Effect of Knee Orthosis Pressure Variation on Muscle Activities during Sit-to-Stand Motion in Patients with Knee Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentation/Materials for Data Collection
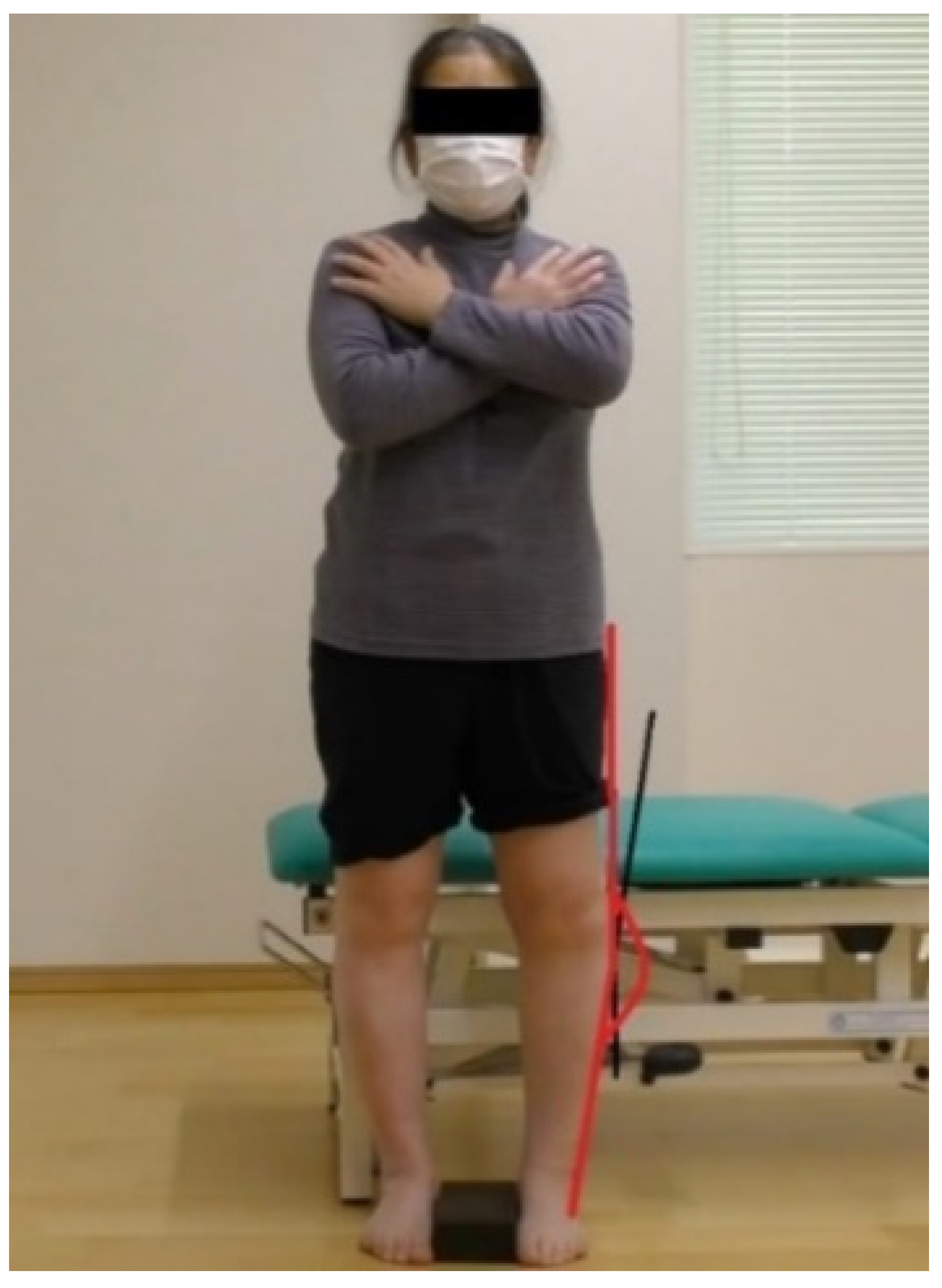
2.3. Procedure
2.4. Assessment of Tibio-Femoral Alignment
2.5. Severity of Osteoarthritis and Quality-of-Life Assessment
2.6. Sit-to-Stand Motion Assessment
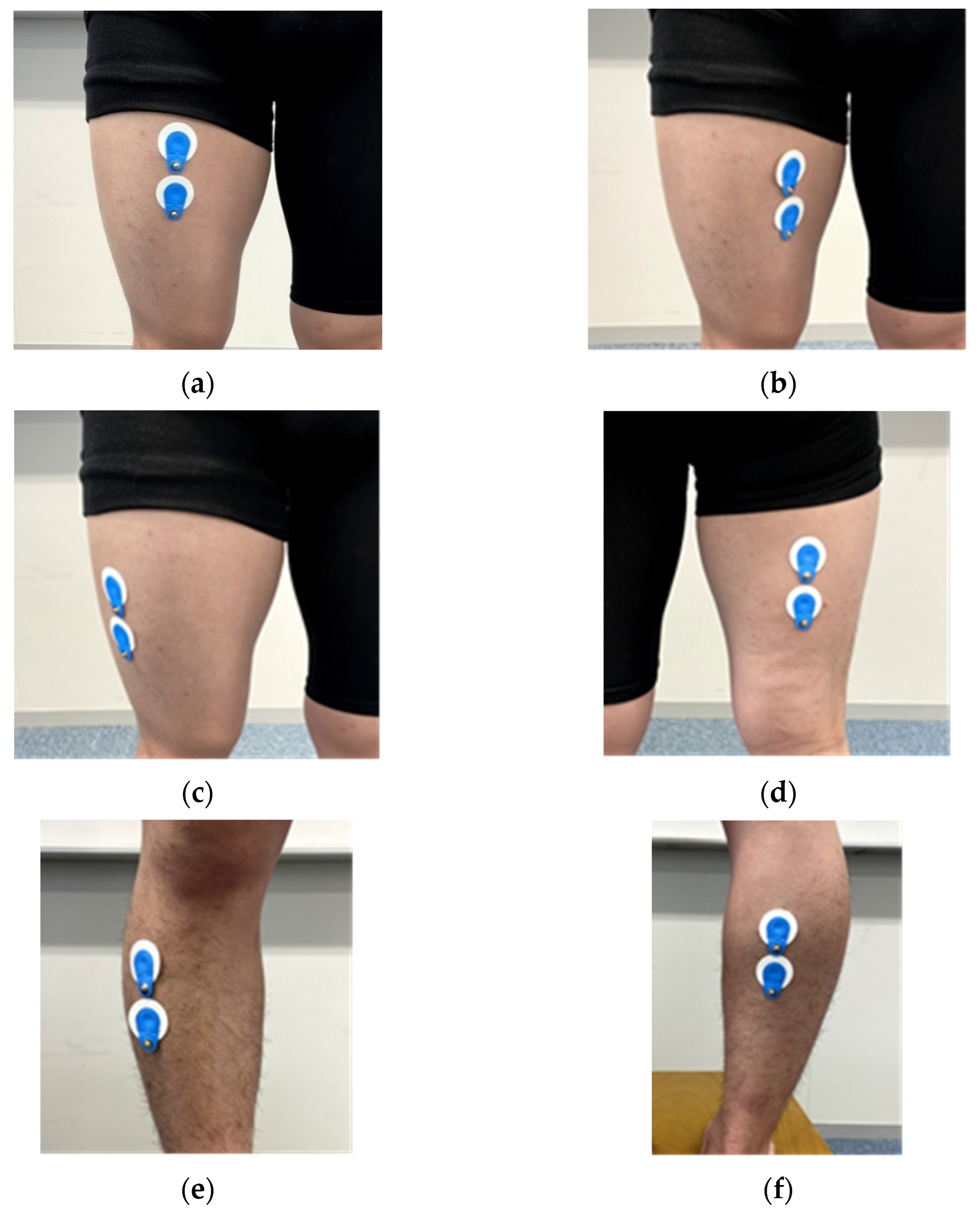
2.7. Measurement of Muscular Activities
2.8. Data Analysis
3. Results
3.1. Sociodemographic Characteristics of the Patients
3.2. The Degree of the Severity of Knee OA
3.3. The Variation in the Knee Orthotics Pressure and Muscle Activities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministry of Health, Labor and Welfare. Overview of the 2016 National Life Basic Survey. Available online: http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa16/index.html (accessed on 9 June 2021).
- Yoshimura, N.; Muraki, S.; Oka, H.; Mabuchi, A.; En-Yo, Y.; Yoshida, M.; Saika, A.; Yoshida, H.; Suzuki, T.; Yamamoto, S.; et al. Prevalence of knee osteoarthritis, lumbar spondylosis and osteoporosis in Japanese men and women. The research on osteoarthritis/osteoporosis against Disability (ROAD). J. Bone Miner. Metab. 2009, 27, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Anan, M.; Tokuda, K.; Kito, N.; Shinkoda, K. Kinematic analysis of chair-standing movement in knee osteoarthritis. Phys. Ther. Sci. 2010, 25, 755–760. [Google Scholar]
- Fujii, T.; Toda, H.; Ishikawa, H.; Kito, N.; Sasaki, H. Age-related changes in muscle function that affect the production of internal hip extension moments during standing up. Physiother. Sci. 2013, 28, 463–468. [Google Scholar]
- Huda, A.; David, O.; Mahmoud, A.; Lu, Z.; Imre, B.; Szimonetta, L.; Bálint, M. Efect of using knee valgus brace on pain and activity level over different time intervals among patients with medial knee OA: Systematic review. BMC Musculoskelet. Disord. 2021, 22, 687–696. [Google Scholar]
- Rannou, F.; Poiraudeau, S.; Beaudreuil, J. Role of bracing in the management of knee osteoarthritis. Curr. Opin. Rheumatol. 2010, 22, 218–222. [Google Scholar] [CrossRef]
- Chuang, S.H.; Huang, M.H.; Chen, T.W.; Weng, M.C.; Liu, C.W.; Chen, C.H. Effect of knee sleeve on static and dynamic balance in patients with knee osteoarthritis. Kaohsiung J. Med. Sci. 2007, 23, 405–411. [Google Scholar] [CrossRef]
- Aoki, O.; Kagawa, S. Effect of orthosis therapy on knee joint position sense in patients with severe knee osteoarthritis. Physiother. Sci. 2005, 20, 43–48. [Google Scholar]
- Jeong, H.S.; Lee, S.C.; Jee, H.; Song, J.B.; Chang, H.S.; Lee, S.Y. Proprioceptive Training and Outcomes of Patients with Knee Osteoarthritis: A Meta-Analysis of Randomized Controlled Trials. J. Athl. Train. 2019, 54, 418–428. [Google Scholar] [CrossRef]
- Sharif, N.A.; Usman, J.; Safwani, W.K.; Li, G.S.; Karim, S.A.; Mohamed, N.A.; Khan, S.S.; Khan, S.J. Effects of simple knee sleeves on pain and knee adduction moment in early unilateral knee osteoarthritis. J. Eng. Med. 2019, 233, 1132–1140. [Google Scholar] [CrossRef]
- Deie, M.; Toriyama, M.; Shimada, N.; Shidabara, K.; Ochi, M. Recent findings of knee orthosis therapy for knee osteoarthritis. Jt. Surg. 2010, 29, 1033–1038. [Google Scholar]
- Kellgren, J.H.; Laurence, J.S. Radiological assessment of osteoarthritis. Am. Rheum. Dis. 1957, 16, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, H.; Hashimoto, N.; Fukumoto, T.; Maeda, S.; Chuman, T.; Hirai, Y.; Sakamoto, K. Relationship between Mikulicz line and FTA: Factors of OA. Orthop. Disaster Surg. 2006, 66, 262–266. [Google Scholar]
- Sugita, T.; Miyatake, N.; Aizawa, T.; Sasaki, A.; Kamimura, M.; Takahashi, A. Quality of life after staged bilateral total knee arthroplasty: A minimum five-year follow-up study of seventy-eight patients. Int. Orthop. 2019, 43, 2309–2314. [Google Scholar] [CrossRef] [PubMed]
- Akai, M.; Doi, T.; Fujino, K.; Iwaya, T.; Kurosawa, H.; Nasu, T. An outcome measure for Japanese people with knee osteoarthritis. J. Rheumatol. 2005, 32, 1524–1532. [Google Scholar]
- Suzuki, Y.; Fukushima, M.; Sakuraba, K.; Sawaki, K.; Sekigawa, K. Krill Oil Improves Mild Knee Joint Pain: A Randomized Control Trial. PLoS ONE 2016, 11, e0162769. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, T.; Hida, M.; Nagasaki, T.; Wada, C. Novel method for evaluation of frontal plane knee alignment using bony prominences in patients with osteoarthritis. J. Phys. Ther. Sci. 2018, 30, 1168–1172. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hirai, M. Clinical application of compression stockings: Especially about elasticity/elongation hardness and Laplace’s law. Veinology 2007, 18, 239–245. [Google Scholar]
- Hoshi, F.; Yamanaka, M.; Takahashi, M.; Takahashi, M.; Fukuda, O.; Wada, T. Motion analysis of standing up from a chair. Phys. Ther. 1992, 19, 43–48. [Google Scholar]
- Sato, S.; Soma, T. Relationship between the speed of the center of gravity and the amount of lower limb muscle activity in the standing posture during standing up. Clin. Physiother. Res. 2013, 30, 1–4. [Google Scholar]
- Genda, E. Mechanical properties required for knee orthosis. J. Jpn. Prosthet. Orthot. 2008, 24, 12–14. [Google Scholar]
- Roebroeck, M.E.; Doorenbosch, C.A.; Harlaar, J.; Jacobs, R.; Lankhors, G.J. Biomechanics and muscular activity during sit-to-stand transfer. Clin. Biomech. 1994, 9, 235–244. [Google Scholar] [CrossRef]
- Tully, E.A.; Fotoohabadi, M.R.; Galea, M.P. Sagittal spine and lower limb movement during sit-to-stand in healthy young subjects. Gait Posture 2005, 22, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Tsuyama, N.; Nakamura, K. Techniques of Manual Examination and Performance Testing, 9th ed.; Kyodo Medical Book Publisher: Tokyo, Japan, 2014; pp. 205–280. [Google Scholar]
- Fujino, H.; Sato, M.; Sano, M.; Sato, Y.; Ishii, N. Effect of Resistance Training under Blood Flow Restriction on Early Rehabilitation after ACL Reconstruction; Society of Physical Education: Tokyo, Japan, 1999. [Google Scholar]
- Sano, S.; Suzuki, M.; Yamaguchi, A. Kinematic analysis of standing up and leaving the knee in patients with knee osteoarthritis. Phys. Ther. Sci. Res. 2015, 6, 41–44. [Google Scholar]
- Nakamura, R.; Saitou, H. Basic Kinematics, 6th ed.; Ishiyaku Publications Inc.: Tokyo, Japan, 1992; pp. 260–288. [Google Scholar]
- Hayata, G.; Oka, H.; Miyagawa, K. Effect of orthosis and taping on knee joint constant velocity exertion torque. Bull. Int. Pac. Univ. 2012, 6, 199–203. [Google Scholar]
- Hodges, P.W.; Hoorn, W.; Wrigley, T.; Hinman, R.; Bowles, K.A.; Cicuttini, F.; Wang, Y.; Bennell, K. Increased duration of co-contraction of medial knee muscles is associated with greater progression of knee osteoarthritis. Man. Ther. 2016, 21, 151–158. [Google Scholar] [CrossRef]


|
| 1. Do you feel stiffness in your knees when you wake up in the morning? 2. Do you feel pain in your knees when you wake up in the morning? 3. How often do you wake up in the night because of pain in your knees? 4. Do you have pain in your knees when you walk on a flat surface? 5. Do you have pain in your knees when ascending stairs? 6. Do you have pain in your knees when desending stairs? 7. Do you have pain in your knees when bending to the floor or standing up? 8. Do you have pain in your knees when standding? |
|
| 9. How diffcult is ascending or descending stairs? 10. How diffcult is bending to the floor or standing up? 11. How diffcult is standing up from sitting on a westem style toilet? 12. How diffcult is wearing pants, skirts, and underwear? 13. How diffcult is putting on socks? 14. How long can you walk on a flat surface without taking a rest? 15. Have you been using a walking stick (cane) recently? 16. How diffcult is shopping for daily necessities? 17. How diffcult is doing light housework (cleaning the dining room after eating, etc)? 18. How diffcult is doing heavy housework (using the vaccum cleaner, etc)? |
|
| 19. Have you gone to an event or to a department store during the last month? 20. Were things that you usualy do (some kind of leason, meeting friends, etc) diffcultbecause of knee pain during the last one month? 21. Did you limit doing things you usualy do because of knee pain during the last month? 22. Did you despair of going outside somewhere close because of knee pain during the last month? 23. Did you despair of going outside somewhere far because of knee pain during the last month? |
|
| 24. Do you think your health during the last month is average? 25. Do you think that knee pain has been negatively affecting your health during the last month? |
| FTA | JKOM | |
|---|---|---|
| ID1 | 189.8 | 14 |
| ID2 | 181.4 | 6 |
| ID3 | 188.8 | 28 |
| ID4 | 182.7 | 27 |
| ID5 | 193.1 | 19 |
| ID6 | 192.4 | 28 |
| ID7 | 187.3 | 48 |
| Mean ± SD | 188.1 ± 4.3 | 24.3 ± 12.3 |
| Control | Low Pressure | Middle Pressure | High Pressure | |
|---|---|---|---|---|
| Rectus femoris | 33.8 ± 18.4 | 22.9 ± 15.4 | 27.8 ± 19.5 | 33.3 ± 20.4 |
| Vastus medialis | 38.0 ± 20.6 | 27.0 ± 11.1 | 28.6 ± 15.0 | 37.5 ± 17.9 |
| Vastus lateralis | 41.9 ± 15.5 | 29.6 ± 13.3 | 35.7 ± 18.8 | 41.5 ± 14.2 |
| Biceps femoris | 34.8 ± 10.6 | 29.7 ± 16.7 | 35.7 ± 28.2 | 36.1 ± 21.7 |
| Tibialis anterior | 25.5 ± 17.9 | 19.3 ± 9.2 | 16.4 ± 8.8 | 23.6 ± 16.7 |
| Gastrocnemius | 47.2 ± 16.8 | 44.1 ± 23.9 | 44.3 ± 23.7 | 49.4 ± 25.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, H.; Okamatsu, S.; Kitagawa, K.; Wada, C. Effect of Knee Orthosis Pressure Variation on Muscle Activities during Sit-to-Stand Motion in Patients with Knee Osteoarthritis. Int. J. Environ. Res. Public Health 2022, 19, 1341. https://doi.org/10.3390/ijerph19031341
Yamamoto H, Okamatsu S, Kitagawa K, Wada C. Effect of Knee Orthosis Pressure Variation on Muscle Activities during Sit-to-Stand Motion in Patients with Knee Osteoarthritis. International Journal of Environmental Research and Public Health. 2022; 19(3):1341. https://doi.org/10.3390/ijerph19031341
Chicago/Turabian StyleYamamoto, Hiroaki, Shogo Okamatsu, Kodai Kitagawa, and Chikamune Wada. 2022. "Effect of Knee Orthosis Pressure Variation on Muscle Activities during Sit-to-Stand Motion in Patients with Knee Osteoarthritis" International Journal of Environmental Research and Public Health 19, no. 3: 1341. https://doi.org/10.3390/ijerph19031341
APA StyleYamamoto, H., Okamatsu, S., Kitagawa, K., & Wada, C. (2022). Effect of Knee Orthosis Pressure Variation on Muscle Activities during Sit-to-Stand Motion in Patients with Knee Osteoarthritis. International Journal of Environmental Research and Public Health, 19(3), 1341. https://doi.org/10.3390/ijerph19031341






