The Intra- and Inter-Rater Reliability of a Variety of Testing Methods to Measure Shoulder Range of Motion, Hand-behind-Back and External Rotation Strength in Healthy Participants
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Raters
2.3. Instruments
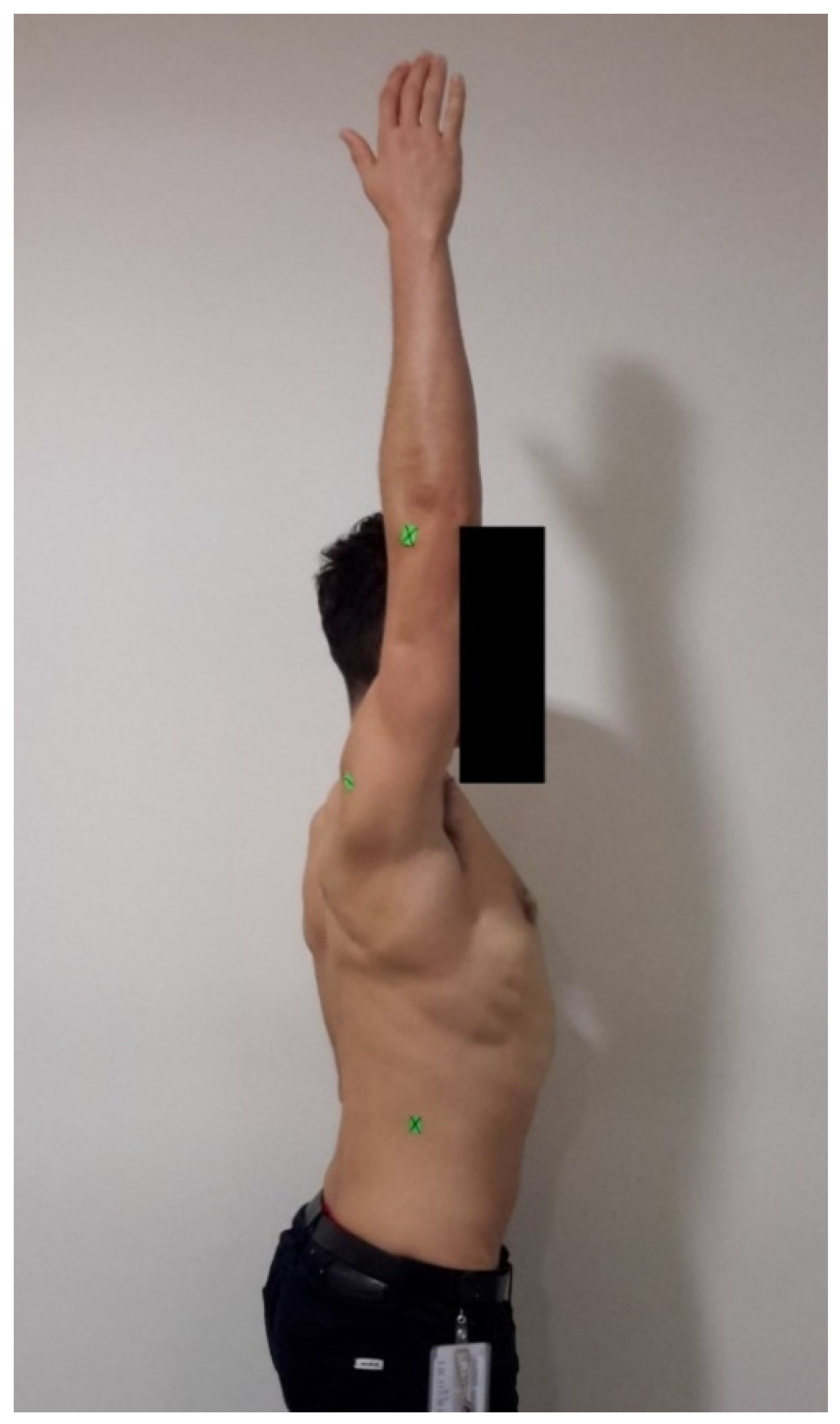
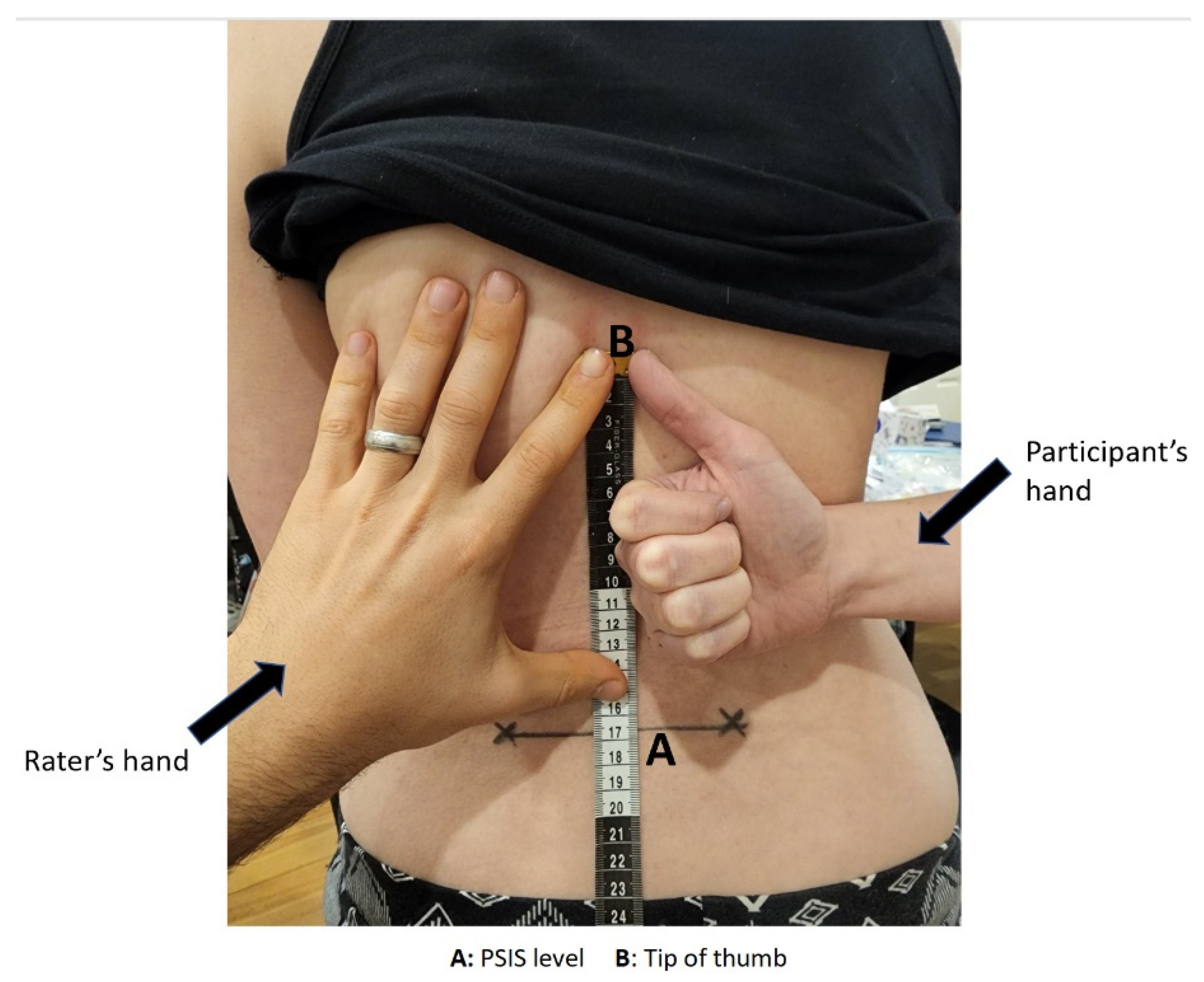
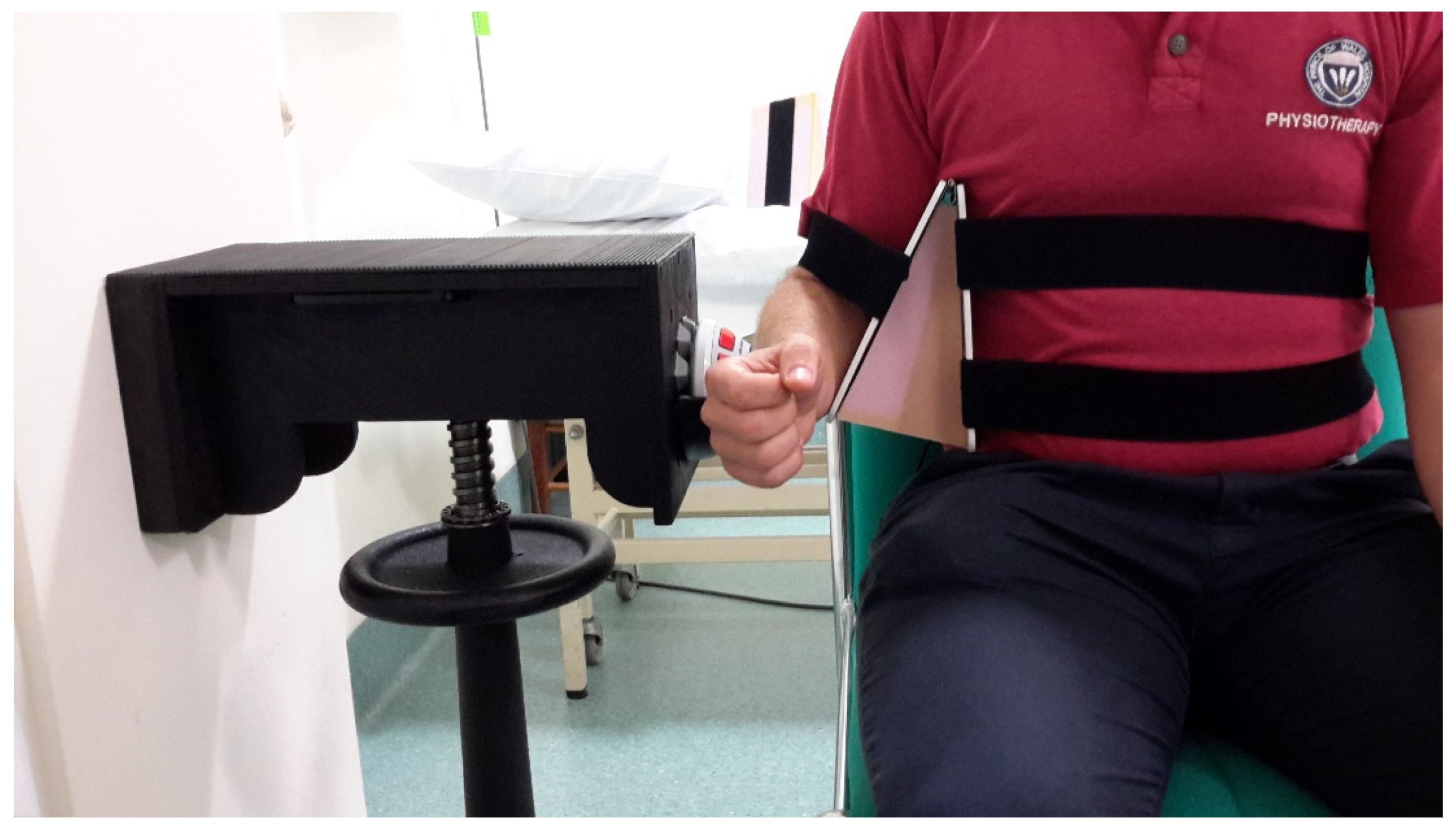
2.4. Procedures
2.5. Statistical Analysis
3. Results
3.1. Intra-Rater Reliability
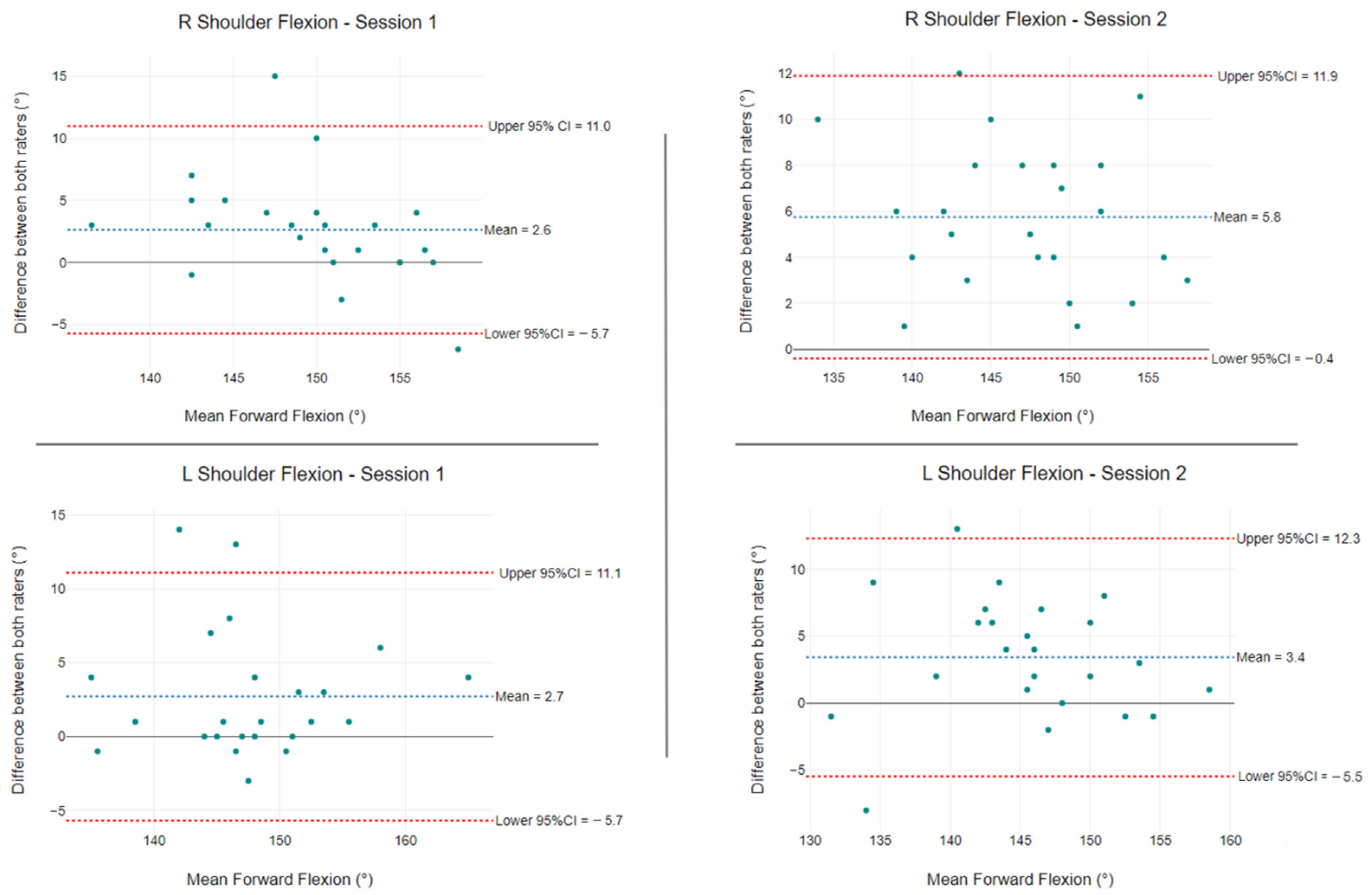
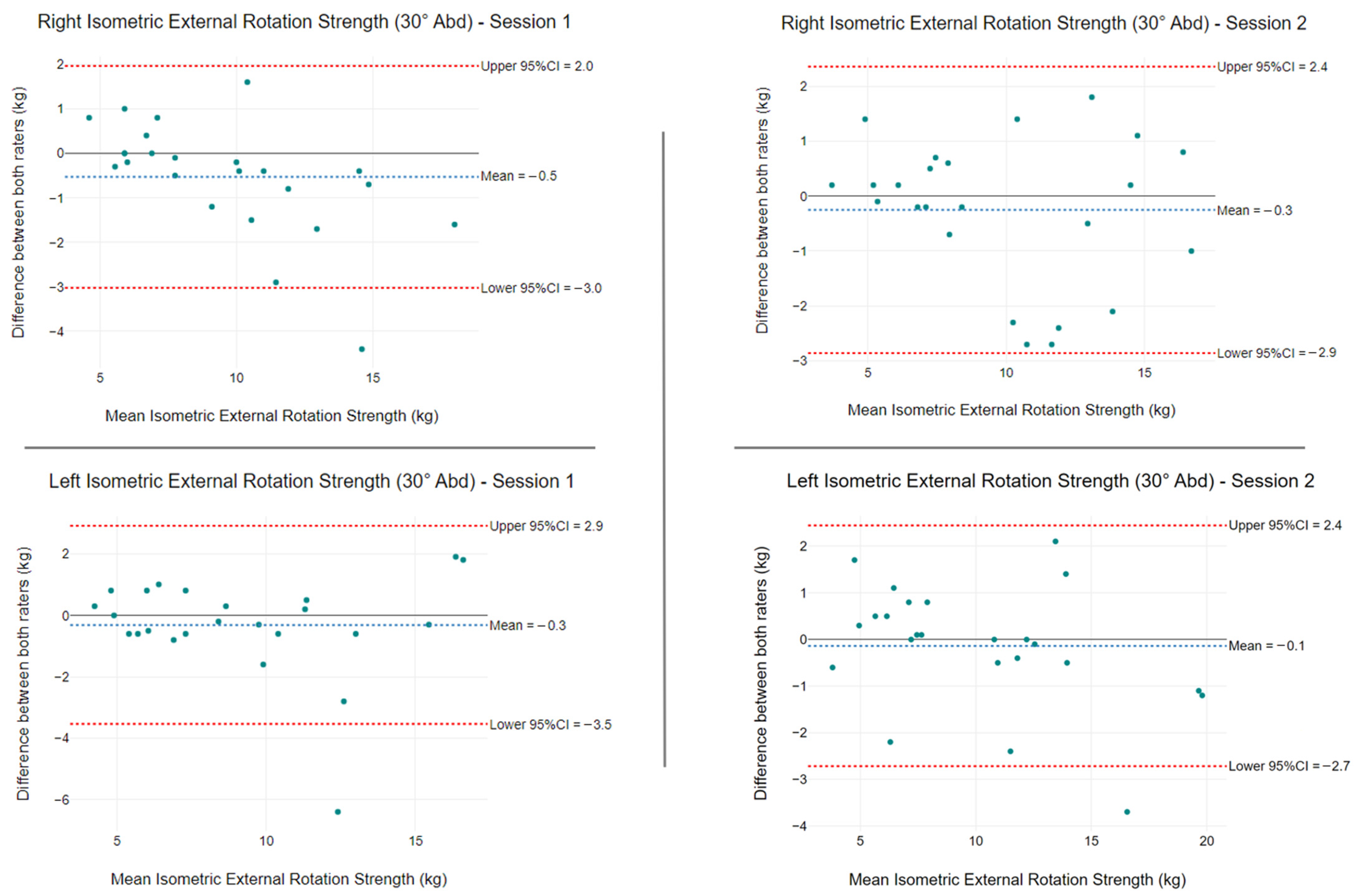
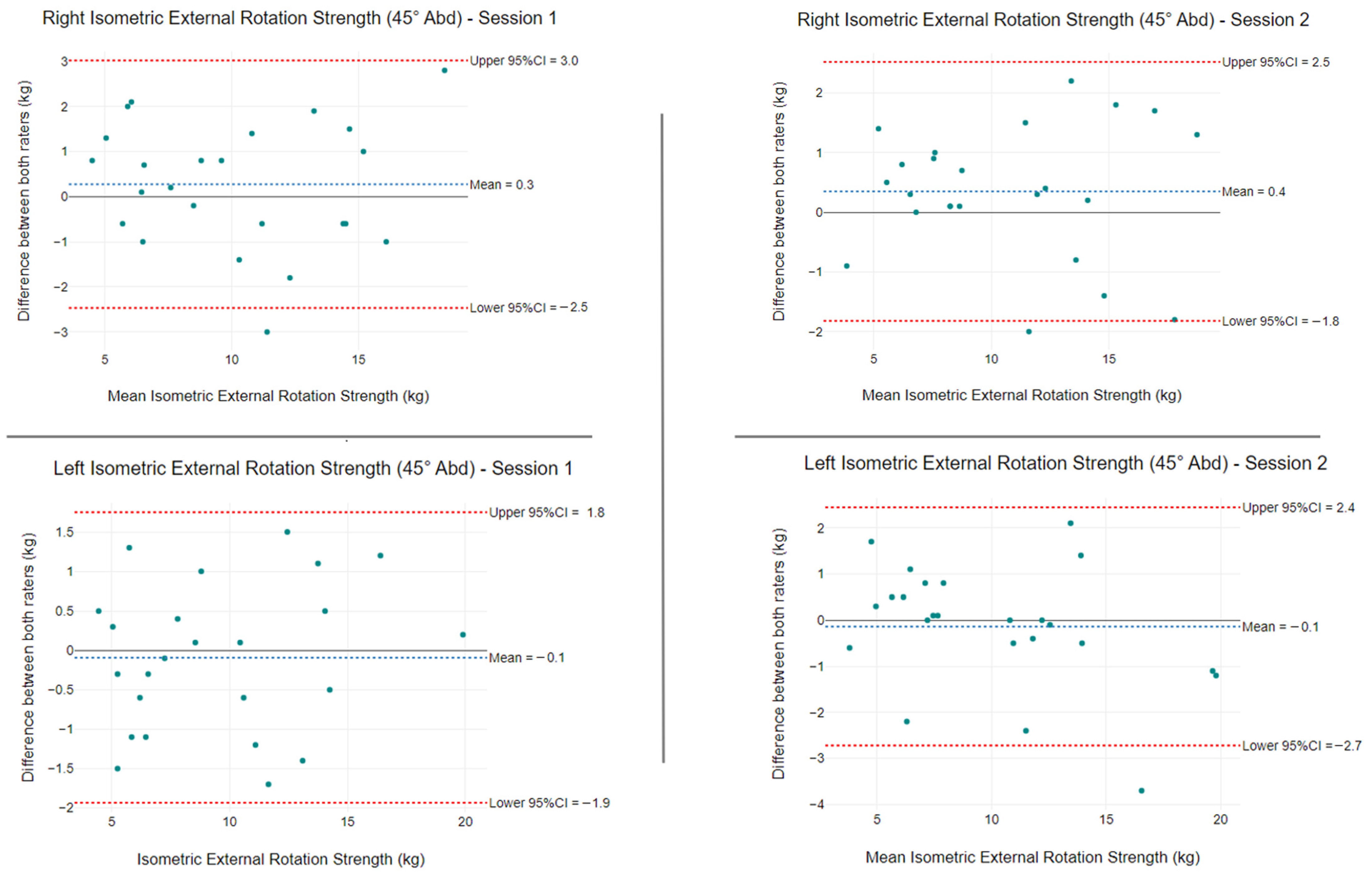
3.2. Inter-Rater Reliability
3.3. Comparisons between the Nominant and Non-Dominant Arm
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A Practical Guide to Their Development and Use, 4th ed.; Oxford University Press: Oxford, UK, 2008; pp. 5–16. [Google Scholar]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: A systematic review. PM&R 2011, 3, 472–479. [Google Scholar] [CrossRef]
- Gajdosik, R.L.; Bohannon, R.W. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys. Ther. 1987, 67, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Reese, N.; Bandy, W. Joint Range of Movement and Muscle Testing, 1st ed.; WB Saunders: Philadelphia, PA, USA, 2002; pp. 3–29. [Google Scholar]
- Boone, D.C.; Azen, S.P.; Lin, C.M.; Spence, C.; Baron, C.; Lee, L. Reliability of goniometric measurements. Phys. Ther. 1978, 58, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; de Winter, A.F.; Scholten, R.J.; Jans, M.P.; Devillé, W.; van Schaardenburg, D.; Bouter, L.M. Interobserver reproducibility of the visual estimation of range of motion of the shoulder. Arch. Phys. Med. Rehabil. 2005, 86, 1356–1361. [Google Scholar] [CrossRef]
- Croft, P.; Pope, D.; Boswell, R.; Rigby, A.; Silman, A. Observer variability in measuring elevation and external rotation of the shoulder. Primary Care Rheumatology Society Shoulder Study Group. Br. J. Rheumatol. 1994, 33, 942–946. [Google Scholar] [CrossRef]
- Kolber, M.J.; Vega, F.; Widmayer, K.; Cheng, M.S. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother. Theory Pract. 2011, 27, 176–184. [Google Scholar] [CrossRef]
- Green, S.; Buchbinder, R.; Forbes, A.; Bellamy, N. A standardized protocol for measurement of range of movement of the shoulder using the Plurimeter-V inclinometer and assessment of its intrarater and interrater reliability. Arthritis Care Res. 1998, 1, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Nadeau, S.; Kovacs, S.; Gravel, D.; Piotte, F.; Moffet, H.; Gagnon, D.; Hébert, L.J. Active movement measurements of the shoulder girdle in healthy subjects with goniometer and tape measure techniques: A study on reliability and validity. Physiother. Theory Pract. 2007, 23, 179–187. [Google Scholar] [CrossRef]
- Han, S.H.; Oh, K.S.; Han, K.J.; Jo, J.; Lee, D.H. Accuracy of measuring tape and vertebral-level methods to determine shoulder internal rotation. Clin. Orthop. Relat. Res. 2012, 470, 562–566. [Google Scholar] [CrossRef]
- Ginn, K.A.; Herbert, R.D.; Khouw, W.; Lee, R. A randomized, controlled clinical trial of a treatment for shoulder pain. Phys. Ther. 1997, 77, 802–811. [Google Scholar] [CrossRef]
- Chen, J.F.; Ginn, K.A.; Herbert, R.D. Passive mobilisation of shoulder region joints plus advice and exercise does not reduce pain and disability more than advice and exercise alone: A randomised trial. Aust. J. Physiother. 2009, 55, 17–23. [Google Scholar] [CrossRef]
- Rajkumar, A.; Vulpi, F.; Bethi, S.R.; Wazir, H.K.; Raghavan, P.; Kapila, V. Wearable Inertial Sensors for Range of Motion Assessment. IEEE Sens. J. 2020, 20, 3777–3787. [Google Scholar] [CrossRef] [PubMed]
- Rigoni, M.; Gill, S.; Babazadeh, S.; Elsewaisy, O.; Gillies, H.; Nguyen, N.; Pathirana, P.N.; Page, R. Assessment of Shoulder Range of Motion Using a Wireless Inertial Motion Capture Device-A Validation Study. Sensors 2019, 19, 1781. [Google Scholar] [CrossRef] [PubMed]
- Werner, B.C.; Holzgrefe, R.E.; Griffin, J.W.; Lyons, M.L.; Cosgrove, C.T.; Hart, J.M.; Brockmeier, S.F. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J. Shoulder Elbow Surg. 2014, 23, e275–e282. [Google Scholar] [CrossRef]
- Shin, S.H.; Ro du, H.; Lee, O.S.; Oh, J.H.; Kim, S.H. Within-day reliability of shoulder range of motion measurement with a smartphone. Man Ther. 2012, 17, 298–304. [Google Scholar] [CrossRef]
- Wilson, J.D.; Khan-Perez, J.; Marley, D.; Buttress, S.; Walton, M.; Li, B.; Roy, B. Can shoulder range of movement be measured accurately using the Microsoft Kinect sensor plus Medical Interactive Recovery Assistant (MIRA) software? J. Shoulder Elbow Surg. 2017, 26, e382–e389. [Google Scholar] [CrossRef]
- Overbeek, C.L.; Geurkink, T.H.; de Groot, F.A.; Klop, I.; Nagels, J.; Nelissen, R.G.; de Groot, J.H. Shoulder movement complexity in the aging shoulder: A cross-sectional analysis and reliability assessment. J. Orthop. Res. 2021, 39, 2217–2225. [Google Scholar] [CrossRef]
- Wilk, K.E.; Reinold, M.M.; Macrina, L.C.; Porterfield, R.; Devine, K.M.; Suarez, K.; Andrews, J.R. Glenohumeral internal rotation measurements differ depending on stabilization techniques. Sports Health 2009, 1, 131–136. [Google Scholar] [CrossRef]
- Hayes, K.; Walton, J.R.; Szomor, Z.R.; Murrell, G.A. Reliability of five methods for assessing shoulder range of motion. Aust. J. Physiother. 2001, 47, 289–294. [Google Scholar] [CrossRef]
- Crasto, J.A.; Sayari, A.J.; Gray, R.R.; Askari, M. Comparative analysis of photograph-based clinical goniometry to standard techniques. Hand 2015, 10, 248–253. [Google Scholar] [CrossRef]
- Blonna, D.; Zarkadas, P.C.; Fitzsimmons, J.S.; O’Driscoll, S.W. Validation of a photography-based goniometry method for measuring joint range of motion. J. Shoulder Elbow Surg. 2012, 21, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; Roldán-Jiménez, C. Validity and reliability of arm abduction angle measured on smartphone: A cross-sectional study. BMC Musculoskelet. Disord. 2016, 17, 93. [Google Scholar] [CrossRef] [PubMed]
- Russo, R.R.; Burn, M.B.; Ismaily, S.K.; Gerrie, B.J.; Han, S.; Alexander, J.; Lenherr, C.; Noble, P.C.; Harris, J.D.; McCulloch, P.C. Is digital photography an accurate and precise method for measuring range of motion of the shoulder and elbow? J. Orthop. Sci. 2018, 23, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Edwards, T.B.; Bostick, R.D.; Greene, C.C.; Baratta, R.V.; Drez, D. Interobserver and intraobserver reliability of the measurement of shoulder internal rotation by vertebral level. J. Shoulder Elbow Surg. 2002, 11, 40–42. [Google Scholar] [CrossRef]
- Hoving, J.L.; Buchbinder, R.; Green, S.; Forbes, A.; Bellamy, N.; Brand, C.; Buchanan, R.; Hall, S.; Patrick, M.; Ryan, P.; et al. How reliably do rheumatologists measure shoulder movement? Ann. Rheum. Dis. 2002, 61, 612–616. [Google Scholar] [CrossRef]
- Van den Dolder, P.A.; Roberts, D.L. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust. J. Physiother. 2003, 49, 183–188. [Google Scholar] [CrossRef]
- van den Dolder, P.A.; Ferreira, P.H.; Refshauge, K. Intra- and inter-rater reliability of a modified measure of hand behind back range of motion. Man Ther. 2014, 19, 72–76. [Google Scholar] [CrossRef]
- Hislop, H.J.; Montgomery, J. Daniels & Worthingham's Muscle Testing: Techniques of Manual Examination; Saunders Elsevier: St. Louis, MO, USA, 2007. [Google Scholar]
- Nagatomi, T.; Mae, T.; Nagafuchi, T.; Yamada, S.I.; Nagai, K.; Yoneda, M. Shoulder manual muscle resistance test cannot fully detect muscle weakness. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2081–2088. [Google Scholar] [CrossRef]
- Hayes, K.; Walton, J.R.; Szomor, Z.L.; Murrell, G.A. Reliability of 3 methods for assessing shoulder strength. J. Shoulder Elbow Surg. 2002, 11, 33–39. [Google Scholar] [CrossRef]
- Karabay, D.; Yesilyaprak, S.S.; Sahiner Picak, G. Reliability and validity of eccentric strength measurement of the shoulder abductor muscles using a hand-held dynamometer. Phys. Ther. Sport 2020, 43, 52–57. [Google Scholar] [CrossRef]
- Johansson, F.R.; Skillgate, E.; Lapauw, M.L.; Clijmans, D.; Deneulin, V.P.; Palmans, T.; Engineer, H.K.; Cools, A.M. Measuring Eccentric Strength of the Shoulder External Rotators Using a Handheld Dynamometer: Reliability and Validity. J. Athl. Train. 2015, 50, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, S.J.; Chesley, A.; Hebert, G.; McFaull, S.; Scullion, D. The validity and reliability of hand-held dynamometry in assessing isometric external rotator performance. J. Orthop. Sports Phys. Ther. 1988, 10, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Holt, K.L.; Raper, D.P.; Boettcher, C.E.; Waddington, G.S.; Drew, M.K. Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Phys. Ther. Sport 2016, 21, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Wikholm, J.B.; Bohannon, R.W. Hand-held dynamometer measurements: Tester strength makes a difference. J. Orthop. Sport. Phys. Ther. 1991, 13, 191–198. [Google Scholar] [CrossRef]
- Stone, C.A.; Nolan, B.; Lawlor, P.G.; Kenny, R.A. Hand-held dynamometry: Tester strength is paramount, even in frail populations. J. Rehabil. Med. 2011, 43, 808–810. [Google Scholar] [CrossRef]
- Wadsworth, C.T.; Krishnan, R.; Sear, M.; Harrold, J.; Nielsen, D.H. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys. Ther. 1987, 67, 1342–1347. [Google Scholar] [CrossRef]
- Reed, R.L.; Den Hartog, R.; Yochum, K.; Pearlmutter, L.; Ruttinger, A.C.; Mooradian, A.D. A comparison of hand-held isometric strength measurement with isokinetic muscle strength measurement in the elderly. J. Am. Geriatr. Soc. 1993, 41, 53–56. [Google Scholar] [CrossRef]
- Agre, J.C.; Magness, J.L.; Hull, S.Z.; Wright, K.C.; Baxter, T.L.; Patterson, R.; Stradel, L. Strength testing with a portable dynamometer: Reliability for upper and lower extremities. Arch. Phys. Med. Rehabil. 1987, 68, 454–458. [Google Scholar]
- Wang, C.Y.; Olson, S.L.; Protas, E.J. Test-retest strength reliability: Hand-held dynamometry in community-dwelling elderly fallers. Arch. Phys. Med. Rehabil. 2002, 83, 811–815. [Google Scholar] [CrossRef]
- Kolber, M.J.; Beekhuizen, K.; Cheng, M.S.; Fiebert, I.M. The reliability of hand-held dynamometry in measuring isometric strength of the shoulder internal and external rotator musculature using a stabilization device. Physiother. Theory Pract. 2007, 23, 119–124. [Google Scholar] [CrossRef]
- Makhni, E.C.; Steinhaus, M.E.; Morrow, Z.S.; Jobin, C.M.; Verma, N.N.; Cole, B.J.; Bach, B.R., Jr. Outcomes assessment in rotator cuff pathology: What are we measuring? J. Shoulder Elbow Surg. 2015, 24, 2008–2015. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 1, 101–110. [Google Scholar] [CrossRef]
- De Vet, H.C.; Terwee, C.B.; Knol, D.L.; Bouter, L.M. When to use agreement versus reliability measures. J. Clin. Epidemiol. 2006, 59, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; F.A. Davis Company: Philadelphia, PA, USA, 2015. [Google Scholar]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- De Winter, A.F.; Heemskerk, M.A.; Terwee, C.B.; Jans, M.P.; Devillé, W.; van Schaardenburg, D.J.; Scholten, R.J.; Bouter, L.M. Inter-observer reproducibility of measurements of range of motion in patients with shoulder pain using a digital inclinometer. BMC Musculoskelet. Disord. 2004, 5, 18. [Google Scholar] [CrossRef]
- Greenfield, B.H.; Donatelli, R.; Wooden, M.J.; Wilkes, J. Isokinetic evaluation of shoulder rotational strength between the plane of scapula and the frontal plane. Am. J. Sports Med. 1990, 18, 124–128. [Google Scholar] [CrossRef]
- Rathbun, J.; Macnab, I. The microvascular pattern of the rotator cuff. J. Bone Jt. Surg. 1970, 52, 540–553. [Google Scholar] [CrossRef]
- Poppen, N.; Walker, P.S. Forces at the glenohumeral joint in abduction. Clin. Orthop. 1978, 135, 165–170. [Google Scholar] [CrossRef]
- Edouard, P.; Samozino, P.; Julia, M.; Gleizes Cervera, S.; Vanbiervliet, W.; Calmels, P.; Gremeaux, V. Reliability of isokinetic assessment of shoulder-rotator strength: A systematic review of the effect of position. J. Sport Rehabil. 2011, 20, 367–383. [Google Scholar] [CrossRef]
- Schrama, P.P.; Stenneberg, M.S.; Lucas, C.; van Trijffel, E. Intraexaminer reliability of hand-held dynamometry in the upper extremity: A systematic review. Arch. Phys. Med. Rehabil. 2014, 12, 2444–2469. [Google Scholar] [CrossRef] [PubMed]
- Mullaney, M.J.; McHugh, M.P.; Johnson, C.P.; Tyler, T.F. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother. Theory Pract. 2010, 5, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Correll, S.; Field, J.; Hutchinson, H.; Mickevicius, G.; Fitzsimmons, A.; Smoot, B. Reliability and validity of the halo digital goniometer for shoulder range of motion in healthy subjects. Int. J. Sports Phys. Ther. 2018, 4, 707–714. [Google Scholar] [CrossRef]
- Muir, S.W.; Corea, C.L.; Beaupre, L. Evaluating change in clinical status: Reliability and measures of agreement for the assessment of glenohumeral range of motion. N. Am. J. Sports Phys. Ther. 2010, 3, 98–110. [Google Scholar]
- Shimizu, H.; Saito, T.; Kouno, C.; Shimoura, K.; Kawabe, R.; Shinohara, Y.; Mukaiyama, K.; Changyu, C.; Kato, M.; Nagai-Tanima, M.; et al. Validity and reliability of a smartphone application for self-measurement of active shoulder range of motion in a standing position among healthy adults. JSES Int. 2022, 6, 655–659. [Google Scholar] [CrossRef]
- Lin, Y.C.; Tsai, Y.J.; Hsu, Y.L.; Yen, M.H.; Wang, J.S. Assessment of Shoulder Range of Motion Using a Wearable Inertial Sensor Network. IEEE Sens. J. 2021, 21, 15330–15341. [Google Scholar] [CrossRef]
- Özsoy, U.; Yıldırım, Y.; Karaşin, S.; Şekerci, R.; Süzen, L.B. Reliability and agreement of Azure Kinect and Kinect v2 depth sensors in the shoulder joint ROM estimation. J Shoulder Elbow Surg. 2022, 31, 2049–2056. [Google Scholar] [CrossRef]
- Fryer, G.; McPherson, H.C.; O’Keefe, P. The effect of training on the inter-examiner and intra-examiner reliability of the seated flexion test and assessment of pelvic anatomical landmarks with palpation. Int. J. Osteopath. Med. 2005, 8, 131–138. [Google Scholar] [CrossRef]


| Characteristics | Mean (SD) or Frequency (%) |
|---|---|
| Age (years) | 31.2 (10.9) |
| BMI (kg/m2) | 23.5 (2.4) |
| Sex | |
| Male | 12 (50%) |
| Female | 12 (50%) |
| Hand dominance | |
| Right | 20 (83%) |
| Left | 4 (17%) |
| Rater A | Rater B | |||||
|---|---|---|---|---|---|---|
| Type of Measurement | ICC (95% CI) | SEM | MDC | ICC (95% CI) | SEM | MDC |
| Shoulder ROM | ||||||
| Photography | ||||||
| Forward Flexion (°) | 0.86 (0.73–0.92) | 2.4 | 5.5 | 0.76 (0.43–0.88) | 3.5 | 8.3 |
| Tape Measure | ||||||
| HBB (cm) | 0.96 (0.93–0.98) | 1.0 | 2.3 | 0.94 (0.88–0.97) | 1.2 | 2.7 |
| Shoulder strength | ||||||
| HHD | ||||||
| ER 30° Abd (kg) | 0.97 (0.96–0.98) | 0.7 | 1.7 | 0.96 (0.93–0.98) | 0.8 | 1.8 |
| ER 45° Abd (kg) | 0.97 (0.94–0.98) | 0.4 | 0.8 | 0.98 (0.95–0.99) | 1.1 | 2.5 |
| Type of Measurement | Rater A | Rater B | ||
|---|---|---|---|---|
| Session 1 | Session 2 | Session 1 | Session 2 | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Shoulder ROM | ||||
| Forward Flexion (°) | 150.0 (6.1) | 148.5 (6.5) | 147.4 (6.9) | 143.9 (6.7) |
| HBB (cm) | 37.1 (5.3) | 37.3 (4.6) | 38.7 (4.9) | 39.5 (4.7) |
| Shoulder strength | ||||
| ER 30° Abd (kg) | 9.2 (3.5) | 9.7 (4.0) | 9.6 (3.9) | 9.8 (3.9) |
| ER 45° Abd (kg) | 9.9 (4.1) | 10.4 (4.3) | 15.7 (9.0) | 10.3 (4.5) |
| Type of Measurement | ICC (95% CI) | SEM | MDC |
|---|---|---|---|
| Shoulder ROM | |||
| Photography | |||
| Forward Flexion (°) | 0.75 (0.40–0.88) | 1.3 | 2.0 |
| Tape measure | |||
| HBB (cm) | 0.91 (0.61–0.96) | 0.7 | 1.0 |
| Shoulder strength | |||
| HHD | |||
| ER 30° Abd (kg) | 0.97 (0.95–0.98) | 0.3 | 0.5 |
| ER 45° Abd (kg) | 0.98 (0.97–0.99) | 0.6 | 1.4 |
| Rater A Measurements | Dominant Arm | Non Dominant Arm | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean Diff | p-Value | |
| Forward Flexion (°) | 150.1 (5.4) | 148.4 (7.1) | 1.6 | 0.057 |
| HBB (cm) | 36.0 (4.5) | 38.2 (5.5) | −2.2 | <0.001 * |
| ER 30° Abd (kg) | 9.6 (3.7) | 9.3 (3.8) | 0.3 | 0.078 |
| ER 45° Abd (kg) | 10.5 (4.3) | 9.8 (4.1) | 0.7 | <0.001 * |
| Rater B measurements | Dominant Arm | Non Dominant Arm | ||
| Mean (SD) | Mean (SD) | Mean Diff | p-Value | |
| Forward Flexion (°) | 146.1 (6.7) | 145.2 (7.1) | 0.9 | 0.143 |
| HBB (cm) | 37.8 (4.3) | 40.4 (4.9) | 2.7 | <0.001 * |
| ER 30° Abd (kg) | 10.0 (3.9) | 9.4 (3.9) | 0.7 | <0.001 * |
| ER 45° Abd (kg) | 10.3 (4.4) | 9.8 (4.2) | 0.5 | <0.011 * |
| Type of Measurement | Rater A | Rater B | ||
|---|---|---|---|---|
| Session 1 | Session 2 | Session 1 | Session 2 | |
| n (%) | n (%) | n (%) | n (%) | |
| Peak Forward Flexion (°) | ||||
| Dominant arm highest | 12 (50) | 14 (58) | 14 (58) | 13 (54) |
| Non-dominant arm highest | 11 (46) | 8 (33) | 8 (33) | 11 (46) |
| Equal | 1 (4) | 2 (8) | 2 (8) | 0 (0) |
| Peak Hand-Behind-Back (cm) | ||||
| Dominant arm highest | 18 (75) | 18 (75) | 22 (75) | 18 (75) |
| Non-dominant arm highest | 6 (25) | 6 (25) | 6 (25) | 5 (21) |
| Equal | 0 (0) | 0 (0) | 1 (4) | 1 (4) |
| Peak ER strength at 30° Abd (kg) | ||||
| Dominant arm highest | 15 (63) | 14 (58) | 18 (75) | 19 (80) |
| Non-dominant arm highest | 8 (33) | 10 (42) | 6 (25) | 4 (17) |
| Equal | 1 (4) | 0 (0) | 0 (0) | 1 (4) |
| Peak ER strength at 45° Abd (kg) | ||||
| Dominant arm highest | 17 (71) | 16 (67) | 17 (71) | 14 (58) |
| Non-dominant arm highest | 7 (29) | 7 (29) | 7 (29) | 10 (42) |
| Equal | 0 (0) | 1 (4) | 0 (0) | 0 (0) |
| Peak ER strength (at 30° and 45° Abd) (kg) | ||||
| Dominant arm highest | 13 (54) | 11 (46) | 12 (50) | 12 (50) |
| Non-dominant arm highest | 4 (17) | 5 (21) | 1 (4) | 3 (13) |
| Stronger in different arms | 7 (29) | 8 (33) | 11 (46) | 9 (38) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beshara, P.; Davidson, I.; Pelletier, M.; Walsh, W.R. The Intra- and Inter-Rater Reliability of a Variety of Testing Methods to Measure Shoulder Range of Motion, Hand-behind-Back and External Rotation Strength in Healthy Participants. Int. J. Environ. Res. Public Health 2022, 19, 14442. https://doi.org/10.3390/ijerph192114442
Beshara P, Davidson I, Pelletier M, Walsh WR. The Intra- and Inter-Rater Reliability of a Variety of Testing Methods to Measure Shoulder Range of Motion, Hand-behind-Back and External Rotation Strength in Healthy Participants. International Journal of Environmental Research and Public Health. 2022; 19(21):14442. https://doi.org/10.3390/ijerph192114442
Chicago/Turabian StyleBeshara, Peter, Ingrid Davidson, Matthew Pelletier, and William R. Walsh. 2022. "The Intra- and Inter-Rater Reliability of a Variety of Testing Methods to Measure Shoulder Range of Motion, Hand-behind-Back and External Rotation Strength in Healthy Participants" International Journal of Environmental Research and Public Health 19, no. 21: 14442. https://doi.org/10.3390/ijerph192114442
APA StyleBeshara, P., Davidson, I., Pelletier, M., & Walsh, W. R. (2022). The Intra- and Inter-Rater Reliability of a Variety of Testing Methods to Measure Shoulder Range of Motion, Hand-behind-Back and External Rotation Strength in Healthy Participants. International Journal of Environmental Research and Public Health, 19(21), 14442. https://doi.org/10.3390/ijerph192114442







