Socioeconomic Deprivation, Sleep Duration, and Mental Health during the First Year of the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Population
2.2. Variables and Measures
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
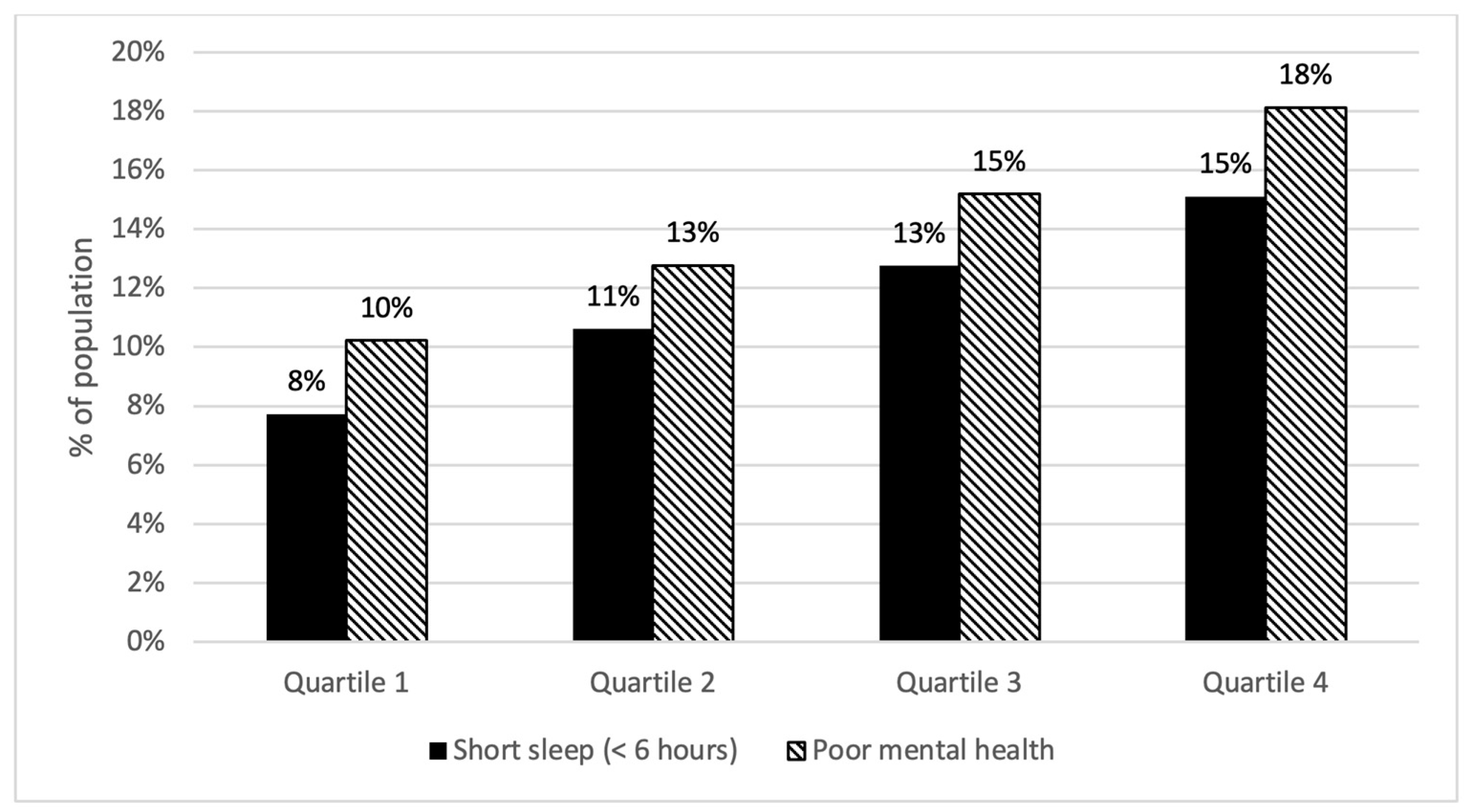
3.2. Socioeconomic Deprivation and Sleep Duration
3.3. Socioeconomic Deprivation and Mental Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethn. Health Disparities 2021, 8, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Bhowmik, T.; Tirtha, S.D.; Iraganaboina, N.C.; Eluru, N. A comprehensive analysis of COVID-19 transmission and mortality rates at the county level in the United States considering socio-demographics, health indicators, mobility trends and health care infrastructure attributes. PLoS ONE 2021, 16, e0249133. [Google Scholar] [CrossRef] [PubMed]
- Jalali, A.M.; Khoury, S.G.; See, J.; Gulsvig, A.M.; Peterson, B.M.; Gunasekera, R.S.; Buzi, G.; Wilson, J.; Galbadage, T. Delayed interventions, low compliance, and health disparities amplified the early spread of COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Robertson, L.S. Predictors of COVID-19-confirmed cases and fatalities in 883 US counties with a population of 50,000 or more: Estimated effect of initial prevention policies. J. Urban Health 2021, 98, 205–210. [Google Scholar] [CrossRef]
- Butler, D.C.; Petterson, S.; Phillips, R.L.; Bazemore, A.W. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv. Res. 2013, 48, 539–559. [Google Scholar] [CrossRef]
- Alshumrani, R.; Qanash, S.; Aldobyany, A.; Alhejaili, F.; AlQassas, I.; Shabrawishi, M.; Alnashiwaty, O.; Badghaish, M.; Adnan, M.; Afeef, A.B.; et al. Sleep quality and mental health in coronavirus disease 2019 patients and general population during the pandemic. Ann. Thorac. Med. 2022, 17, 21–27. [Google Scholar] [CrossRef]
- Singu, S.; Acharya, A.; Challagundla, K.; Byrareddy, S.N. Impact of Social Determinants of Health on the Emerging COVID-19 Pandemic in the United States. Front. Public Health 2020, 8, 406. [Google Scholar] [CrossRef]
- Tsai, J.; Wilson, M. COVID-19: A potential public health problem for homeless populations. Lancet Public Health 2020, 5, e186–e187. [Google Scholar] [CrossRef]
- Grandner, M.A. Epidemiology of insufficient sleep and poor sleep quality. In Sleep and Health; Elsevier: Amsterdam, The Netherlands, 2019; pp. 11–20. [Google Scholar]
- Jacobson, A.; Ryan, C.; Cleary, P.; Waberski, B.; Weinger, K.; Musen, G.; Dahms, W. Biomedical risk factors for decreased cognitive functioning in type 1 diabetes: An 18 year follow-up of the Diabetes Control and Complications Trial (DCCT) cohort. Diabetologia 2011, 54, 245–255. [Google Scholar] [CrossRef]
- Knutson, K.L.; van Cauter, E. Associations between sleep loss and increased risk of obesity and diabetes. Ann. N. Y. Acad. Sci. 2008, 1129, 287–304. [Google Scholar] [CrossRef]
- Kohatsu, N.D.; Tsai, R.; Young, T.; VanGilder, R.; Burmeister, L.F.; Stromquist, A.M.; Merchant, J.A. Sleep duration and body mass index in a rural population. Arch. Intern. Med. 2006, 166, 1701–1705. [Google Scholar] [CrossRef] [PubMed]
- Leproult, R.; van Cauter, E. Role of sleep and sleep loss in hormonal release and metabolism. Pediatr. Neuroendocrinol. 2010, 17, 11–21. [Google Scholar]
- Van Cauter, E.; Holmbäck, U.; Knutson, K.; Leproult, R.; Miller, A.; Nedeltcheva, A.; Pannain, S.; Penev, P.; Tasali, E.; Spiegel, K. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm. Res. Paediatr. 2007, 67, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Alhaj, O.A.; Humood, A.M.; Alenezi, A.F.; Fekih-Romdhane, F.; AlRasheed, M.M.; Saif, Z.Q.; Bragazzi, N.L.; Pandi-Perumal, S.R.; BaHammam, A.S.; et al. Sleep disturbances during the COVID-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022, 62, 101591. [Google Scholar] [CrossRef]
- Kocevska, D.; Blanken, T.F.; van Someren, E.J.W.; Rösler, L. Sleep quality during the COVID-19 pandemic: Not one size fits all. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Sinha, M.; Pande, B.; Sinha, R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: A national survey. J. Public Health Res. 2020, 9, 1826. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, R.; Dhawan, A.; Rao, R.; Mishra, A.K.; Jain, R.; Sinha, S. Assessment of Subjective Sleep Problems in Men with Opioid Dependence Maintained on Buprenorphine. J. Addict. Med. 2020, 14, 132–138. [Google Scholar] [CrossRef]
- Grandner, M.A.; Patel, N.P.; Gehrman, P.R.; Xie, D.; Sha, D.; Weaver, T.; Gooneratne, N. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010, 11, 470–478. [Google Scholar] [CrossRef]
- Grandner, M.A.; Seixas, A.; Shetty, S.; Shenoy, S. Sleep Duration and Diabetes Risk: Population Trends and Potential Mechanisms. Curr. Diabetes Rep. 2016, 16, 106. [Google Scholar] [CrossRef]
- Williams, N.J.; Grandner, M.A.; Wallace, D.M.; Cuffee, Y.; Airhihenbuwa, C.; Okuyemi, K.; Ogedegbe, G.; Jean-Louis, G. Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 2016, 18, 103–107. [Google Scholar] [CrossRef]
- Grandner, M.A.; Patel, N.P. From sleep duration to mortality: Implications of meta-analysis and future directions. J. Sleep Res. 2009, 18, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Hale, L.; Moore, M.; Patel, N.P. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med. Rev. 2010, 14, 191–203. [Google Scholar] [CrossRef] [PubMed]
- Krueger, P.M.; Friedman, E.M. Sleep duration in the United States: A cross-sectional population-based study. Am. J. Epidemiol. 2009, 169, 1052–1063. [Google Scholar] [CrossRef] [PubMed]
- Major, J.M.; Doubeni, C.A.; Freedman, N.D.; Park, Y.; Lian, M.; Hollenbeck, A.R.; Schatzkin, A.; Graubard, B.I.; Sinha, R. Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS ONE 2010, 5, e15538. [Google Scholar] [CrossRef]
- Twaits, A.; Alwan, N.A. The association between area-based deprivation and change in body-mass index over time in primary school children: A population-based cohort study in Hampshire, UK. Int. J. Obes. 2020, 44, 628–636. [Google Scholar] [CrossRef]
- Willems, S.J.; Castells, M.C.; Baptist, A.P. The Magnification of Health Disparities during the COVID-19 Pandemic. J. Allergy Clin. Immunol. Pract. 2022, 10, 903–908. [Google Scholar] [CrossRef]
- Griggs, S.; Harper, A.; Pignatiello, G.; Hickman, R.L. “Feeling Anxious about Catching COVID”: Facilitators and Barriers of Sleep Health among Young Adults with Type 1 Diabetes. Behav. Sleep Med. 2022, 20, 357–367. [Google Scholar] [CrossRef]
- Arrona-Palacios, A.; Rebolledo-Mendez, G.; Escamilla, J.; Hosseini, S.; Duffy, J. Effects of COVID-19 lockdown on sleep duration, sleep quality and burnout in faculty members of higher education in Mexico. Ciênc. Saúde Coletiva 2022, 27, 2985–2993. [Google Scholar] [CrossRef]
- Wesley, K.L.; Cooper, E.H.; Brinton, J.T.; Meier, M.; Honaker, S.; Simon, S.L. A National Survey of U.S. Adolescent Sleep Duration, Timing, and Social Jetlag during the COVID-19 Pandemic. Behav. Sleep Med. 2022, 1–13. [Google Scholar] [CrossRef]
- Coelho, J.; Micoulaud-Franchi, J.A.; Wiet, A.S.; Nguyen, D.; Taillard, J.; Philip, P. Circadian misalignment is associated with Covid-19 infection. Sleep Med. 2022, 93, 71–74. [Google Scholar] [CrossRef]
- Blackwelder, A.; Hoskins, M.; Huber, L. Effect of Inadequate Sleep on Frequent Mental Distress. Prev. Chronic Dis. 2021, 18, E61. [Google Scholar] [CrossRef] [PubMed]
- Burhamah, W.; AlKhayyat, A.; Oroszlányová, M.; AlKenane, A.; Almansouri, A.; Behbehani, M.; Karimi, N.; Jafar, H.; AlSuwaidan, M. The psychological burden of the COVID-19 pandemic and associated lockdown measures: Experience from 4000 participants. J. Affect. Disord. 2020, 277, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Planchuelo-Gómez, Á.; Odriozola-González, P.; Irurtia, M.J.; de Luis-García, R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020, 277, 842–849. [Google Scholar] [CrossRef]
- Lee, H.; Singh, G.K. Monthly trends in self-reported health status and depression by race/ethnicity and socioeconomic status during the COVID-19 Pandemic, United States, April 2020–May 2021. Ann. Epidemiol. 2021, 63, 52–62. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Terlizzi, E.P.; Schiller, J.S. Mental Health Treatment among Adults Aged 18–44: United States, 2019–2021. NCHS Data Brief 2022, 1–8. Available online: https://www.cdc.gov/nchs/products/databriefs/db444.htm (accessed on 19 October 2022).
- Vahratian, A.; Blumberg, S.J.; Terlizzi, E.P.; Schiller, J.S. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020–February 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 490. [Google Scholar] [CrossRef]
- Fernandez-Mendoza, J.; He, F.; Calhoun, S.L.; Vgontzas, A.N.; Liao, D.; Bixler, E.O. Objective short sleep duration increases the risk of all-cause mortality associated with possible vascular cognitive impairment. Sleep Health 2020, 6, 71–78. [Google Scholar] [CrossRef]
- Asdigian, N.L.; Bear, U.R.; Beals, J.; Manson, S.M.; Kaufman, C.E. Mental health burden in a national sample of American Indian and Alaska Native adults: Differences between multiple-race and single-race subgroups. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 521–530. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Self-reported frequent mental distress among adults—United States, 1993–2001. MMWR Morb. Mortal. Wkly. Rep. 2004, 53, 963–966. [Google Scholar]
- Basile Ibrahim, B.; Barcelona, V.; Condon, E.M.; Crusto, C.A.; Taylor, J.Y. The Association Between Neighborhood Social Vulnerability and Cardiovascular Health Risk Among Black/African American Women in the InterGEN Study. Nurs. Res. 2021, 70, S3–S12. [Google Scholar] [CrossRef]
- Jean-Louis, G.; Williams, N.J.; Sarpong, D.; Pandey, A.; Youngstedt, S.; Zizi, F.; Ogedegbe, G. Associations between inadequate sleep and obesity in the US adult population: Analysis of the national health interview survey (1977–2009). BMC Public Health 2014, 14, 290. [Google Scholar] [CrossRef] [PubMed]
- Knutson, K.L.; van Cauter, E.; Rathouz, P.J.; DeLeire, T.; Lauderdale, D.S. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep 2010, 33, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Neculicioiu, V.S.; Colosi, I.A.; Costache, C.; Sevastre-Berghian, A.; Clichici, S. Time to Sleep?—A Review of the Impact of the COVID-19 Pandemic on Sleep and Mental Health. Int. J. Environ. Res. Public Health 2022, 19, 3497. [Google Scholar] [CrossRef] [PubMed]
- Hisler, G.C.; Twenge, J.M. Sleep characteristics of U.S. adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021, 276, 113849. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport 2021, 38, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Committee on Sleep Medicine Research. The National Academies Collection: Reports funded by National Institutes of Health. In Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; Colten, H.R., Altevogt, B.M., Eds.; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Hale, L. Who has time to sleep? J. Public Health 2005, 27, 205–211. [Google Scholar] [CrossRef]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Rathouz, P.J.; Hulley, S.B.; Sidney, S.; Liu, K. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. Am. J. Epidemiol. 2006, 164, 5–16. [Google Scholar] [CrossRef]
- Friedman, E.M.; Love, G.D.; Rosenkranz, M.A.; Urry, H.L.; Davidson, R.J.; Singer, B.H.; Ryff, C.D. Socioeconomic status predicts objective and subjective sleep quality in aging women. Psychosom. Med. 2007, 69, 682–691. [Google Scholar] [CrossRef]
- Adams, J. Socioeconomic position and sleep quantity in UK adults. J. Epidemiol. Community Health 2006, 60, 267–269. [Google Scholar] [CrossRef]
- Hale, L.; Do, D.P. Racial differences in self-reports of sleep duration in a population-based study. Sleep 2007, 30, 1096–1103. [Google Scholar] [CrossRef]
- Nunes, J.; Jean-Louis, G.; Zizi, F.; Casimir, G.J.; von Gizycki, H.; Brown, C.D.; McFarlane, S.I. Sleep duration among black and white Americans: Results of the National Health Interview Survey. J. Natl. Med. Assoc. 2008, 100, 317–322. [Google Scholar] [CrossRef]
- Patel, S.R. Social and demographic factors related to sleep duration. Sleep 2007, 30, 1077–1078. [Google Scholar] [CrossRef] [PubMed]
- Sickel, A.E.; Moore, P.J.; Adler, N.E.; Williams, D.R.; Jackson, J.S. The differential effects of sleep quality and quantity on the relationship between SES and health. Ann. N. Y. Acad. Sci. 1999, 896, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Strine, T.W.; Chapman, D.P. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005, 6, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Kapp, J.M.; Micheas, L.; Holmes, S.; Stormont, M.; Reinke, W.M. Prevalence of Poor Mental Health Days and Adverse Childhood Experience Reporting in U.S. Adults Before and After COVID-19. Community Ment. Health J. 2022. [Google Scholar] [CrossRef]
- Ransome, Y.; Luan, H.; Song, I.; Fiellin, D.A.; Galea, S. Association of Poor Mental-Health Days with COVID-19 Infection Rates in the U.S. Am. J. Prev. Med. 2022, 62, 326–332. [Google Scholar] [CrossRef]
- Wright, L.; Steptoe, A.; Fancourt, D. Are adversities and worries during the COVID-19 pandemic related to sleep quality? Longitudinal analyses of 46,000 UK adults. PLoS ONE 2021, 16, e0248919. [Google Scholar] [CrossRef]
- Diz-Ferreira, E.; Díaz-Vidal, P.; Da Cunha Soares Nicolau, M.L.; Criado-Santos, M.P.; Ayán, C.; Diz, J.C. Effect of confinement during COVID-19 outbreak on sleep quality in Galicia. Rev. Esp. Salud Pública 2021, 95. Available online: https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1063742 (accessed on 19 October 2022).
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Ptacek, R.; Ptackova, H.; Martin, A.; Stefano, G.B. Psychiatric Manifestations of COVID-19 and Their Social Significance. Med. Sci. Monit. 2020, 26, e930340. [Google Scholar] [CrossRef]
- Necka, E.A.; Rowland, L.M.; Evans, J.D. Social Disconnection in Late Life Mental Illness—Commentary from the National Institute of Mental Health. Am. J. Geriatr. Psychiatry 2021, 29, 727–730. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, M.A.; Grundy, E. Area deprivation, perceived neighbourhood cohesion and mental health at older ages: A cross lagged analysis of UK longitudinal data. Health Place 2021, 67, 102470. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Chisholm, D.; Parikh, R.; Charlson, F.J.; Degenhardt, L.; Dua, T.; Ferrari, A.J.; Hyman, S.; Laxminarayan, R.; Levin, C.; et al. Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet 2016, 387, 1672–1685. [Google Scholar] [CrossRef]
- Griggs, S.; Conley, S.; Batten, J.; Grey, M. A systematic review and meta-analysis of behavioral sleep interventions for adolescents and emerging adults. Sleep Med. Rev. 2020, 54, 101356. [Google Scholar] [CrossRef] [PubMed]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Liu, K.; Rathouz, P.J. Sleep duration: How well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiology 2008, 19, 838. [Google Scholar] [CrossRef]
- Paine, S.J.; Gander, P.H.; Harris, R.; Reid, P. Who reports insomnia? Relationships with age, sex, ethnicity, and socioeconomic deprivation. Sleep 2004, 27, 1163–1169. [Google Scholar] [CrossRef]
| Variable | Number (%) or Mean (SD) |
|---|---|
| Age | 54.9 (18.1) |
| Race/Ethnicity White African American/Black Asian American Indian/Alaskan Native Other Hispanic | 12,754 (86.9) 992 (6.8) 139 (0.9) 96 (0.7) 385 (2.6) 310 (2.1) |
| Sex at Birth Female Male | 7970 (54.3) 6706 (45.7) |
| Years of Education Never Attended or Only Kindergarten Elementary (Grades 1–8) Some Highschool (Grades 9–11) High School Graduate Some College (1–3 years) College Graduate (4 or more years) | 6 (0) 165 (1.1) 732 (5) 4932 (33.6) 4086 (27.7) 4723 (32.2) |
| Annual Household Income Less than USD 10,000 Less than USD 25,000 Less than USD 50,000 Less than USD 75,000 USD 75,000 or more | 495 (3.4) 2667 (18.5) 2965 (20.6) 1897 (13.2) 3666 (25.5) |
| Marital Status Married Divorced/Widowed/Separated/Never Married | 7185 (49) 7335 (50) |
| Body Mass Index | 29.1 (6.9) |
| Model | Independent Variable/s | Dependent Variable/s | B | SE | β | p Value | R2 |
|---|---|---|---|---|---|---|---|
| Model 1 | SDI | Sleep Health | −0.003 | 0.001 | −0.049 | <0.001 | 0.002 |
| Mental Health | 0.033 | 0.003 | 0.098 | <0.001 | 0.010 | ||
| Model 2 | SDI | Sleep Health | −0.002 | 0.001 | −0.037 | <0.001 | 0.018 |
| Mental Health | 0.022 | 0.003 | 0.064 | <0.001 | 0.060 |
| Social Deprivation Index | ||||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | aOR | 95% CI | p Value | |
| Short sleep | 1.57 | [1.34, 1.83] | <0.001 | 1.33 | [1.12, 1.57] | 0.001 |
| Poor mental health | 1.47 | [1.26, 1.71] | <0.001 | 1.18 | [1.01, 1.39] | 0.043 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Griggs, S.; Horvat Davey, C.; Howard, Q.; Pignatiello, G.; Duwadi, D. Socioeconomic Deprivation, Sleep Duration, and Mental Health during the First Year of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 14367. https://doi.org/10.3390/ijerph192114367
Griggs S, Horvat Davey C, Howard Q, Pignatiello G, Duwadi D. Socioeconomic Deprivation, Sleep Duration, and Mental Health during the First Year of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(21):14367. https://doi.org/10.3390/ijerph192114367
Chicago/Turabian StyleGriggs, Stephanie, Christine Horvat Davey, Quiana Howard, Grant Pignatiello, and Deepesh Duwadi. 2022. "Socioeconomic Deprivation, Sleep Duration, and Mental Health during the First Year of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 21: 14367. https://doi.org/10.3390/ijerph192114367
APA StyleGriggs, S., Horvat Davey, C., Howard, Q., Pignatiello, G., & Duwadi, D. (2022). Socioeconomic Deprivation, Sleep Duration, and Mental Health during the First Year of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(21), 14367. https://doi.org/10.3390/ijerph192114367






