Can Hip-Knee Line Angle Distinguish the Size of Pelvic Incidence?—Development of Quick Noninvasive Assessment Tool for Pelvic Incidence Classification
Abstract
:1. Introduction
2. Materials and Methods (Study 1: Exploring Effective Surrogate Angles for PI Classification Focusing on the Buttocks)
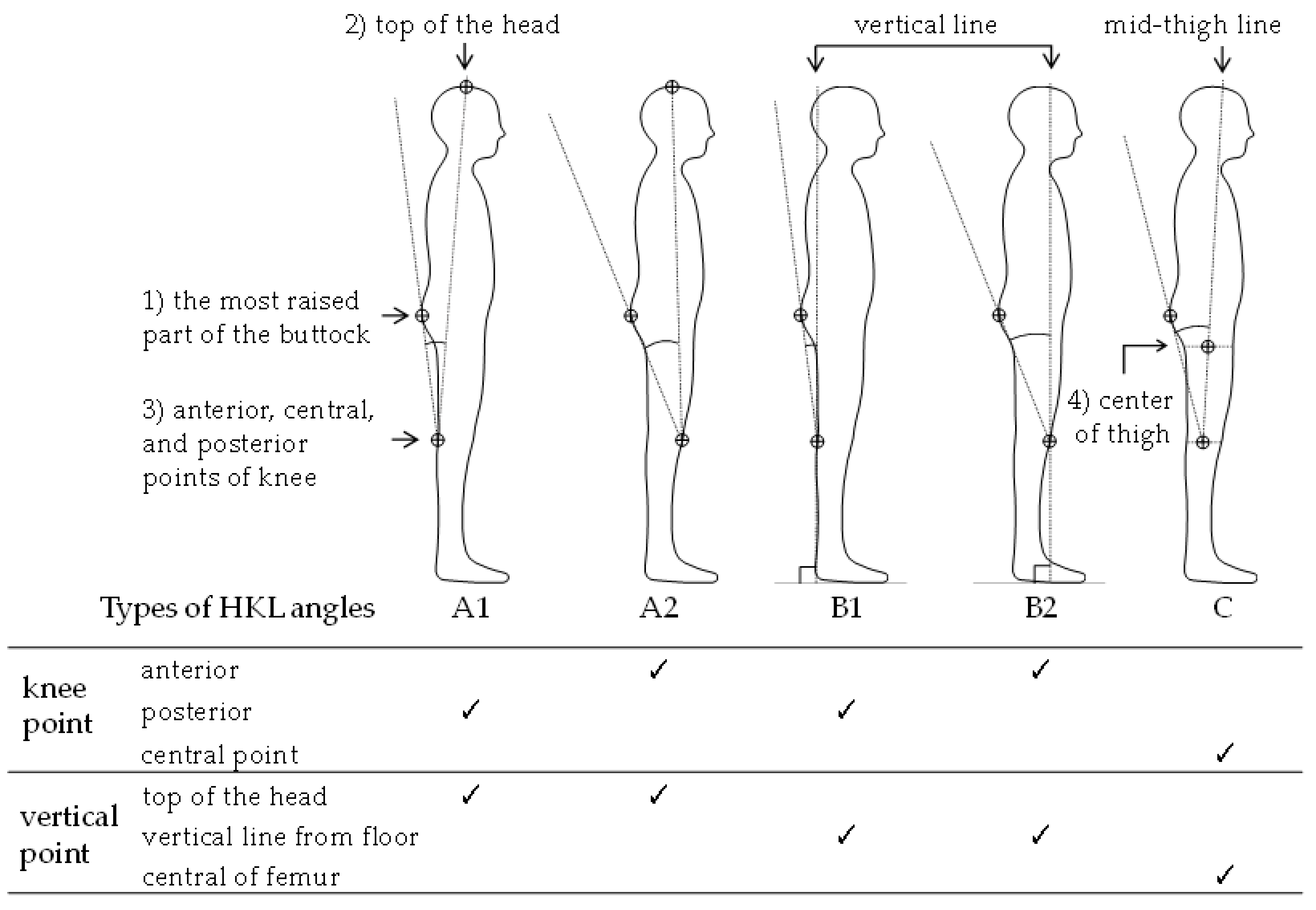
2.1. Measurement Angular Definition
2.2. Procedures
2.3. Measurement of HKL Angles and Outcome Variable
2.4. Data Analysis and Statistical Analyses
2.5. Criteria for Selecting Cut-Off Points Applicable to Practical PI Classification Tools Using Buttock Thickness
3. Results (Study 1)
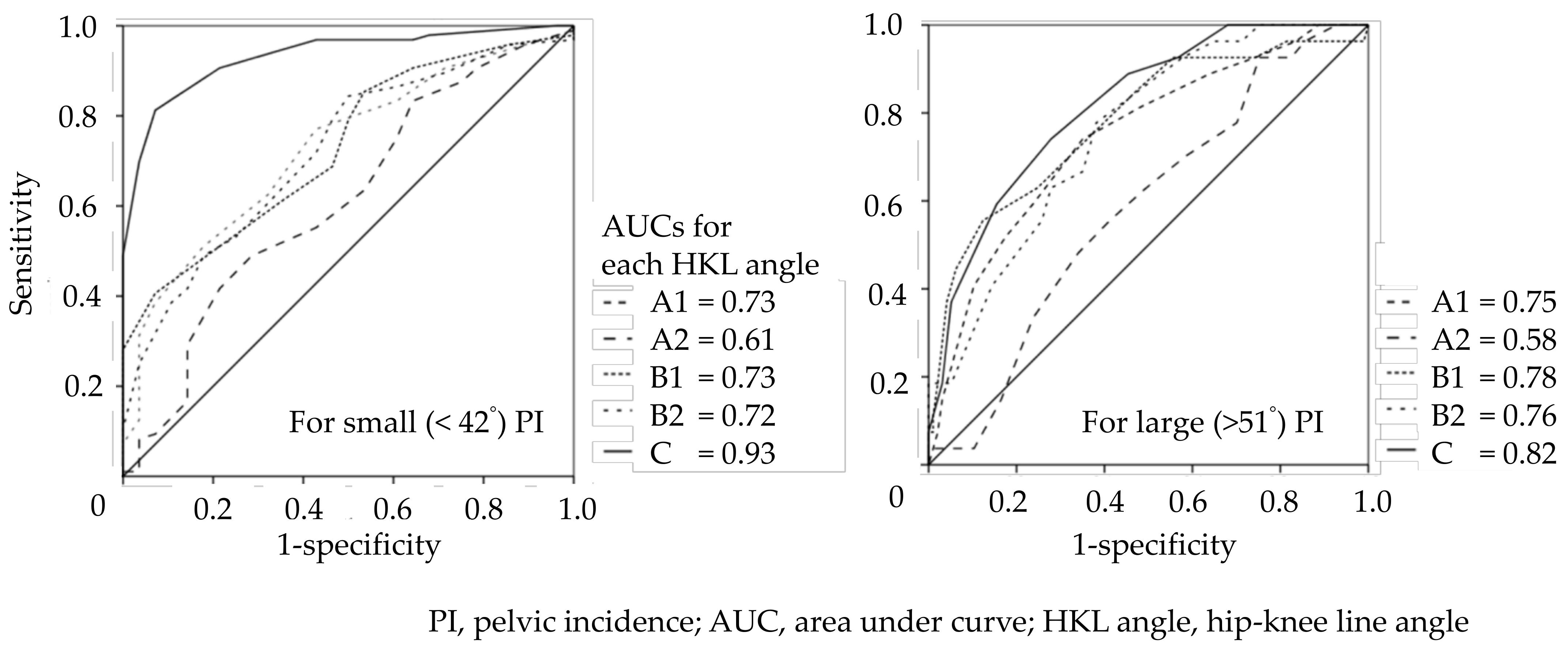
3.1. AUCs of HKL Angles Discriminating Small or Large PIs
3.2. Cut-Off Points Applicable to Practical PI Classification Tool Using the Thickness of the Buttocks
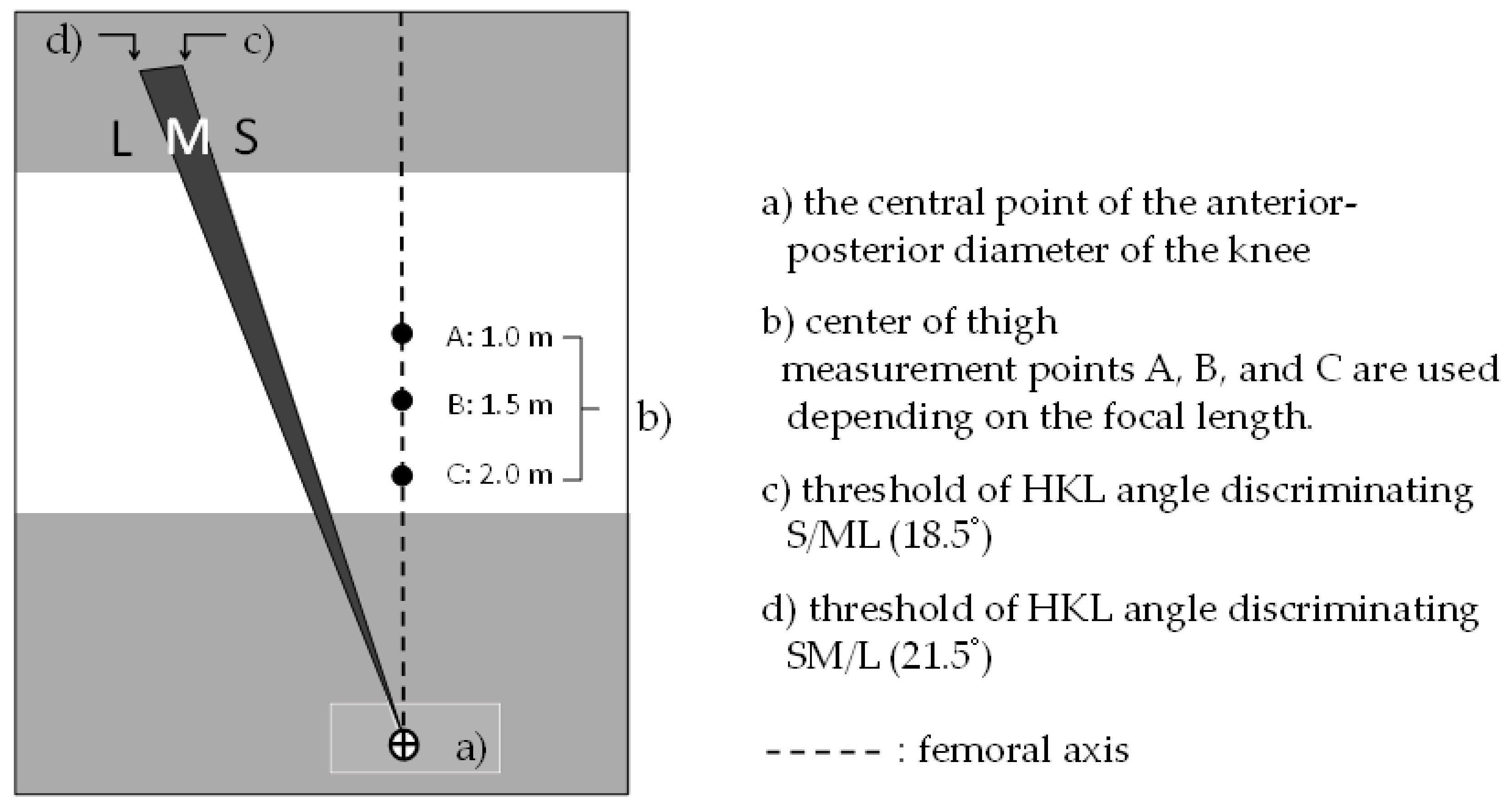
3.3. Devised PI Classification Tool Using the HKL Angle
4. Materials and Methods (Study 2: Assessing Intra-/Inter-Rater Reliability of the PI Classification Tool Using the HKL Angle)
4.1. Participants
4.2. Materials Used for the Assessment
4.3. Procedures
4.4. Data Analysis and Statistical Analysis
5. Results (Study 2)
5.1. Usability Metrics
5.2. Intra-/Inter-Rater Reliability
6. Discussion
6.1. Relationship between the HKL Angle and PI Using the Visual Buttock Silhouette
6.2. Optimal Cut-Off Points Applicable to Practical PI Classification Tool
6.3. Intra-/Inter-Rater Reliability of Tool Using HKL Angle
6.4. Practical Implication and Limitation
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ganesan, S.; Acharya, A.S.; Chauhan, R.; Acharya, S. Prevalence and risk factors for low back pain in 1,355 young adults: A cross-sectional study. Asian Spine J. 2017, 11, 610–617. [Google Scholar] [CrossRef]
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Manchikanti, L.; Singh, V.; Falco, F.J.; Benyamin, R.M.; Hirsch, J.A. Epidemiology of low back pain in adults. Neuromodulation 2014, 17 (Suppl. S2), 3–10. [Google Scholar] [CrossRef]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M. Prevalence of chronic low back pain: Systematic review. Rev. Saude Publica 2015, 49, 73. [Google Scholar] [CrossRef]
- Diseases, G.B.D.; Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Itoh, H.; Kitamura, F.; Yokoyama, K. Estimates of annual medical costs of work-related low back pain in Japan. Ind. Health 2013, 51, 524–529. [Google Scholar] [CrossRef] [Green Version]
- Punnett, L.; Pruss-Utun, A.; Nelson, D.I.; Fingerhut, M.A.; Leigh, J.; Tak, S.; Phillips, S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am. J. Ind. Med. 2005, 48, 459–469. [Google Scholar] [CrossRef] [PubMed]
- Steffens, D.; Maher, C.G.; Pereira, L.S.; Stevens, M.L.; Oliveira, V.C.; Chapple, M.; Teixeira-Salmela, L.F.; Hancock, M.J. Prevention of low back pain: A systematic review and meta-analysis. JAMA Intern. Med. 2016, 176, 199–208. [Google Scholar] [CrossRef]
- Verbeek, J.H.; Martimo, K.P.; Karppinen, J.; Kuijer, P.P.; Viikari-Juntura, E.; Takala, E.P. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst Rev. 2011, 6. [Google Scholar] [CrossRef]
- Legaye, J.; Duval-Beaupere, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.P.; Lafage, V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef]
- Schwab, F.J.; Blondel, B.; Bess, S.; Hostin, R.; Shaffrey, C.I.; Smith, J.S.; Boachie-Adjei, O.; Burton, D.C.; Akbarnia, B.A.; Mundis, G.M.; et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: A prospective multicenter analysis. Spine 2013, 38, e803–e812. [Google Scholar] [CrossRef] [Green Version]
- Chen, R.Q.; Hosogane, N.; Watanabe, K.; Funao, H.; Okada, E.; Fujita, N.; Hikata, T.; Iwanami, A.; Tsuji, T.; Ishii, K.; et al. Reliability analysis of spino-pelvic parameters in adult spinal deformity: A comparison of whole spine and pelvic radiographs. Spine 2016, 41, 320–327. [Google Scholar] [CrossRef] [Green Version]
- Tyrakowski, M.; Yu, H.; Siemionow, K. Pelvic incidence and pelvic tilt measurements using femoral heads or acetabular domes to identify centers of the hips: Comparison of two methods. Eur. Spine J. 2015, 24, 1259–1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowe, T.; Berven, S.H.; Schwab, F.J.; Bridwell, K.H. The SRS classification for adult spinal deformity: Building on the King/Moe and Lenke classification systems. Spine 2006, 31, s119–s125. [Google Scholar] [CrossRef]
- Bao, H.; Liabaud, B.; Varghese, J.; Lafage, R.; Diebo, B.G.; Jalai, C.; Ramchandran, S.; Poorman, G.; Errico, T.; Zhu, F.; et al. Lumbosacral stress and age may contribute to increased pelvic incidence: An analysis of 1625 adults. Eur. Spine J. 2018, 27, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Place, H.M.; Hayes, A.M.; Huebner, S.B.; Hayden, A.M.; Israel, H.; Brechbuhler, J.L. Pelvic incidence: A fixed value or can you change it? Spine J. 2017, 17, 1565–1569. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.M.; Roussouly, P.; Berthonnaud, E.; Guigui, P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur. Spine J. 2011, 20 (Suppl. S5), 572–577. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.F.; Zhao, C.Q. Pelvic incidence variation among individuals: Functional influence versus genetic determinism. J. Orthop. Surg. Res. 2018, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Yamada, S.; Ebara, T.; Uehara, T.; Kimura, S.; Aoki, K.; Inada, A.; Kamijima, M. Reliability of anthropometric landmarks on body surface for estimating pelvic incidence without lateral X-ray. Occup Environ Med. 2021, 3. [Google Scholar] [CrossRef]
- Yamada, S.; Ebara, T.; Uehara, T.; Kimura, S.; Satsukawa, Y.; Aoki, K.; Inada, A.; Kamijima, M. Exploring the anthropometric parameters for improving reliability of estimation model of pelvic incidence. In Proceedings of the 46th International Society for the Study of the Lumbar Spine Annual Meeting, Kyoto, Japan, 3–7 June 2019; p. 461. [Google Scholar]
- Ramchandran, S. Pelvic Incidence (PI) is more easily understood as the pelvic base angle (PBA). Spine Res. 2017, 3. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.; Romani, W. Muscles: Testing and Function with Posture and Pain, 5th ed.; Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Guimond, S.; Massrieh, W. Intricate correlation between body posture, personality trait and incidence of body pain: A cross-referential study report. PLoS ONE 2012, 7, e37450. [Google Scholar] [CrossRef]
- Yamada, S.; Ebara, T.; Uehara, T.; Inada, A.; Kamijima, M. Can postural pattern assessment be used to estimate pelvic incidence?: Reliability and validity of simple classification tools for postural pattern assessment. Jpn. J. Ergon. 2021, 57, 288–293. [Google Scholar]
- Day, B.L.; Steiger, M.J.; Thompson, P.D.; Marsden, C.D. Effect of vision and stance width on human body motion when standing: Implications for afferent control of lateral sway. J. Physiol. 1993, 469, 479–499. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Stolinski, L.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. Standardization; Terminology Committee of the International Society of, B. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. Int. Soc. Biomech. J. Biomech 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Savage, J.W.; Patel, A.A. Fixed sagittal plane imbalance. Global. Spine J. 2014, 4, 287–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwab, F.; Lafage, V.; Boyce, R.; Skalli, W.; Farcy, J.P. Gravity line analysis in adult volunteers: Age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine 2006, 31, e959–e967. [Google Scholar] [CrossRef]
- Segi, N.; Nakashima, H.; Ando, K.; Kobayashi, K.; Seki, T.; Ishizuka, S.; Takegami, Y.; Machino, M.; Ito, S.; Koshimizu, H.; et al. Spinopelvic imbalance is associated with increased sway in the center of gravity: Validation of the “cone of economy” concept in healthy subjects. Global. Spine J. 2021, 21925682211038897. [Google Scholar] [CrossRef] [PubMed]
- Kanemura, T. Sagittal spino-pelvic alignment in an asymptomatic japanese population. J. Spine Res. 2011, 2, 52–58. [Google Scholar]
- Endo, K.; Suzuki, H.; Nishimura, H.; Tanaka, H.; Shishido, T.; Yamamoto, K. Characteristics of sagittal spino-pelvic alignment in Japanese young adults. Asian Spine J. 2014, 8, 599–604. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.S.; Chung, S.S.; Kang, K.C.; Park, S.J.; Shin, S.K. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine 2011, 36, e1648–e1654. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Joint. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef]
- Jānis Šavlovskis, K.R. The Bony Pelvis & Gender Differences in Pelvic Anatomy. Available online: https://www.anatomystandard.com/Pelvis/Pelvis.html (accessed on 18 January 2022).
- Rosa, F.; Piero, Q. Fleiss’ kappa stastic wuthout paradoxes. Qual. Quant. 2014, 49, 463–470. [Google Scholar]
- Handa, V.L.; Lockhart, M.E.; Fielding, J.R.; Bradley, C.S.; Brubaker, L.; Cundiff, G.W.; Ye, W.; Richter, H.E. Pelvic Floor Disorders, Network, Racial differences in pelvic anatomy by magnetic resonance imaging. Obstet. Gynecol. 2008, 111, 914–920. [Google Scholar] [CrossRef] [Green Version]
- Branco, P.; Torgo, L.; Ribeiro, R. A survey of predictive modelling under imbalanced distributions. ACM Comput. Surv. 2017, 49, 1–50. [Google Scholar] [CrossRef]

| HKL Angle C | Cut-Off | Total (n = 125) | Male (n = 71) | Female (n = 54) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| sen. | spec. | Y. I | sen. | spec. | Y. I | sen. | spec. | Y. I | ||
| S/ML | 13.0 | 1.00 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | – | – | – |
| 14.5 | 1.00 | 0.04 | 0.04 | 1.00 | 0.05 | 0.05 | 1.00 | 0.00 | 0.00 | |
| 15.5 | 0.98 | 0.32 | 0.30 | 1.00 | 0.38 | 0.38 | 0.96 | 0.10 | 0.10 | |
| 16.5 | 0.97 | 0.36 | 0.33 | 1.00 | 0.57 | 0.43 | – | – | – | |
| 17.5 | 0.97 | 0.57 | 0.54 | 1.00 | 0.71 | 0.71 | 0.94 | 0.08 | 0.08 | |
| 18.5 | 0.91 | 0.79 | 0.69 | 0.98 | 0.81 | 0.79 | 0.83 | 0.71 | 0.54 | |
| 19.5 | 0.81 | 0.93 | 0.74 | 0.90 | 0.95 | 0.85 | 0.72 | 0.86 | 0.58 | |
| 20.5 | 0.70 | 0.96 | 0.66 | 0.76 | 0.95 | 0.71 | 0.63 | 1.00 | 0.63 | |
| 21.5 | 0.50 | 1.00 | 0.49 | 0.54 | 1.00 | 0.54 | 0.44 | 1.00 | 0.44 | |
| 22.5 | 0.32 | 1.00 | 0.32 | 0.32 | 1.00 | 0.32 | 0.33 | 1.00 | 0.33 | |
| 23.5 | 0.16 | 1.00 | 0.16 | 0.14 | 1.00 | 0.14 | 0.17 | 1.00 | 0.17 | |
| 24.5 | 0.09 | 1.00 | 0.08 | 0.08 | 1.00 | 0.08 | 0.09 | 1.00 | 0.09 | |
| 25.5 | 0.02 | 1.00 | 0.02 | 0.02 | 1.00 | 0.02 | 0.02 | 1.00 | 0.02 | |
| 26.5 | 0.01 | 1.00 | 0.01 | 0.00 | 1.00 | 0.00 | – | – | – | |
| 28.0 | 0.00 | 1.00 | 0.00 | – | – | – | 0.00 | 1.00 | 0.00 | |
| HKL | Cut-off | Total (n = 125) | Male (n = 71) | Female (n = 54) | ||||||
| angle C | sen. | spec. | Y. I | sen. | spec. | Y. I | sen. | spec. | Y. I | |
| SM/L | 13.0 | 1.00 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | – | – | – |
| 14.5 | 1.00 | 0.01 | 0.01 | 1.00 | 0.02 | 0.02 | 1.00 | 0.00 | 0.00 | |
| 15.5 | 1.00 | 0.11 | 0.11 | 1.00 | 0.13 | 0.13 | 1.00 | 0.08 | 0.08 | |
| 16.5 | 1.00 | 0.13 | 0.13 | 1.00 | 0.15 | 0.15 | – | – | – | |
| 17.5 | 1.00 | 0.20 | 0.20 | 1.00 | 0.25 | 0.25 | 1.00 | 0.11 | 0.11 | |
| 18.5 | 1.00 | 0.32 | 0.32 | 1.00 | 0.30 | 0.30 | 1.00 | 0.36 | 0.36 | |
| 19.5 | 0.93 | 0.43 | 0.36 | 1.00 | 0.41 | 0.41 | 0.88 | 0.47 | 0.36 | |
| 20.5 | 0.89 | 0.55 | 0.44 | 1.00 | 0.53 | 0.53 | 0.82 | 0.58 | 0.41 | |
| 21.5 | 0.74 | 0.72 | 0.46 | 0.90 | 0.70 | 0.61 | 0.65 | 0.75 | 0.40 | |
| 22.5 | 0.59 | 0.84 | 0.44 | 0.80 | 0.87 | 0.67 | 0.47 | 0.81 | 0.28 | |
| 23.5 | 0.37 | 0.95 | 0.32 | 0.50 | 0.97 | 0.47 | 0.29 | 0.92 | 0.21 | |
| 24.5 | 0.19 | 0.97 | 0.15 | 0.30 | 0.98 | 0.28 | 0.12 | 0.94 | 0.06 | |
| 25.5 | 0.07 | 1.00 | 0.07 | 0.10 | 1.00 | 0.10 | 0.06 | 1.00 | 0.06 | |
| 26.5 | 0.04 | 1.00 | 0.04 | 0.00 | 1.00 | 0.00 | – | – | – | |
| 28.0 | 0.00 | 1.00 | 0.00 | – | – | – | 0.00 | 1.00 | 0.00 | |
| Sub. No. | Mean Time (s/photo) | Correct Rate (%) | Intrarater Reliability Cohen Kappa (95% CI) | Inter-Rater Fleiss’s Kappa (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 1st | 2nd | Total (n = 24) | Male (n = 14) | Female (n = 10) | 1st | 2nd | |
| 1 | 20.0 | 13.8 | 88 | 83 | 0.87 (0.72–1.00) | 0.93 (0.77–1.00) | 0.68 (0.34–1.00) | total 0.50 (0.47–0.53) male 0.43 (0.39–0.47) female 0.56 (0.46–0.68) | total 0.54 (0.51–0.57) male 0.50 (0.27–0.57) female 0.57 (0.51–0.73) |
| 2 | 17.5 | 13.8 | 79 | 88 | 0.80 (0.61–0.99) | 0.83 (0.58–1.00) | 0.69 (0.38–1.00) | ||
| 3 | 13.1 | 12.9 | 83 | 71 | 0.82 (0.67–0.97) | 0.74 (0.52–0.96) | 1.00 (1.00–1.00) | ||
| 4 | 14.6 | 12.0 | 79 | 83 | 0.87 (0.71–1.00) | 0.78 (0.68–0.89) | 0.78 (0.39–1.00) | ||
| 5 | 19.6 | 17.1 | 67 | 83 | 0.75 (0.56–0.94) | 0.75 (0.50–0.99) | 0.69 (0.38–1.00) | ||
| 6 | 16.0 | 14.0 | 83 | 83 | 0.78 (0.60–0.97) | 0.71 (0.48–0.95) | 0.85 (0.63–1.00) | ||
| 7 | 13.2 | 12.6 | 83 | 71 | 0.67 (0.45–0.90) | 0.58 (0.27–0.88) | 0.80 (0.44–1.00) | ||
| 8 | 11.3 | 10.6 | 79 | 88 | 0.75 (0.57–0.94) | 0.71 (0.42–0.99) | 0.79 (0.52–1.00) | ||
| 9 | 12.5 | 11.3 | 75 | 75 | 0.83 (0.67–1.00) | 0.70 (0.41–0.99) | 1.00 (1.00–1.00) | ||
| 10 | 15.0 | 13.1 | 67 | 79 | 0.67 (0.45–0.88) | 0.69 (0.43–0.95) | 0.59 (0.29–0.90) | ||
| 11 | 24.6 | 18.3 | 71 | 67 | 0.82 (0.64–0.99) | 0.91 (0.75–1.00) | 0.63 (0.38–0.88) | ||
| 12 | 21.7 | 10.3 | 67 | 88 | 0.81 (0.66–0.97) | 0.89 (0.74–1.00) | 0.63 (0.38–0.88) | ||
| 13 | 26.3 | 19.8 | 83 | 83 | 0.77 (0.58–0.95) | 0.83 (0.61–1.00) | 0.65 (0.43–0.87) | ||
| 14 | 12.8 | 10.4 | 75 | 75 | 0.82 (0.65–0.99) | 0.83 (0.62–1.00) | 0.76 (0.42–1.00) | ||
| mean (sd) | 17.0 (4.7) | 13.6 (2.9) | 77.1 (6.9) | 79.8 (6.9) | 0.79 (0.61–0.96) | 0.78 (0.59–0.97) | 0.75 (0.50–0.97) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, S.; Ebara, T.; Uehara, T.; Matsuki, T.; Kimura, S.; Satsukawa, Y.; Yoshihara, A.; Aoki, K.; Inada, A.; Kamijima, M. Can Hip-Knee Line Angle Distinguish the Size of Pelvic Incidence?—Development of Quick Noninvasive Assessment Tool for Pelvic Incidence Classification. Int. J. Environ. Res. Public Health 2022, 19, 1387. https://doi.org/10.3390/ijerph19031387
Yamada S, Ebara T, Uehara T, Matsuki T, Kimura S, Satsukawa Y, Yoshihara A, Aoki K, Inada A, Kamijima M. Can Hip-Knee Line Angle Distinguish the Size of Pelvic Incidence?—Development of Quick Noninvasive Assessment Tool for Pelvic Incidence Classification. International Journal of Environmental Research and Public Health. 2022; 19(3):1387. https://doi.org/10.3390/ijerph19031387
Chicago/Turabian StyleYamada, Shota, Takeshi Ebara, Toru Uehara, Taro Matsuki, Shingo Kimura, Yuya Satsukawa, Akira Yoshihara, Kazuji Aoki, Atsushi Inada, and Michihiro Kamijima. 2022. "Can Hip-Knee Line Angle Distinguish the Size of Pelvic Incidence?—Development of Quick Noninvasive Assessment Tool for Pelvic Incidence Classification" International Journal of Environmental Research and Public Health 19, no. 3: 1387. https://doi.org/10.3390/ijerph19031387
APA StyleYamada, S., Ebara, T., Uehara, T., Matsuki, T., Kimura, S., Satsukawa, Y., Yoshihara, A., Aoki, K., Inada, A., & Kamijima, M. (2022). Can Hip-Knee Line Angle Distinguish the Size of Pelvic Incidence?—Development of Quick Noninvasive Assessment Tool for Pelvic Incidence Classification. International Journal of Environmental Research and Public Health, 19(3), 1387. https://doi.org/10.3390/ijerph19031387






