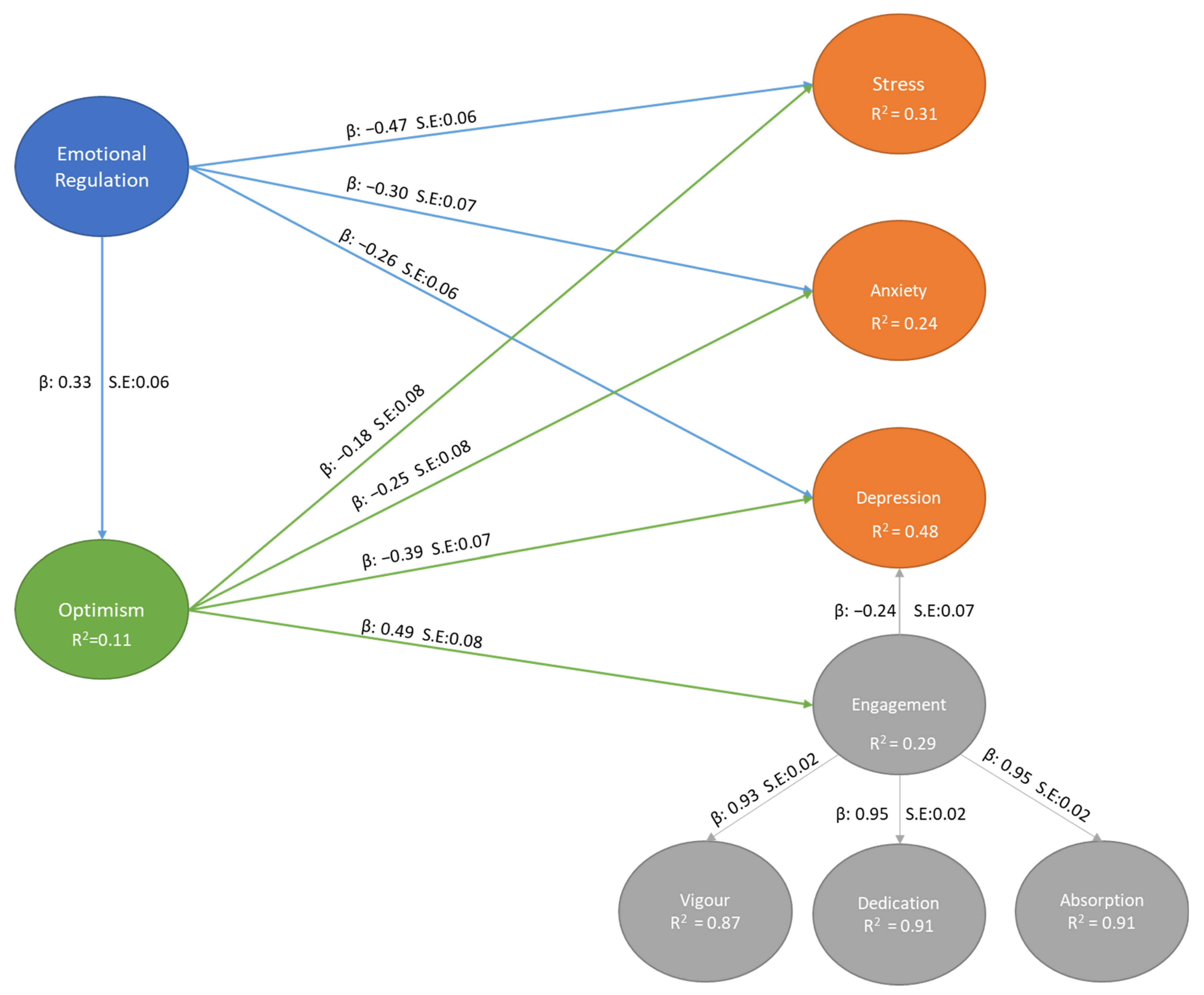
3.3. Estimating the Structural Model
3.4. Assessing the Indirect Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PEC | Profile of Emotional Competence |
| LOT-R | Life Orientation Test-Revised |
| UWES | Utrecht Work Engagement Scale |
| DAS-21 | Depression, Anxiety and Stress Scale-21 |
References
- Chen, R.-N.; Liang, S.-W.; Peng, Y.; Li, X.-G.; Chen, J.-B.; Tang, S.-Y.; Zhao, J.-B. Mental health status and change in living rhythms among college students in China during the COVID-19 pandemic: A large-scale survey. J. Psychosom. Res. 2020, 137, 110219. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.H.; Sultana, M.S.; Hossain, S.; Hasan, M.T.; Ahmed, H.U.; Sikder, T. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. J. Affect. Disord. 2020, 277, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Salman, M.; Asif, N.; Mustafa, Z.U.; Khan, T.M.; Shehzadi, N.; Hussain, K.; Tahir, H.; Raza, M.H.; Khan, M.T. Psychological Impact of COVID-19 on Pakistani University Students and How They Are Coping. Medrxiv 2020, 1–7. [Google Scholar] [CrossRef]
- Van Zyl, L.E. Social Study Resources and Social Wellbeing Before and During the Intelligent COVID-19 Lockdown in The Netherlands. Soc. Indic. Res. 2021, 157, 393–415. [Google Scholar] [CrossRef]
- Van Zyl, L.E.; Rothmann, S.; Zondervan-Zwijnenburg, M.A.J. Longitudinal Trajectories of Study Characteristics and Mental Health Before and During the COVID-19 Lockdown. Front. Psychol. 2021, 12, 633533. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 2021, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, R.P.; Alonso, J.; Axinn, W.G.; Cuijpers, P.; Ebert, D.D.; Green, J.G.; Hwang, I.; Kessler, R.C.; Liu, H.; Mortier, P.; et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol. Med. 2016, 46, 2955–2970. [Google Scholar] [CrossRef] [Green Version]
- Tang, F.; Byrne, M.; Qin, P. Psychological distress and risk for suicidal behavior among university students in contemporary China. J. Affect. Disord. 2018, 228, 101–108. [Google Scholar] [CrossRef]
- Larcombe, W.; Finch, S.; Sore, R.; Murray, C.M.; Kentish, S.; Mulder, R.A.; Lee-Stecum, P.; Baik, C.; Tokatlidis, O.; Williams, D.A. Prevalence and socio-demographic correlates of psychological distress among students at an Australian university. Stud. High. Educ. 2014, 41, 1074–1091. [Google Scholar] [CrossRef]
- Shankland, R.; Genolini, C.; Franca, L.R.; Guelfi, J.-D.; Ionescu, S. Student adjustment to higher education: The role of alternative educational pathways in coping with the demands of student life. High. Educ. 2009, 59, 353–366. [Google Scholar] [CrossRef]
- Saleh, D.; Camart, N.; Romo, L. Predictors of Stress in College Students. Front. Psychol. 2017, 8, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baghurst, T.; Kelley, B.C. An Examination of Stress in College Students Over the Course of a Semester. Health Promot. Pract. 2014, 15, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Conley, C.S.; Ma, L.V.T.; Bryant, F.B. Promoting Psychosocial Adjustment and Stress Management in First-Year College Students: The Benefits of Engagement in a Psychosocial Wellness Seminar. J. Am. Coll. Health 2013, 61, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Shankland, R.; Kotsou, I.; Vallet, F.; Bouteyre, E.; Dantzer, C.; Leys, C. Burnout in university students: The mediating role of sense of coherence on the relationship between daily hassles and burnout. High. Educ. 2019, 78, 91–113. [Google Scholar] [CrossRef]
- Houghton, J.D.; Wu, J.; Godwin, J.L.; Neck, C.P.; Manz, C.C. Self-Leadership, and Student Stress Coping. J. Manag. Educ. 2012, 36, 220–238. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Thomas, M.R.; Shanafelt, T.D. Systematic Review of Depression, Anxiety, and Other Indicators of Psychological Distress Among, U.S. and Canadian Medical Students. Acad. Med. 2006, 81, 354–373. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Thomas, M.R.; Massie, F.S.; Power, D.V.; Eacker, A.; Harper, W.; Durning, S.; Moutier, C.; Szydlo, D.W.; Novotny, P.J.; et al. Burnout and Suicidal Ideation among U.S. Medical Students. Ann. Intern. Med. 2008, 149, 334–341. [Google Scholar] [CrossRef]
- Kumar, H. Psychological Distress and Life Satisfaction among University Students. J. Psychol. Clin. Psychiatry 2016, 5, 00283. [Google Scholar] [CrossRef] [Green Version]
- Nacht, J. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis. J. Emerg. Med. 2016, 50, 805. [Google Scholar] [CrossRef]
- Papazisis, G.; Papanikolaou, N.; Vlasiadis, I.; Sapountzi-Krepia, D. Psychological Distress, Anxiety and Depression among Nursing Students in Greece. Int. J. Caring Sci. 2008, 1, 42–46. [Google Scholar]
- Pulido-Martos, M.; Augusto-Landa, J.; Lopez-Zafra, E. Sources of stress in nursing students: A systematic review of quantitative studies. Int. Nurs. Rev. 2011, 59, 15–25. [Google Scholar] [CrossRef]
- Chan, C.K.; So, W.K.; Fong, D.Y. Hong Kong Baccalaureate Nursing Students’ Stress and Their Coping Strategies in Clinical Practice. J. Prof. Nurs. 2009, 25, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Lo, R. A longitudinal study of perceived level of stress, coping and self-esteem of undergraduate nursing students: An Australian case study. J. Adv. Nurs. 2002, 39, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Galbraith, N.D.; Brown, K.E. Assessing intervention effectiveness for reducing stress in student nurses: Quantitative systematic review. J. Adv. Nurs. 2011, 67, 709–721. [Google Scholar] [CrossRef]
- Marzouk, M.; Ouanes-Besbes, L.; Ouanes, I.; Hammouda, Z.; Dachraoui, F.; Abroug, F. Prevalence of anxiety and depressive symptoms among medical residents in Tunisia: A cross-sectional survey. BMJ Open 2018, 8, e020655. [Google Scholar] [CrossRef] [Green Version]
- Kwok, S.Y.C.L.; Gu, M. The Role of Emotional Competence in the Association Between Optimism and Depression Among Chinese Adolescents. Child Indic. Res. 2017, 10, 171–185. [Google Scholar] [CrossRef]
- Shaheen, H.; Jahan, M. The Role of Optimism in experience of Student Stress and Suicidal Ideation. IOSR J. Humanit. Soc. Sci. 2014, 19, 23–34. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology 2002, 39, 281–291. [Google Scholar] [CrossRef] [Green Version]
- Lopes, P.N.; Brackett, M.A.; Nezlek, J.; Schütz, A.; Sellin, I.; Salovey, P. Emotional Intelligence and Social Interaction. Pers. Soc. Psychol. Bull. 2004, 30, 1018–1034. [Google Scholar] [CrossRef] [Green Version]
- Lopes, P.N.; Salovey, P.; Côté, S.; Beers, M. Emotion Regulation Abilities and the Quality of Social Interaction. Emotion 2005, 5, 113–118. [Google Scholar] [CrossRef] [Green Version]
- Lopes, P.N.; Salovey, P.; Straus, R. Emotional intelligence, personality, and the perceived quality of social relationships. Pers. Individ. Differ. 2003, 35, 641–658. [Google Scholar] [CrossRef]
- Capone, V.; Caso, D.; Donizzetti, A.; Procentese, F. University Student Mental Well-Being during COVID-19 Outbreak: What Are the Relationships between Information Seeking, Perceived Risk and Personal Resources Related to the Academic Context? Sustainability 2020, 12, 7039. [Google Scholar] [CrossRef]
- Cilliers, J.; Mostert, K.; Nel, J. Study demands, study resources and the role of personality characteristics in predicting the engagement of fist-year university students. S. Afr. J. High. Educ. 2017, 32, 49–70. [Google Scholar] [CrossRef] [Green Version]
- Lea, R.; Davis, S.; Mahoney, B.; Qualter, P. Does Emotional Intelligence Buffer the Effects of Acute Stress? A Systematic Review. Front. Psychol. 2019, 10, 810. [Google Scholar] [CrossRef] [PubMed]
- Drigas, A.; Papoutsi, C. The Need for Emotional Intelligence Training Education in Critical and Stressful Situations: The Case of COVID-19. Int. J. Recent Contrib. Eng. Sci. IT 2020, 8, 20–36. [Google Scholar] [CrossRef]
- Gross, J.J. The Emerging Field of Emotion Regulation: An Integrative Review. Rev. Gen. Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion Regulation: Current Status and Future Prospects. Psychol. Inq. 2015, 26, 1–26. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Regulation of Positive Emotions: Emotion Regulation Strategies that Promote Resilience. J. Happiness Stud. 2007, 8, 311–333. [Google Scholar] [CrossRef]
- Ashby, F.G.; Isen, A.M.; Turken, A.U. A neuropsychological theory of positive affect and its influence on cognition. Psychol. Rev. 1999, 106, 529–550. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient Individuals Use Positive Emotions to Bounce Back from Negative Emotional Experiences. J. Pers. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef] [Green Version]
- Vizoso, C.; Arias-Gundín, O.; Rodríguez, C. Exploring coping and optimism as predictors of academic burnout and performance among university students. Educ. Psychol. 2019, 39, 768–783. [Google Scholar] [CrossRef]
- Burris, J.L.; Brechting, E.H.; Salsman, J.; Carlson, C.R. Factors Associated with the Psychological Well-Being and Distress of University Students. J. Am. Coll. Health 2009, 57, 536–543. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C. Effects of optimism on psychological and physical well-being: Theoretical overview and empirical update. Cogn. Ther. Res. 1992, 16, 201–228. [Google Scholar] [CrossRef]
- Gómez-Molinero, R.; Zayas, A.; Ruíz-González, P.; Guil, R. Optimism and resilience among university students. Int. J. Dev. Ment. Educ. Psychol. Rev. INFAD Psicol. 2018, 1, 147–154. [Google Scholar] [CrossRef] [Green Version]
- Peterson, C.; Steen, T.A. Optimistic Explanatory Style. In Handbook of Positive Psychology; Snyder, C.R., Lopez, S.J., Eds.; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Lesener, T.; Pleiss, L.S.; Gusy, B.; Wolter, C. The Study Demands-Resources Framework: An Empirical Introduction. Int. J. Environ. Res. Public Health 2020, 17, 5183. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Salanova, M.; González-Romá, V.; Bakker, A.B. The Measurement of Engagement and Burnout: A Two Sample Confirmatory Factor Analytic Approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Martinez, I.M.M.; Pinto, A.M.; Salanova, M.; Bakker, A.B. Burnout and Engagement in University Students. J. Cross-Cult. Psychol. 2002, 33, 464–481. [Google Scholar] [CrossRef] [Green Version]
- Schaufeli, W.B. General Engagement: Conceptualization and Measurement with the Utrecht General Engagement Scale (UGES). J. Well-Being Assess. 2017, 1, 9–24. [Google Scholar] [CrossRef]
- Salanova, M.; Schaufeli, W.; Martinez, I.M.M.; Breso, E. How obstacles and facilitators predict academic performance: The mediating role of study burnout and engagement. AnxietyStress Coping 2010, 23, 53–70. [Google Scholar] [CrossRef]
- Tayama, J.; Schaufeli, W.; Shimazu, A.; Tanaka, M.; Takahama, A. Validation of a Japanese Version of the Work Engagement Scale for Students. Jpn. Psychol. Res. 2019, 61, 262–272. [Google Scholar] [CrossRef] [Green Version]
- Brasseur, S.; Grégoire, J.; Bourdu, R.; Mikolajczak, M. The Profile of Emotional Competence (PEC): Development and Validation of a Self-Reported Measure that Fits Dimensions of Emotional Competence Theory. PLoS ONE 2013, 8, e62635. [Google Scholar] [CrossRef] [Green Version]
- Segerstrom, S.C.; Evans, D.R.; Eisenlohr-Moul, T.A. Optimism and pessimism dimensions in the Life Orientation Test-Revised: Method and meaning. J. Res. Pers. 2011, 45, 126–129. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Salanova, M. The Measurement of Work Engagement with a Short Questionnaire: A Cross-National Study. Educ. Psychol. Meas. 2006, 66, 701–716. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B. UWES-Utrecht Work Engagement Scale: Test Manual; Utrecht University: Utrecht, The Netherlands, 2003. [Google Scholar]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Coker, A.; Coker, O.; Sanni, D. Psychometric properties of the 21-item Depression Anxiety Stress Scale (DASS-21). Afr. Res. Rev. 2018, 12, 135. [Google Scholar] [CrossRef]
- IBM. SPSS Statistics for Windows, Version 26.0; IBM Corp.: Armonk, NY, USA, 2019.
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Mplus: Los Angeles, CA, USA, 2020. [Google Scholar]
- Kim, H.-Y. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef]
- Raykov, T. Evaluation of Scale Reliability for Unidimensional Measures Using Latent Variable Modeling. Meas. Evaluation Couns. Dev. 2009, 42, 223–232. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research. In Methodology in the Social Sciences; Guilford Press: New York, NY, USA, 2006; ISBN 978-1-59385-275-7. [Google Scholar]
- Hu, L.-T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- McNeish, D.; Hancock, G.R. The effect of measurement quality on targeted structural model fit indices: A comment on Lance, Beck, Fan, and Carter (2016). Psychol. Methods 2018, 23, 184–190. [Google Scholar] [CrossRef]
- Preacher, K.J.; Zhang, Z.; Zyphur, M. Alternative Methods for Assessing Mediation in Multilevel Data: The Advantages of Multilevel SEM. Struct. Equ. Model. A Multidiscip. J. 2011, 18, 161–182. [Google Scholar] [CrossRef]
- Asparouhov, T.; Muthén, B. Exploratory Structural Equation Modeling. Struct. Equ. Model. A Multidiscip. J. 2009, 16, 397–438. [Google Scholar] [CrossRef]
- Kline, B. Principles and Practice of Structural Equation Modeling, 3rd ed.; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Alnazly, E.; Khraisat, O.M.; Al-Bashaireh, A.M.; Bryant, C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS ONE 2021, 16, e0247679. [Google Scholar] [CrossRef]
- Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef]
- Brissette, I.; Scheier, M.F.; Carver, C.S. The role of optimism in social network development, coping, and psychological adjustment during a life transition. J. Pers. Soc. Psychol. 2002, 82, 102–111. [Google Scholar] [CrossRef]
- Fredrickson, B.L. What Good Are Positive Emotions? Rev. Gen. Psychol. 1998, 2, 300–319. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The Role of Positive Emotions in Positive Psychology. Am. Psychol. 2001, 56, 218. [Google Scholar] [CrossRef]
- Denovan, A.; Dagnall, N.; Macaskill, A.; Papageorgiou, K. Future time perspective, positive emotions and student engagement: A longitudinal study. Stud. High. Educ. 2019, 45, 1533–1546. [Google Scholar] [CrossRef]
- Van der Velden, P.G.; Kleber, R.J.; Fournier, M.; Grievink, L.; Drogendijk, A.; Gersons, B.P. The association between dispositional optimism and mental health problems among disaster victims and a comparison group: A prospective study. J. Affect. Disord. 2007, 102, 35–45. [Google Scholar] [CrossRef]
- Ouweneel, E.; Le Blanc, P.M.; Schaufeli, W.B. Flourishing students: A longitudinal study on positive emotions, personal resources, and study engagement. J. Posit. Psychol. 2011, 6, 142–153. [Google Scholar] [CrossRef] [Green Version]
- Van Zyl, L.E.; Deacon, E.; Rothmann, S. Towards happiness: Experiences of work-role fit, meaningfulness and work engagement of industrial/organisational psychologists in South Africa. SA J. Ind. Psychol. 2010, 36, 10. [Google Scholar] [CrossRef] [Green Version]
- Mascaro, N.; Rosen, D.H. Existential Meaning’s Role in the Enhancement of Hope and Prevention of Depressive Symptoms. J. Pers. 2005, 73, 985–1014. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Schaufeli, W.B. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J. Affect. Disord. 2012, 141, 415–424. [Google Scholar] [CrossRef] [Green Version]
- Ausín, B.; González-Sanguino, C.; Castellanos, M.Á.; Muñoz, M. Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. J. Gend. Stud. 2020, 30, 29–38. [Google Scholar] [CrossRef]
- Barros, C.; Sacau-Fontenla, A. New Insights on the Mediating Role of Emotional Intelligence and Social Support on University Students’ Mental Health during COVID-19 Pandemic: Gender Matters. Int. J. Environ. Res. Public Health 2021, 18, 12935. [Google Scholar] [CrossRef]
- Batra, K.; Sharma, M.; Batra, R.; Singh, T.; Schvaneveldt, N. Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare 2021, 9, 222. [Google Scholar] [CrossRef]
- Prowse, R.; Sherratt, F.; Abizaid, A.; Gabrys, R.L.; Hellemans, K.G.; Patterson, Z.R.; McQuaid, R.J. Coping with the COVID-19 Pandemic: Examining Gender Differences in Stress and Mental Health Among University Students. Front. Psychiatry 2021, 12, 439. [Google Scholar] [CrossRef]
- Harrer, M.; Apolinário-Hagen, J.; Fritsche, L.; Drüge, M.; Krings, L.; Beck, K.; Salewski, C.; Zarski, A.-C.; Lehr, D.; Baumeister, H.; et al. Internet- and App-Based Stress Intervention for Distance-Learning Students with Depressive Symptoms: Protocol of a Randomized Controlled Trial. Front. Psychiatry 2019, 10, 361. [Google Scholar] [CrossRef]
- Hintz, S.; Frazier, P.A.; Meredith, L. Evaluating an online stress management intervention for college students. J. Couns. Psychol. 2015, 62, 137–147. [Google Scholar] [CrossRef]
- Lintvedt, O.K.; Griffiths, K.M.; Sørensen, K.; Østvik, A.R.; Wang, C.E.A.; Eisemann, M.; Waterloo, K. Evaluating the effectiveness and efficacy of unguided internet-based self-help intervention for the prevention of depression: A randomized controlled trial. Clin. Psychol. Psychother. 2011, 20, 10–27. [Google Scholar] [CrossRef]
- Nguyen-Feng, V.N.; Frazier, P.A.; Greer, C.S.; Howard, K.G.; Paulsen, J.A.; Meredith, L.; Kim, S. A randomized controlled trial of a web-based intervention to reduce distress among students with a history of interpersonal violence. Psychol. Violence 2015, 5, 444–454. [Google Scholar] [CrossRef]
- Orbach, G.; Lindsay, S.; Grey, S. A randomised placebo-controlled trial of a self-help Internet-based intervention for test anxiety. Behav. Res. Ther. 2007, 45, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Saleh, D.; Camart, N.; Sbeira, F.; Romo, L. Can we learn to manage stress? A randomized controlled trial carried out on university students. PLoS ONE 2018, 13, e0200997. [Google Scholar] [CrossRef] [Green Version]
- George, D.R.; Dellasega, C.; Whitehead, M.M.; Bordon, A. Facebook-based stress management resources for first-year medical students: A multi-method evaluation. Comput. Hum. Behav. 2013, 29, 559–562. [Google Scholar] [CrossRef]
- Harrer, M.; Adam, S.H.; Fleischmann, R.J.; Baumeister, H.; Auerbach, R.; Bruffaerts, R.; Cuijpers, P.; Kessler, R.C.; Berking, M.; Lehr, D.; et al. Effectiveness of an Internet- and App-Based Intervention for College Students with Elevated Stress: Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e136. [Google Scholar] [CrossRef]
- Davies, E.B.; Morriss, R.; Glazebrook, C.; Gulliver, A.; Spates, C. Computer-Delivered and Web-Based Interventions to Improve Depression, Anxiety, and Psychological Well-Being of University Students: A Systematic Review and Meta-Analysis. J. Med. Internet Res. 2014, 16, e130. [Google Scholar] [CrossRef] [Green Version]
- Day, V.; McGrath, P.; Wojtowicz, M. Internet-based guided self-help for university students with anxiety, depression and stress: A randomized controlled clinical trial. Behav. Res. Ther. 2013, 51, 344–351. [Google Scholar] [CrossRef]
- Baños, R.M.; Etchemendy, E.; Farfallini, L.; García-Palacios, A.; Quero, S.; Botella, C. EARTH of Well-Being System: A pilot study of an Information and Communication Technology-based positive psychology intervention. J. Posit. Psychol. 2014, 9, 482–488. [Google Scholar] [CrossRef] [Green Version]
- Hammill, J.; Nguyen, T.; Henderson, F. Student engagement: The impact of positive psychology interventions on students. Act. Learn. High. Educ. 2020, 146978742095058. [Google Scholar] [CrossRef]
- Machado, L.; De Oliveira, I.R.; Peregrino, A.; Cantilino, A. Common mental disorders and subjective well-being: Emotional training among medical students based on positive psychology. PLoS ONE 2019, 14, e0211926. [Google Scholar] [CrossRef]
- Sitbon, A.; Shankland, R.; Krumm, C.-M. Interventions efficaces en psychologie positive: Une revue systématique. Can. Psychol. Can. 2019, 60, 35–54. [Google Scholar] [CrossRef]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to reduce stress in university students: A review and meta-analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef] [PubMed]
- De Vibe, M.; Solhaug, I.; Tyssen, R.; Friborg, O.; Rosenvinge, J.H.; Sørlie, T.; Bjørndal, A. Mindfulness training for stress management: A randomised controlled study of medical and psychology students. BMC Med. Educ. 2013, 13, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galante, J.; Dufour, G.; Benton, A.; Howarth, E.; Vainre, M.; Croudace, T.; Wagner, A.P.; Stochl, J.; Jones, P.B. Protocol for the Mindful Student Study: A randomised controlled trial of the provision of a mindfulness intervention to support university students’ well-being and resilience to stress. BMJ Open 2016, 6, e012300. [Google Scholar] [CrossRef] [Green Version]
- Theurel, A.; Gimbert, F.; Gentaz, E. Quels sont les bénéfices académiques, cognitifs, socio-émotionnels et psychologiques des interventions basées sur la pleine conscience en milieu scolaire? Une Synthèse De 2018, 154, 1–16. [Google Scholar]
- Barnes, N.; Hattan, P.; Black, D.S.; Schuman-Olivier, Z. An examination of mindfulness-based programs in U.S. medical schools. Mindfulness 2017, 8, 489–494. [Google Scholar] [CrossRef]
- Drigas, A.; Papoutsi, C.; Skianis, C. Metacognitive and Metaemotional Training Strategies through the Nine-layer Pyramid Model of Emotional Intelligence. Int. J. Recent Contrib. Eng. Sci. IT 2021, 9, 58–76. [Google Scholar] [CrossRef]
| Participants’ Characteristics | Frequency | Percentage | |
|---|---|---|---|
| Gender | Females | 344 | 94 |
| Males | 22 | 6 | |
| Accommodation | With Family | 126 | 34.4 |
| Student Residence | 161 | 44 | |
| Rental with friends | 65 | 17.8 | |
| Rental alone | 14 | 3.8 | |
| Marital status (%) | Single | 360 | 98.6 |
| Married | 5 | 1.4 | |
| Children | Yes | 5 | 1.4 |
| No | 361 | 98.6 | |
| Academic field | Podiatry | 43 | 11.7 |
| Emergency Care | 114 | 31.1 | |
| Operating Instrumentation | 77 | 21 | |
| Paediatric care | 96 | 26.2 | |
| Research Masters | 36 | 9.8 | |
| Year of enrolment | 1st year | 142 | 38.8 |
| 2nd year | 128 | 35 | |
| 3rd year | 96 | 26.2 | |
| Repetition of academic year | No | 363 | 99.2 |
| Yes | 3 | 0.8 | |
| Depression | Normal (0–9) | n = 48 | 13.1 |
| Mild (10–13) | n = 127 | 34.7 | |
| Moderate (14–20) | n = 162 | 44.3 | |
| Severe (21–27) | n = 29 | 7.9 | |
| Extremely severe (28+) | --- | --- | |
| Anxiety | Normal (0–7) | n = 6 | 1.6 |
| Mild (8–9) | n = 38 | 10.4 | |
| Moderate (10–14) | n = 160 | 43.7 | |
| Severe (15–19) | n = 123 | 33.6 | |
| Extremely severe (20+) | n = 39 | 10.7 | |
| Stress | Normal (0–14) | n = 186 | 50.8 |
| Mild (15–18) | n = 131 | 35.8 | |
| Moderate (19–25) | n = 47 | 12.8 | |
| Severe (26–33) | n = 2 | 0.5 | |
| Extremely severe (34+) | --- | --- | |
| Vigour | Very low ≤ 2 | n = 8 | 2.2 |
| Low 2.01–3.25 | n = 6 | 1.6 | |
| Average 3.26–4.80 | n = 20 | 5.5 | |
| High 4.81–5.65 | n = 25 | 6.8 | |
| Very High ≥ 5.66 | n = 307 | 83.9 | |
| Dedication | Very low ≤ 1.33 | n = 13 | 3.6 |
| Low 1.34–2.90 | n = 10 | 2.7 | |
| Average 2.91–4.70 | n = 25 | 6.8 | |
| High 4.71–5.69 | n = 9 | 2.5 | |
| Very high ≥ 5.70 | n = 309 | 84.4 | |
| Absorption | Very low ≤ 1.17 | n = 8 | 2.2 |
| Low 1.18–2.33 | n = 13 | 3.6 | |
| Average 2.34–4.20 | n = 23 | 6.3 | |
| High 4.21–5.33 | n = 18 | 4.9 | |
| Very high ≥ 5.51 | n = 304 | 83.1 | |
| Fit Indices | Cut-Off Criterion | Sensitive to N | Penalty for Model Complexity |
|---|---|---|---|
| Absolute fit indices | |||
| Chi-Square (χ2) | Lowest comparative value between measurement models | Yes | No |
| Non-Significant Chi-Square (p > 0.01) | |||
| Approximate Fit Indices | |||
| Root-Means-Square Error of Approximation (RMSEA) | 0.06 to 0.08 (Marginally Acceptable); 0.01 to 0.05 (Excellent) | No | Yes |
| Non-Significant RMSEA (p > 0.01) | |||
| 90% Confidence Interval Range should not include zero | |||
| Standardized Root Mean Square Residual (SRMR) | 0.06 to 0.08 (Marginally Acceptable); 0.01 to 0.05 (Excellent) | Yes | No |
| Incremental fit indices | |||
| Comparative Fit Index (CFI) | 0.90 to 0.95 (Marginally Acceptable Fit); 0.96 to 0.99 (Excellent) | No | No |
| Tucker-Lewis Index (TLI) | 0.90 to 0.95 (Marginally Acceptable Fit); 0.96 to 0.99 (Excellent) | No | Yes |
| Akaike Information Criterion (AIC) | Lowest value in comparative measurement models | Yes | Yes |
| Bayes Information Criterion (BIC) | Lowest value in comparative measurement models | Yes | Yes |
| No | Factor | Mean | SD | Skewness | Kurtosis | ρ | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Stress | 2.11 | 0.46 | 0.38 | 0.29 | 0.77 | - | |||||||
| 2 | Depression | 1.99 | 0.56 | 0.58 | −0.06 | 0.88 | 0.71 | - | - | - | - | - | - | - |
| 3 | Anxiety | 2.03 | 0.56 | 0.41 | −0.16 | 0.85 | 0.87 | 0.76 | - | - | - | - | - | - |
| 4 | Vigour | 3.84 | 1.50 | 0.06 | −0.77 | 0.71 | −0.21 | −0.49 | −0.27 | - | - | - | - | - |
| 5 | Dedication | 4.62 | 1.56 | −0.50 | −0.54 | 0.79 | −0.21 | −0.50 | −0.27 | 0.89 | - | - | - | - |
| 6 | Absorption | 4.29 | 1.41 | −0.19 | −0.54 | 0.65 | −0.21 | −0.50 | −0.27 | 0.89 | 0.91 | - | - | - |
| 7 | Overall Study Engagement | 4.25 | 1.30 | −0.18 | −0.60 | 0.96 | −0.22 | −0.52 | −0.29 | 0.93 | 0.95 | 0.95 | - | - |
| 8 | Optimism | 3.44 | 0.70 | −0.29 | 0.02 | 0.61 | −0.33 | −0.61 | −0.39 | 0.49 | 0.50 | 0.50 | 0.53 | - |
| 9 | Emotion Regulation | 3.44 | 0.92 | −0.36 | −0.32 | 0.74 | −0.53 | −0.46 | −0.41 | 0.26 | 0.27 | 0.27 | 0.28 | 0.33 |
| Model | χ2 | p-Value | df | χ2/df | CFI | TLI | RMSEA | SRMR | OFV | 90% C.I RMSEA | Meets Criteria | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||||||
| Model 1 | 968.72 | 0.00 | 649 | 1.49 | 0.93 | 0.93 | 0.04 | 0.05 | 0.11 | 0.032 | 0.041 | Yes |
| Model 2 | 1169.58 | 0.00 | 688 | 1.70 | 0.90 | 0.89 | 0.04 | 0.06 | 0.15 | 0.039 | 0.048 | No |
| Model 3 | 1338.01 | 0.00 | 694 | 1.93 | 0.87 | 0.86 | 0.05 | 0.07 | 0.18 | 0.046 | 0.054 | No |
| Model 4 | 1153.74 | 0.00 | 703 | 1.64 | 0.90 | 0.89 | 0.05 | 0.06 | 0.15 | 0.041 | 0.050 | No |
| Model 5 | 1122.60 | 0.00 | 667 | 1.68 | 0.90 | 0.89 | 0.04 | 0.06 | 0.15 | 0.039 | 0.048 | No |
| Variable | Estimate | S.E. | p-Value | 95% BC CI | Indirect Effect Present |
|---|---|---|---|---|---|
| Emotional regulation indirectly affects engagement through Optimism | 0.16 | 0.05 | 0.00 | [0.09; 0.27] | Yes |
| Emotional regulation indirectly affects stress through Optimism | −0.06 | 0.04 | 0.09 | [−0.14; 0.01] | No |
| Emotional regulation indirectly affects depression through Optimism | −0.13 | 0.04 | 0.00 | [−0.23; −0.06] | Yes |
| Emotional regulation indirectly affects anxiety through Optimism | −0.08 | 0.04 | 0.02 | [−0.17; −0.03] | Yes |
| Optimism indirectly affects depression through Engagement | −0.12 | 0.04 | 0.00 | [−0.20; −0.05] | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krifa, I.; van Zyl, L.E.; Braham, A.; Ben Nasr, S.; Shankland, R. Mental Health during COVID-19 Pandemic: The Role of Optimism and Emotional Regulation. Int. J. Environ. Res. Public Health 2022, 19, 1413. https://doi.org/10.3390/ijerph19031413
Krifa I, van Zyl LE, Braham A, Ben Nasr S, Shankland R. Mental Health during COVID-19 Pandemic: The Role of Optimism and Emotional Regulation. International Journal of Environmental Research and Public Health. 2022; 19(3):1413. https://doi.org/10.3390/ijerph19031413
Chicago/Turabian StyleKrifa, Imen, Llewellyn Ellardus van Zyl, Amel Braham, Selma Ben Nasr, and Rebecca Shankland. 2022. "Mental Health during COVID-19 Pandemic: The Role of Optimism and Emotional Regulation" International Journal of Environmental Research and Public Health 19, no. 3: 1413. https://doi.org/10.3390/ijerph19031413
APA StyleKrifa, I., van Zyl, L. E., Braham, A., Ben Nasr, S., & Shankland, R. (2022). Mental Health during COVID-19 Pandemic: The Role of Optimism and Emotional Regulation. International Journal of Environmental Research and Public Health, 19(3), 1413. https://doi.org/10.3390/ijerph19031413







