Reliability and Validity of the Japanese Version of the Assessment of Readiness for Mobility Transition (ARMT-J) for Japanese Elderly
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Basic Information
2.2.2. Instruments
- ARMT
- The12-item short-form health survey: SF-12
- Life Space Assessment: LSA
- Geriatric Depression Scale—Short Version—Japanese (GDS-S-J)
2.3. Statistical Analysis
2.4. Validity and Reliability
2.4.1. Validity
- Content Validity:
- Criterion Validity
- Construct Validity
2.4.2. Reliability
- Internal Consistency
- Reliability (Test–Retest Reliability)
- Measurement Error
3. Results
3.1. Participants and Basic Information
3.2. Validity: Construct Validity
3.2.1. Cross-Cultural Validity
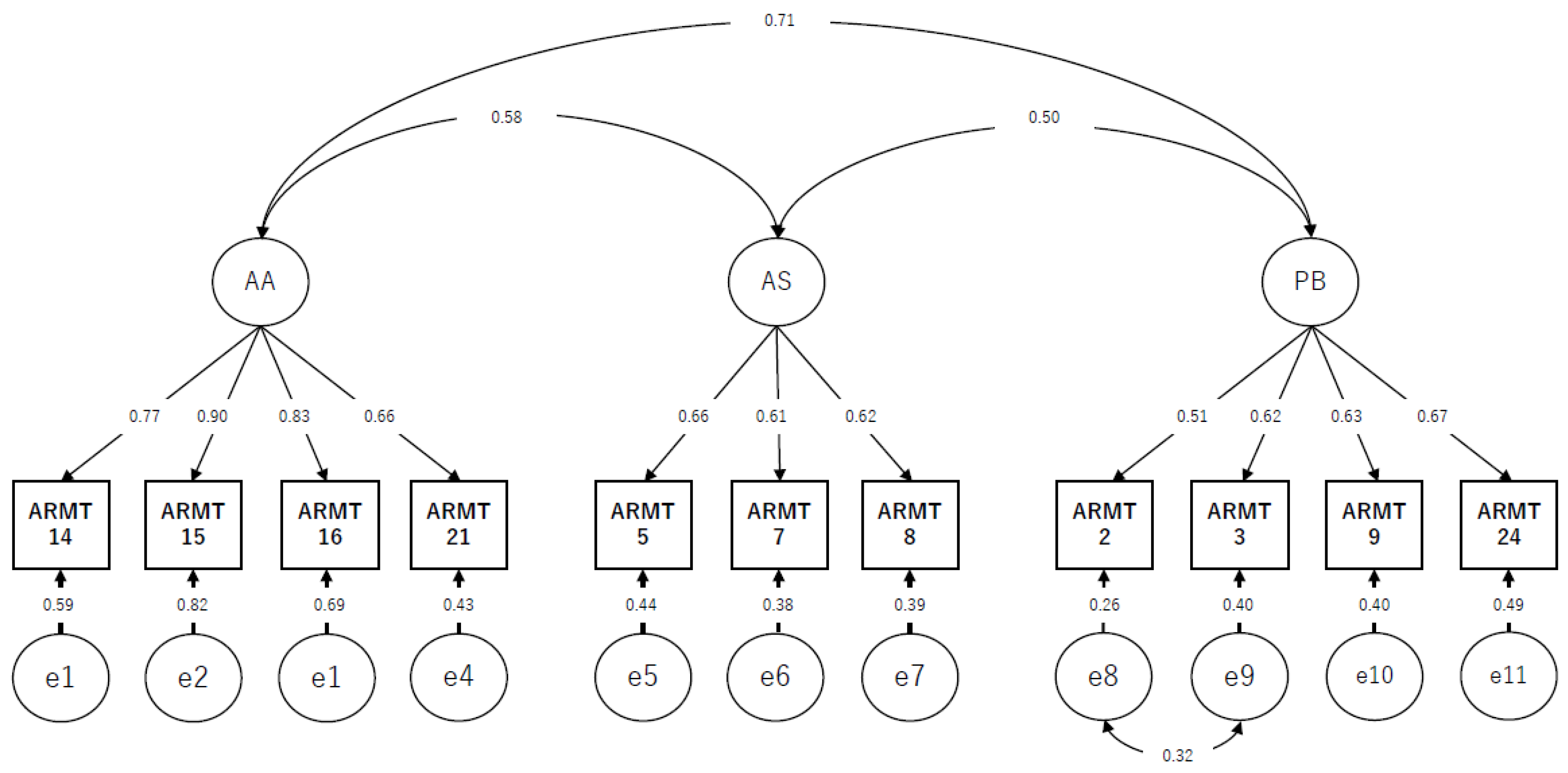
3.2.2. Structural Validity
3.2.3. Hypotheses-Testing
3.3. Reliability
3.3.1. Internal Consistency
3.3.2. Measurement Error
4. Discussion
4.1. Validity
4.2. Reliability
4.3. Limitation
4.4. Implication
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Violence and Injury Prevention. Road Traffic Injuries. Available online: https://www.who.int/publications/i/item/world-report-on-road-traffic-injury-prevention (accessed on 18 August 2022).
- Ouchi, Y.; Rakugi, H.; Arai, H.; Akishita, M.; Ito, H.; Toba, K.; Kai, I. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr. Gerontol. Int. 2017, 17, 1045–1047. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Phillips, D.; Lee, J. Disability prevalence in midlife (aged 55–65 years): Cross-Country comparisons of gender differences and time trends. Women’s Midlife Health 2021, 7, 1. [Google Scholar] [CrossRef]
- Persson, H.C.; Selander, H. Transport mobility 5 years after stroke in an urban setting. Top Stroke Rehabil. 2018, 25, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Stasiulis, E.; Rapoport, M.J.; Sivajohan, B.; Naglie, G. The Paradox of Dementia and Driving Cessation: “It’s a Hot Topic,” “Always on the Back Burner”. Gerontologist 2020, 60, 1261–1272. [Google Scholar] [CrossRef] [PubMed]
- Anstey, K.J.; Wood, J.; Lord, S.; Walker, J.G. Cognitive, sensory, and physical factors enabling driving safety in older adults. Clin. Psychol. Rev. 2005, 25, 45–65. [Google Scholar] [CrossRef] [PubMed]
- Desapriya, E.; Wijeratne, H.; Subzwari, S.; Babul-Wellar, S.; Turcotte, K.; Rajabali, F.; Kinney, J.; Pike, I. Vision screening of older drivers for preventing road traffic injuries and fatalities. Cochrane Database Syst. Rev. 2011, 3, Cd006252. [Google Scholar] [CrossRef]
- Lacherez, P.; Wood., J.M.; Anstey., K.J.; Lord, S.R. Sensorimotor and postural control factors associated with driving safety in a community-dwelling older driver population. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 240–244. [Google Scholar] [CrossRef] [PubMed]
- About the Characteristics of Traffic Accidents. Available online: https://www.npa.go.jp/publications/statistics/koutsuu/toukeihyo.html (accessed on 18 August 2022).
- O’Connor, M.L.; Edwards, J.D.; Small, B.J.; Andel, R. Patterns of level and change in self-reported driving behaviors among older adults: Who self-regulates? J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2012, 67, 437–446. [Google Scholar] [CrossRef]
- O’Connor, M.L.; Edwards, J.D.; Wadley, V.G.; Crowe, M. Changes in mobility among older adults with psychometrically defined mild cognitive impairment. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2010, 65b, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Kahana, E.; Kahana, B.; Zhang, Y. Driving Cessation in Old Age: Gender Influences on Mortality. J. Aging Health 2021, 33, 447–457. [Google Scholar] [CrossRef] [PubMed]
- Chihuri, S.; Mielenz, T.J.; DiMaggio, C.J.; Betz, M.E.; DiGuiseppi, C.; Jones, V.C.; Li, G. Driving cessation and health outcomes in older adults. J. Am. Geriatr. Soc. 2016, 64, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Fonda, S.J.; Wallace, R.B.; Herzog, A.R. Changes in driving patterns and worsening depressive symptoms among older adults. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2001, 56, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Ishii, H.; Doi, T.; Tsutsumimoto, K.; Nakakubo, S.; Kurita, S.; Shimada, H. Driving cessation and physical frailty in community-dwelling older adults: A longitudinal study. Geriatr. Gerontol. Int. 2021, 21, 1047–1052. [Google Scholar] [CrossRef] [PubMed]
- Qin, W.; Xiang, X.; Taylor, H. Driving Cessation and Social Isolation in Older Adults. J. Aging Health 2020, 32, 962–971. [Google Scholar] [CrossRef]
- Al-Hassani, S.B.; Alotaibi, N.M. The Impact of Driving Cessation on Older Kuwaiti Adults: Implications to Occupational Therapy. Occup. Ther. Health Care 2014, 28, 264–276. [Google Scholar] [CrossRef]
- Nakamura, A.; Maruta, M.; Makizako, H.; Miyata, M.; Miyata, H.; Han, G.; Ikeda, Y.; Shimokihara, S.; Tokuda, K.; Tabira, T.; et al. Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation. Int. J. Environ. Res. Public Health 2021, 18, 13270. [Google Scholar] [CrossRef]
- Mezuk, B.; Rebok, G.W. Social integration and social support among older adults following driving cessation. J. Gerontol. B Psychol. Sci. Soc. Sci. 2008, 63, 298–303. [Google Scholar] [CrossRef]
- Curl, A.L.; Stowe, J.D.; Cooney, T.M.; Proulx, C.M. Giving up the keys: How driving cessation affects engagement in later life. Gerontologist 2014, 54, 423–433. [Google Scholar] [CrossRef]
- Gaulton, T.G.; Neuman, M.D.; Brown, R.T.; Betz, M.E. Association of hospitalization with driving reduction and cessation in older adults. J. Am. Geriatr. Soc. 2021, 69, 2231–2239. [Google Scholar] [CrossRef]
- Moon, S.; Park, K. The Predictors of Driving Cessation among Older Drivers in Korea. Int. J. Environ. Res. Public Health 2020, 17, 7206. [Google Scholar] [CrossRef]
- Strogatz, D.; Mielenz, T.J.; Johnson, A.K.; Baker, I.R.; Robinson, M.; Mebust, S.P.; Andrews, H.A.; Betz, M.E.; Edy, D.W.; Johnson, R.M.; et al. Importance of Driving and Potential Impact of Driving Cessation for Rural and Urban Older Adults. J. Rural Health 2020, 36, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Ang, B.H.; Oxley, J.A.; Chen, W.S.; Yap, M.K.K.; Song, K.P.; Lee, S.W.H. The influence of spouses and their driving roles in self-regulation: A qualitative exploration of driving reduction and cessation practices amongst married older adults. PLoS ONE 2020, 15, e0232795. [Google Scholar] [CrossRef] [PubMed]
- Vivoda, J.M.; Walker, R.M.; Cao, J.; Koumoutzis, A. How Accumulated Wealth Affects Driving Reduction and Cessation. Gerontologist 2020, 60, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Allan, C.L.; Behrman, S.; Baruch, N.; Ebmeier, K.P. Driving and dementia: A clinical update for mental health professionals. Evid. Based Ment. Health 2016, 19, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Betz, M.E.; Jones, J.; Petroff, E.; Schwartz, R. “I wish we could normalize driving health”: A qualitative study of clinician discussions with older drivers. J. Gen. Intern. Med. 2013, 28, 1573–1580. [Google Scholar] [CrossRef]
- Pellichero, A.; Lafont, S.; Paire-Ficout, L.; Fabrigoule, C.; Chavoix, C. Barriers and facilitators to social participation after driving cessation among older adults: A cohort study. Ann. Phys. Rehabil. Med. 2020, 64, 101373. [Google Scholar] [CrossRef]
- Berg-Weger, M.; Meuser, T.M.; Stowe, J. Addressing individual differences in mobility transition counseling with older adults. J. Gerontol. Soc. Work 2013, 56, 201–218. [Google Scholar] [CrossRef]
- Meuser, T.M.; Berg-Weger, M.; Chibnall, J.T.; Harmon, A.C.; Stowe, J.D. Assessment of Readiness for Mobility Transition (ARMT): A tool for mobility transition counseling with older adults. J. Appl. Gerontol. 2013, 32, 484–507. [Google Scholar] [CrossRef]
- Assessment of Readiness for Mobility Transition (ARMT). Available online: https://www.umsl.edu/mtci/PDFs/ARMT%20Manual%208-11pdf (accessed on 18 August 2022).
- Nasu, S.; Yanane, S.; Kobayashi, S. Assessment of Readiness for Mobility Transition: Development of the Japanese Version of the ARMT and Verification of Linguistic Validity. Jpn. J. Rehabil. Med. 2022, 59, 532–540. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Prinsen, C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.; Caroline, B.T. COSMIN Methodology for Systematic Reviews of Patient-Reported Outcome Measures (PROMs). User Manual; Amsterdam Public Health Research Institute: Amsterdam, The Netherlands, 2018; Volume 78, p. 1. [Google Scholar]
- Marx, R.G.; Menezes, A.; Horovitz, L.; Jones, E.C.; Warren, R.F. A comparison of two time intervals for test-retest reliability of health status instruments. J. Clin. Epidemiol. 2003, 56, 730–735. [Google Scholar] [CrossRef]
- Jenkinson, C.; Layte, R. Development and testing of the UK SF-12 (short form health survey). J. Health Serv. Res. Policy 1997, 2, 14–18. [Google Scholar] [CrossRef]
- Suzukamo, Y.; Fukuhara, S.; Green, J.; Kosinski, M.; Gandek, B.; Ware, J.E. Validation testing of a three-component model of Short Form-36 scores. J. Clin. Epidemiol. 2011, 64, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.; Baker, P.S.; Allman, R.M. A life-space approach to functional assessment of mobility in the elderly. J. Gerontol. Nurs. 2002, 35, 35–55. [Google Scholar] [CrossRef]
- Harada, K.; Shimada, H.; Sawyer, P.; Asakawa, Y.; Nihei, K.; Kaneya, S.; Furuna, T.; Ishizaki, T.; Yasumura, S. Life-space of community-dwelling older adults using preventive health care services in Japan and the validity of composite scoring methods for assessment. Jpn. J. Public Health 2010, 57, 526–537. [Google Scholar]
- Sugishita, H.; Asahi, T. The creation of the Geriatric Depression Scale-Short version-Japanese (GDS-S-J). Jpn. J. Cogn. Neurosci. 2009, 12, 87–90. (In Japanese) [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- King, M.D.; Meuser, T.M.; Berg-Weger, M.; Chibnall, J.T.; Harmon, A.C.; Yakimo, R. Decoding the Miss Daisy Syndrome: An examination of subjective responses to mobility change. J. Gerontol. Soc. Work 2011, 54, 29–52. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.C. A review of exploratory factor analysis decisions and overview of current practices: What we are doing and how can we improve? Int. J. Hum.-Comput. Int. 2016, 32, 51–62. [Google Scholar] [CrossRef]
- Akaike, H. Factor analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- McDonald, R.P.; Ho, M.H. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272. [Google Scholar] [CrossRef]
- Velicer, W.F.; Eaton, C.A.; Fava, J.L. Construct explication through factor or component analysis. A review and evaluation of alternative procedures for determining the number of factors or components. In Problems and Solutions in Human Assessment: Honoring Douglas N. Jackson at Seventy, 2nd ed.; Goffin, R., Helmes, E., Eds.; Springer Science & Business Media: Totowa, NJ, USA, 2000; pp. 41–71. [Google Scholar]
- Horn, J.L. A rationale and technique for estimating the number of factors in factor analysis. Psychometrika 1965, 30, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Costello, A.B.; Osborne, J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 7. [Google Scholar] [CrossRef]
- Taber, K.S. The use of Cronbach’s alpha when developing and reporting research instruments in science education. J. Res. Sci. Teach. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Qin, S.; Nelson, L.; McLeod, L.; Eremenco, S.; Coons, S.J. Assessing test-retest reliability of patient-reported outcome measures using intraclass correlation coefficients: Recommendations for selecting and documenting the analytical formula. Qual. Life Res. 2019, 28, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Kliebsch, U. Dependence of weighted kappa coefficients on the number of categories. Epidemiology 1996, 7, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Fleiss, J.L.; Levin, B.; Paik, M.C. The Measurement of Interrater Agreement: Statistical Methods for Rates and Proportions, 2nd ed.; Wiley: Hoboken, NJ, USA, 1981; pp. 212–236. [Google Scholar]
| Number (%) | ||
| Sex | Female | 57 (33) |
| Male | 116 (67) | |
| age | 55–60 | 50 (29) |
| 61–65 | 35 (20) | |
| 66–70 | 32 (19) | |
| 71–75 | 28 (16) | |
| ≥76 | 28 (16) | |
| Type of Living | Alone | 38 (22) |
| With someone | 135 (78) | |
| Education | Junior high school | 18 (10) |
| High school | 76 (44) | |
| Vocational school | 42 (24) | |
| University | 34 (20) | |
| Graduate school | 3 (2) | |
| Primary disease | None (Wellness) | 30 (17) |
| Stroke | 95 (55) | |
| Traumatic brain injury | 6 (4) | |
| Bone fracture | 9 (5) | |
| Spinal cord injury | 15 (9) | |
| Others | 18 (10) | |
| Driving status | Driving | 77 (45) |
| Driving cessation | 96 (55) | |
| Residential area | Rural | 115 (66) |
| Urban | 58 (34) | |
| Accessibility of public transportation | Exclent | 34 (20) |
| Very good | 68 (39) | |
| Fair | 39 (22) | |
| Poor | 22 (13) | |
| Unacceptable | 10 (6) |
| Items | Communality | 2 Factors | 3 Factors | 4 Factors | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F1 | F2 | F3 | F1 | F2 | F3 | F4 | ||
| ARMT1 | 0.46 | 0.409 | 0.187 | 0.107 | 0.066 | −0.045 | −0.657 | |||
| ARMT2 | 0.51 | −0.011 | 0.056 | 0.604 | 0.111 | −0.082 | 0.192 | −0.511 | ||
| ARMT3 | 0.48 | 0.456 | 0.049 | −0.071 | −0.048 | 0.859 | ||||
| ARMT4 | 0.48 | 0.013 | 0.092 | 0.004 | −0.646 | |||||
| ARMT5 | 0.46 | 0.059 | 0.694 | 0.001 | 0.620 | 0.099 | −0.042 | 0.600 | 0.027 | −0.251 |
| ARMT6 | 0.52 | −0.102 | 0.104 | 0.737 | −0.094 | |||||
| ARMT7 | 0.37 | −0.015 | 0.647 | −0.105 | 0.702 | 0.059 | −0.045 | 0.629 | 0.116 | −0.033 |
| ARMT8 | 0.33 | 0.176 | 0.424 | 0.217 | 0.520 | −0.114 | 0.247 | 0.509 | −0.045 | 0.084 |
| ARMT9 | 0.42 | 0.162 | 0.009 | 0.455 | 0.189 | −0.039 | 0.632 | 0.064 | ||
| ARMT10 | 0.57 | 0.743 | −0.017 | 0.575 | −0.033 | 0.066 | −0.264 | |||
| ARMT11 | 0.33 | |||||||||
| ARMT12 | 0.49 | 0.611 | 0.045 | 0.497 | 0.090 | 0.123 | −0.061 | |||
| ARMT13 | 0.13 | |||||||||
| ARMT14 | 0.63 | 0.685 | 0.114 | 0.596 | 0.262 | 0.040 | 0.683 | 0.240 | 0.089 | 0.091 |
| ARMT15 | 0.73 | 0.945 | −0.120 | 0.822 | 0.010 | 0.121 | 0.846 | −0.007 | 0.072 | −0.025 |
| ARMT16 | 0.71 | 0.985 | −0.261 | 0.910 | −0.119 | 0.039 | 0.879 | −0.097 | −0.026 | −0.058 |
| ARMT17 | 0.46 | |||||||||
| ARMT18 | 0.43 | 0.448 | 0.122 | |||||||
| ARMT19 | 0.28 | |||||||||
| ARMT20 | 0.29 | |||||||||
| ARMT21 | 0.56 | 0.596 | 0.160 | 0.451 | 0.221 | 0.135 | 0.482 | 0.159 | −0.036 | −0.210 |
| ARMT22 | 0.62 | |||||||||
| ARMT23 | 0.54 | 0.531 | 0.226 | |||||||
| ARMT24 | 0.48 | 0.172 | 0.060 | 0.463 | ||||||
| Factor correlation | F1 | F2 | F1 | F2 | F3 | F1 | F2 | F3 | F4 | |
| F2 | 0.558 | - | 0.469 | - | 0.414 | - | ||||
| F3 | 0.534 | 0.383 | - | 0.419 | 0.287 | - | ||||
| F4 | −0.478 | −0.366 | −0.384 | - | ||||||
| Model | Items | χ2 | df | χ2/df | p | GFI | CFI | RMSEA | AIC |
|---|---|---|---|---|---|---|---|---|---|
| Two-factor model | F1: 1, 3, 10, 12, 14–16, 18, 21, 23 | 120.19 | 64 | 1.88 | p < 0.000 | 0.903 | 0.938 | 0.071 | 174.19 |
| F2: 5, 7, 8 | |||||||||
| Three-factor model | F1: 14–16, 21 | 70.67 | 41 | 1.72 | p < 0.003 | 0.930 | 0.956 | 0.065 | 120.67 |
| F2: 5, 7, 8 | |||||||||
| F3: 2, 3, 9, 24 | |||||||||
| Four-factor model | F1: 10, 12, 14–16 | 137.21 | 71 | 1.93 | p < 0.000 | 0.901 | 0.931 | 0.074 | 205.21 |
| F2: 5, 7, 8 | |||||||||
| F3: 6, 9 | |||||||||
| F4: 1, 2, 4 |
| ARMT-AA | ARMT-PB | ARMT-AS | ARMT-TS | GDS | LSA | SF-36 PCS | SF-36 MCS | SF-36 RCS | |
|---|---|---|---|---|---|---|---|---|---|
| ARMT-AA | 1.000 | ||||||||
| ARMT-PB | 0.566 ** | 1.000 | |||||||
| ARMT-AS | 0.492 ** | 0.334 ** | 1.000 | ||||||
| ARMT-TS | 0.883 ** | 0.806 ** | 0.69 ** | 1.000 | |||||
| GDS | 0.250 ** | 0.262 ** | 0.238 ** | 0.324 ** | 1.000 | ||||
| LSA | 0.033 | 0.073 | −0.126 | 0.016 | −0.163 * | 1.000 | |||
| SF-36 PCS | 0.092 | 0.011 | 0.044 | 0.061 | −0.054 | 0.302 ** | 1.000 | ||
| SF-36 MCS | 0.005 | −0.076 | −0.005 | −0.043 | −0.42 ** | −0.118 | −0.113 | 1.000 | |
| SF-36 RCS | −0.173 * | −0.120 | −0.059 | −0.165 * | −0.266 ** | 0.23 ** | −0.239 ** | −0.095 | 1.000 |
| Test | Retest | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Scale | Score Range |
Mean (SD) | Median (IQR) |
Mean (SD) | Median (IQR) | Cohen’s Weighted κ (95% CI) | ICC (95% CI) | SEM | SDC |
| ARMT-TS | 11–55 | 31.91 (10.29) | 31 (24.5–41) | 31.94 (10.81) | 31 (24–39.5) | 0.76 (0.71–0.80) | 0.93 (0.91–0.95) | 0.72 | 2.00 |
| ARMT—PB | 4–20 | 12.54 (4.33) | 13 (9–16) | 12.49 (4.44) | 12 (9–16) | 0.65 (0.58–0.72) | 0.84 (0.78–0.88) | 0.31 | 0.86 |
| Item 2 | 1–5 | 3.01 (1.42) | 3 (2–4) | 3.01 (1.34) | 3 (2–4) | 0.48 (0.37–0.58) | 0.60 (0.48–0.70) | 0.11 | 0.30 |
| Item 3 | 1–5 | 3.20 (1.33) | 3 (2–4) | 3.20 (1.36) | 3 (2–4) | 0.60 (0.50–0.70) | 0.72 (0.62–0.79) | 0.10 | 0.29 |
| Item 9 | 1–5 | 3.27 (1.36) | 4 (2–4) | 3.15 (1.43) | 3 (2–4) | 0.70 (0.61–0.78) | 0.81 (0.74–0.86) | 0.11 | 0.28 |
| Item 24 | 1–5 | 3.06 (1.44) | 3 (2–4) | 3.12 (1.33) | 3 (2–4) | 0.57 (0.47–0.67) | 0.69 (0.59–0.77) | 0.10 | 0.28 |
| ARMT—AS | 3–15 | 8.51 (3.23) | 9 (6–11) | 8.45 (3.19) | 8 (6–11) | 0.73 (0.60–0.74) | 0.85 (0.79–0.89) | 0.24 | 0.66 |
| Item 5 | 1–5 | 2.92 (1.48) | 3 (1–4) | 2.92 (1.42) | 3 (2–4) | 0.58 (0.47–0.68) | 0.69 (0.58–0.78) | 0.10 | 0.30 |
| Item 7 | 1–5 | 2.88 (1.28) | 3 (2–4) | 2.97 (1.21) | 3 (2–4) | 0.45 (0.33–0.57) | 0.54 (0.40–0.65) | 0.10 | 0.27 |
| Item 8 | 1–5 | 2.71 (1.44) | 3 (1–4) | 2.55 (1.38) | 2 (1–4) | 0.65 (0.56–0.74) | 0.77 (0.69–0.83) | 0.10 | 0.28 |
| ARMT—AA | 4–20 | 10.86 (4.82) | 11 (7–14.5) | 11.00 (4.67) | 11 (8–14) | 0.68 (0.60–0.75) | 0.84 (0.78–0.89) | 0.35 | 0.96 |
| Item14 | 1–5 | 2.61 (1.39) | 2 (1–4) | 2.71 (1.40) | 3 (1–4) | 0.63 (0.55–0.73) | 0.76 (0.68–0.83) | 0.10 | 0.27 |
| Item15 | 1–5 | 2.69 (1.44) | 3 (1–4) | 2.70 (1.39) | 3 (1–4) | 0.60 (0.51–0.69) | 0.76 (0.67–0.82) | 0.10 | 0.29 |
| Item16 | 1–5 | 2.98 (1.46) | 3 (2–4) | 2.96 (1.39) | 3 (2–4) | 0.57 (0.47–0.68) | 0.66 (0.55–0.75) | 0.11 | 0.30 |
| Item21 | 1–5 | 2.57 (1.31) | 2 (1–2) | 2.61 (1.24) | 2 (2–4) | 0.64 (0.55–0.74) | 0.74 (0.66–0.81) | 0.10 | 0.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nasu, S.; Ishibashi, Y.; Ikuta, J.; Yamane, S.; Kobayashi, R. Reliability and Validity of the Japanese Version of the Assessment of Readiness for Mobility Transition (ARMT-J) for Japanese Elderly. Int. J. Environ. Res. Public Health 2022, 19, 13957. https://doi.org/10.3390/ijerph192113957
Nasu S, Ishibashi Y, Ikuta J, Yamane S, Kobayashi R. Reliability and Validity of the Japanese Version of the Assessment of Readiness for Mobility Transition (ARMT-J) for Japanese Elderly. International Journal of Environmental Research and Public Health. 2022; 19(21):13957. https://doi.org/10.3390/ijerph192113957
Chicago/Turabian StyleNasu, Satonori, Yu Ishibashi, Junichi Ikuta, Shingo Yamane, and Ryuji Kobayashi. 2022. "Reliability and Validity of the Japanese Version of the Assessment of Readiness for Mobility Transition (ARMT-J) for Japanese Elderly" International Journal of Environmental Research and Public Health 19, no. 21: 13957. https://doi.org/10.3390/ijerph192113957
APA StyleNasu, S., Ishibashi, Y., Ikuta, J., Yamane, S., & Kobayashi, R. (2022). Reliability and Validity of the Japanese Version of the Assessment of Readiness for Mobility Transition (ARMT-J) for Japanese Elderly. International Journal of Environmental Research and Public Health, 19(21), 13957. https://doi.org/10.3390/ijerph192113957







