Prognostic Factor of Lower Limb Amputation among Diabetic Foot Ulcer Patients in North-East Peninsular Malaysia
Abstract
1. Introduction
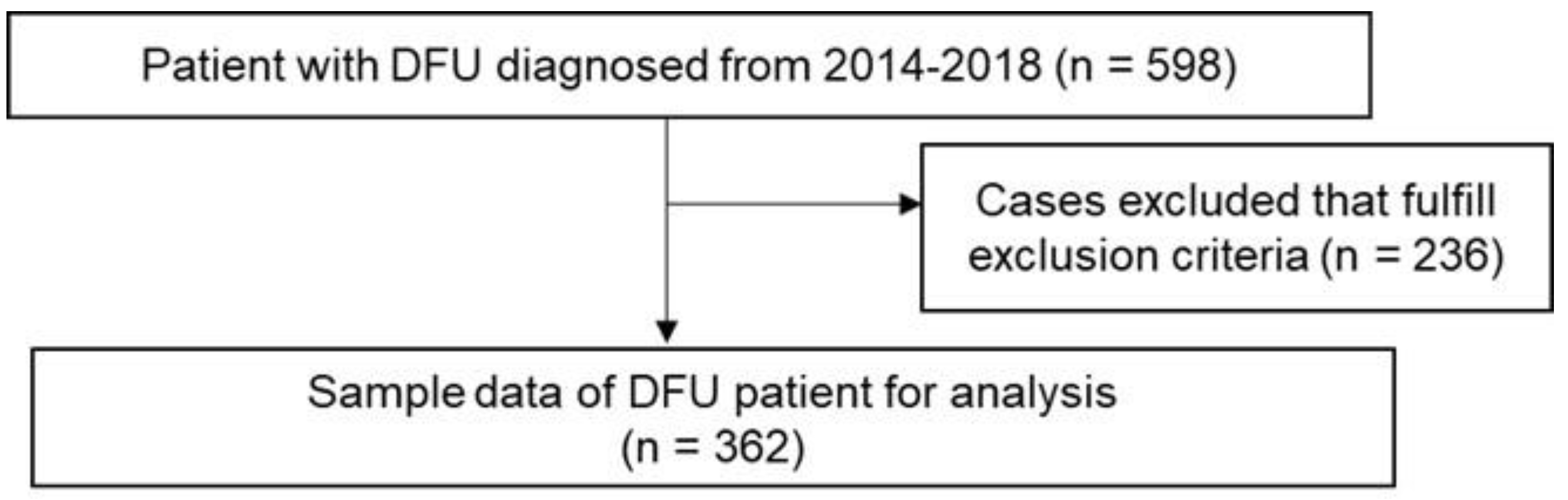
2. Materials and Methods
3. Results
3.1. Descriptive Statistics of DFU Patients
3.2. Univariate and Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IDF Diabetes. IDF Diabetes Atlas, 9th ed.; IDF Diabetes: Brussels, Belgium, 2019. [Google Scholar]
- Van Netten, J.J.; Bus, S.A.; Apelqvist, J.; Lipsky, B.A.; Hinchliffe, R.J.; Game, F.; Rayman, G.; Lazzarini, P.A.; Forsythe, R.O.; Peters, E.J.; et al. Definitions and criteria for diabetic foot disease. Lancet Diabetes Endocrinol. 2019, 2019, e3268. [Google Scholar] [CrossRef] [PubMed]
- Abdissa, D.; Adugna, T.; Gerema, U.; Dereje, D. Prevalence of Diabetic Foot Ulcer and Associated Factors among Adult Diabetic Patients on Follow-Up Clinic at Jimma Medical Center, Southwest Ethiopia, 2019: An Institutional-Based Cross-Sectional Study. J. Diabetes Res. 2020, 2020, 4106383. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann. Med. 2016, 49, 106–116. [Google Scholar] [CrossRef]
- Mariam, T.G.; Alemayehu, A.; Tesfaye, E.; Mequannt, W.; Temesgen, K.; Yetwale, F.; Limenih, M.A. Prevalence of Diabetic Foot Ulcer and Associated Factors among Adult Diabetic Patients Who Attend the Diabetic Follow-Up Clinic at the University of Gondar Referral Hospital, North West Ethiopia, 2016: Institutional-Based Cross-Sectional Study. J. Diabetes Res. 2017, 2017, 2879249. [Google Scholar] [CrossRef] [PubMed]
- Hadi, A.A.; Aris, M.A.M.; Azmi, N.H.; Nasreen, H.E.; Che, A. A Review of the Diabetic Foot in the Malaysian Perspective. World J. Pharm. Med. Res. 2019, 5, 40–43. [Google Scholar]
- Jamani, N.A.; Muhammad, N.A. Foot Problem and Foot Care Practices Among Diabetic Patients in a Primary Care Clinic, Kuala Lumpur. Int. J. Allied Health Sci. 2018, 2, 435–444. [Google Scholar]
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Boulton, A.J.M. The diabetic foot. Medicine 2010, 38, 644–648. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Swerdlow, M.A.; Armstrong, A.A.; Conte, M.S.; Padula, W.V.; Bus, S.A. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J. Foot Ankle Res. 2020, 13, 16. [Google Scholar] [CrossRef]
- Lin, J.H.; Jeon, S.Y.; Romano, P.S.; Humphries, M.D. Rates and timing of subsequent amputation after initial minor amputation. J. Vasc. Surg. 2020, 72, 268–275. [Google Scholar] [CrossRef]
- Chandran, A.; Abdullah, M.N.; Abdul, F. National Diabetes Registry Report 2013–2019; Ministry of Health Malaysia: Putrajaya, Malaysia, 2019; pp. 1–34.
- Ministry of Health Malaysia. Clinical Practice Guideline Management of Dyslipidaemia, 5th ed.; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017.
- Vadiveloo, T.; on behalf of the Scottish Diabetes Research Network Epidemiology Group; Jeffcoate, W.; Donnan, P.T.; Colhoun, H.C.; McGurnaghan, S.; Wild, S.; McCrimmon, R.; Leese, G.P. Amputation-free survival in 17,353 people at high risk for foot ulceration in diabetes: A national observational study. Diabetologia 2018, 61, 2590–2597. [Google Scholar] [CrossRef] [PubMed]
- HakimahAbRahman, N.; Aziz, A.; Mohammad, W.M.W.; NawfarSadagatullah, A.; Yassin, W.A.K.; Nordin, Z. Prognostic factors of major amputation among hospitalized diabetic foot patients in a tertiary teaching hospital, Malaysia. Malays. J. Public Health Med. 2016, 16, 41–47. [Google Scholar]
- Robinson, T.E.; Kenealy, T.; Garrett, M.; Bramley, D.; Drury, P.L.; Elley, C.R. Ethnicity and risk of lower limb amputation in people with Type 2 diabetes: A prospective cohort study. Diabet. Med. 2015, 33, 55–61. [Google Scholar] [CrossRef]
- Gould, L.; Abadir, P.; Brem, H.; Carter, M.; Conner-Kerr, T.; Davidson, J.; A DiPietro, L.; Falanga, V.; E Fife, C.; E Gardner, S.; et al. Chronic wound repair and healing in older adults: Current status and future research. J. Am. Geriatr. Soc. 2015, 63, 427–438. [Google Scholar] [CrossRef]
- Guénette, L.; Moisan, J.; Breton, M.-C.; Sirois, C.; Grégoire, J.-P. Difficulty adhering to antidiabetic treatment: Factors associated with persistence and compliance. Diabetes Metab. 2013, 39, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.L.; Chan, C.W.; Wong, P.S. Medication Adherence of Persons with Type 2 Diabetes in Malaysia: A Scoping Review and Meta-Analysis. J. ASEAN Fed. Endocr. Soc. 2022, 37, 75–82. [Google Scholar] [CrossRef]
- Low, S.K.; Khoo, J.K.; Tavintharan, S.; Lim, S.C.; Sum, C.F. Missed Appointments at a Diabetes Centre: Not a Small Problem. Ann. Acad. Med. Singap. 2016, 45, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Medical Care Quality Section. Wound Care Manual, 1st ed.; Ministry of Health Malaysia: Putrajaya, Malaysia, 2014; pp. 1–19.
- Hainer, V.; Aldhoon-Hainerová, I. Obesity Paradox Does Exist. Diabetes Care 2013, 36 (Suppl. 2), S276–S281. [Google Scholar] [CrossRef]
- Sohn, M.-W.; Budiman-Mak, E.; Oh, E.H.; Park, M.S.; Stuck, R.M.; Stone, N.; Pearce, W.B. Obesity paradox in amputation risk among nonelderly diabetic men. Obesity 2012, 20, 460–462. [Google Scholar] [CrossRef]
- Banack, H.R.; Stokes, A. The ‘obesity paradox’ may not be a paradox at all. Int. J. Obes. 2017, 41, 1162–1163. [Google Scholar] [CrossRef]
- Marques, L.R.; Diniz, T.A.; Antunes, B.M.; Rossi, F.E.; Caperuto, E.C.; Lira, F.S.; Gonçalves, D.C. Reverse cholesterol transport: Molecular mechanisms and the non-medical approach to enhance HDL cholesterol. Front. Physiol. 2018, 9, 526. [Google Scholar] [CrossRef] [PubMed]
- Kontush, A.; Chapman, M.J. Antiatherogenic function of HDL particle subpopulations: Focus on antioxidative activities. Curr. Opin. Lipidol. 2010, 21, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Sugano, M.; Tsuchida, K.; Makino, N. High-density lipoproteins protect endothelial cells from tumor necrosis factor-α-induced apoptosis. Biochem. Biophys. Res. Commun. 2000, 272, 872–876. [Google Scholar] [CrossRef]
- Brown, R.A.; Shantsila, E.; Varma, C.; Lip, G.Y. Current Understanding of Atherogenesis. Am. J. Med. 2016, 130, 268–282. [Google Scholar] [CrossRef] [PubMed]
- Ikura, K.; Hanai, K.; Shinjyo, T.; Uchigata, Y. HDL cholesterol as a predictor for the incidence of lower extremity amputation and wound-related death in patients with diabetic foot ulcers. Atherosclerosis 2015, 239, 465–469. [Google Scholar] [CrossRef]
- Kaneko, M.; Fujihara, K.; Yamamoto, M.; Kitazawa, M.; Ishizawa, M.; Osawa, T.; Harada, M.; Matsubayashi, Y.; Yamada, T.; Sone, H. Incidence and Risk Factors for Amputation in Patients with Diabetes in Japan—Historical Cohort Study Using a Nationwide Claims Database. Diabetes 2018, 67, 637-P. [Google Scholar] [CrossRef]
| Characteristic | n (%) | Censored | Amputation |
|---|---|---|---|
| n (%) | n (%) | ||
| Age at diagnosis of DFU (years) | 59.0 (10.0) * | ||
| Age at diagnosis of DFU (years) | |||
| Less than 60 | 175 (48.34) | 134 (76.6) | 41 (23.4) |
| 60 or more | 187 (51.66) | 162 (86.6) | 25 (13.4) |
| Sex | |||
| Male | 139 (38.4) | 116 (83.5) | 23 (16.5) |
| Female | 223 (61.6) | 180 (80.7) | 43 (19.3) |
| Ethnicity | |||
| Malay | 350 (96.7) | 285 (81.4) | 65 (18.6) |
| Non-Malay | 12 (3.3) | 11 (91.7) | 1 (8.3) |
| Duration of DM at diagnosis DFU (years) | |||
| Less than 10 | 211 (58.3) | 171 (81.0) | 40 (19.0) |
| 10 or more | 151 (41.7) | 125 (82.8) | 26 (17.2) |
| Smoking status | |||
| No | 296 (92.8) | 242 (81.8) | 54 (18.2) |
| Yes | 23 (7.2) | 20 (87.0) | 3 (13.0) |
| Body Mass Index | |||
| Normal | 74 (23.0) | 58 (78.4) | 16 (21.6) |
| Underweight | 14 (4.4) | 8 (57.1) | 6 (42.9) |
| Overweight | 54 (16.8) | 45 (83.3) | 9 (16.7) |
| Obese | 180 (55.9) | 158 (87.8) | 22 (12.2) |
| Hba1c (%) | |||
| Less than 6.5 | 39 (12.5) | 33 (84.5) | 6 (15.5) |
| 6.5 or more | 272 (87.5) | 222 (81.6) | 50 (18.4) |
| Triglyceride (mmol/L) | |||
| Less than 1.7 | 130 (44.5) | 107 (82.3) | 23(17.7) |
| 1.7 or more | 162 (55.5) | 131 (80.9) | 31(19.1) |
| HDL-Cholesterol | |||
| Normal | 170 (62.7) | 143 (84.1) | 27 (15.9) |
| Abnormal | 101 (37.3) | 75 (74.3) | 26 (25.7) |
| LDL-Cholesterol (mmol/L) | |||
| Less than 2.6 | 66 (24.7) | 54 (81.8) | 12 (18.2) |
| 2.6 or more | 201 (75.3) | 161 (80.1) | 40 (19.9) |
| Ischaemic Heart Disease | |||
| No | 299 (87.9) | 246 (82.3) | 53 (17.7) |
| Yes | 41 (12.1) | 30 (73.2) | 11 (26.8) |
| Nephropathy | |||
| No | 253 (73.1) | 209 (82.6) | 44 (17.4) |
| Yes | 93 (26.9) | 73 (78.5) | 20 (21.5) |
| Hypertension | |||
| No | 67 (18.9) | 59 (88.1) | 8 (11.9) |
| Yes | 287 (81.1) | 231 (80.5) | 56 (19.5) |
| Dyslipidaemia | |||
| No | 79 (22.4) | 67 (84.8) | 12 (15.2) |
| Yes | 273 (77.6) | 220 (80.6) | 53 (19.4) |
| Metformin | |||
| No | 124 (34.3) | 99 (79.8) | 25 (20.2) |
| Yes | 238 (65.7) | 197 (82.8) | 41 (17.2) |
| Sulphonylurea | |||
| No | 255 (70.4) | 201 (78.8) | 54 (21.2) |
| Yes | 107 (29.6) | 95 (88.8) | 12 (11.2) |
| Insulin | |||
| No | 132 (36.5) | 114 (86.4) | 18 (13.6) |
| Yes | 230 (63.5) | 182 (79.1) | 48 (20.9) |
| Statin | |||
| No | 86 (23.8) | 72 (83.7) | 14 (16.3) |
| Yes | 276 (76.2) | 224 (81.2) | 52 (18.8) |
| Variables | Regression Coefficient (β) | Crude Hazard Ratio (95% CI) | Wald Stats | p-Value |
|---|---|---|---|---|
| Sex | ||||
| Male | 1 | |||
| Female | 0.18 | 1.20 (0.72, 2.00) | 0.49 | 0.485 |
| Age at diagnosis of DFU (years) | ||||
| Less than 60 | 1 | |||
| 60 or more | −0.61 | 0.54 (0.33, 0.89) | 5.79 | 0.016 |
| Ethnic | ||||
| Malay | 1 | |||
| Non-Malay | −0.85 | 0.43 (0.06, 3.08) | 0.71 | 0.398 |
| Duration of DM at diagnosis of DFU | ||||
| Less than 10 | 1 | |||
| 10 years and more | −0.06 | 0.94 (0.57, 1.54) | 0.07 | 0.798 |
| BMI | ||||
| Normal | 1 | |||
| Underweight | −0.69 | 1.98 (0.78, 5.07) | 2.05 | 0.153 |
| Overweight | −0.27 | 0.76 (0.34, 1.72) | 0.43 | 0.512 |
| Obese | −0.63 | 0.53 (0.28, 1.01) | 3.69 | 0.055 |
| Hba1c (%) | ||||
| Less than 6.5 | 1 | |||
| 6.5 or more | 0.19 | 1.21 (0.52, 2.82) | 0.19 | 0.661 |
| Triglyceride (mmol/L) | ||||
| Less than 1.7 | 1 | |||
| 1.7 or more | 0.06 | 1.06 (0.62, 1.82) | 0.05 | 0.828 |
| HDL-Cholesterol | ||||
| Normal | 1 | |||
| Abnormal | 0.52 | 1.69 (0.99, 2.90) | 3.64 | 0.056 |
| LDL-Cholesterol (mmol/L) | ||||
| Less than 2.6 | 1 | |||
| 2.6 or more | 0.10 | 1.10 (0.58, 2.09) | 0.08 | 0.773 |
| Smoking Status | ||||
| No | 1 | |||
| Yes | −0.32 | 0.72(0.23, 2.32) | 0.30 | 0.586 |
| Ischaemic Heart Disease | ||||
| Absent | 1 | |||
| Present | 0.44 | 1.55 (0.81, 2.96) | 1.74 | 0.187 |
| Nephropathy | ||||
| Absent | 1 | |||
| Present | 0.24 | 1.28 (0.75, 2.17) | 0.81 | 0.368 |
| Hypertension | ||||
| Absent | 1 | |||
| Present | 0.53 | 1.71 (0.81, 3.58) | 1.99 | 0.158 |
| Dyslipidaemia | ||||
| Absent | 1 | |||
| Present | 0.24 | 1.27 (0.68, 2.37) | 0.55 | 0.457 |
| Metformin | ||||
| No | 1 | |||
| Yes | −0.17 | 0.84 (0.51, 1.39) | 0.46 | 0.499 |
| Sulphonylurea | ||||
| No | 1 | |||
| Yes | −0.69 | 0.50 (0.27, 0.94) | 4.70 | 0.030 |
| Insulin | ||||
| No | 1 | |||
| Yes | 0.47 | 1.59 (0.93, 2.74) | 2.83 | 0.093 |
| Statin | ||||
| No | 1 | |||
| Yes | 0.13 | 1.13 (0.63, 2.05) | 0.173 | 0.677 |
| Variables | Regression Coefficient (β) | Adjusted Hazard Ratio (95% CI) | Wald Stats | p-Value |
|---|---|---|---|---|
| Age at diagnosis of DFU (years) | ||||
| Less than 60 | 1 | |||
| 60 or more | −0.73 | 0.48 (0.27, 0.89) | 5.52 | 0.019 |
| BMI (kg/m2) | ||||
| Normal | 1 | |||
| Underweight | 0.77 | 2.17 (0.78, 6.07) | 2.17 | 0.140 |
| Overweight | −0.39 | 0.68 (0.28, 1.62) | 0.77 | 0.381 |
| Obese | −0.81 | 0.45 (0.22, 0.89) | 5.22 | 0.039 |
| HDL-Cholesterol | ||||
| Normal | 1 | |||
| Abnormal | 0.78 | 2.18 (1.21, 3.92) | 4.55 | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosedi, A.; Hairon, S.M.; Abdullah, N.H.; Yaacob, N.A. Prognostic Factor of Lower Limb Amputation among Diabetic Foot Ulcer Patients in North-East Peninsular Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 14212. https://doi.org/10.3390/ijerph192114212
Rosedi A, Hairon SM, Abdullah NH, Yaacob NA. Prognostic Factor of Lower Limb Amputation among Diabetic Foot Ulcer Patients in North-East Peninsular Malaysia. International Journal of Environmental Research and Public Health. 2022; 19(21):14212. https://doi.org/10.3390/ijerph192114212
Chicago/Turabian StyleRosedi, Anas, Suhaily Mohd Hairon, Noor Hashimah Abdullah, and Nor Azwany Yaacob. 2022. "Prognostic Factor of Lower Limb Amputation among Diabetic Foot Ulcer Patients in North-East Peninsular Malaysia" International Journal of Environmental Research and Public Health 19, no. 21: 14212. https://doi.org/10.3390/ijerph192114212
APA StyleRosedi, A., Hairon, S. M., Abdullah, N. H., & Yaacob, N. A. (2022). Prognostic Factor of Lower Limb Amputation among Diabetic Foot Ulcer Patients in North-East Peninsular Malaysia. International Journal of Environmental Research and Public Health, 19(21), 14212. https://doi.org/10.3390/ijerph192114212







