Access and Use of Health Services by People with Diabetes from the Item Response Theory
Abstract
1. Introduction
2. Material and Methods
2.1. Data Source
2.2. Population
2.3. Indicators of Access and Use of Health Services
2.4. Independent Variables
2.5. Statistical Analysis
2.6. Ethical Aspects
3. Results
3.1. Sample Characteristics
3.2. Indicators of Access and Use of Health Services
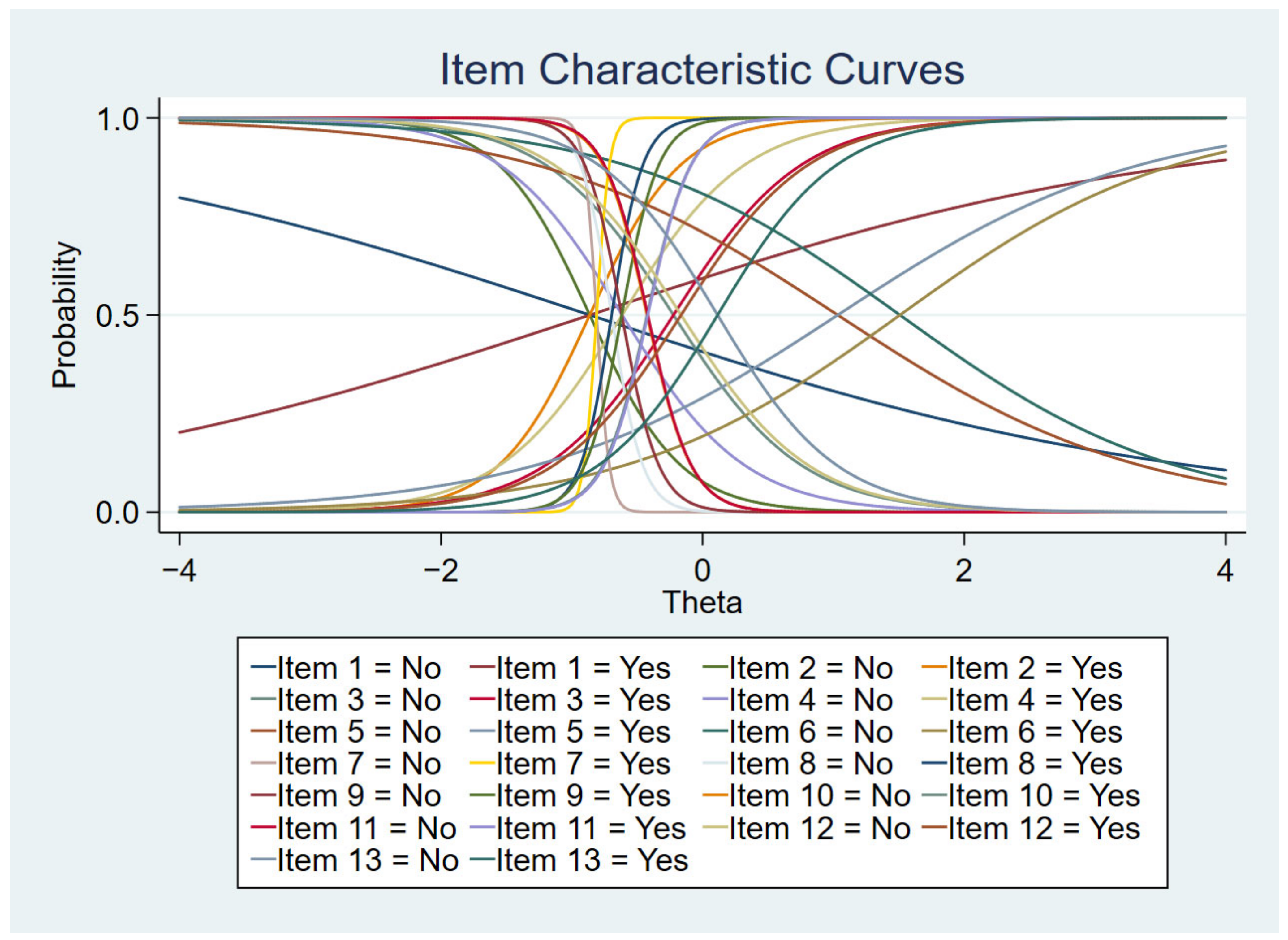
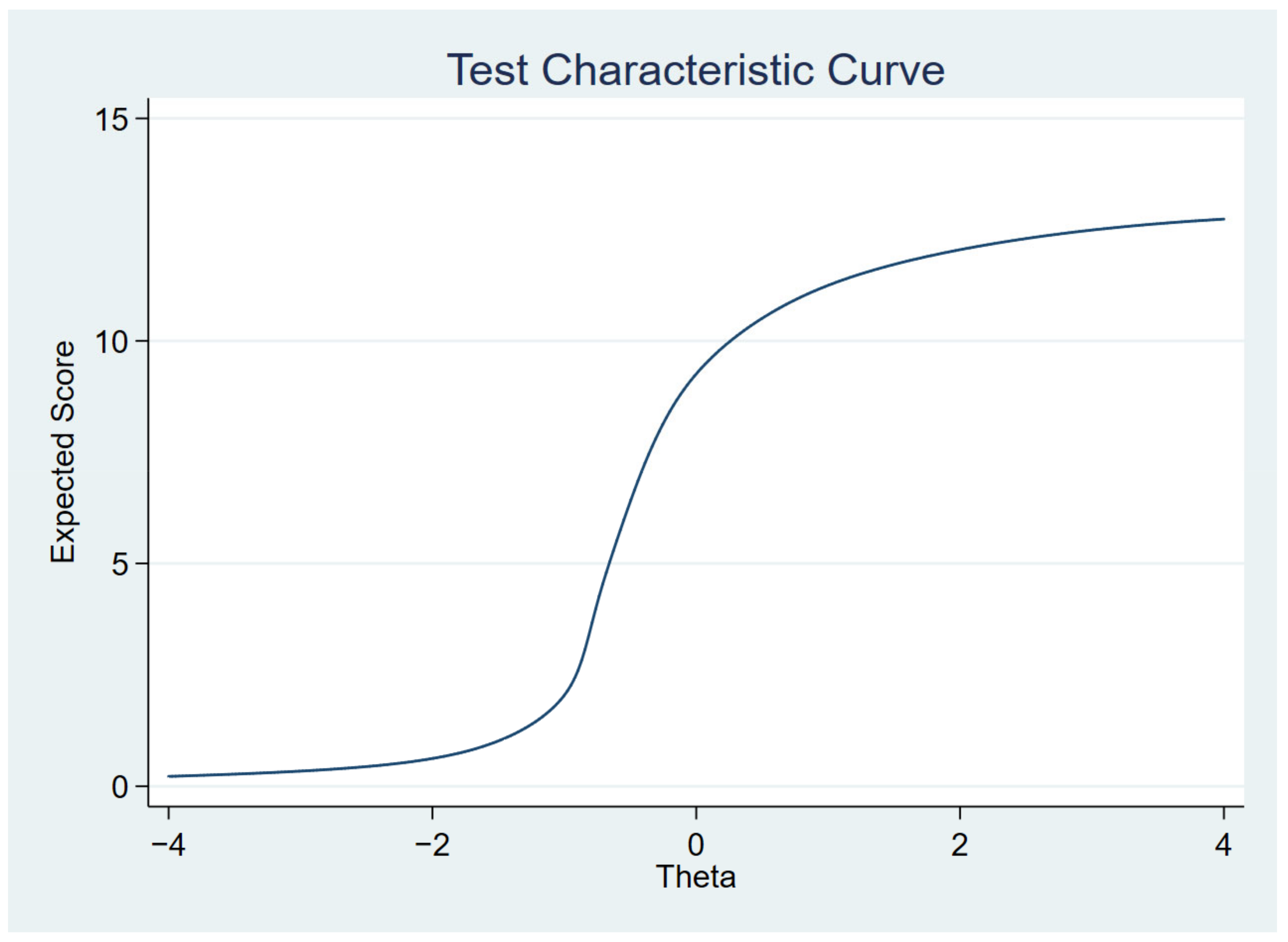
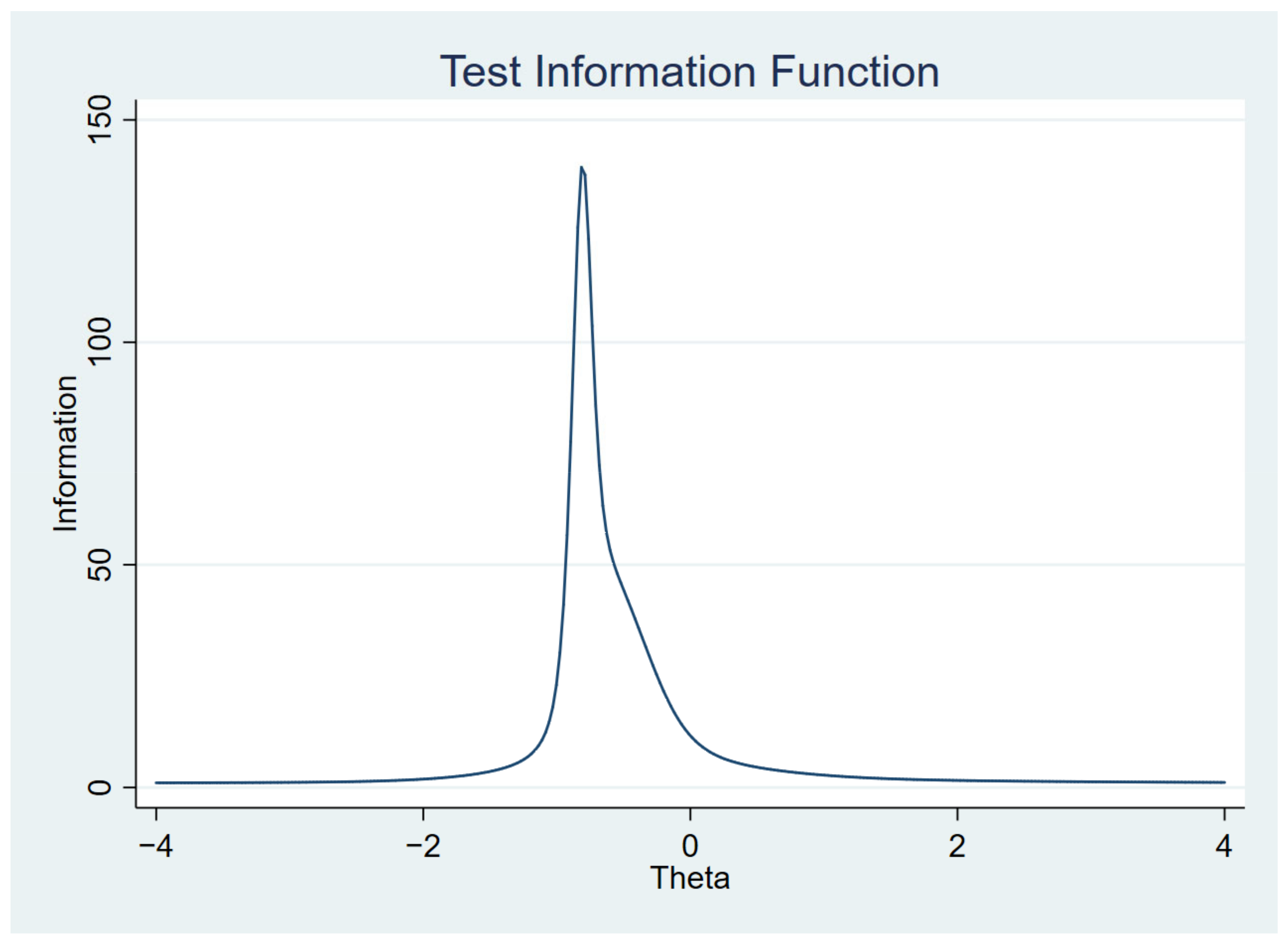
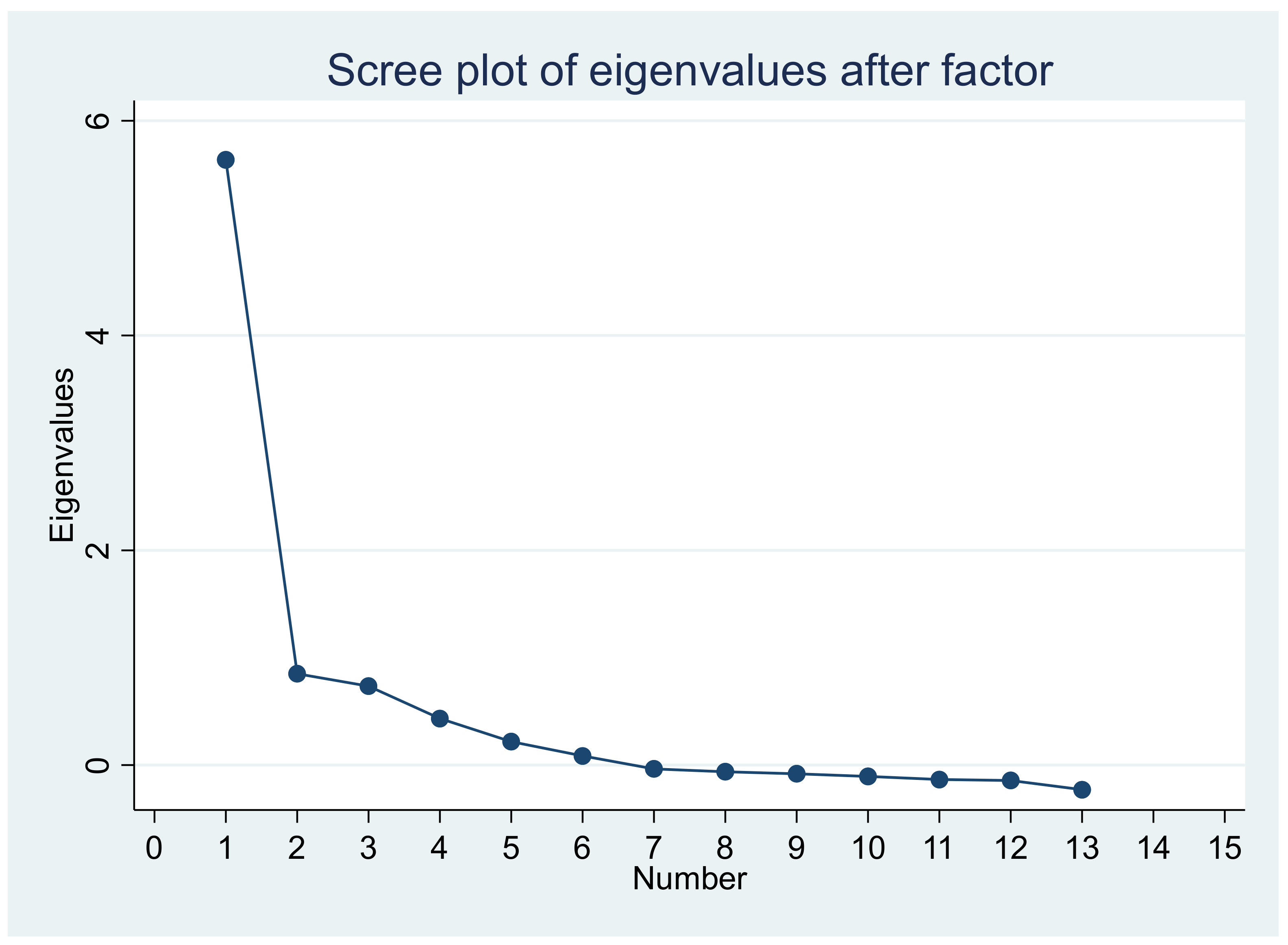
3.3. Access and Use Analysis According to Item Response Theory (IRT)
3.4. Analysis of Access/Use Scores by Sociodemographic Variables
4. Discussion
4.1. Access and Use Indicators
4.2. Scores of Access and Use of Services
4.3. Limitations and Strengths
5. Conclusions
6. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; Fernandes, J.D.R.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas Eighth Edition 2017. Brussels, Belgium: International Diabetes Federation. 2017. Available online: https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf (accessed on 22 July 2022).
- Malta, D.C.; Duncan, B.B.; Schmidt, M.I.; Machado, I.E.; Silva, A.G.; Bernal, R.T.I.; Pereira, C.A.; Damacena, G.N.; Stopa, S.R. Prevalence of diabetes mellitus as determined by glycated hemoglobin in the Brazilian adult population, National Health Survey. Rev. Bras. Epidemiol. 2019, 22, E190006.SUPL.2. [Google Scholar] [CrossRef]
- Ministério da Saúde. Agência Nacional de Saúde Suplementar. Vigitel Brasil 2017 Saúde Suplementar: Vigilância de Fatores de risco e Proteção Para Doenças Crônicas por Inquérito Telefônico. Brasília, Distrito Federal: Ministério da Saúde. Agência Nacional de Saúde Suplementar. 2018; p. 130. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2017_saude_suplementar.pdf (accessed on 22 July 2022).
- Costa, A.F.; Flor, L.S.; Campos, M.R.; Oliveira, A.F.; Costa, M.F.S.; Silva, R.S.; Lobato, L.C.P.; Schramm, J.M. Burden of type 2 diabetes mellitus in Brazil. Cad. Saúde Pública. 2017, 33, e00197915. [Google Scholar] [CrossRef] [PubMed]
- Borges, D.B.; Lacerda, J.T. Actions aimed at the Diabetes Mellitus control in Primary Health Care: A proposal of evaluative model. Saúde Debate 2018, 42, 162–178. [Google Scholar] [CrossRef]
- Artilheiro, M.M.V.S.A.; Franco, S.C.; Schulz, V.C.; Coelho, C.C. Quem são e como são tratados os pacientes que internam por diabetes mellitus no SUS? Saúde Debate 2014, 38, 210–224. [Google Scholar] [CrossRef]
- Ministério da Saúde. Política Nacional de Atenção Básica—PNAB. Brasília: Secretaria de Atenção à Saúde. Departamento de Atenção Básica. 2012, p. 110. Available online: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf (accessed on 22 July 2022).
- Lima, J.G.; Giovanella, L.; Fausto, M.C.R.; Bousquat, A.; Silva, E.V. Atributos essenciais da Atenção Primária à Saúde: Resultados nacionais do PMAQ-AB. Saúde Debate 2018, 42, 52–66. [Google Scholar] [CrossRef]
- Pereira, M.J.B.; Abrahão-Curvo, P.; Fortuna, C.M.; Coutinho, S.S.; Queluz, M.C.; Campos, L.V.O.; Fermino, T.Z.; Santos, C.B. Avaliação das características organizacionais e de desempenho de uma unidade de Atenção Básica à Saúde. Rev. Gaúcha Enferm. 2011, 32, 48–55. [Google Scholar] [CrossRef][Green Version]
- Travassos, C.; Martins, M. Uma revisão sobre os conceitos de acesso e utilização de serviços de saúde. Cad. Saúde Pública. 2004, 20, S190–S198. [Google Scholar] [CrossRef]
- Araújo, M.E.A.; Silva, M.T.; Andrade, K.R.C.; Galvão, T.F.; Pereira, M.G. Prevalence of health services utilization in Brazil: A systematic review and meta-analysis. Epidemiol. Serv. Saúde 2017, 26, 589–604. [Google Scholar] [CrossRef]
- Malta, D.C.; Iser, B.P.M.; Chueiri, P.S.; Stopa, S.R.; Szwarcwald, C.L.; Schmidt, M.I.; Duncan, B.B. Health care among adults with self-reported diabetes mellitus in Brazil, National Health Survey, 2013. Rev. Bras. Epidemiol. 2015, 18, 17–32. [Google Scholar] [CrossRef]
- Viacava, F.; Porto, S.M.; Carvalho, C.C.; Bellido, J.G. Health inequalities by region and social group based on data from household surveys (Brazil, 1998–2013). Ciência Saúde Coletiva. 2019, 24, 2745–2760. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.L.; Andrade, C.J.N.; Santos MSd Silva Neto MFd Porto, T.D. Percepção de usuários com diabetes acerca da assistência recebida na Atenção Primária à Saúde. Rev. APS 2018, 21, 251–258. [Google Scholar] [CrossRef]
- Ministério da Saúde. Portaria nº 2.979, de 12 de Novembro de 2019. Institui o Programa Previne Brasil, Que Estabelece Novo Modelo de Financiamento de Custeio da Atenção Primária à Saúde no Âmbito do Sistema Único de Saúde, Por Meio da alteração da Portaria de Consolidação nº 6/GM/MS, de 28 de Setembro de 2017. Ministério da Saúde. Gabinete do Ministro. 2019. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2019/prt2979_13_11_2019.html (accessed on 22 July 2022).
- Szwarcwald, C.L.; Malta, D.C.; Pereira, C.A.; Vieira, M.L.F.P.; Conde, W.L.; Souza Júnior, P.R.B.S.; Damacena, G.N.; Azevedo, L.O.; Silva, G.A.; Theme Filha, M.M.; et al. National Health Survey in Brazil: Design and methodology of application. Ciência Saúde Coletiva 2014, 19, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Damacena, G.N.; Szwarcwald, C.L.; Malta, D.C.; Souza Júnior, P.R.B.; Vieira, M.L.F.P.; Pereira, C.A.; Morais Neto, O.L.; Silva Júnior, J.B. The Development of the National Health Survey in Brazil, 2013. Epidemiol. Serv. Saúde 2015, 24, 197–206. [Google Scholar] [CrossRef]
- Souza Júnior, P.R.B.; Freitas, M.P.S.; Antonaci, G.A.; Szwarcwald, C.L. Sampling Design for the National Health Survey, Brazil 2013. Epidemiol. Serv. Saúde 2015, 24, 207–216. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde-2013: Questionário dos moradores do domicílio. Rio de Janeiro: Ministério do Planejamento, Orçamento e Gestão. Diretoria de Pesquisas. Instituto Brasileiro de Geografia e Estatística—IBGE. Coordenação de Trabalho e Rendimento. 2013. Available online: https://www.pns.icict.fiocruz.br/questionarios/ (accessed on 22 July 2022).
- Instituto Brasileiro de Geografia e Estatística. Características étnico-raciais da população. Classificações e Identidades. Ministério do Planejamento, Orçamento e Gestão. 2013. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv63405.pdf (accessed on 22 July 2022).
- Kean, J.; Brodke, D.S.; Biber, J.; Gross, P. An introduction to Item Response Theory and Rasch Analysis of the Eating Assessment Tool (EAT-10). Brain Impair. 2018, 19, 91–102. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis Fot the Behavioral Sciences; Earlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Ministério da Saúde. Estratégias para o cuidado da pessoa com doença crônica: Diabetes mellitus. Cadernos de Atenção Básica, n° 36. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. 2013. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/estrategias_cuidado_pessoa_diabetes_mellitus_cab36.pdf (accessed on 22 July 2022).
- Silva, S.S.; Mambrini, J.V.M.; Turci, M.A.; Macinko, J.; Lima-Costa, M.F. Uso de serviços de saúde por diabéticos cobertos por plano privado em comparação aos usuários do Sistema Único de Saúde no Município de Belo Horizonte, Minas Gerais, Brasil. Cad. Saúde Pública 2016, 32, e00014615. [Google Scholar] [CrossRef]
- Ministério da Saúde. Portaria nº 483, de 1º de abril de 2014. Redefine a Rede de Atenção à Saúde das Pessoas com Doenças Crônicas no Âmbito do Sistema Único de Saúde (SUS) e estabelece diretrizes para a organização das Suas Linhas de Cuidado.: Gabinete do Ministro. Sistema de Legislação da Saúde. 2014. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2014/prt0483_01_04_2014.html (accessed on 22 July 2022).
- Salci, M.A.; Meirelles, B.H.S.; Silva, D.M.V.G. Prevention of chronic complications of diabetes mellitus according to complexity. Rev. Bras. Enferm. 2017, 70, 996–1003. [Google Scholar] [CrossRef]
- Franco, L.F.; Mafra, A.C.C.N.; Bracco, M.M.; Franco, L.J.; Naves, L.K.; Ribeiro, G.M.F.; Mangueira, C.L.P. Fasting glucose of patients from public health care in the southern region of São Paulo: Correlation with glycated hemoglobin and lipid levels. Rev. Bras. Epidemiol. 2019, 22, E190058. [Google Scholar] [CrossRef]
- Bassotto, H.; Locatelli, C. Avaliação da correlação diagnóstica dos níveis de HbA1c e microalbuminúria em pacientes com Diabetes mellitus tipo 2 como marcador de prevenção de complicações renais. RBAC 2020, 52, 359–365. [Google Scholar] [CrossRef]
- Birabwa, C.; Bwambale, M.F.; Waiswa, P.; Mayega, R.W. Quality and barriers of outpatient diabetes care in rural health facilities in Uganda—A mixed methods study. BMC Health Serv. Res. 2019, 19, 706. [Google Scholar] [CrossRef]
- Silva, L.B.; Silva, P.A.B.; Santos, J.F.G.; Silqueira, S.M.F.; Borges, E.L.; Soares, S.M. Risk strata and quality of care for the elderly in Primary Health Care. Rev. Lat. Am. Enfermagem. 2019, 27, e3166. [Google Scholar] [CrossRef] [PubMed]
- Siddique, K.B.; Islam, S.M.S.; Banik, P.C.; Rawal, L.B. Diabetes knowledge and utilization of healthcare services among patients with type 2 diabetes mellitus in Dhaka, Bangladesh. BMC Health Serv. Res. 2017, 17, 586. [Google Scholar] [CrossRef]
- Chandler, R.F.; Monnat, S.M. Racial/Ethnic Differences in Use of Health Care Services for Diabetes Management. Health Educ Behav. 2015, 42, 783–792. [Google Scholar] [CrossRef]
- American Diabetes Association. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018, 41, S105–S118. [Google Scholar] [CrossRef]
- Menezes, L.M.; Morais, N.N.A. Fundoscopy findings of diabetic and/or hipertensive patients. Rev. Bras. Oftalmol. 2020, 79, 28–32. [Google Scholar] [CrossRef]
- Santos, I.C.R.V.; Sobreira, C.M.M.; Nunes, E.N.S.; Morais, M.C.A. Prevalência e fatores associados a amputações por pé diabético. Ciênc. Saúde Coletiva 2013, 18, 3007–3014. [Google Scholar] [CrossRef]
- Nascimento, R.C.R.M.; Alvares, J.; Guera, A.A.; Gomes, I.C.; Costa, E.A.; Leite, S.N.; Costa, K.S.; Soeiro, O.M.; Guibu, I.A.; Karnikowski, M.G.O.; et al. Availability of essential medicines in primary health care of the Brazilian Unified Health System. Rev. Saúde Pública 2017, 51, 10s. [Google Scholar] [CrossRef]
- World Health Organization. Essential Medicines and Basic Health Technologies for Non Comunicable Diseases: Towards a Set of Actions to Improve Equitable Access in Member States. Geneva; 2015. Available online: https://www.who.int/nmh/ncd-tools/targets/Final_medicines_and_technologies_02_07_2015.pdf (accessed on 22 July 2022).
- Santos, A.L.; Marcon, S.S.; Teston, E.F.; Back, I.R.; Lino, I.G.T.; Batista, V.C.; Matsuda, L.M.; Haddad, M.C.F.L. Adherence to the treatment of diabetes mellitus and relationship with assistance in primary care. Rev. Min. Enferm. 2020, 24, e–1279. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1051306 (accessed on 31 October 2022). [CrossRef]
- de Lima Santos, A.; Marcon, S.S.; Silva, N.C.; Nati, V.H.; Pacheco, G.G.; Bolsoni, L.L.; de Freitas Góes, H.L. Avaliação positiva da assistência às pessoas com diabetes mellitus na atenção básica. Ciênc. Cuid. Saúde 2020, 19, e50402. [Google Scholar]
- Organização Pan-Americana da Saúde. O cuidado das condições crônicas na atenção primária à saúde: O imperativo da consolidação da estratégia da saúde da família. Eugênio Vilaça Mendes. 2012. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/cuidado_condicoes_atencao_primaria_saude.pdf (accessed on 22 July 2022).
- Macinko, J.; Mullachery, P.; Proietti, F.A.; Lima-Costa, M.F. Who experiences discrimination in Brazil? Evidence from a large metropolitan region. Int. J. Equity Health 2012, 11, 80. [Google Scholar] [CrossRef]
- Oliveira, F.E.G.; Griep, R.H.; Chor, D.; Giatti, L.; Machado, L.A.C.; Barreto, S.M.; Pereira, A.C.; Fonseca, M.J.M.; Bastos, L.S. Racial inequalities in multimorbidity: Baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Public Health 2022, 22, 1319. [Google Scholar] [CrossRef]
- Carrillo-Balam, G.; Cantoral, A.; Rodríguez-Carmona, Y.; Christensen, D.L. Health-care coverage and access to health care in the context of type 2 diabetes and hypertension in rural Mexico: A systematic literature review. Public Health 2020, 181, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Luiza, G.; Lima, J.G.; Rocha, E.S.C.; Herkrath, F.J. Access and coverage of Primary Health Care for rural and urban populations in the northern region of Brazil. Saúde Debate 2018, 42, 81–99. [Google Scholar] [CrossRef]

| Item | Percentage (%) of People with DM Who | Answer |
|---|---|---|
| 1 | Received medical care for diabetes in the last 12 months | Q39. When was the last time you received medical care for diabetes? |
| 2 | Received the last treatment for diabetes in primary care | Q40. Where was the last time you received medical care for diabetes? Option response: 01. Basic health unit (health center or family health unit). |
| 3 | Received the last treatment by the SUS | Q43. Was this service provided by the SUS? |
| 4 | Received medical care from the same doctor as the previous consultation | Q44. In the last consultation, was it the same doctor who attended you in the previous consultations? |
| 5 | Received a request for blood tests | Q47. Was any test requested in any of the diabetes care services? The. Blood test (cholesterol, blood glucose, triglycerides). |
| 6 | Received a request for glycated hemoglobin | Q47. Was any test requested in any of the diabetes care services? B. glycated hemoglobin. |
| 7 | Received requests for urine tests | Q47. Was any test requested in any of the diabetes care services? d. Urine analysis. |
| 8 | Performed requested exams | Q48. Did you perform all the requested exams? |
| 9 | Were referred to specialists and attended consultations with a specialist doctor | Q50. In any of the consultations for diabetes, was there a referral to a specialist doctor, such as a cardiologist, endocrinologist, nephrologist or ophthalmologist? Q51. Did you go to all consultations with a specialist doctor? |
| 10 | Eyes examined in the last 12 months | Q53. When was the last time you had an eye exam or fundus in which your pupil dilated? |
| 11 | Feet examined in the last 12 months | Q54. When was the last time a doctor or healthcare professional examined your feet for sensitivity or the presence of sores or irritations? |
| 12 | Hospitalization for DM or for some complication | Q56. Have you ever been hospitalized because of diabetes or any complications? |
| 13 | Obtained medication for DM or insulin from the Popular Pharmacy Program | Q36. Were any of the diabetes medications or insulin obtained from the Popular Pharmacy Program? |
| 14 | Obtained medication for DM or insulin obtained from a SUS service | Q37. Were any of the diabetes medications or insulin obtained from a public health service? |
| 15 | Received guidance on healthy eating | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? Option response: a. Maintain a healthy diet (with fruits and vegetables). |
| 16 | Received guidance on maintaining adequate weight | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? Option response: b. maintaining adequate weight. |
| 17 | Received guidance on physical activity | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? Option response: c. Practice regular physical activity. |
| 18 | Received guidance on not smoking | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? |
| 19 | Received guidance on not drinking to excess | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? |
| 20 | Received guidance on measuring blood glucose at home | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? Option response: g. Measure blood glucose at home. |
| 21 | Received guidance on examining their feet regularly | Q46. In any of the diabetes consultations, did a doctor or other health professional give you any of these recommendations? Option response: h. Examine your feet regularly. |
| 22 | Have a private health plan | I1. Does the participant have any private, company or public health plan (medical or dental?) |
| Variables | n | % | 95% CI |
|---|---|---|---|
| Age range (years) | |||
| 18–29 | 12 | 2. | 1.2–6.2 |
| 30–39 | 32 | 7.9 | 5.1–12.0 |
| 40–59 | 209 | 39.9 | 35.0–45.4 |
| ≥60 | 239 | 49.4 | 43.5–55.5 |
| Sex | |||
| Female | 314 | 61.0 | 55.0–66.8 |
| Male | 178 | 39.0 | 33.2–45.1 |
| Education level (years) | |||
| No education/Incomplete elementary school | 289 | 60.5 | 54.5–66.2 |
| Complete elementary school/incomplete high school | 61 | 12.3 | 9.0–16.6 |
| Complete high school/incomplete higher education | 84 | 17.1 | 13.2–21.9 |
| Complete higher education or more | 58 | 10.1 | 7.4–13.5 |
| Race/skin color | |||
| White | 197 | 40.3 | 34.2–46.6 |
| Black | 53 | 9.6 | 7.1–13.0 |
| Mixed-race | 232 | 48.2 | 42.2–54.3 |
| Others * | 10 | 1.9 | 0.9–4.1 |
| Married/partner | |||
| No | 245 | 39.0 | 33.7–44.6 |
| Yes | 247 | 61.0 | 55.4–66.3 |
| Place of residence | |||
| Capital | 257 | 39.5 | 34.0–45.2 |
| Metropolitan region | 52 | 14.3 | 10.0–20.1 |
| Other places | 183 | 46.2 | 40.4–52.2 |
| Federation Units | |||
| Goiás | 146 | 43.0 | 36.9–49.3 |
| Distrito Federal | 101 | 17.0 | 13.7–20.9 |
| Mato Grosso | 103 | 20.2 | 16.0–25.1 |
| Mato Grosso do Sul | 142 | 19.8 | 16.5–23.7 |
| Indicators | n | % | 95% CI |
|---|---|---|---|
| Received medical care for diabetes in the last 12 months | 364 | 74.6 | 69.1–79.3 |
| Received the last treatment for diabetes in primary care | 228 | 46.4 | 40.6–52.4 |
| Received the last treatment by the SUS | 292 | 57.3 | 51.2–63.2 |
| Received medical care from the same doctor as the previous consultation | 271 | 56.6 | 50.4–62.6 |
| Received a request for blood tests | 393 | 77.7 | 71.2–83.2 |
| Received a request for glycated hemoglobin | 290 | 55.6 | 49.2–61.8 |
| Received requests for urine tests | 349 | 70.4 | 63.8–76.2 |
| Performed requested exams | 384 | 97.8 | 95.6–98.9 |
| Were referred to specialists and attended consultations with a specialist doctor | 69 | 25.7 | 19.4–33.1 |
| Eyes examined in the last 12 months | 158 | 29.3 | 24.5–34.7 |
| Feet examined in the last 12 months | 114 | 18.9 | 14.7–23.9 |
| Hospitalization for DM or for some complication | 68 | 13.5 | 10.2–17.7 |
| Obtained medication for DM or insulin from the Popular Pharmacy Program | 226 | 66.5 | 60.0–72.5 |
| Obtained medication for DM or insulin obtained from a SUS service | 239 | 70.8 | 63.5–77.2 |
| Received guidance on healthy eating | 414 | 83.8 | 78.9–87.2 |
| Received guidance on maintaining adequate weight | 397 | 80.7 | 75.8–84.8 |
| Received guidance on physical activity | 384 | 77.2 | 71.1–82.3 |
| Received guidance on not smoking | 348 | 68.9 | 63.1–74.2 |
| Received guidance on not drinking to excess | 347 | 69.4 | 63.6–74.6 |
| Received guidance on measuring blood glucose at home | 281 | 55.7 | 49.5–61.6 |
| Received guidance on examining their feet regularly | 236 | 44.5 | 38.8–50.5 |
| Have a private health plan | 184 | 36.4 | 30.7–42.6 |
| Items | α 1 (95% CI) | p-Value * | β 2 (IC95%) | p-Value ** |
|---|---|---|---|---|
| Received medical care for diabetes in the last 12 months | 1.69 (1.28; 2.11) | <0.001 | −0.85 (−1.05; −0.64) | <0.001 |
| Received a request for blood tests | 2.90 (2.16; 3.63) | <0.001 | −0.88 (−1.05; −0.71) | <0.001 |
| Received a request for glycated hemoglobin | 2.04 (1.54; 2.53) | <0.001 | −0.24 (−0.38; −0.10) | <0.001 |
| Received requests for urine tests | 2.16 (1.64; 2.6) | <0.001 | −0.63 (−0.79;−0.46) | <0.001 |
| Eyes examined in the last 12 months | 0.92 (0.62; 1.21) | <0.001 | 0.97 (0.64;1.29) | <0.001 |
| Feet examined in the last 12 months | 1.01 (0.68; 1.35) | <0.001 | 1.42 (1.00;1.83) | <0.001 |
| Received guidance on healthy eating | 17.9 (−0.18; 36.0) | 0.052 | −0.83 (−0.97;−0.68) | <0.001 |
| Received guidance on maintaining adequate weight | 8.01 (4.77; 11.2) | <0.001 | −0.71 (−0.4;−0.59) | <0.001 |
| Received guidance on physical activity | 6.84 (4.35; 9.33) | <0.001 | −0.63 (−0.75; −0.51) | <0.001 |
| Received guidance on not smoking | 5.63 (3.44; 7.81) | <0.001 | −0.44 (−0.55; −0.33) | <0.001 |
| Received guidance on not drinking to excess | 5.75 (3.53; 7.97) | <0.001 | −0.43 (−0.54; −0.33) | <0.001 |
| Received guidance on measuring blood glucose at home | 2.00 (1.51; 2.49) | <0.001 | −0.18 (−0.32; −0.04) | 0.009 |
| Received guidance on examining their feet regularly | 2.19 (1.65; 2.73) | <0.001 | 0.09 (−0.03–0.22) | 0.145 |
| Variables | Scores | p-Value | Cohen’s d | |
|---|---|---|---|---|
| Mean ± SE | 95%CI | |||
| Age range (years) | ||||
| 21–29 | 50.0 (9.6) | 30.9–69.0 | 0.970 * | 0.08 |
| 30–39 | 51.0 (4.8) | 41.6–60.3 | ||
| 40–59 | 50.9 (1.7) | 47.5–54.3 | ||
| ≥60 | 52.0 (1.6) | 48.8–55.1 | ||
| Sex | ||||
| Male | 51.3 (1.4) | 48.5–54.1 | 0.959 ** | 0.09 |
| Female | 51.6 (1.4) | 47.9–55.3 | ||
| Education level (years) | ||||
| Complete higher education or more | 50.8 (1.4) | 48.1–53.4 | 0.186 * | 0.22 |
| Complete high school/incomplete higher education | 50.3 (3.6) | 43.3–57.3 | ||
| Complete elementary school/incomplete high school | 51.3 (3.0) | 45.3–57.1 | ||
| No education/Incomplete elementary school | 55.9 (3.7) | 48.6–63.2 | ||
| Race/skin color *** | ||||
| White | 54.0 (1.8) | 50.4–57.4 | 0.020 * | 0.21 |
| Black | 54.6 (3.3) | 48.2–61.1 | ||
| Mixed race | 48.4 (1.6) | 45.2–51.6 | ||
| Place of residence | ||||
| Capital | 55.6 (1.6) | 52.4–58.8 | <0.001 * | 0.41 |
| Metropolitan region | 50.3 (2.8) | 44.7–55.9 | ||
| Other places | 45.9 (1.8) | 42.4–49.4 | ||
| Total | 52.3 (1.1) | 50.2–54.5 | ||
| Variables | β | 95% CI | p-Value |
|---|---|---|---|
| Age range (years) | |||
| 21–29 ® | |||
| 30–39 | 1.04 | −15.83; 17.92 | 0.903 |
| 40–59 | 1.66 | −13.08; 16.42 | 0.824 |
| ≥60 | 2.45 | −12.35; 17.25 | 0.745 |
| Sex | |||
| Male ® | |||
| Female | −0.53 | −5.20; 4.13 | 0.823 |
| Education level (years) | |||
| Complete higher education or more® | |||
| Complete high school/incomplete higher education | −3.89 | −12.41; 4.63 | 0.371 |
| Complete elementary school/incomplete high school | −3.29 | −12.43; 5.84 | 0.479 |
| No education/Incomplete elementary school | −0.56 | −8.26; 7.12 | 0.884 |
| Race/color (self-declared) | |||
| White ® | |||
| Black | −0.01 | −7.62; −7.60 | 0.997 |
| Mixed-race | −4.97 | −9.77; −0.18 | 0.042 |
| Place of residence | |||
| Capital ® | |||
| Metropolitan region | −5.32 | −12.93; 2.27 | 0.169 |
| Other places | −9.71 | −14.78; −4.63 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siqueira, I.S.L.d.; Guimarães, R.A.; Pagotto, V.; Rosso, C.F.W.; Batista, S.R.R.; Barbosa, M.A. Access and Use of Health Services by People with Diabetes from the Item Response Theory. Int. J. Environ. Res. Public Health 2022, 19, 14612. https://doi.org/10.3390/ijerph192114612
Siqueira ISLd, Guimarães RA, Pagotto V, Rosso CFW, Batista SRR, Barbosa MA. Access and Use of Health Services by People with Diabetes from the Item Response Theory. International Journal of Environmental Research and Public Health. 2022; 19(21):14612. https://doi.org/10.3390/ijerph192114612
Chicago/Turabian StyleSiqueira, Isabela Silva Levindo de, Rafael Alves Guimarães, Valéria Pagotto, Claci Fátima Weirich Rosso, Sandro Rogério Rodrigues Batista, and Maria Alves Barbosa. 2022. "Access and Use of Health Services by People with Diabetes from the Item Response Theory" International Journal of Environmental Research and Public Health 19, no. 21: 14612. https://doi.org/10.3390/ijerph192114612
APA StyleSiqueira, I. S. L. d., Guimarães, R. A., Pagotto, V., Rosso, C. F. W., Batista, S. R. R., & Barbosa, M. A. (2022). Access and Use of Health Services by People with Diabetes from the Item Response Theory. International Journal of Environmental Research and Public Health, 19(21), 14612. https://doi.org/10.3390/ijerph192114612







