Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Search Strategy
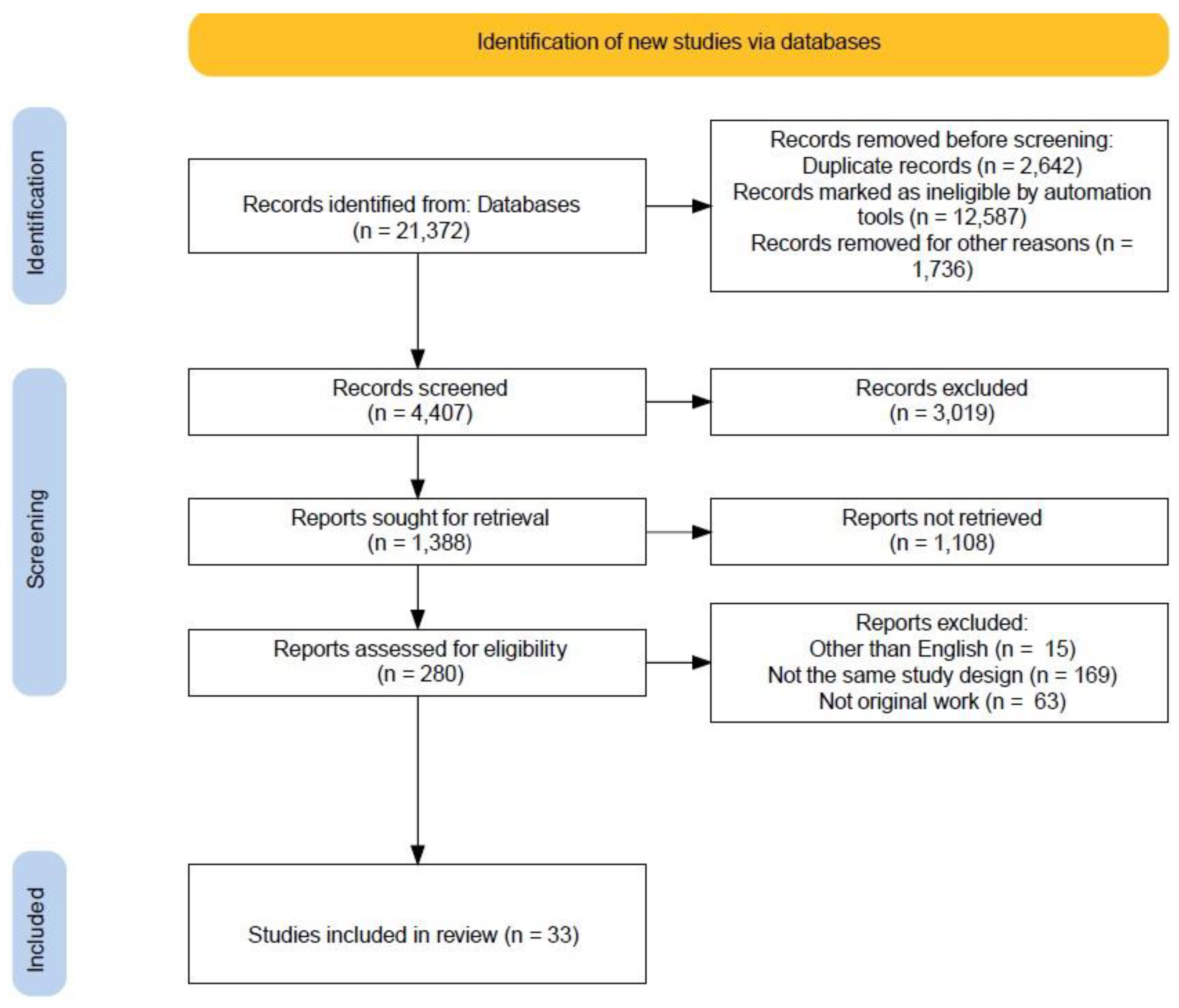
2.2. Study Screening and Selection
2.3. Data Extraction
2.4. Eligibility Criteria
2.5. Quality Assessment
2.6. Barriers to Hypertension Control
3. Results
3.1. Overview of the Included Studies
3.2. Methodological Quality of Included Studies
3.3. Barriers to Hypertension Control
4. Discussion
4.1. Barriers to Optimal Hypertension Control
4.1.1. Patient-Related Barriers
Sociodemographic Factors
Comorbidity
4.1.2. Medication Nonadherence
4.1.3. Lifestyle Factors
4.1.4. Pharmacotherapy-Related Barriers
4.2. Implications for Hypertension Control across Different Countries
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 10 February 2021).
- Gheorghe, A.; Griffiths, U.; Murphy, A.; Legido-Quigley, H.; Lamptey, P.; Perel, P. The Economic Burden of Cardiovascular Disease and Hypertension in Low- and Middle-Income Countries: A Systematic Review. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Ab Majid, N.L.; Omar, M.A.; Khoo, Y.Y.; Mahadir Naidu, B.; Ling Miaw Yn, J.; Rodzlan Hasani, W.S.; Mat Rifin, H.; Abd Hamid, H.A.; Robert Lourdes, T.G.; Mohd Yusoff, M.F. Prevalence, Awareness, Treatment and Control of Hypertension in the Malaysian Population: Findings from the National Health and Morbidity Survey 2006–2015. J. Hum. Hypertens. 2018, 32, 617–624. [Google Scholar] [CrossRef] [PubMed]
- White, W.B. Importance of Blood Pressure Control Over a 24-Hour Period. J. Manag. Care Pharm. 2007, 13, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.; Kearney, P.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies from 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B. PRISMA-S: An Extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef]
- DistillerSR Risk of Bias Instrument for Cross Sectional Surveys of Attitudes and Practices. Available online: https://www.evidencepartners.com/resources/methodological-resources/risk-of-bias-instrument-for-cross-sectional-surveys-of-attitudes-and-practices-distillersr (accessed on 6 April 2022).
- Animut, Y.; Assefa, A.T.; Lemma, D.G. Blood Pressure Control Status and Associated Factors among Adult Hypertensive Patients on Outpatient Follow-up at University of Gondar Referral Hospital, Northwest Ethiopia: A Retrospective Follow-up Study. Integr. Blood Press. Control. 2018, 11, 37–46. [Google Scholar] [CrossRef]
- Sibomana, J.P.; McNamara, R.L.; Walker, T.D. Patient, Clinician and Logistic Barriers to Blood Pressure Control among Adult Hypertensives in Rural District Hospitals in Rwanda: A Cross-Sectional Study. BMC Cardiovasc. Disord. 2019, 19, 1–8. [Google Scholar] [CrossRef]
- Paquissi, F.C.; Cuvinje, A.B.P.; Cuvinje, A.B.; Paquissi, A.M. Hypertension among Outpatients at a General Hospital in South Angola: Prevalence, Awareness, Treatment, and Control. Clin. Med. Insights. Cardiol. 2016, 10, 111–116. [Google Scholar] [CrossRef]
- Zack, R.M.; Irema, K.; Kazonda, P.; Leyna, G.H.; Liu, E.; Spiegelman, D.; Fawzi, W.; Njelekela, M.; Killewo, J.; Danaei, G. Determinants of High Blood Pressure and Barriers to Diagnosis and Treatment in Dar Es Salaam, Tanzania. J. Hypertens. 2016, 34, 2353. [Google Scholar] [CrossRef]
- Duboz, P.; Boëtsch, G.; Gueye, L.; Macia, E. Hypertension Prevalence, Awareness, Treatment and Control in Dakar (Senegal). J. Hum. Hypertens. 2014, 28, 489–493. [Google Scholar] [CrossRef]
- Menanga, A.; Edie, S.; Nkoke, C.; Boombhi, J.; Musa, A.J.; Mfeukeu, L.K.; Kingue, S. Factors Associated with Blood Pressure Control amongst Adults with Hypertension in Yaounde, Cameroon: A Cross-Sectional Study. Cardiovasc. Diagn. Ther. 2016, 6, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Okwuonu, C.G.; Ojimadu, N.E.; Okaka, E.I.; Akemokwe, F.M. Patient-Related Barriers to Hypertension Control in a Nigerian Population. Int. J. Gen. Med. 2014, 7, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Iloh, G.U.P.; Ofoedu, J.N.; Njoku, P.U.; Amadi, A.N.; Godswill-Uko, E.U. Medication Adherence and Blood Pressure Control amongst Adults with Primary Hypertension Attending a Tertiary Hospital Primary Care Clinic in Eastern Nigeria. Afr. J. Prim. Health Care Fam. Med. 2013, 5, 1–6. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Mobula, L.M.; Burnham, G.; Ansong, D.; Plange-Rhule, J.; Sarfo-Kantanka, O.; Ofori-Adjei, D. Factors Associated with Uncontrolled Blood Pressure among Ghanaians: Evidence from a Multicenter Hospital-Based Study. PLoS ONE 2018, 13, 1–19. [Google Scholar] [CrossRef]
- Harrison, M.A.; Marfo, A.F.A.; Opare-Addo, M.N.A.; Ankrah, D.N.A.; Acheampong, F.; Nelson, F.; Buabeng, K.O. Anti-Hypertensive Medication Access and Affordability and Their Association with Blood Pressure Control at a Teaching Hospital in Ghana. Pan Afr. Med. J. 2021, 39, 184. [Google Scholar] [CrossRef]
- Devkota, S.; Dhungana, R.R.; Pandey, A.R.; Bista, B.; Panthi, S.; Thakur, K.K.; Gajurel, R.M. Barriers to Treatment and Control of Hypertension among Hypertensive Participants: A Community-Based Cross-Sectional Mixed Method Study in Municipalities of Kathmandu, Nepal. Front Cardiovasc. Med. 2016, 3, 26. [Google Scholar] [CrossRef] [PubMed]
- Dhungana, R.R.; Pedisic, Z.; Dhimal, M.; Bista, B.; de Courten, M. Hypertension Screening, Awareness, Treatment, and Control: A Study of Their Prevalence and Associated Factors in a Nationally Representative Sample from Nepal. Glob. Health Action. 2022, 15, 2000092. [Google Scholar] [CrossRef]
- Son, P.T.; Quang, N.N.; Viet, N.L.; Khai, P.G.; Wall, S.; Weinehall, L.; Bonita, R.; Byass, P. Prevalence, Awareness, Treatment and Control of Hypertension in Vietnamresults from a National Survey. J. Hum. Hypertens. 2012, 26, 268–280. [Google Scholar] [CrossRef]
- Wang, Y.B.; Kong, D.G.; Ma, L.L.; Wang, L.X. Patient Related Factors for Optimal Blood Pressure Control in Patients with Hypertension. Afr. Health Sci. 2013, 13, 579–583. [Google Scholar] [CrossRef][Green Version]
- Li, Y.; Feng, X.; Zhang, M.; Zhou, M.; Wang, N.; Wang, L. Clustering of Cardiovascular Behavioral Risk Factors and Blood Pressure among People Diagnosed with Hypertension: A Nationally Representative Survey in China. Sci. Rep. 2016, 6, 1–7. [Google Scholar] [CrossRef]
- Xu, D.; Chen, W.; Li, X.; Zhang, Y.; Li, X.; Lei, H.; Wei, Y.; Li, W.; Hu, D.; Wedick, N.M.; et al. Factors Associated with Blood Pressure Control in Hypertensive Patients with Coronary Heart Disease: Evidence from the Chinese Cholesterol Education Program. PLoS ONE 2013, 8, e63135. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Xu, S.K.; Guo, Q.H.; Hu, Z.; Wang, H.Y.; Yu, J.; Li, W.H.; Tang, G.B.; Zhang, H.F.; Li, Y.; et al. Barriers to Blood Pressure Control in China in a Large Opportunistic Screening. J. Clin. Hypertens. 2020, 22, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; He, Y.; Jiang, B.; Sun, D.; Wang, J.; Liu, M.; Yang, S.; Wang, Y. Trends in Prevalence, Awareness, Treatment and Control of Hypertension during 2001-2010 in an Urban Elderly Population of China. PLoS ONE 2015, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Rao, L.; Li, H. Comparison of the Management and Control of Hypertension by Public and Private Primary Care Providers in Shenzhen, China. Heliyon 2021, 7, e06280. [Google Scholar] [CrossRef]
- de Souza, C.S.; Stein, A.T.; Bastos, G.A.N.; Pellanda, L.C. Blood Pressure Control in Hypertensive Patients in the “Hiperdia Program”: A Territory-Based Study. Arq. Bras. Cardiol. 2014, 102, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Gala, P.; Moshokgo, V.; Seth, B.; Ramasuana, K.; Kazadi, E.; M’buse, R.; Pharithi, S.; Gobotsamang, K.; Szymanowski, P.; Kerobale, R.O.; et al. Medication Errors and Blood Pressure Control Among Patients Managed for Hypertension in Public Ambulatory Care Clinics in Botswana. J. Am. Heart Assoc. 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Nassr, O.A.; Forsyth, P. Evaluation of Blood Pressure Control and Associated Factors among Patients with Hypertension in Iraq: A Prospective Cross-Sectional Study. J. Pharm. Bioallied. Sci. 2019, 11, 232–239. [Google Scholar] [CrossRef]
- Lerner, A.G.; Bernabe-Ortiz, A.; Gilman, R.H.; Smeeth, L.; Miranda, J.J. The ‘Rule of Halves’ Does Not Apply in Peru: Awareness, Treatment, and Control of Hypertension and Diabetes in Rural, Urban and Rural-to-Urban Migrants. Crit. Pathw. Cardiol. 2013, 12, 53. [Google Scholar] [CrossRef]
- Zhang, J.; Healy, H.G.; Venuthurupalli, S.K.; Tan, K.S.; Wang, Z.; Cameron, A.; Hoy, W.E. Blood Pressure Management in Hypertensive People with Non-Dialysis Chronic Kidney Disease in Queensland, Australia. BMC Nephrol. 2019, 20, 1–10. [Google Scholar] [CrossRef]
- Santosa, A.; Zhang, Y.; Weinehall, L.; Zhao, G.; Wang, N.; Zhao, Q.; Wang, W.; Ng, N. Gender Differences and Determinants of Prevalence, Awareness, Treatment and Control of Hypertension among Adults in China and Sweden. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Li, Y.T.; Wang, H.H.X.; Liu, K.Q.L.; Lee, G.K.Y.; Chan, W.M.; Griffiths, S.M.; Chen, R.L. Medication Adherence and Blood Pressure Control Among Hypertensive Patients With Coexisting Long-Term Conditions in Primary Care Settings. Medicine 2016, 95, e3572. [Google Scholar] [CrossRef] [PubMed]
- Khayyat, S.M.; Khayyat, S.M.S.; Hyat Alhazmi, R.S.; Mohamed, M.M.A.; Hadi, M.A. Predictors of Medication Adherence and Blood Pressure Control among Saudi Hypertensive Patients Attending Primary Care Clinics: A Cross-Sectional Study. PLoS ONE 2017, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, D.; Bravo, M.; Koch, E.; Gatica, S.; Ahlers, I.; Henríquez, O.; Romero, T. Overcoming Barriers in the Management of Hypertension: The Experience of the Cardiovascular Health Program in Chilean Primary Health Care Centers. Int. J. Hypertens. 2012, 2012, 405892. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ham, O.K.; Yang, S.J. Lifestyle Factors Associated with Blood Pressure Control among Those Taking Antihypertensive Medication. Asia Pac. J. Public Health 2011, 23, 485–495. [Google Scholar] [CrossRef]
- Tiffe, T.; Morbach, C.; Rücker, V.; Gelbrich, G.; Wagner, M.; Faller, H.; Störk, S.; Heuschmann, P.U. Impact of Patient Beliefs on Blood Pressure Control in the General Population: Findings from the Population-Based STAAB Cohort Study. Int. J. Hypertens. 2019, 2019, 9385397. [Google Scholar] [CrossRef]
- Cordero, A.; Bertomeu-Martínez, V.; Mazón, P.; Fácila, L.; Bertomeu-González, V.; Cosín, J.; Galve, E.; Núñez, J.; Lekuona, I.; González-Juanatey, J.R. Factors Associated With Uncontrolled Hypertension in Patients With and Without Cardiovascular Disease. Revista Española de Cardiología 2011, 64, 587–593. [Google Scholar] [CrossRef]
- Murphy, C.M.; Kearney, P.M.; Shelley, E.B.; Fahey, T.; Dooley, C.; Kenny, R.A. Hypertension Prevalence, Awareness, Treatment and Control in the over 50s in Ireland: Evidence from the Irish Longitudinal Study on Ageing. J. Public Health 2016, 38, 450–458. [Google Scholar] [CrossRef]
- Liew, S.J.; Lee, J.T.; Tan, C.S.; Koh, C.H.G.; van Dam, R.; Müller-Riemenschneider, F. Sociodemographic Factors in Relation to Hypertension Prevalence, Awareness, Treatment and Control in a Multi-Ethnic Asian Population: A Cross-Sectional Study. BMJ Open 2019, 9, 1–10. [Google Scholar] [CrossRef]
- Chmiel, C.; Wang, M.; Senn, O.; Del Prete, V.; Zoller, M.; Rosemann, T.; Steurer-Stey, C. Uncontrolled Arterial Hypertension in Primary Care—Patient Characteristics and Associated Factors. Swiss. Med. Wkly. 2012, 142, w13693. [Google Scholar] [CrossRef]
- Reckelhoff, J.F. Gender Differences in the Regulation of Blood Pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef]
- Shimboa, D.; Levitanb, E.B.; IIIc, J.N.B.; Calhound, D.A.; Judde, S.E.; Lacklandf, D.T.; Saffordg, M.M.; Oparilg, S.; Muntnerb, P. The Contributions of Unhealthy Lifestyle Factors to Apparent Resistant Hypertension: Findings from the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. J. Hypertens. 2013, 3, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Gee, M.E.; Bienek, A.; Campbell, N.R.C.; Bancej, C.M.; Robitaille, C.; Kaczorowski, J.; Joffres, M.; Dai, S.; Gwadry-Sridar, F.; Nolan, R.P. Prevalence of, and Barriers to, Preventive Lifestyle Behaviors in Hypertension (from a National Survey of Canadians with Hypertension). Am. J. Cardiol. 2012, 109, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Tapela, N.; Collister, J.; Clifton, L.; Turnbull, I.; Rahimi, K.; Hunter, D.J. Prevalence and Determinants of Hypertension Control among Almost 100 000 Treated Adults in the UK. Open Heart 2021, 8, e001461. [Google Scholar] [CrossRef] [PubMed]
- Elnaem, M.H.; Kamarudin, N.H.; Syed, N.K.; Huri, H.Z.; Dehele, I.S.; Cheema, E. Associations between Socio-Demographic Factors and Hypertension Management during the Covid-19 Pandemic: Preliminary Findings from Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 9306. [Google Scholar] [CrossRef] [PubMed]
- Krousel-Wood, M.A.; Muntner, P.; Islam, T.; Morisky, D.E.; Webber, L.S. Barriers to and Determinants of Medication Adherence in Hypertension Management: Perspective of the Cohort Study of Medication Adherence Among Older Adults. Med. Clin. N. Am. 2009, 93, 753–769. [Google Scholar] [CrossRef] [PubMed]
- Arauz-Pacheo, C.; Parrott, M.A.; Raskin, P. Treatment of Hypertension in Adults With Diabetes. Clin. Diabetes 2003, 21, 120–121. [Google Scholar] [CrossRef][Green Version]
- Khangura, D.; Kurukulasuriya, L.R.; Whaley-Connell, A.; Sowers, J.R. Diabetes and Hypertension: Clinical Update. Am. J. Hypertens. 2018, 31, 515–521. [Google Scholar] [CrossRef]
- De Boer, I.H.; Bangalore, S.; Benetos, A.; Davis, A.M.; Michos, E.D.; Muntner, P.; Rossing, P.; Zoungas, S.; Bakris, G. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care 2017, 40, 1273–1284. [Google Scholar] [CrossRef]
- Rubio-Guerra, A.F.; Rodriguez-Lopez, L.; Vargas-Ayala, G.; Huerta-Ramirez, S.; Serna, D.C.; Lozano-Nuevo, J.J. Depression Increases the Risk for Uncontrolled Hypertension. Exp. Clin. Cardiol. 2013, 18, 10–12. [Google Scholar]
- Al-Ramahi, R. Adherence to Medications and Associated Factors: A Cross-Sectional Study among Palestinian Hypertensive Patients. J. Epidemiol. Glob. Health 2015, 5, 125–132. [Google Scholar] [CrossRef]
- Wachholz, P.A.; Masuda, P.Y.; Ferrari, A.C.; Villas Boas, P.J.F. Factors Related to Blood Pressure Control in a Prospective Cohort of Hypertensive Outpatients. Acta Sci.-Health Sci. 2016, 38, 57–63. [Google Scholar] [CrossRef][Green Version]
- Elnaem, M.H.; Rosley, N.F.F.; Alhifany, A.A.; Elrggal, M.E.; Cheema, E. Impact of Pharmacist-Led Interventions on Medication Adherence and Clinical Outcomes in Patients with Hypertension and Hyperlipidemia: A Scoping Review of Published Literature. J. Multidiscip. Healthc. 2020, 13, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Zeki, A.M.; Ramadan, A.M.; Zeb, F.K.; Ibrahim, M. Impact of Life-Style on Health and Physical Capability: A Data Mining Approach. In Proceedings of the 2nd Mediterranean Conference on Pattern Recognition and Artificial Intelligence, Rabat, Morocco, 27–28 March 2018; ACM International Conference Proceeding Series. Association for Computing Machinery: New York, NY, USA, 2018; Volume 2018-March, pp. 119–124. [Google Scholar]
- Gradman, A.H.; Basile, J.N.; Carter, B.L.; Bakris, G.L. Combination Therapy in Hypertension. J. Am. Soc. Hypertens. 2010, 4, 90–98. [Google Scholar] [CrossRef]
- Nelson, S.A.E.; Dresser, G.K.; Vandervoort, M.K.; Wong, C.J.; Feagan, B.G.; Mahon, J.L.; Feldman, R.D. Barriers to Blood Pressure Control: A STITCH Substudy. J. Clin. Hypertens. 2011, 13, 73–80. [Google Scholar] [CrossRef]
- Choudhry, N.K.; Kronish, I.M.; Vongpatanasin, W.; Ferdinand, K.C.; Pavlik, V.N.; Egan, B.M.; Schoenthaler, A.; Miller, N.H.; Hyman, D.J. Medication Adherence and Blood Pressure Control: A Scientific Statement From the American Heart Association. Hypertension 2022, 79, E1–E14. [Google Scholar] [CrossRef] [PubMed]
- Yue, Z.; Bin, W.; Weilin, Q.; Aifang, Y. Effect of Medication Adherence on Blood Pressure Control and Risk Factors for Antihypertensive Medication Adherence. J. Eval. Clin. Pract. 2015, 21, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Elnaem, M.H.; Nik Mohamed, M.H.; Zaman Huri, H.; Azarisman, S.M. Effectiveness and Prescription Pattern of Lipid-Lowering Therapy and Its Associated Factors among Patients with Type 2 Diabetes Mellitus in Malaysian Primary Care Settings. Ther. Clin. Risk Manag. 2019, 18, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Elnaem, M.H.; Nik Mohamed, M.H.; Hazim, A.; Rabiatul, I. Evaluation of Proton Pump Inhibitors Prescribing among Non-Critically Ill Hospitalized Patients in a Malaysian Tertiary Hospital. J. Appl. Pharm. Sci. 2017, 7, 77–83. [Google Scholar] [CrossRef]
- Elnaem, M.H.; Nik Mohamed, M.H.; Huri, H.Z. Pharmacist-Led Academic Detailing Improves Statin Therapy Prescribing for Malaysian Patients with Type 2 Diabetes: Quasi- Experimental Design. PLoS ONE 2019, 14, e0220458. [Google Scholar] [CrossRef]
- Chowdhury, E.K.; Owen, A.; Krum, H.; Wing, L.M.H.; Ryan, P.; Nelson, M.R.; Reid, C.M. Barriers to Achieving Blood Pressure Treatment Targets in Elderly Hypertensive Individuals. J. Hum. Hypertens. 2013, 27, 545–551. [Google Scholar] [CrossRef]
- Elnaem, M.H.; Elrggal, M.E.; Syed, N.; Naqvi, A.A.; Hadi, M.A. Knowledge and Perceptions towards Cardiovascular Disease Prevention among Patients with Type 2 Diabetes Mellitus: A Review of Current Assessments and Recommendations. Curr. Diabetes. Rev. 2020, 17, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J.; Shrestha, A.D.; Neupane, D.; Kallestrup, P. Non-Adherence to Anti-Hypertensive Medication in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis of 92443 Subjects. J. Hum. Hypertens. 2017, 31, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Elnaem, M.H.; Irwan, N.A.; Abubakar, U.; Sulaiman, S.A.S.; Elrggal, M.E.; Cheema, E. Impact of Medication Regimen Simplification on Medication Adherence and Clinical Outcomes in Patients with Long-Term Medical Conditions. Patient Prefer. Adherence 2020, 14, 2135–2145. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, C.; Khan, H.A.; Gudleski, G.; Reynolds, J.L.; Bakhai, S.Y. Multifaceted Strategies to Improve Blood Pressure Control in a Primary Care Clinic: A Quality Improvement Project. Int. J. Cardiol. Hypertens 2020, 7, 100060. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Manias, E.; Walker, R.; Gorelik, A. A Multifactorial Intervention to Improve Blood Pressure Control in Co-Existing Diabetes and Kidney Disease: A Feasibility Randomized Controlled Trial. J. Adv. Nurs. 2012, 68, 2515–2525. [Google Scholar] [CrossRef]
- Stephen, C.; Halcomb, E.; McInnes, S.; Batterham, M.; Zwar, N. Improving Blood Pressure Control in Primary Care: The ImPress Study. Int. J. Nurs. Stud. 2019, 95, 28–33. [Google Scholar] [CrossRef]
- Carter, B.L.; Coffey, C.S.; Ardery, G.; Uribe, L.; Ecklund, D.; James, P.; Egan, B.; Weg, M.V.; Chrischilles, E.; Vaughn, T. Cluster-Randomized Trial of a Physician/Pharmacist Collaborative Model to Improve Blood Pressure Control. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 235–243. [Google Scholar] [CrossRef]
| No | Author | Country and Income Class | Sample Included | Significant Findings |
|---|---|---|---|---|
| 1 | Animut, et al., 2018 [8] | Ethiopia (Low-income) | 395 hypertensive patients. | 50.4% had their BP controlled. Salt intake, overweight, and obesity were negatively associated with BP control. Physical activity, duration on antihypertensive drugs (2–4 or ≥5 yrs.), and high adherence were positively correlated with BP control. |
| 2 | Sibomana, et al., 2019 [9] | Rwanda (Low-income) | 112 patients from four district rural hospitals. | 29% had their BP controlled. 77% reported medication adherence associated with literacy and lack of adverse effects. 50% highlighted physicians’ nonadherence to clinical guidelines. |
| 3 | Paquissi, et al., 2016 [10] | Angola (Lower-middle-income) | 102 hypertensive patients. | 7.8% had their BP controlled, while 54.9% and 28.4% were aware and treated, respectively. Younger (<37 years) and male patients were more likely to be unaware of their disease. |
| 4 | Duboz, et al., 2014 [12] | Senegal (Lower-middle-income) | 165 hypertensive patients. | 5.4% had their BP controlled, while 27.8% and 17% were aware and treated, respectively. Older patients (≥50 years) were more likely to be aware of and treated for their HTN. |
| 5 | Zack, et al., 2016 [11] | Tanzania (Lower-middle-income) | 803 hypertensive patients. | 10% had their BP controlled, while 48% and 22% were aware and treated, respectively. Higher BP readings were reported in male, older, uneducated, unemployed, overweight, obese, and physically-inactive patients. |
| 6 | Menanga, et al., 2016 [13] | Cameroon (Lower-middle-income) | 440 hypertensive patients in an urban city. | 36.8% had their BP controlled. Optimal medication adherence and dietary lifestyle changes were significantly associated with BP control. |
| 7 | Okwuonu, et al., 2014 [14] | Nigeria (Lower-middle-income) | 252 adults with hypertension. | 32.9% had their BP controlled (affected by knowledge and lifestyle changes) Low medication adherence was reported in 68.7% of patients due to forgetfulness (61.2%), financial barriers (56.6%), a heavy pill burden (22.5%), and side effects (17.3%). |
| 8 | IIoh, et al., 2013 [15] | Nigeria (Lower-middle-income) | 140 adults with primary HTN on treatment for at least six months. | 35% had their BP controlled, and 42.9% were adherent. Adherence, HTN duration (≥3 years), and receiving > one anti-HTN therapy were related to better blood pressure control. |
| 9 | Sarfo, et al., 2018 [16] | Ghana (Lower-middle-income) | 2870 hypertensive participants enrolled at five different hospitals. | 42.3% had their BP controlled. Uncontrolled BP was attributed to receiving therapy at a tertiary care level, longer HTN duration, poor adherence, and number of and access to anti-HTN treatments. |
| 10 | Harrison, et al., 2021 [17] | Ghana (Lower-middle-income) | 310 hypertensive participants | 41.8% had their BP controlled. Affordability (OR, 1.917; 95% CI: 1.013–3.630) and accessibility (OR, 1.642; 95% CI, 0.843–3.201) were more significantly linked to blood pressure control. |
| 11 | Gala, et al., 2020 [28] | Botswana (Upper-middle-income) | 280 adult patients with HTN on medications. | 45% had their BP controlled. 34% had ≥ one medication error. Having ≥ one medication error was significantly associated with uncontrolled HTN compared with no errors. |
| 12 | Devkota, et al., 2016 [18] | Nepal (Lower-middle-income) | 191 hypertensive patients. | 24% had their BP controlled, while 61.8% and 78.8% were aware and treated, respectively. BP control was associated with combination therapy, medication adherence, follow-up care, and healthcare providers’ counselling |
| 13 | Dhungana, et al., 2022 [19] | Nepal (Lower-middle-income) | 2792 hypertensive patients. | Only 3.8% had their BP controlled. About 10.3% received antihypertensive treatment. 20% were aware of their hypertension. |
| 14 | Son, et al., 2012 [20] | Vietnam (Lower-middle-income) | 2467 hypertensive patients. | Only 10.7% had their BP controlled. About 29.6% received antihypertensive treatment. 48.4% were aware of their hypertension. |
| 15 | De Souza, et al., 2014 [27] | Brazil (Upper-middle-income) | 383 adult patients with HTN. | 33.7% had their BP controlled. Only 54.3% reported adherence to anti-HTN therapy. Diabetes mellitus (DM) was observed in 31% of participants, with only 15.7% having their BP controlled. |
| 16 | Lerner, et al., 2013 [30] | Peru (Upper-middle-income) | 205 hypertensive patients. | 4.9% had their BP controlled, while 48.3% and 40% were aware and treated, respectively. Women were more aware of their HTN than men. |
| 17 | Nassr, et al., 2019 [29] | Iraq (Upper-middle-income) | 300 adult patients with hypertension. | 38.7% had their BP controlled. Age < 60 years, male gender, and diabetes were predictors of uncontrolled BP. |
| 18 | Wang, et al., 2013 [21] | China (Upper-middle-income) | 556 hypertensive patients from a rural community. | 12.5% had their BP controlled among only 429 patients aware of being hypertensive. Optimal HTN control was hindered by inadequate knowledge (82.8%), treatment cost (39.4%), poor medication adherence (65%), and lack of counselling sessions (95.1%). |
| 19 | Li, et al., 2016 [22] | China (Upper-middle-income) | 31,694 adult respondents were diagnosed with HTN. | 29.5% had their BP controlled. Higher BP levels positively correlate with the number of risk factors in both genders. |
| 20 | Xu, et al., 2013 [23] | China (Upper-middle-income) | 3279 HTN and CHD patients. | 18% had their BP controlled. Non-dihydropyridine CCB was associated with a low BP control rate. Independent factors of poor BP control include being overweight, stable angina pectoris, and a family history of diabetes. |
| 21 | Chen, et al., 2020 [24] | China (Upper-middle-income) | 89,925 hypertensive patients. | 25.4% had their BP controlled. Lower odds of uncontrolled BP were reported in women, those with diabetes, and CHD. Older patients, current smokers, and monotherapy users had higher odds of uncontrolled BP. |
| 22 | Lei wu, et al., 2015 [25] | China (Upper-middle-income) | 1409 elderly (≥60 years) with hypertension. | 30.3% had their BP controlled, while 74.5% and 63.7% were aware and treated, respectively. BP control was significantly associated with higher education levels, family history of HTN, and CVD comorbidity. |
| 23 | Xia, et al., 2021 [26] | China (Upper-middle-income) | 1046 hypertensive patients. | 48.3% and 37.6% had their BP controlled in public vs. private clinics. Higher treatment (87.5% vs. 66.8%), higher adherence (91.5% vs. 82.5%), and lower depression levels (8.5% vs. 18.2%) in public vs. private clinics. |
| 24 | Santosa, et al., 2020 [32] | Sweden and China (High-income “Sweden”) | Sweden (n = 25,511) and China (n = 25,356). | 47.6% of males and 58.7% of females had their BP controlled in Sweden vs. 33.2% and 37.6% in China. Awareness was higher among patients in Sweden (63.7%” males” and 69.1% “females”) compared to China (50.2%” males” and 44.3% “females”). Higher odds of BP control in Sweden were reported for those with normal weight, controlled lipid profiles, and men with diabetes. |
| 25 | Ting li, et al., 2016 [33] | Hong Kong (High-income) | 2445 hypertensive patients. | 51.3% had their BP controlled, 53.4% had good adherence, and 47.4% had multiple comorbidities. Poor BP control was more likely among those with multiple comorbidities (Diabetes was the most prevalent). |
| 26 | Liew, et al., 2019 [40] | Singapore (High-income) | 10 215 participants from a multi-ethnic cohort. | 37.6% had their BP controlled. Older age was associated with uncontrolled HTN. Younger age, male gender, and lower educational level were associated with untreated HTN. |
| 27 | Ham, et al., 2011 [36] | South Korea (High-income) | 690 adult patients with HTN on medications. | 54.3% had their BP controlled. Higher control rates were observed at a younger age, for those with ≥one comorbidity, and ≥4 days physically active. Being overweight, heavy alcohol consumption, and mild to severe stress reduced BP control. |
| 28 | Khayyat, et al., 2017 [34] | Saudi Arabia (High-income) | 204 hypertensive patients. | 69.6% had their BP controlled. Higher odds were observed with high medication adherence and normal-weight individuals. 46% were adherent. Higher odds were observed among males, older individuals (>65 yrs), and patients with diabetes. |
| 29 | Sandoval, et al., 2012 [35] | Chile (High-income) | 1194 hypertensive patients. | 59.7% had their BP controlled. Women and non-diabetics had better BP control than men and diabetics |
| 30 | Zhang, et al., 2019 [31] | Australia (High-income) | 1750 CKD patients with HTN. | 36.3% had their BP controlled. Those with CVD had lower odds of uncontrolled BP. Participants ≥65 years old and those with severe albuminuria or proteinuria were at higher odds of uncontrolled BP. |
| 31 | Murphy, et al., 2016 [39] | Ireland (High-income) | 3579 hypertensive adults aged over 50 years. | 54.5% and 58.9% were aware and treated (affected by financial barriers). Among those treated, 51.6% had their BP controlled. Higher odds of BP control were observed among those with previous CVD history and those living in rural areas compared with a country area. |
| 32 | Tiffe, et al., 2019 [37] | Germany (High-income) | 293 adult patients with HTN on medications. | 50.2% had their BP controlled. Women who reported higher levels of concern had a higher chance of controlling HTN. |
| 33 | Cordero, et al., 2011 [38] | Spain (High-income) | 10743 patients with HTN. | 55.4% had their BP controlled. BP control rate was similar in those with and without CVD. Higher rates of poor BP control were reported for males, active smokers, obese individuals, and diabetics. |
| N | Barriers to Hypertension Control | Examples of Individual Barriers | |
|---|---|---|---|
| 1 | Patient-related | Sociodemographic factors | Age: Older age is a strong predictor of uncontrolled HTN |
| Gender: The role of gender depends on age and health conditions, such as menopause. | |||
| Socioeconomic status: Socioeconomically underprivileged patients are more prone to suboptimal BP levels despite treatment | |||
| Geographical area: Patients residing in rural areas are more prone to having poor BP control | |||
| Comorbidities | Diabetes: One of the strong predictors of uncontrolled HTN | ||
| Coronary artery disease | |||
| Chronic kidney disease: Patients with severe albuminuria or proteinuria are at greater risk | |||
| Depression: This shows that mental health can also influence BP control | |||
| Hyperlipidemia | |||
| Hyperuricaemia | |||
| 2 | Medication nonadherence | Forgetfulness: The most reported reason | |
| Financial barrier | |||
| High pill burden | |||
| Side effects of antihypertensive agents | |||
| Low measured BP | |||
| 3 | Lifestyle-related | Smoking | |
| Obesity | |||
| Salt intake | |||
| Alcohol intake | |||
| Stress | |||
| Physical inactivity | |||
| 4 | Affordability and accessibility-related barriers | Direct cost of treatment | |
| Cost associated with access to care | |||
| Cost associated with regular follow-up | |||
| 5 | Awareness-related barriers | Disease-related knowledge | |
| Health literacy regarding risk factors | |||
| 6 | Pharmacotherapy-related | Number of used antihypertensive agents | |
| Choice of antihypertensive agents | |||
| Duration of taking antihypertensive agents | |||
| Medication error avoidance | |||
| Barriers to Hypertension Control | LMIC Studies (N = 23) | HIC Studies (N = 10) | Total |
|---|---|---|---|
| Patient-related barriers | 10 | 10 | 20 |
| Medication adherence barriers | 9 | 1 | 10 |
| Lifestyle-related barriers | 6 | 2 | 8 |
| Affordability and accessibility-related barriers | 7 | 1 | 8 |
| Awareness-related barriers | 6 | 1 | 7 |
| Pharmacotherapy-related barriers | 6 | 0 | 6 |
| Total no. of barriers | 44 | 15 | 59 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elnaem, M.H.; Mosaad, M.; Abdelaziz, D.H.; Mansour, N.O.; Usman, A.; Elrggal, M.E.; Cheema, E. Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14571. https://doi.org/10.3390/ijerph192114571
Elnaem MH, Mosaad M, Abdelaziz DH, Mansour NO, Usman A, Elrggal ME, Cheema E. Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(21):14571. https://doi.org/10.3390/ijerph192114571
Chicago/Turabian StyleElnaem, Mohamed Hassan, Manar Mosaad, Doaa H Abdelaziz, Noha O. Mansour, Abubakar Usman, Mahmoud E. Elrggal, and Ejaz Cheema. 2022. "Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 21: 14571. https://doi.org/10.3390/ijerph192114571
APA StyleElnaem, M. H., Mosaad, M., Abdelaziz, D. H., Mansour, N. O., Usman, A., Elrggal, M. E., & Cheema, E. (2022). Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review. International Journal of Environmental Research and Public Health, 19(21), 14571. https://doi.org/10.3390/ijerph192114571







