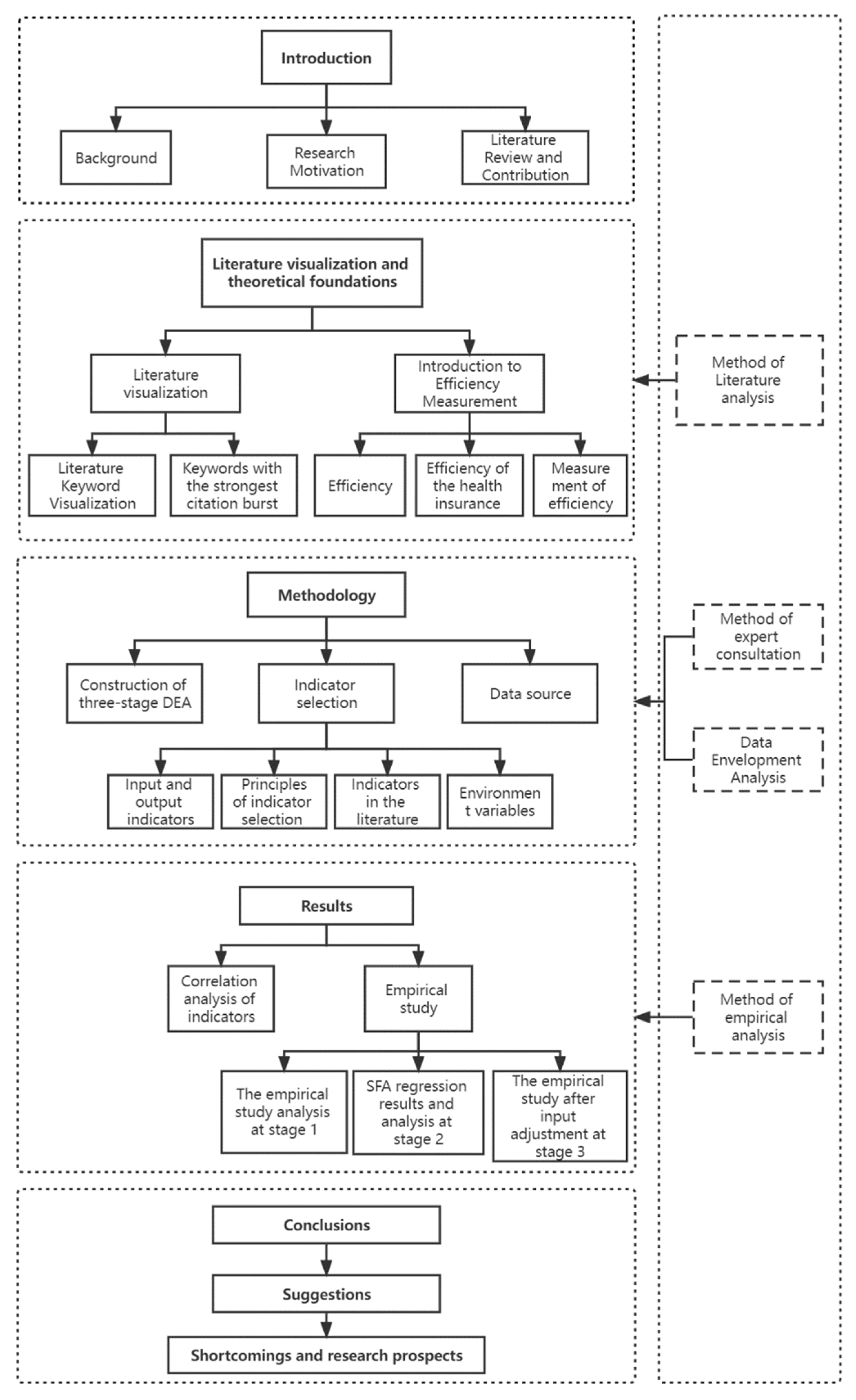
Analysis of the Operational Efficiency of Basic Medical Insurance for Urban and Rural Residents: Based on a Three-Stage DEA Model
Abstract
1. Introduction
1.1. Background of the Study
1.2. Research Motivation
1.3. Literature Review and Contribution
2. Literature Visualization and Theoretical Foundations
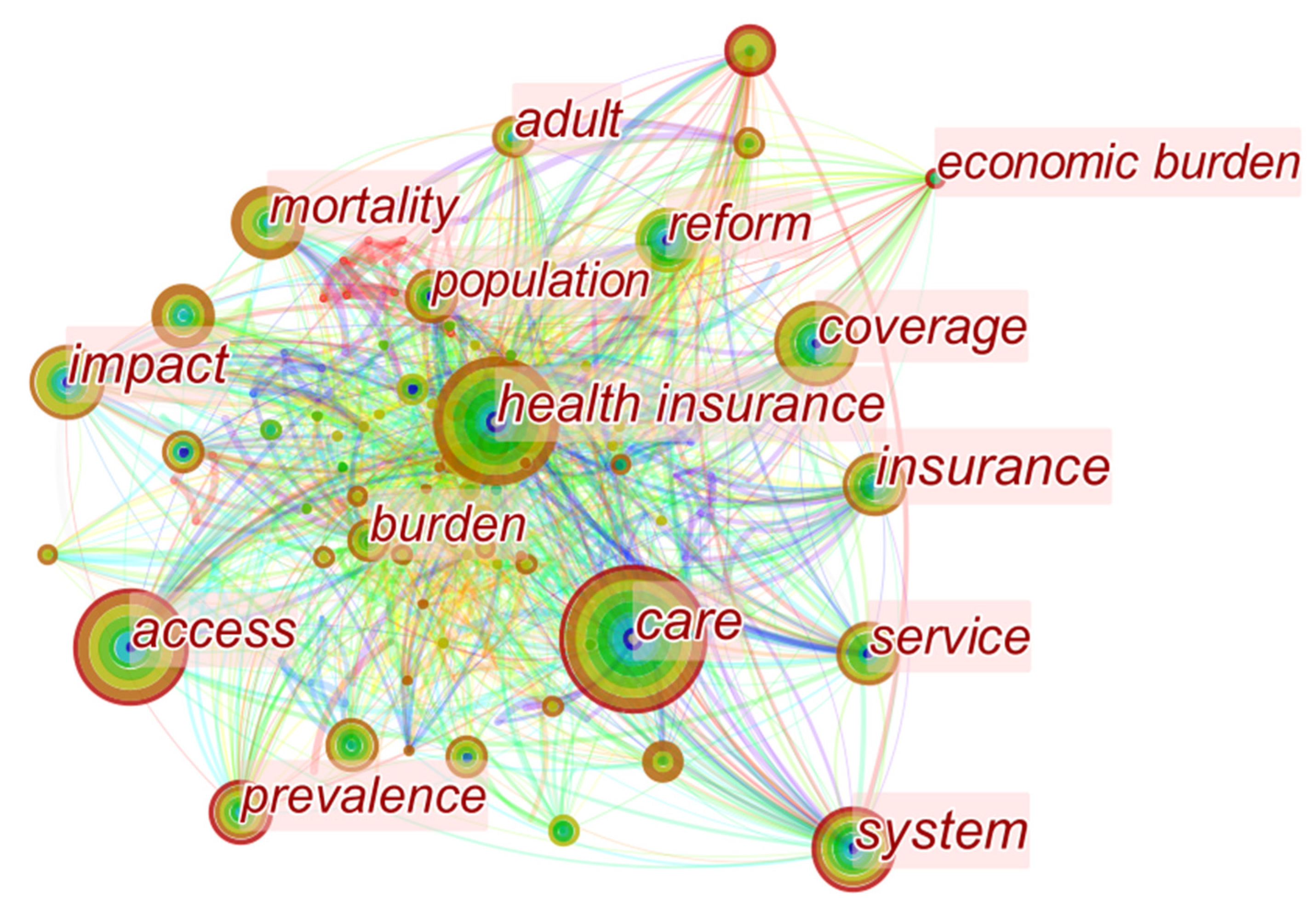
2.1. Literature Visualization
2.1.1. Visual Statistical Map of the Literature Keywords
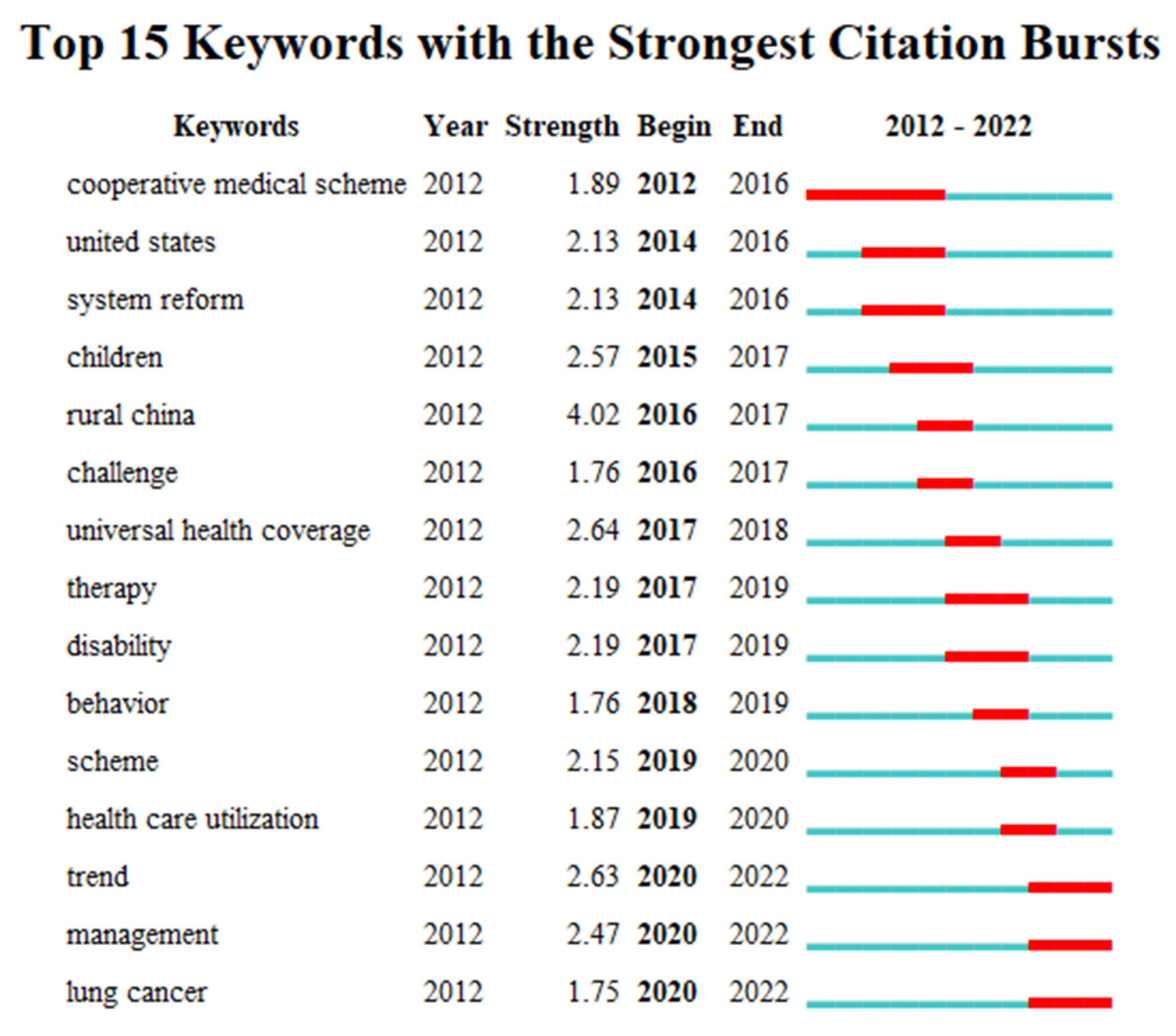
2.1.2. Keywords with the Strongest Citation Burst
2.2. Introduction to the Efficiency Measurement
2.2.1. Efficiency
2.2.2. Efficiency of the Health Insurance System
2.2.3. Measurement of the Efficiency
3. Methodology
3.1. Construction of the Three-Stage DEA
3.2. Indicator Selection
3.2.1. Input and Output Indicators
3.2.2. Principles of the Indicator Selection
- (1)
- Principle of comprehensiveness. Medical insurance is a complex system project, so the evaluation indicators should follow the principle of comprehensiveness. The representative and regular indicators, among the indicators reflecting the operating efficiency of the medical insurance fund, must be found using the scientific comprehensive evaluation method.
- (2)
- Principle of objectivity. Medical insurance is a highly practical work, and its evaluation indicators system should reflect the real situation of the medical insurance fund operation. Since the economic development of each region is different and there are differences in their implemented medical insurance, the indicators with a high degree of specificity should be developed for the actual situation of each region. In order to ensure the objectivity of the evaluation indicators of the operation efficiency of the medical insurance fund, the indicators in this study are obtained from the National Bureau of Statistics, to ensure a high degree of objectivity and accuracy.
- (3)
- Principle of operability. The evaluation indicators of the medical insurance operation efficiency should be selected to reflect the specific content of the fund operation or the indicators with easily accessible data. The accessibility and representativeness of the evaluation indicators are related to the feasibility of the evaluation indicator system. Therefore, the selected indicators should be derived from the specific work of the health insurance fund operation, taking into account the government’s and the residents’ financial and burdens, in order to ensure the sustainability of the health insurance fund operation.
3.2.3. Extraction of the Indicators through the Literature Summary
3.2.4. Environmental Variables
3.3. Data Source
4. Results
4.1. Correlation Analysis
4.2. Empirical Study
4.2.1. The Empirical Study Analysis at Stage 1
4.2.2. SFA Regression Results and Analysis at Stage 2
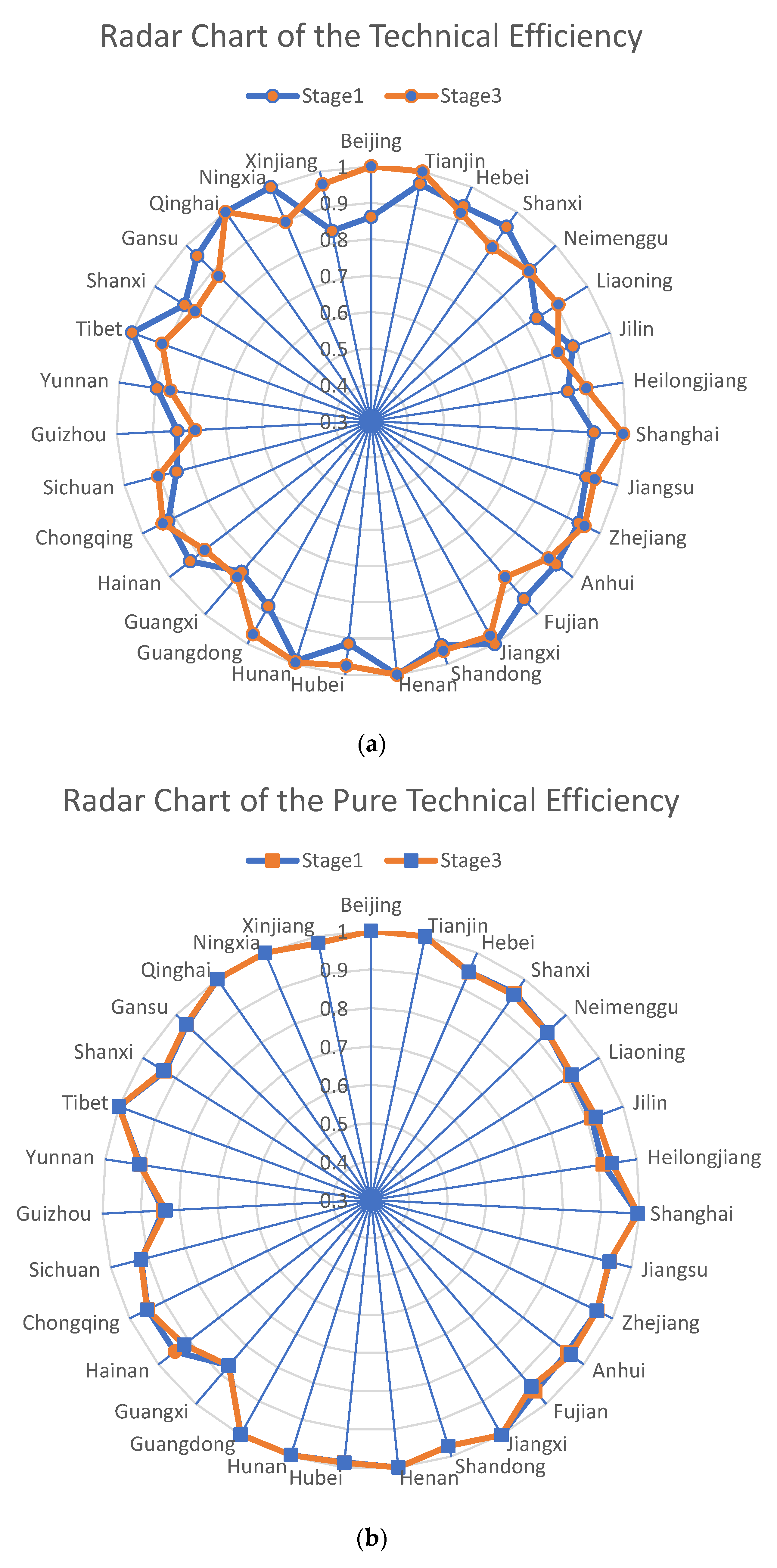
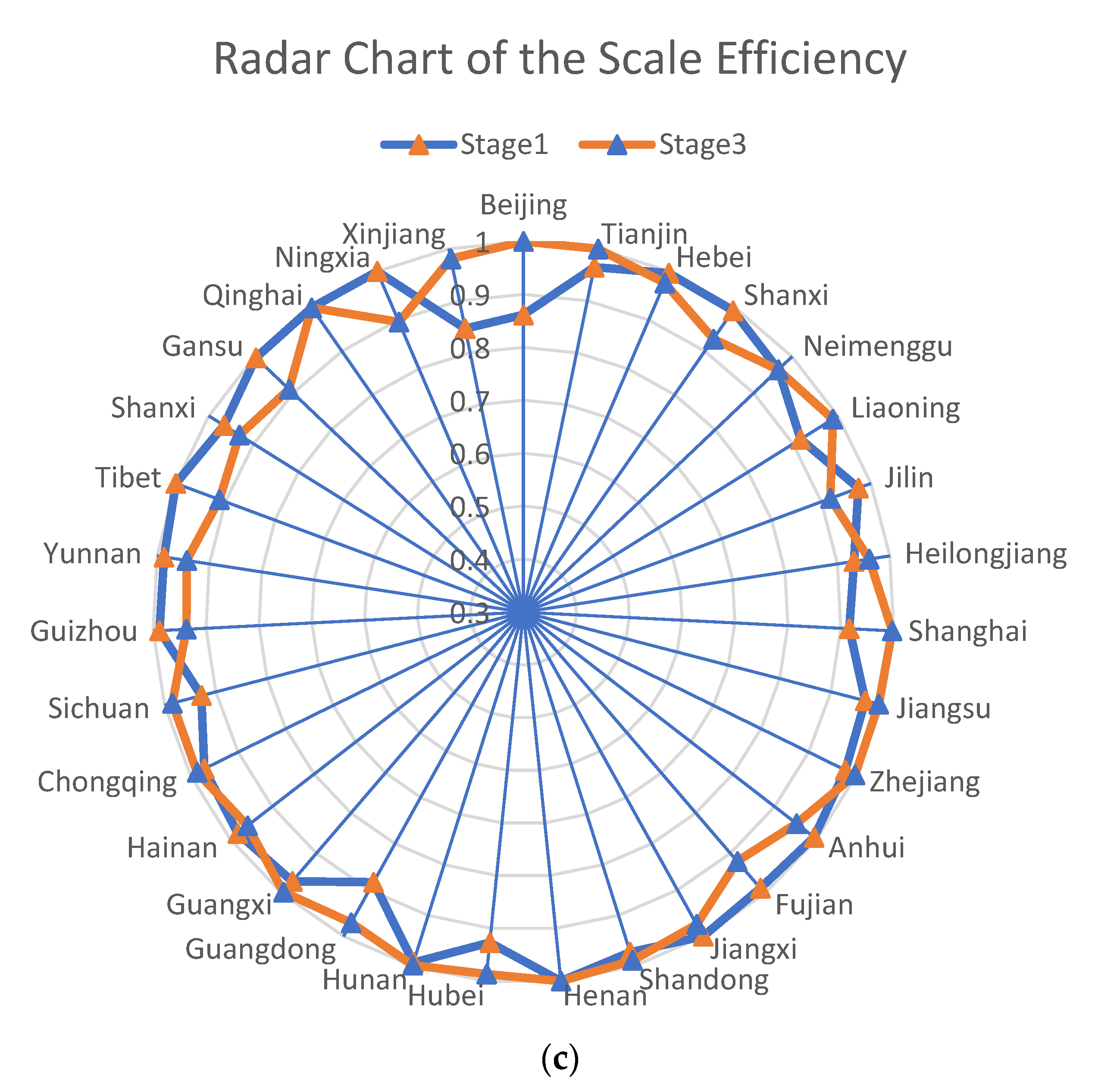
4.2.3. The Empirical Study after the Input Adjustment at Stage 3
Analysis of the Operational Efficiency Value of the Basic Medical Insurance for Urban and Rural Residents in China
Regional Distribution of the Technical Efficiency of the Basic Medical Insurance Funds in China
5. Conclusions
- (1)
- From the efficiency results, the efficiency values in the third stage differ from those in the first stage, and the number of the efficiency frontier regions decreases from five to four, indicating that the operation of the basic medical insurance is disturbed by the external environment, and it is necessary to exclude the environmental factors when measuring the efficiency values. Following the adjustment, except for two regions (Henan Province and Qinghai Province), which are in the efficiency frontier both before and after the adjustment, the efficiency of the basic medical insurance operations in all other regions has changed, to different degrees, compared with that before the adjustment, and there are great differences in the efficiency of the basic medical insurance fund operations in the different regions of China.
- (2)
- In terms of the environmental factors, the increase of the GDP per capita and the financial investment in the social security and employment, effectively reduce the input redundancy in the operation of the basic medical insurance, which is conducive to improving the efficiency of the medical insurance operation and to better protecting the health of residents. The high level of the GDP represents the economic development, which is conducive to increase the financial investment to improve the development level and speed of health care; the government increases the investment in the social security business, which can fundamentally improve the social security level to drive the high speed development of the medical insurance business; the financial income and expenditure ratio represents the government financial freedom, the higher the financial freedom, the greater the likelihood of the government’s investment in health technicians, which is conducive to the operation of the medical insurance, but it is undesirable to blindly increase this factor, which should make the operation efficiency of the basic medical insurance effectively improved on the basis of moderation.
- (3)
- In a cross-sectional comparison, Guizhou province has the lowest efficiency value of the basic health insurance operation, which, considering the local economic situation, indicates that the economic development affects the investment in health in Guizhou province, which in turn affects the level of social health and the efficiency of the health insurance operation there. However, a blind increase in the investment is not the best decision to improve the efficiency, and some provinces and cities with a good economic development are not in the efficiency frontier after excluding the environmental factors, which indicates that the investment of resources may cause waste, and a reasonable macro coordination is still needed to achieve the best efficiency.
- (4)
- In terms of a longitudinal comparison, the efficiency values of the 31 provinces, from 2017–2020, have been fluctuating erratically, indicating that China’s health insurance operation is still in a developmental stage and has not yet found an applicable and stable solution for the sustainable health insurance development.
6. Suggestions
- (1)
- Focusing on the economic construction and increasing the GDP, developing the economy, as the first priority, can improve the expansion of the social capital, enrich the medical talent team, and increase the number of health technicians. By enlarging the financial investment in health, we can improve the social health and health level, and fundamentally improve the efficiency of the health insurance operation. At the same time, we should improve the investment efficiency of the health insurance funds and broaden the investment channels.
- (2)
- While increasing investment in health care, it is more important to improve the level of health care services, reduce the slack variable of the investment, and improve the efficiency driven by quality. First, the government and hospitals should improve the level of management and allocation of resources, taking into account the regional economy, the health service level and other factors, to promote the standardized and high-efficiency development of the health care. Second, the technological innovation should be used to promote a high-quality development, develop technology platforms, develop “Internet+” medical care, improve the ability to monitor the health insurance funds, conduct real-time monitoring of the health insurance funds, and promptly identify problems in the operation of health insurance funds.
- (3)
- Complete the corresponding laws and regulations, improve the level of the health insurance supervision, and facilitate the transparency of the health insurance operation. At the same time, the system of using the medical insurance funds is refined to make the medical insurance system more sound. A robust medical insurance regulation is beneficial for the medical insurance funds to be taken from and used by the people, and to play a role in protecting people’s health, thus improving its operational efficiency. At the same time, the hybrid payment methods can be explored to curb the spike in medical expenditures. Currently there is an inflation of the health insurance fund expenditures, due to fraud, and due to the influential relationship of the payment methods on the irrational use of health insurance funds. China has been reforming its health insurance system in recent years, including the diagnosis-related groups by disease (DRGs) in hospitals, as well as the capitation and prepayment systems in the basic level [2]. Scientific payment methods are the key to control the overuse of services and drugs and the growing health care expenditures, which will drive the reform of the health insurance system [29], so the promotion of hybrid payments for health insurance is necessary.
7. Shortcomings and Research Prospects of This Paper
7.1. Shortcomings
- (1)
- Since the basic medical insurance for urban and rural residents in China started in 2016, the data were counted from 2017. The operation time is not long enough, and the model used is an efficiency measure for the current situation, so the results obtained, when conducting the empirical model analysis, cannot make a clear judgment on the expected development.
- (2)
- The resident health insurance system contains many elements and has a wide scope. This paper is based on the existing literature, as a reference, and the economic principles, as a guide to measure and analyze, so there are limitations in the selection of perspectives, the relevant indicators and the influencing factors.
7.2. Prospect
- (1)
- Continued data collection in subsequent studies may allow for the predictions of efficiency that could better improve the efficiency of the basic health insurance.
- (2)
- Based on this paper, we should continue to conduct a multi-faceted and more in-depth study on the basic medical insurance for urban and rural residents, in order to have a richer and stereoscopic research result. At the same time, since the studies on the operational efficiency of the basic medical insurance for urban and rural residents are still few, there is a need to refer to the relevant research methods in other fields for enrichment.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Outline of the Healthy China 2030 Plan. Available online: http://www.gov.cn/xinwen/2016-10/25/content_5124174.htm (accessed on 25 October 2016).
- Liu, K.; Liu, W.; Frank, R.; Lu, C. Assessing the long-term effects of Basic Medical Insurance on catastrophic health spending in China. Health Policy Plan. 2022, 37, 747–759. [Google Scholar] [CrossRef]
- Jing, L.; Chen, R.; Jing, L.; Qiao, Y.; Lou, J.; Xu, J.; Wang, J.; Chen, W.; Sun, X. Development and enrolee satisfaction with basic medical insurance in China: A systematic review and stratified cluster sampling survey. Int. J. Health Plan. Manag. 2017, 32, 285–298. [Google Scholar] [CrossRef]
- Jia, H. The Institutional Change of Basic Medical Insurance and the Improvement for Citizens’ Sense of Gain. Soc. Sci. J. 2022, 3, 39–49+52. [Google Scholar]
- China Built the World’s Largest Social Security System. Available online: http://www.gov.cn/xinwen/2020-12/07/content_5567819.htm (accessed on 7 December 2020).
- Charnes, A.; Cooper, W.W.; Rhodes, E. Measuring the efficiency of decision making units. Eur. J. Oper. Res. 1979, 2, 429–444. [Google Scholar] [CrossRef]
- Wang, S.; Yang, C.; Li, Z. Spatio-Temporal Evolution Characteristics and Spatial Interaction Spillover Effects of New-Urbanization and Green Land Utilization Efficiency. Land 2021, 10, 1105. [Google Scholar] [CrossRef]
- Fried, H.O.; Lovell, C.A.K.; Schmidt, S.S.; Yaisawarng, S. Accounting for Environmental Effects and Statistical Noise in Data Envelopment Analysis. J. Prod. Anal. 2002, 17, 157–174. [Google Scholar] [CrossRef]
- Hu, Y.; Wu, Y.; Zhou, W.; Li, T.; Li, L. A three-stage DEA-based efficiency evaluation of social security expenditure in China. PLoS ONE 2020, 15, e0226046. [Google Scholar] [CrossRef] [PubMed]
- Yi, M.; Peng, J.; Zhang, L.; Zhang, Y. Is the allocation of medical and health resources effective? Characteristic facts from regional heterogeneity in China. Int. J. Equity Health 2020, 19, 89. [Google Scholar] [CrossRef]
- Li, Z.; Si, X.; Ding, Z.; Li, X.; Zheng, S.; Wang, Y.; Wei, H.; Guo, Y.; Zhang, W. Measurement and Evaluation of the Operating Efficiency of China’s Basic Pension Insurance: Based on Three-Stage DEA Model. Risk Manag. Healthc. Policy 2021, 14, 3333–3348. [Google Scholar] [CrossRef]
- Chen, G.; Yan, X. Demand for voluntary basic medical insurance in urban China: Panel evidence from the Urban Resident Basic Medical Insurance scheme. Health Policy Plan. 2012, 27, 658–668. [Google Scholar] [CrossRef] [PubMed]
- Dong, K. Medical insurance system evolution in China. China Econ. Rev. 2009, 20, 591–597. [Google Scholar] [CrossRef]
- Zhu, K.; Zhang, L.; Yuan, S.; Zhang, X.; Zhang, Z. Health financing and integration of urban and rural residents’ basic medical insurance systems in China. Int. J. Equity Health 2017, 16, 194. [Google Scholar] [CrossRef]
- Liu, H.; Wang, C.; Wu, L. Decision Rights Allocation, Earnings Management and Investment Efficiency. Econ. Res. J. 2014, 49, 93–106. [Google Scholar]
- Medicare Payment Advisory Commission. Promoting Greater Efficiency in Medicare. In Report to the Congress; Medicare Payment Advisory Commission: Washington, DC, USA, 2007; Volume 6. [Google Scholar]
- Fang, P.; Zhang, X. China’s Basic Medical Insurance System: Evaluation and Outlook; Huazhong University of Science and Technology Press: Wuhan, China, 2015; Volume 1, pp. 99–100. [Google Scholar]
- Aigner, D.; Lovell, C.A.K.; Schmidt, P. Formulation and estimation of stochastic frontier production function models. J. Econom. 1977, 6, 21–37. [Google Scholar] [CrossRef]
- Banker, R.D.; Charnes, A.; Cooper, W.W. Some Models for Estimating Technical and Scale Inefficiencies in Data Envelopment Analysis. Manag. Sci. 1984, 30, 1078–1092. [Google Scholar] [CrossRef]
- Jondrow, J.; Lovell, C.A.K.; Materov, I.S.; Schmidt, P. On the estimation of technical inefficiency in the stochastic frontier production function model. J. Econom. 1982, 19, 233–238. [Google Scholar] [CrossRef]
- Dengyue, L. A Note on Estimating Managerial Inefficiency of Three-Stage DEA Model. Stat. Res. 2012, 29, 104–107. [Google Scholar]
- Chiu, C.-M.; Chen, M.-S.; Lin, C.-S.; Lin, W.-Y.; Lang, H.-C. Evaluating the comparative efficiency of medical centers in Taiwan: A dynamic data envelopment analysis application. BMC Health Serv. Res. 2022, 22, 435. [Google Scholar] [CrossRef] [PubMed]
- Ngobeni, V.; Breitenbach, M.C.; Aye, G.C. Technical efficiency of provincial public healthcare in South Africa. Cost Eff. Resour. Alloc. 2020, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Audibert, M.; Mathonnat, J.; Pelissier, A.; Huang, X.X.; Ma, A. Health insurance reform and efficiency of township hospitals in rural China: An analysis from survey data. China Econ. Rev. 2013, 27, 326–338. [Google Scholar] [CrossRef]
- Brockett, P.L.; Chang, R.E.; Rousseau, J.J.; Semple, J.H.; Yang, C. A Comparison of HMO Efficiencies as a Function of Provider Autonomy. J. Risk Insur. 2004, 71, 1–19. [Google Scholar] [CrossRef]
- Chuang, C.-L.; Chang, P.-C.; Lin, R.-H. An Efficiency Data Envelopment Analysis Model Reinforced by Classification and Regression Tree for Hospital Performance Evaluation. J. Med. Syst. 2011, 35, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
- Brockett, P.L.; Golden, L.L.; Yang, C.C. Potential “Savings” of Medicare: The Analysis of Medicare Advantage and Accountable Care Organizations. N. Am. Actuar. J. 2018, 22, 458–472. [Google Scholar] [CrossRef]
- Park, J.K.; Ryu, D.; Lee, K. What determines the economic size of a nation in the world: Determinants of a nation’s share in world GDP vs. per capita GDP. Struct. Chang. Econ. Dyn. 2019, 51, 203–214. [Google Scholar] [CrossRef]
- Singhvi, A.; Joshi, A.; Bagul, N.; Bhatia, S.; Singh, G.; Gupta, R. The insight for initiation and maintenance of areca nut chewing habit and its effects on oral health status among school age population in Western Rajasthan, India. J. Clin. Diagn. Res. 2016, 10, ZC15–ZC18. [Google Scholar] [CrossRef]

| Author | Region | Period of Study | Methods | Input Indicators | Output Indicators |
|---|---|---|---|---|---|
| Li et al. (2021) [9] | China | 2014–2019 | Three-stage DEA model | Fund income; Number of insured persons; | Fund expenditure; Number of recipients; |
| Chiu et al. (2022) [22] | Taiwan | 2015–2018 | Dynamic data envelopment analysis (DDEA) model | The number of doctors; The number of beds; Equipment expenditure. | Inpatient and outpatient revenue; Earnings; Rate of emergency transfer to the inpatient. |
| Ngobeni et al. (2020) [23] | South Africa | 2017–2018 | Data envelopment analysis (DEA) | Total health spending; Total health staff. | IMR (infant mortality rate). |
| Audibert et al. (2011) [24] | China | 2000–2008 | Two-stage DEA | The number of staff and equipment. | Number of recipients |
| Brockett et al. (2004) [25] | The U.S. | 1995 | Data envelopment analysis (DEA) | Total premium; Total expenses. | Ambulatory encounters; Hospital days. |
| Chuang et al. (2011) [26] | Taiwan | 2006 | DEA-ANN approach | The number of patient beds; The number of physicians and nurses; The number of professionals. | The number of inpatient days; The number of outpatient/emergency visits; The in-hospital survival rate. |
| Patrick et al. (2018) [27] | The U.S. | 2014 | Data envelopment analysis (DEA) | Health expenditures. | Enrollment; Inpatient admissions; Ambulatory encounters; |
| Yi et al. (2020) [10] | China | 2005–2017 | Three-stage DEA model | Financial input (GE); Labor input. | Diagnoses and treatment numbers; Mortality rate; Incidence rates. |
| Category | Variables | Mean | Standard Deviation | Minimum | Maximum | |
|---|---|---|---|---|---|---|
| Input indicators | Fund income | 262.8585484 | 215.73983 | 4.70 | 1561.00 | |
| Number of health technicians | 319,278.2903 | 202,100.02738 | 16,526.00 | 829,396.00 | ||
| Government health expenditure | 524.4196 | 308.28872 | 93.80 | 1772.99 | ||
| Output indicators | Fund expenditure | 229.2443548 | 170.43871 | 3.50 | 682.70 | |
| Epidemic morbidity rate | 227.7126613 | 91.90986 | 80.80 | 589.41 | ||
| Resident health insurance expenditure | 1756.071774 | 574.78107 | 271.50 | 3739.70 | ||
| Environmental Variables | GDP per capita | 66,532.7177 | 30,122.06163 | 28,497.00 | 164,889.00 | |
| Government financial level | Social security and employment expenditure | 879.3052 | 430.11084 | 107.92 | 1998.67 | |
| Fiscal revenue expenditure ratio | 0.4471 | 0.18748 | 0.10 | 0.88 | ||
| Fund Expenditure | Epidemic Morbidity Rate | Resident Health Insurance Expenditure | Fund Income | Number of Health Technicians | Government Health Expenditure | |
|---|---|---|---|---|---|---|
| Fund expenditure | 1 | |||||
| Epidemic morbidity rate | −0.258 *** | 1 | ||||
| Resident health insurance expenditure | −0.100 | −0.448 *** | 1 | |||
| Fund income | 0.802 *** | −0.164 | −0.107 | 1 | ||
| Number of health technicians | 0.899 *** | −0.314 *** | 0.035 | 0.730 *** | 1 | |
| Government health expenditure | 0.850 *** | −0.216 ** | −0.001 | 0.710 *** | 0.925 *** | 1 |
| Province | 2017 | 2018 | 2019 | 2020 | Mean |
|---|---|---|---|---|---|
| Beijing | 0.816 | 0.907 | 1 | 0.722 | 0.861 |
| Tianjin | 0.861 | 1 | 1 | 1 | 0.965 |
| Hebei | 0.915 | 0.936 | 0.945 | 0.974 | 0.943 |
| Liaoning | 0.795 | 0.926 | 0.877 | 0.745 | 0.836 |
| Shanghai | 0.981 | 1 | 0.795 | 0.873 | 0.912 |
| Jiangsu | 0.862 | 0.862 | 0.933 | 0.984 | 0.910 |
| Zhejiang | 1 | 0.999 | 0.865 | 0.876 | 0.935 |
| Fujian | 0.87 | 0.945 | 0.963 | 1 | 0.946 |
| Shandong | 1 | 0.94 | 0.898 | 0.944 | 0.946 |
| Guangdong | 0.878 | 0.94 | 0.811 | 0.899 | 0.882 |
| Hainan | 0.875 | 0.913 | 0.927 | 1 | 0.929 |
| Shanxi | 0.851 | 0.986 | 1 | 0.965 | 0.9505 |
| Jilin | 0.875 | 0.894 | 1 | 0.793 | 0.8905 |
| Heilongjiang | 0.866 | 0.846 | 0.911 | 0.764 | 0.847 |
| Anhui | 0.79 | 0.981 | 1 | 1 | 0.943 |
| Jiangxi | 1 | 1 | 1 | 1 | 1 |
| Henan | 1 | 1 | 1 | 1 | 1 |
| Hubei | 0.825 | 0.914 | 0.939 | 0.98 | 0.915 |
| Hunan | 0.966 | 0.995 | 0.998 | 1 | 0.990 |
| Neimenggu | 0.894 | 1 | 0.875 | 0.835 | 0.901 |
| Guangxi | 0.623 | 0.807 | 0.953 | 1 | 0.846 |
| Chongqing | 0.956 | 0.878 | 0.887 | 0.961 | 0.921 |
| Sichuan | 0.823 | 0.806 | 0.845 | 0.935 | 0.852 |
| Guizhou | 0.666 | 0.976 | 0.828 | 0.862 | 0.833 |
| Yunnan | 0.871 | 0.885 | 0.891 | 0.934 | 0.895 |
| Tibet | 1 | 1 | 1 | 1 | 1 |
| Shanxi | 0.97 | 0.996 | 0.908 | 0.742 | 0.904 |
| Gansu | 1 | 1 | 0.927 | 0.91 | 0.959 |
| Qinghai | 1 | 1 | 1 | 1 | 1 |
| Ningxia | 1 | 1 | 1 | 1 | 1 |
| Xinjiang | 0.717 | 0.984 | 0.971 | 0.663 | 0.834 |
| Mean | 0.889 | 0.946 | 0.934 | 0.915 | 0.921 |
| Variables | Fund Income | Number of Health Technicians | Government Health Expenditure |
|---|---|---|---|
| GDP per capita | −73.78 *** | −38,597.19 *** | −152.38 * |
| Social security and employment expenditure | −87.84 *** | −58,345.06 *** | −125.65 * |
| Fiscal revenue expenditure ratio | 10.02 *** | −1226.08 *** | 6.90 * |
| Sigma-squared | 18,275.43 *** | 4,360,611,600.00 *** | 6886.31 * |
| Gamma | 0.87 *** | 0.53 *** | 0.02 * |
| Log likelihood function | −712.59 *** | −1518.81 *** | −729.46 * |
| LR test of the one-sided error | 124.86 *** | 17.89 *** | 4.64 * |
| Results of Stage 1 | Results of Stage 3 | |||||
|---|---|---|---|---|---|---|
| TE | PTE | SE | TE | PTE | SE | |
| Beijing | 0.86125 | 1 | 0.86125 | 1 | 1 | 1 |
| Tianjin | 0.96525 | 1 | 0.96525 | 1 | 1 | 1 |
| Hebei | 0.9425 | 0.9455 | 0.9965 | 0.9235 | 0.946 | 0.97625 |
| Shanxi | 0.9505 | 0.95625 | 0.99325 | 0.88175 | 0.9505 | 0.92825 |
| Neimenggu | 0.901 | 0.9335 | 0.96475 | 0.89775 | 0.9335 | 0.964 |
| Liaoning | 0.83575 | 0.91175 | 0.91675 | 0.906 | 0.9165 | 0.98875 |
| Jilin | 0.8905 | 0.9125 | 0.97475 | 0.84725 | 0.92425 | 0.91825 |
| Heilongjiang | 0.84675 | 0.91075 | 0.93175 | 0.89775 | 0.93475 | 0.96075 |
| Shanghai | 0.91225 | 0.995 | 0.91625 | 0.99275 | 0.9955 | 0.99725 |
| Jiangsu | 0.91025 | 0.94125 | 0.96675 | 0.93425 | 0.94075 | 0.99325 |
| Zhejiang | 0.935 | 0.956 | 0.97725 | 0.95275 | 0.955 | 0.99775 |
| Anhui | 0.94275 | 0.94725 | 0.99425 | 0.9165 | 0.9575 | 0.95225 |
| Fujian | 0.9445 | 0.95675 | 0.987 | 0.865 | 0.94075 | 0.92 |
| Jiangxi | 1 | 1 | 1 | 0.97425 | 1 | 0.97425 |
| Shandong | 0.9455 | 0.97175 | 0.973 | 0.961 | 0.97175 | 0.98925 |
| Henan | 1 | 1 | 1 | 1 | 1 | 1 |
| Hubei | 0.9145 | 0.98675 | 0.92725 | 0.975 | 0.988 | 0.98675 |
| Hunan | 0.98975 | 0.99625 | 0.9935 | 0.99475 | 0.99625 | 0.9985 |
| Guangdong | 0.882 | 0.99875 | 0.88325 | 0.9695 | 0.99875 | 0.9705 |
| Guangxi | 0.84575 | 0.86775 | 0.96975 | 0.865 | 0.86875 | 0.99625 |
| Hainan | 0.92875 | 0.94525 | 0.98225 | 0.8785 | 0.9155 | 0.959 |
| Chongqing | 0.9205 | 0.948 | 0.97125 | 0.9375 | 0.9495 | 0.9865 |
| Sichuan | 0.85225 | 0.9185 | 0.92825 | 0.9045 | 0.919 | 0.985 |
| Guizhou | 0.833 | 0.84175 | 0.9885 | 0.784 | 0.8355 | 0.93725 |
| Yunnan | 0.89525 | 0.90775 | 0.98675 | 0.858 | 0.91 | 0.94325 |
| Tibet | 1 | 1 | 1 | 0.91225 | 1 | 0.91225 |
| Shanxi | 0.904 | 0.933 | 0.96625 | 0.8705 | 0.937 | 0.932 |
| Gansu | 0.95925 | 0.962 | 0.997 | 0.87875 | 0.964 | 0.9105 |
| Qinghai | 1 | 1 | 1 | 1 | 1 | 1 |
| Ningxia | 1 | 1 | 1 | 0.896 | 1 | 0.896 |
| Xinjiang | 0.83375 | 0.982 | 0.8465 | 0.96425 | 0.982 | 0.981 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.; Gao, Y.; Li, H.; Zhang, L.; Sun, J. Analysis of the Operational Efficiency of Basic Medical Insurance for Urban and Rural Residents: Based on a Three-Stage DEA Model. Int. J. Environ. Res. Public Health 2022, 19, 13831. https://doi.org/10.3390/ijerph192113831
Liu T, Gao Y, Li H, Zhang L, Sun J. Analysis of the Operational Efficiency of Basic Medical Insurance for Urban and Rural Residents: Based on a Three-Stage DEA Model. International Journal of Environmental Research and Public Health. 2022; 19(21):13831. https://doi.org/10.3390/ijerph192113831
Chicago/Turabian StyleLiu, Tong, Yufei Gao, Hui Li, Liping Zhang, and Jiangjie Sun. 2022. "Analysis of the Operational Efficiency of Basic Medical Insurance for Urban and Rural Residents: Based on a Three-Stage DEA Model" International Journal of Environmental Research and Public Health 19, no. 21: 13831. https://doi.org/10.3390/ijerph192113831
APA StyleLiu, T., Gao, Y., Li, H., Zhang, L., & Sun, J. (2022). Analysis of the Operational Efficiency of Basic Medical Insurance for Urban and Rural Residents: Based on a Three-Stage DEA Model. International Journal of Environmental Research and Public Health, 19(21), 13831. https://doi.org/10.3390/ijerph192113831






